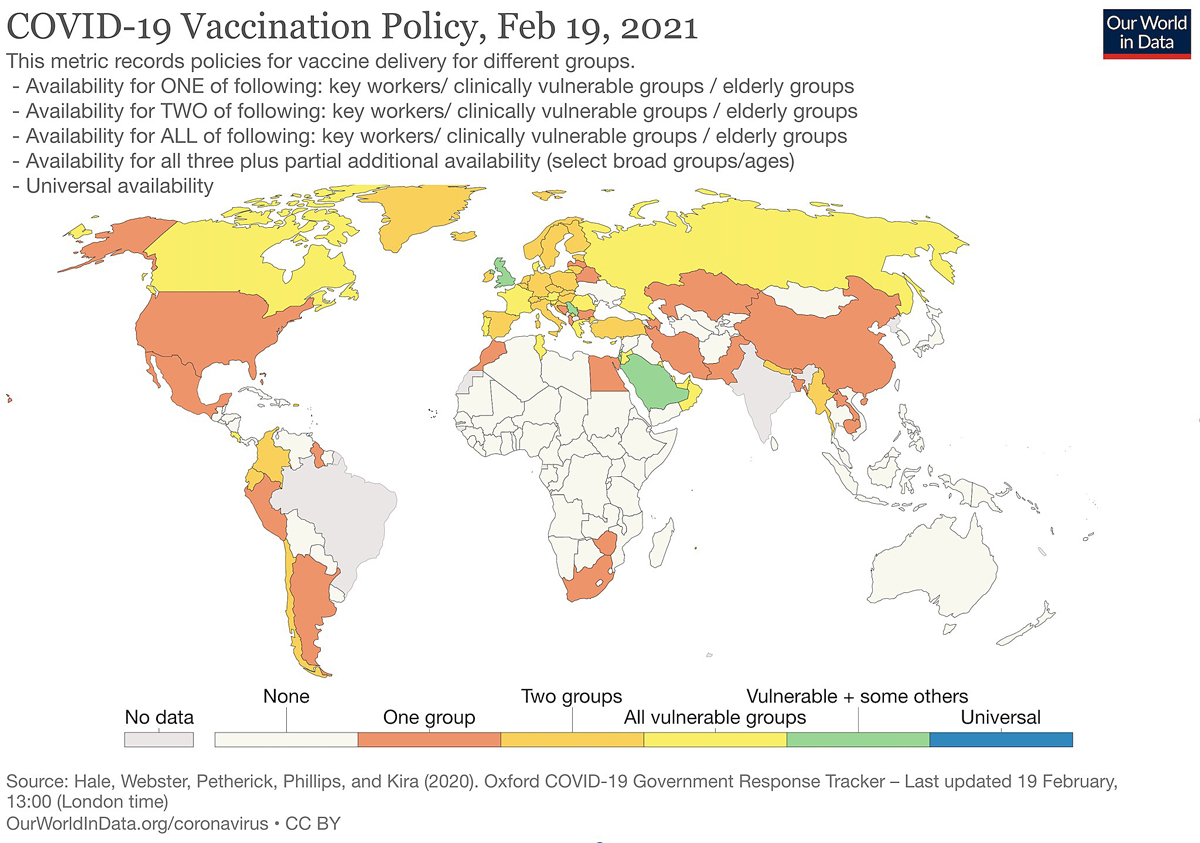
Figure 1 Access to vaccines and vaccination policy according to country.
DOI: https://doi.org/10.4414/smw.2021.20488
Over past months, several effective COVID-19 vaccine candidates have been developed in different countries around the world, with some of them still being in the approval phase. At the same time, the impossibility of having enough vaccines for everyone in the near future has opened the floor for a debate about the priority of values and ethical principles that should guide vaccine allocation. There are, most notably, two main opposing ideas, with several views in between. Some argue that vaccines should be allocated equitably at the global level, and others claim that it is right and proper for governments to prioritise populations at the national level. What we currently see is that some high-income countries (HICs) have launched massive COVID-19 vaccination campaigns, whereas many low- and middle-income countries (LMICs) will have to wait considerably before immunisation can be started because of limited access to vaccines. As current data suggest, vaccination has barely started and progressed in many LMICS, which means that the most vulnerable groups and healthcare workers remain unprotected (figures 1 and 2 ). In view of the current situation, it is crucial to address if (at all) and why wealthier countries should support less affluent populations.
