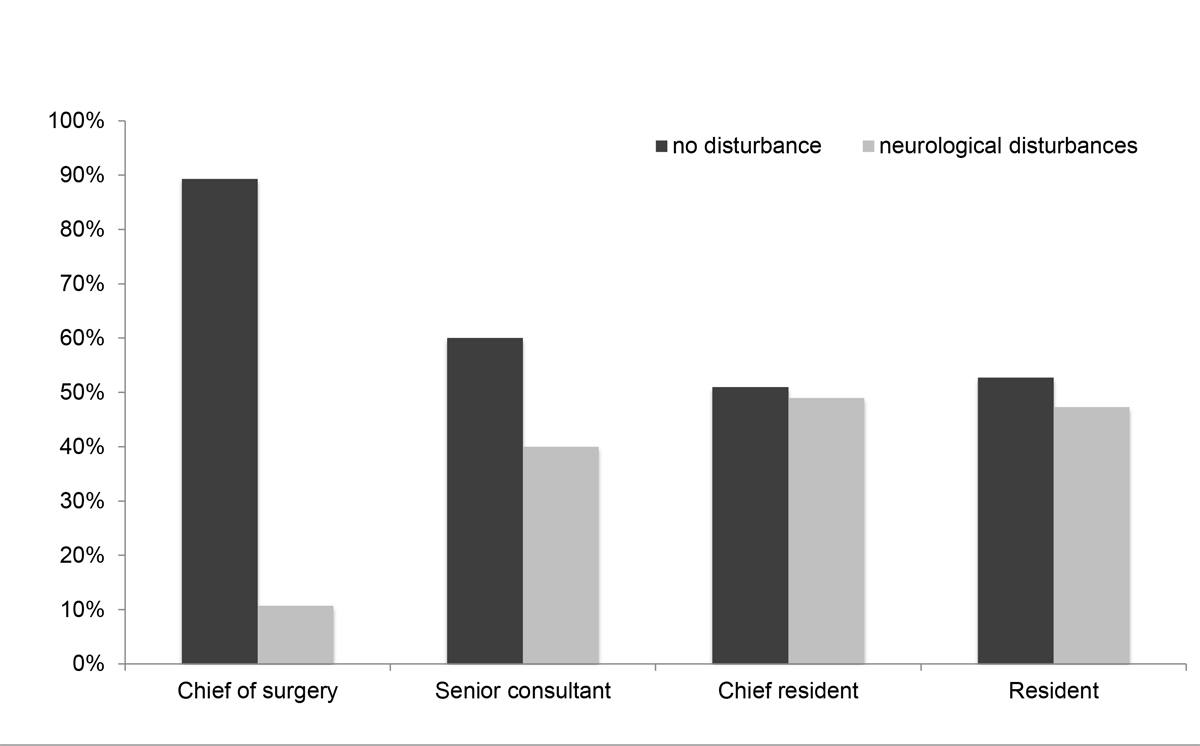
Figure 1 Incidence of neurological disturbances according to the training level of the operating surgeon at 6 week follow up.
DOI: https://doi.org/10.4414/smw.2021.20455
The lifetime risk for symptomatic inguinal hernia in adult men is up to 16%, making hernioplasty one of the most frequent surgical procedures around the world [1]. In the last decades the Lichtenstein technique became the gold standard of open inguinal hernia repair [2, 3]. As an alternative approach, endoscopic operations are increasingly performed, with comparable results according to the European Hernia Society [4]. Annually, there are more than 17,500 inguinal hernia operations performed in Switzerland [5]. Even though the recurrence rate – less than 5% – is satisfying, up to 11% of patients are reported to suffer from posthernioplastic chronic pain [6, 7]. Persistent pain affects everyday activities in 5–8% of these patients even several years after the initial surgical intervention [6, 8, 9]. Associated subsequent problems include depression, long time off work and job loss [10]. Decreasing the incidence of postoperative chronic pain is therefore the major challenge of modern hernia surgery [11]. Postoperative chronic pain is thought to originate from subsequent tissue reaction, nerve resection during surgery, nerve compression due to the sutures, a periostal reaction due to too deep applied sutures at the caudal mesh, tension on muscle fibres or a foreign body reaction caused by the mesh [1, 6].