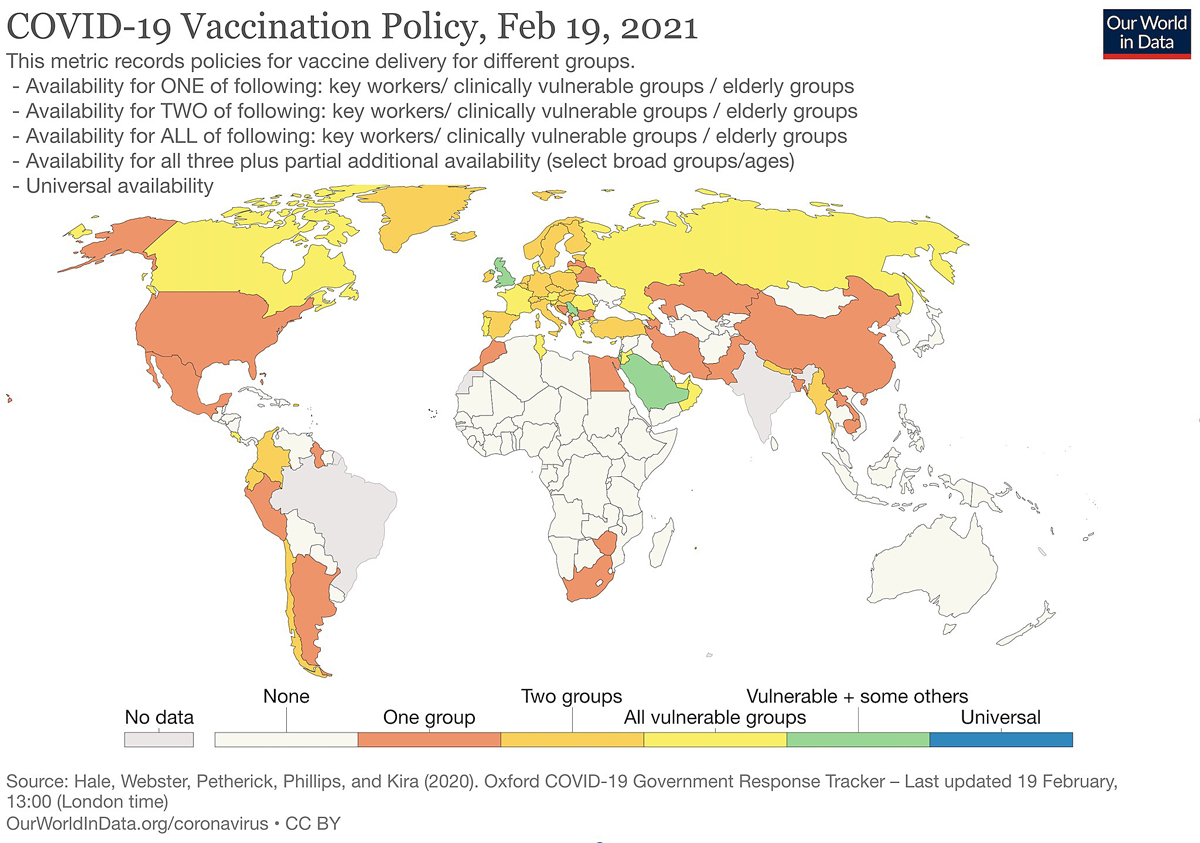
Figure 1 Access to vaccines and vaccination policy according to country.
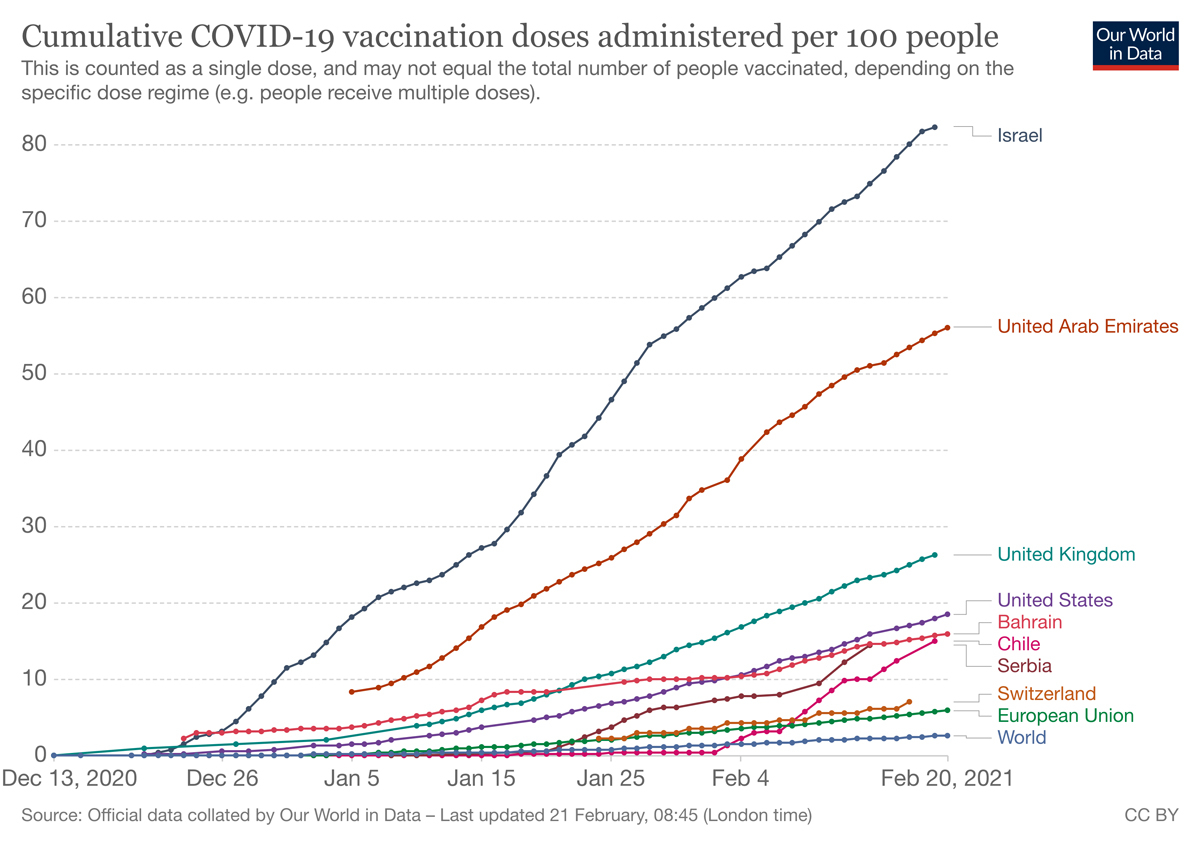
Figure 2 Cumulative COVID-19 vaccination doses administered by country.
The view in favour of prioritising populations at the national level is commonly referred to as “vaccine nationalism”. This position encourages governments to use law and other mechanisms to secure priority access to future vaccines, for example through Advance Purchase Commitments (APAs) with vaccine manufacturers. APAs are one way to serve national interest, but at the same time they erode collaboration between countries (many countries end up hoarding more vaccines than needed). APAs have been criticised for lacking transparency and, importantly, for driving up the prices of vaccine candidates and related materials as countries start competing against each other [1].
There is no doubt that global cooperation is necessary to effectively stop the pandemic. Reducing virus circulation, preventing the spread of new virus mutations, protecting the vulnerable, and ultimately decreasing suffering and death will only be achieved through strong cooperative efforts at the international level. This insight is well captured by the slogan “no one is safe until everyone is safe”, which appeals to a certain degree of self-interest while serving as a rationale for countries to cooperate at the international level, and similarly for the World Health Organization (WHO), United Nations Children’s Fund (UNICEF) and non-governmental organisations to sustain such cooperation.