In the early years of the Lichtenstein hernioplasty technique, monofilament, polypropylene meshes were commonly used. Alternatively there is a polyester mesh, which according to Sadowski gives comparable outcomes in terms of postoperative pain and quality of life [12]. The Parietex ProGrip™ mesh, a self-gripping and lightweight macroporous mesh, is about 45% lighter than a standard polypropylene mesh [13]. Use of this mesh was meant to eliminate the risk of accidental nerve suturing and to diminish fibrosis during recovery, and therefore to reduce the incidence of chronic inguinal pain [13, 14].
There is an ongoing debate as to whether self-gripping meshes have an increased recurrence rate or are comparable to standard mesh [6, 13, 15, 16]. There is a similar debate about postoperative pain with self-gripping versus standard mesh [17]. The necessity of optimising the outcome of open inguinal hernia repair still remains and has capacity for improvement. The aim of this study was to assess the feasibility, safety, implementation, and short- and long-term outcomes of open inguinal hernia repair using a self-gripping lightweight mesh in a university affiliated peripheral teaching hospital.
This was a retrospective single-centre, single-cohort outcomes study evaluating the use of self-gripping lightweight mesh (Parietex ProGrip™) in patients undergoing open inguinal hernia repair according to the Lichtenstein technique.
Patients were operated on at the Cantonal Hospital Olten, Switzerland, a university-affiliated peripheral teaching hospital, between 1 October 2010 and 31 January 2012, in both an in- and an outpatient setting. The hospital setting is the surgical department of the Cantonal Hospital Olten. The catchment area for the hospital is about 100,000 people in the surrounding area. The study protocol was approved by the ethics committee (Ethikkommission Nordwest- und Zentralschweiz EKNZ) and was conducted in accordance with the Declaration of Helsinki. Data were reported according to the STROBE guidelines [18].
Inclusion criteria were symptomatic uni- or bilateral inguinal hernia, confirmed clinically by a consultant surgeon in the outpatient clinic. Written informed consent for surgery had to be given prior to the operation. Because of the retrospective study design, informed consent for study participation was not obtained. Exclusion criteria were previous surgery for inguinal hernia, age younger than 18 years or planned endoscopic hernia repair.
A general preoperative assessment according to a questionnaire was performed with specific inquiries about preoperative pain and change of sensation, such as hypaesthesia or paraesthesia. The questions used were: “From a scale from zero to ten (zero as no pain, ten as maximum pain), how severe was the pain before surgery, before hospital discharge and at 6-week follow up?”, “How long was your inability of work in days?”, “How many painkillers did you take after surgery due to postoperative pain (numbers of tablets)?”, “Do you feel any loss of sensation? (yes or no)”, “Do you have or did you notice any swelling in the groin? (yes or no)”, “Do you have any load-dependent pain in the groin? (yes or no)”, “Do you have symptoms that make you think you have a recurrent hernia? (yes or no)”.
During surgery, the type of hernia, nerve identification and, if needed, nerve resection as well as suture fixation and the level of the operating surgeon were noted. During the hospital stay – after surgery – pain and surgical site infection were assessed. Within the first scheduled follow-up examination at the outpatient clinic 6 weeks postoperatively, pain and need for painkillers, as well as sensation disturbance or neuralgia and hernia recurrence were recorded. The final assessment included review of the medical charts, up to 5 years postoperatively until August 2016, for specific consultations, recurrences and reoperations. There was no formal sample size calculation. Instead, a study period duration of 16 months was considered to be adequate and feasible.
For further analyses, the quantitative variables were entered in a single Excel spreadsheet using a numeric code. Our patient group was not divided prior to data analyses; all patients were analysed in one cohort.
The surgical technique used for inguinal hernia repair was the Lichtenstein technique [2]. After an open approach to the inguinal hernia, the transversalis fascia, which builds the weak posterior wall of the inguinal canal, is reinforced with a tension-free mesh. The mesh is anchored at the inferior border of the inguinal ligament and the fascia of the internal oblique muscle. In our study, we used a self-gripping lightweight mesh which is described in detail elsewhere [19].