The COVAX facility is a recent example of a distributive scheme to strengthen global cooperation in a way that is compatible with national interests. It offers access to a minimum stock of vaccines to all countries, regardless of their ability to pay [2–5]. Aligned with WHO, the facility has the goal of distributing vaccines equitably – to LMICs as well as to HICs – within a global allocation framework, which is being set up to ensure that persons in especially vulnerable situations get priority. So far, COVAX’s distribution framework is conceptualised in a way that countries pay according to their ability, which later allows them to access a certain number of doses sufficient to cover up to 20% of their population. Very poor countries are even guaranteed access to vaccines without any financial contribution [2–4, 6]. Within this scheme, high priority populations – especially health workers, high-risk groups and the elderly – will benefit the most.
Effective control of COVID-19 is not the only goal of COVAX. The facility is also thought to offer a redistribution mechanism through which especially low-income countries get access to vaccines that would otherwise be unaffordable for them. But rich countries stand to benefit as well because the facility offers an insurance mechanism: countries are guaranteed access to a portfolio of successful vaccine candidates. Thus, if one vaccine fails in development, participating countries will still have the option to obtain other candidates, which ensures that risks are spread. There is widespread consensus – motivated by solidarity or simple self-interest – that everyone should have access to a safe and effective COVID-19 vaccine, at least until herd immunity has been established globally. Still, a normative discussion needs to identify the actors who have a duty to contribute towards this goal, that is, HIC governments, international organisations, the industry and other stakeholders. It also needs to be discussed how far-reaching these duties are. For instance, can pharmaceutical companies be expected to offer COVID-19 vaccines at production costs or to forgo their intellectual property rights all together? Is a country morally obliged to limit vaccine access to high-risk groups, and provide access to other citizens only once high-risk groups have been served globally?
Here, we will focus on the role of governments. “Vaccine nationalists” would endorse the view that every government has a (moral) duty to give priority to its own population before helping citizens abroad. This seems to be the position of some HICs, which have ordered and hoarded more vaccines than what their current populations need. This would imply that nation states are allowed to negotiate multiple (and redundant) APAs, and to forgo their participation in a redistributive scheme. Wealthier countries may ex ante enter into bilateral negotiations with the manufacturers to safeguard high quantities of vaccine doses for their own population, given that global cooperation efforts under non-ideal circumstances are not guaranteed and that there is no certainty of the approval and success of all vaccines under development.
This is contrasted by the position “vaccine cosmopolitans” hold, that is, the view of distributive justice for vaccines according to which citizenship or community membership is ethically irrelevant. Vaccine cosmopolitans claim that justice demands that vaccine allocation should be independent of the recipients’ national identities and, generally speaking, associative ties, which implies we ought to find other (fair) allocation criteria, irrespective of borders. Most notably, such criteria will prioritise supply to countries according to their need (considering, e.g., the rate of deaths and infections) or will allocate vaccines in proportion to the size of a country’s population [7–9]. Cosmopolitans may differ in their vision of fair distribution principles, but agree that any allocation principle ought to give equal consideration to individuals independently of their national ties. Translating this view into allocation models, “vaccine cosmopolitans” would most likely support global allocation mechanisms, such as COVAX, and morally condemn (excessive) bilateral agreements made by affluent countries.
Just as cosmopolitanism comes in different shades, nationalism, too, exists in stronger and weaker forms. An intermediary nationalist position may, for instance, argue that limited national partiality in allocating vaccines is not necessarily an obstacle to justice considerations, but can be part of them [10]. Countries have community-embedded responsibilities to prioritise their own population. However, prioritising one’s own population is not irreconcilable with the recognition of certain duties towards all persons, regardless of citizenship and identity. Following this argument, the question arises of just how much commitment and self-limitation can be asked from wealthier countries in order to promote access to vaccines for poorer countries. Can they buy vaccines for their entire population? Just enough to get herd immunity, or even less when there are other countries in much more need? Should there be caps limiting how much countries can buy through APAs?