Continuous variables were compared with student’s t-test, the Mann-Whitney U-test, and the Kruskal-Wallis H-test, where appropriate. Differences between proportions derived from categorical data were compared using the Fisher exact test and the Pearson χ2 test, where appropriate. Hernia recurrence was assessed with the Kaplan-Maier function; the log-rank test was used for comparison purposes. Patients who were lost to follow up or for whom follow up ended were censored. All p-values were two-sided and considered statistically significant if p <0.05. Statistical analysis was performed using R version 3.3.2 (R Core Team, GNU GPL v2 License), R Studio version 1.0.44 (RStudio, Inc. GNU Affero General Public License v3, Boston, MA, 2016) with the graphical user interface (GUI) rBiostatistics.com alpha version (rBiostatistics.com, London, UK, 2017).
A total of 162 patients were included in this study, 53 of whom were treated in an outpatient setting. In total, 157 patients had a unilateral inguinal hernia and 5 patients had bilateral hernias. Complete follow-up data were available for 152 patients, with 10 patients lost to follow up. Baseline characteristics are reported in table 1. Direct, indirect and combined inguinal hernias were detected in 64, 84 and 12 patients, respectively, and 1 patient had a femoral hernia. The mesh was additionally fixed with sutures in the first nine patients owing to initial concerns that the mesh could displace, which turned out to be unfounded. In 32 patients, it was found intraoperatively that a nerve running through the surgical site would probably lead to postoperative pain, which is why it was resected; resection of the ilioinguinal nerve, the genital nerve or both was performed in 15, 9 and 8 patients, respectively. The mean duration of postoperative pain medication was 4.85 days (interquartile range [IQR] 0.0–7.0). The follow-up examination was after a median of 6.0 weeks (IQR 6.0–6.14). The mean time of inability to work was 13.76 days (IQR 0–21).
Table 1 Baseline characteristics.
| n (%) | median | min | max | ||
|---|---|---|---|---|---|
| Patients | 162 | ||||
| Age in years, median (IQR) | 59.0 (47.6 - 72.1) | 19 | 99 | ||
| Gender | Male | 158 (97.5) | |||
| Female | 4 (2.5) | ||||
| Hernia type | Direct | 64 (39.5) | |||
| Indirect | 84 (51.9) | ||||
| Combined | 12 (7.4) | ||||
| Femoral | 1 (0.6) | ||||
| Not mentioned | 1 (0.6) | ||||
| Hernia side | Left | 75 (46.3) | |||
| Right | 82 (50.6) | ||||
| Bilateral | 5 (3.1) | ||||
| Suturing | Yes | 9 (5.6) | |||
| No | 151 (93.2) | ||||
| Not mentioned | 2 (1.2) | ||||
| Nerve resection | None | 129 (79.6) | |||
| Ilioinguinal | 15 (9.3) | ||||
| Genital branch | 9 (5.6) | ||||
| Both | 8 (4.9) | ||||
| Need of pain medication in days, median (IQR) | 2.0 (0.0-7.0) | 0 | 42 | ||
| Inability of work in days, median (IQR) | 7.0 (0.0-25.0) | 0 | 90 | ||
| Pain in NRS, median (IQR) | Postoperatively | 2.0 (0.0 bis 5.0) | 0 | 10 | |
| At 6 week follow up | 1.0 (1.0-1.0) | 0 | 8 | ||
| Pain in NRS, mean (SD) | Before hospital discharge | 2.74 (2.63) | |||
| At 6 week follow up | 1.12 (1.06) | ||||
| Surgical site infection | Yes | 1 (0.6) | |||
| No | 149 (92.0) | ||||
| Neurological disturbances or neuralgia | Yes | 86 (53.1) | |||
| No | 57 (35.2) | ||||
| Hernia recurrence | Yes | 5 (3.2 3.1) | |||
| No | 149 (92.0) | ||||
| Reoperation | Recurrence | 3 (1.9) | |||
| Hematoma relief | 2 (1.3) | ||||
| Arterial bleeding | 1 (0.6) | ||||
| Anesthesia type | Spinal anesthesia | 104 (64.2) | |||
| Intubation narcosis | 45 (27.8) | ||||
| Laryngeal mask airway | 12 (7.4) | ||||
| local anesthesia | 1 (0.6) | ||||
| Follow up after surgery in weeks, median (IQR) | 6.0 (6.0-6.1) | 2 | 60 | ||
| Senior consultant | 101 (62.3) | ||||
| Chief resident | 47 (29.0) | ||||
| 1st surgeon level | Chief of surgery | 32 (19.8) | |||
| Senior consultant | 13 (8.0) | ||||
| Chief resident | 55 (34.0) | ||||
| Resident | 57 (35.2) | ||||
| Operation duration in minutes, median (IQR) | 40.0 (25.0-55.8) | 10 | 120 | ||
IQR: Inter-quartile range. Results may not add to 162 due to missing values. Percentages may not add to 100% due to missing values of defined.
Median time to last follow up was 5.6 years and hernia recurrence occurred in five patients (three patients operated on by a chief resident, two by a resident). The 1-, 3- and 5-year recurrence rates were 1%, 2% and 3%, respectively. Six patients had a reoperation, of whom three were due to the recurrence (after 1, 3, and 5 years postoperatively), two for a haematoma (8 and 14 days postoperatively) and 1 due to arterial bleeding (reoperation on the same day of the hernia repair).
One patient had a surgical site infection, requiring antibiotic treatment. The mean comprehensive complication index was 20.33 (standard deviation [SD] 11.79), concerning a total of nine patients. Other reported complications were epididymitis (one patient), wound healing disorder (one patient), reduced perfusion of the testis (one patient), seroma (one patient), haematoma (three patients) and arterial bleeding (one patient). The comprehensive complication index is a measure of the burden of all complications, weighted for their severity [20].
The mean intensity of postoperative pain on the numeric pain rating scale (NRS) was 2.74 (SD 2.63) before hospital discharge and 1.12 (SD 1.06) on the 6-week follow-up examination. NRS evaluation ended with postoperative week 6.
When the data were stratified according to the training level of the operating surgeon, the incidence of neurological disturbance or neuralgia at the 6-week follow-up was 10.7% if the operation was performed by the chief of surgery, 40% if performed by a senior consultant, 49% if performed by chief residents and 47.3% when performed by residents (fig. 1). At the first follow-up consultation 6 weeks postoperatively, neurological disturbances or neuralgias were reported by 33.7% of 95 patients followed up, but not necessarily operated on, by a senior consultant and 52.2% of 46 patients followed up by an attending surgeon, (odds ratio [OR] 2.15, 95% confidence interval [CI] 1.05–4.4; p = 0.044).
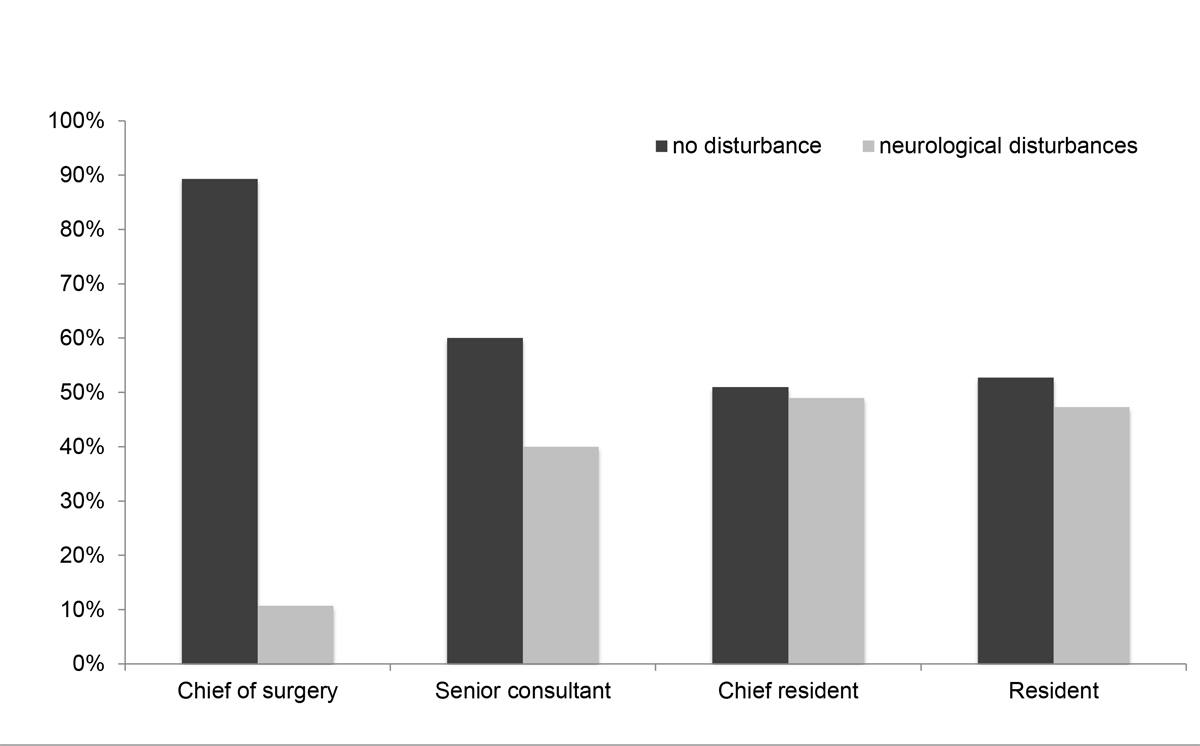
Figure 1 Incidence of neurological disturbances according to the training level of the operating surgeon at 6 week follow up.