Since there is to date no global governance mechanism coordinating or sanctioning non-cooperating countries, distributive schemes, such as COVAX, can only be implemented as a voluntary cooperative, which implies that wealthier countries need to be incentivised to join the facility. Global coordination offered by the COVAX facility still lacks “teeth”: without a persuasive and solid rationale for global collaboration, countries prefer to safeguard vaccines within bilateral agreements, even when they join COVAX. In the realm of Realpolitik, other options are not in sight for many countries. So far, only very few vaccine doses have been administered in low-income countries [11]. Many middle-income countries are in a difficult situation: not poor enough to access vaccines through donations mediated by international health organisations. Although they do not have the purchasing power to get good deals, they still try to enter in bilateral agreements [1].
Defining who should have access to vaccines first and why is a complex, important and pressing task. We need to publicly debate what we mean by “equitable access” to COVID-19 vaccines, whether the prioritisation of individuals should take place at a global level or be decided by countries, and what allocation criteria and mechanisms should look like. Although vaccine allocation will have to start before consensus has been reached, such debates will contribute to the improvement, legitimation and acceptance of evolving policies, and will eventually foster societies’ pandemic resilience.
Figure 3 Invitation to the Forum for Global Health Ethics: Equitable Access to COVID-19 Vaccines (online event ‒ click here to join the event, password 621417. No registration needed.)
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Bollyky TJ , Bown CP . The Tragedy of Vaccine Nationalism: Only Cooperation Can End the Pandemic. Foreign Aff. 2020;99:96. Available from: https://www.foreignaffairs.com/articles/united-states/2020-07-27/vaccine-nationalism-pandemic.
2Gavi, the Vaccine Alliance. COVID-19 Vaccine Global Access (COVAX) Facility. Preliminary technical design. Discussion document, 2020 June 11. Available from: https://www.keionline.org/wp-content/uploads/COVAX-Facility-Preliminary-technical-design-061120-vF.pdf
3Gavi, the Vaccine Alliance. What is the COVAX pillar, why do we need it and how will it work? Gavi CEO Dr Seth Berkley explains why it is so important for countries to join the COVAX Pillar and how this will help bring the COVID-19 pandemic to an end. Interview published 2020 June 26. Available from: https://www.gavi.org/vaccineswork/gavi-ceo-dr-seth-berkley-explains-covax-pillar
4Gavi, the Vaccine Alliance. The COVAX facility. Global procurement for COVID-19 vaccines. 2020. Online available at https://www.gavi.org/sites/default/files/covid/COVAX-Facility-background.pdf+
5 Phelan AL , Eccleston-Turner M , Rourke M , Maleche A , Wang C . Legal agreements: barriers and enablers to global equitable COVID-19 vaccine access. Lancet. 2020;396(10254):800–2. doi:.https://doi.org/10.1016/S0140-6736(20)31873-0
6 Lie RK , Miller FG . Allocating a COVID-19 Vaccine: Balancing National and International Responsibilities. Milbank Q. 2020;1468-0009.12494. doi:.https://doi.org/10.1111/1468-0009.12494
7 Emanuel EJ , Persad G , Kern A , Buchanan A , Fabre C , Halliday D , et al. An ethical framework for global vaccine allocation. Science. 2020;369(6509):1309–12. doi:.https://doi.org/10.1126/science.abe2803
8 Emanuel EJ , Luna F , Schaefer GO , Tan KC , Wolff J . Enhancing the WHO’s proposed framework for distributing COVID-19 vaccines among countries. Am J Public Health. 2021;111(3):371–3. doi:.https://doi.org/10.2105/AJPH.2020.306098
9World Health Organization (WHO). Fair allocation mechanism for COVID-19 vaccines through the COVAX facility. 2020 September 9. Available from: https://www.who.int/publications/m/item/fair-allocation-mechanism-for-covid-19-vaccines-through-the-covax-facility
10 Ferguson K , Caplan A . Love thy neighbour? Allocating vaccines in a world of competing obligations. J Med Ethics. 2020;0:1–4.
11Safi M. WHO: just 25 Covid vaccine doses administered in low-income countries. The Guardian. 2021 January 18. Available from: https://www.theguardian.com/society/2021/jan/18/who-just-25-covid-vaccine-doses-administered-in-low-income-countries
No financial support and no other potential conflict of interest relevant to this article was reported.