The results of the t-test (table 2) showed that patients with neurological disturbances or neuralgia at the 6-week follow-up were younger (mean age difference 12.2 years), had a higher NRS score before hospital discharge (+1.3 points in the NRS) and have a longer period of inability to work (+ 6.7 days) compared with patients without neurological disturbances or neuralgia (p <0.001, p = 0.013, p = 0.033 respectively).
Table 2 Group characteristics between patients with and without neurological disturbances or neuralgia at 6 week follow up.
| No neurological disturbances or neuralgia | Neurological disturbances or neuralgia | p-value | |||
|---|---|---|---|---|---|
| n | mean (SD) | n | mean (SD) | ||
| Age | 86 | 62.47 (17.2) | 57 | 50.22 (14.84) | <0.001 |
| Operation duration (min) | 86 | 40.28 (21.95) | 56 | 44.04 (14.41) | 0.22 |
| Hospital stay (days) | 86 | 2.2 (1.4) | 55 | 1.87 (0.8) | 0.126 |
| NRS postoperatively | 67 | 2.37 (2.18) | 46 | 3.7 (2.18) | 0.013 |
| NRS at 6 week follow-up | 55 | 1.02 (0.68) | 40 | 1.25 (1.43) | 0.346 |
| Inability to work (days) | 67 | 11.66 (17.19) | 48 | 18.33 (15.63) | 0.033 |
SD: standard deviation, NRS: numeric rating scale, min: minutes, n: numbers.
The Pearson correlation showed that the younger the patients were, the higher was the NRS before hospital discharge postoperatively (Pearson correlation −0.320, p <0.001), and at 6-week follow-up (−0.303, p = 0.003; table 3). A higher NRS score postoperatively (Pearson correlation 0.248, p = 0.036), a longer time of inability to work (Pearson correlation 0.460, p = 0.000) and a greater need for pain medication (Pearson correlation 0.346, p = 0.001) correlated with a higher NRS score at 6-week follow up.
Table 3 Factors influencing pain before hospital discharge and at 6 week follow up.
| NRS before hospital discharge | NRS 6 week follow up | |
|---|---|---|
| Age | -0.320 (p<0.001) | -0.303 (p=0.003) |
| NRS before hospital discharge | 0.248 (p=0.036) | |
| NRS 6 week follow up | 0.248 (p=0.036) | |
| Inability to work | 0.319 (p=0.001) | 0.460 (p<0.001) |
| Need of pain-medication | 0.450 (p<0.001) | 0.346 (p=0.01) |
Comparing the effect of the NRS before hospital discharge and 6 week follow up on age, NRS before hospital discharge and 6 week follow up, inability to work and need of pain medication. NRS: numeric rating scale.
The study presented here evaluated the feasibility, safety and implementation of, as well as short- and long-term outcomes after open inguinal hernia repair with a newly introduced self-gripping lightweight macroporous mesh in a peripheral teaching hospital. The mesh was implemented at our clinic at a very early stage after clinical introduction of the self-gripping technology.
As a major incidental finding, this study identified significant differences in postoperative neurological disturbances or neuralgia according to the training level of the operating surgeon. Whereas the lowest incidence of neurological disturbances or neuralgia occurred in patients operated on by the chief of surgery or senior consultant surgeons, surgeons with less experience tended to have more patients suffering from neurological disturbances or neuralgia. These results are surprising as open inguinal hernia repair is considered to be a rather easy operation and is one of the first procedures young surgeons in training learn. Lederhuber showed that patients operated on relief of unsupervised trainees experienced more severe postoperative pain than patients operated on by specialists (OR 1.84, 95% CI 1.14–2.98; p = 0.001) [21].
However, the number of patients reporting postoperative pain in our study was comparable to results from previously reported studies comparing different mesh types in open inguinal hernia repair. Nienhuijs et al. compared three different techniques of open inguinal hernia repair (Lichtenstein procedure, mesh plug repair and Prolene Hernia System) and reported chronic postoperative pain in 43.3% of patients, irrespective of the technique used [22]. The multicentre study by Droeser et al. comparing Lichtenstein’s operation with a prolene mesh vs mesh plug repair also could not identify differences in postoperative chronic pain (OR 0.58, 95% CI 0.31–1.09; p = 0.088) [23]. Investigating the effect of self-gripping meshes on postoperative and on chronic pain, Sanders et al. showed a significantly lower surgical pain scale score within the first week after surgery in patients treated with a self-gripping mesh compared with those treated with a sutured mesh (+4.2 vs +9.7, p = 0.027) [24]. The study by Verhagen et al. showed significantly less postoperative pain on a visual analogue scale at 3-week follow-up with a self-gripping mesh than with a standard polypropylene mesh (p = 0.016) [13]. Interestingly, in both studies, the difference between the type of mesh used and reported pain was no longer evident at 1-year follow up. Molegraaf also found no difference in chronic postoperative inguinal pain in patients treated with self-gripping as compared with sutured mesh (7.3% vs 6.6%, p = 0.57) [25]. Furthermore, Pierides et al. did not detect any difference between self-gripping and sutured meshes in a visual analogue scale score for pain during the two first weeks postoperatively [15]. A meta-analysis by Ismail et al. including 12 randomised, controlled trials and 5 cohort studies showed a lower VAS pain score on postoperative day seven for self-gripping mesh as compared with sutured mesh fixation (mean difference −1.66, 95% CI −2.55 to −0.78; p <0.0001). The VAS pain score after one month therefore showed no difference (mean difference −0.88, 95% CI −1.79 to 0.04; p = 0.06) [26]. The review by Li et al. did not detect any difference in acute postoperative and chronic (>3 months) pain when comparing a self-gripping and a sutured mesh (OR 1.32, 95% CI 0.68–2.55; OR 0.74, 95% CI 0.51–1.08). In addition to the results of Li et al we furthermore evaluated the NRS according to the training level of the operating surgeon [6]. According to these results we assume that the implantation of a self-gripping mesh at our institution was not associated with altered post-operative pain in the patient cohort.
A main argument favouring the use of a self-gripping mesh is the reduction of the operation time. Rönka et al. observed a significant difference in mean operation duration favouring a self-gripping mesh over a sutured mesh (32 minutes [202 patients] vs 38 minutes [207 patients], p <0.001) [16]. Similar findings were reported by Pierides et al, with a mean operation duration of 36 minutes (198 patients) versus 45 minutes (196 patients), (p <0.001) [15] and by Molegraaf (mean duration 44.4 minutes [169 patients] versus 53.4 minutes [207 patients], p = 0.001) [24]. The operation duration in our study was slightly longer compared to Rönka et al. and Pierides et al. which was mainly because open hernia repair is used as a teaching operation at our institution [15, 16]. But the duration was shorter than that reported by Molegraaf, where there were also different training levels of the operating surgeon [25]. Most interestingly, we detected a trend towards less pain with shorter operations. However, the reported operation duration was not much longer then the reported times for conventional hernia repair, indicating that implementation of a self-gripping mesh is feasible even in a peripheral teaching hospital. Lederhuber showed the lowest incidence of reoperation due to recurrence in operation durations between 43 and 57 minutes [21].
We report recurrence rates of 3% after 5 years. These recurrence rates are comparable to the results of a meta-analysis of randomised controlled trials of mesh repair with a recurrence rate of 2% [27]. The systematic review from Ismail et al. did not demonstrate an advantage concerning recurrence rates for either self-gripping or for sutured mesh (OR 1.08, 95% CI 0.57–2.06; p = 0.8) [26]. In the meta-analysis from Li et al., results did not differ after a 12-month follow-up (OR 0.70, 95% CI 1.19–2.49) [6]. The multicentre study by Droeser et al. comparing Lichtenstein technique using a sutured mesh with mesh plug repair in teaching hospitals (including our institution), revealed recurrence rates of 7.8% and 8.1% respectively (adjusted OR 1.0, 95% CI 0.54–1.85; p = 1.0) at a median follow up of 6.5 years [23]. Zwaans showed a higher recurrence rate after 3 years (16 patients with recurrence in 139 patients with Parietex ProGrip™ mesh) than we did in the present study with a recurrence rate of 3.0% after 5 years, showing that no higher recurrence rates are to be expected with self-gripping lighweighted mesh [28]. The study from Molegraaf showed a similar recurrence rate of 2.4% after 2 years as compared with our results [23].
The aim of this study was to investigate the feasibility of introducing a self-gripping mesh in a peripheral teaching hospital. At the start of the procedure, there was some uncertainty as to whether a fixating medial stitch had to be placed in patients with a bigger hernia diameter, and this is why the first nine patients in our study received a medial fixating stitch when the procedure was introduced. It was demonstrated by Kingsnorth et al. that a single stitch, especially when placed too deep, leads to a higher risk for chronic groin pain due to subsequent periostitis [9]. Although we did not detect such an increase in neurological disturbances or neuralgia in sutured self-gripping mesh, we did not proceed with stich fixation as we learned from our own data that hernia recurrence rates are very rare with this type of mesh.
Our results showed a trend towards more pain in younger patients. This finding is consistent with the results from Nienhuijs et al. demonstrating chronic pain more frequently in patients under 50 years [22]. Although the reason for such a difference in age is not clear, it is conceivable that younger patients may speak more openly to their surgeon about postoperative complaints.
The analysis of our results show additional risk factors for a high NRS score at 6 weeks postoperatively, such as a high NRS score immediately after surgery, which leads to a longer period of inability to work and a higher need for pain medications. These findings highlight the importance of postoperative pain management for the reduction of neurological disturbances or neuralgia. Our results compare favourably with the findings from Callesen et al. on postoperative pain as a risk factor for chronic pain. These authors demonstrated a higher frequency of inguinal pain 1 year postoperatively in patients with severe pain at 1 week (9% vs 3% with a cumulated pain scale ≥11 and ≤10, respectively) and 4 weeks (24% vs 3% of patients with moderate or severe pain vs none or light pain) postoperatively (p <0.05, p <0.001, respectively) [29].
Smeds et al. suggested nerve identification as well as resection of nerves at risk (because traumatised owing to their topography or interference with the mesh), aiming for a better outcome as the authors had detected less postoperative pain in patients with resection of nerves at risk [30]. In our study we did not detect any significant difference between nerve resection and neurological disturbance or neuralgia. The difference from the results of Smeds might be due to a smaller number of nerve resections in our study-population.
We would like to acknowledge the limitations of our study. First, the study was not a randomised trial comparing two different techniques. However, the main objective of our study was to assess the feasibility, safety and implementation, as well as short- and long-term complications, of a self-gripping mesh in a peripheral teaching hospital and not to compare two different techniques. Second, although we report only a small number of patients who were lost to follow up, it is conceivable that some of the patients with recurrent inguinal hernia sought treatment at another institution, which could have decreased the number of recurrences in our cohort. As we did an exact follow up of the medical charts of each patient up to 5 years after surgery this is unlikely. As long term clinical follow-up was performed with a chart review, it is possible that not all recurrences were detected. With the retrospective study design, however, there is hardly a better way to detect hernia recurrence.
A further limitation is that we evaluated the NRS only at 6 weeks postoperatively and that no further physical examinations were planned. However, further consistent surveys were not planned in this study setting, and it can be assumed that patients who would have developed pain afterwards would have presented themselves again in the outpatient clinic. Also, a detailed analysis of differences in the baseline characteristics related to participants lost to follow up would add more value for further studies.
Also, patients, especially younger patients, are more likely to report disturbances with a younger or less experienced surgeon. One explanation for this finding could be a higher functional demand and activity level. Furthermore, the lack of significance for a correlation between side and type of hernia and neurological disturbance or neuralgia confirms the good quality of the study and the constant and high surgical performance regardless of the side and type of hernia. As some patients were followed up by the chief of surgery or operating consultant themselves, there is the hypothetical chance that neurological disturbances or neuralgia might be overlooked during follow-up examination. Additionally, as surgeons with different levels of experience were involved in the follow up, postoperative neurological disturbances and neuralgia might have been reported differently, according to the experience of the performing surgeon. However, in our study we wanted to assess the feasibility of introducing a new mesh in a peripheral teaching hospital, therefore also the follow up should be performed in the same manner as before the study.
In summary, this study demonstrates that introduction of a self-gripping and lightweight macroporous mesh in a peripheral teaching hospital is feasible at a very early stage right after market launch without a higher complication and recurrent hernia rate. The here presented results furthermore suggest performing open inguinal hernia repair in patients prone to pain and of younger age by a well-experienced surgeon which is surprising as the Lichtenstein technique is supposed to be an easily learned operation by young residents.
There is heterogeneous data in the literature about the outcome of less chronic pain with self-gripping mesh. The percentage of patients with neurological disturbances or neuralgia six weeks postoperatively, the operation duration and especially the recurrence rate are satisfying for a peripheral teaching hospital and we therefore use these products in favour of standard mesh in daily clinical practice. Thus, our study demonstrates that introduction of a self-gripping mesh in a peripheral teaching hospital is feasible.
No financial support and no potential conflict of interest relevant to this article was reported.
1 Paajanen H . A single-surgeon randomized trial comparing three composite meshes on chronic pain after Lichtenstein hernia repair in local anesthesia. Hernia. 2007;11(4):335–9. doi:.https://doi.org/10.1007/s10029-007-0236-1
2 Amid PK . Lichtenstein tension-free hernioplasty: its inception, evolution, and principles. Hernia. 2004;8(1):1–7. doi:.https://doi.org/10.1007/s10029-003-0160-y
3 Lichtenstein IL , Shulman AG . Ambulatory outpatient hernia surgery. Including a new concept, introducing tension-free repair. Int Surg. 1986;71(1):1–4.
4 HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22(1):1–165. doi:.https://doi.org/10.1007/s10029-017-1668-x
6 Li J , Ji Z , Li Y . The comparison of self-gripping mesh and sutured mesh in open inguinal hernia repair: the results of meta-analysis. Ann Surg. 2014;259(6):1080–5. doi:.https://doi.org/10.1097/SLA.0000000000000408
7 Nienhuijs S , Staal E , Strobbe L , Rosman C , Groenewoud H , Bleichrodt R . Chronic pain after mesh repair of inguinal hernia: a systematic review. Am J Surg. 2007;194(3):394–400. doi:.https://doi.org/10.1016/j.amjsurg.2007.02.012
8 Aasvang EK , Kehlet H . The effect of mesh removal and selective neurectomy on persistent postherniotomy pain. Ann Surg. 2009;249(2):327–34. doi:.https://doi.org/10.1097/SLA.0b013e31818eec49
9 Kingsnorth A , Gingell-Littlejohn M , Nienhuijs S , Schüle S , Appel P , Ziprin P , et al. Randomized controlled multicenter international clinical trial of self-gripping Parietex™ ProGrip™ polyester mesh versus lightweight polypropylene mesh in open inguinal hernia repair: interim results at 3 months. Hernia. 2012;16(3):287–94. doi:.https://doi.org/10.1007/s10029-012-0900-y
10 Fountain Y . The chronic pain policy coalition. Ann R Coll Surg Engl. 2006;88(8):279. doi:.https://doi.org/10.1308/147363506X144015
11 Eklund A , Montgomery A , Bergkvist L , Rudberg C ; Swedish Multicentre Trial of Inguinal Hernia Repair by Laparoscopy (SMIL) study group. Chronic pain 5 years after randomized comparison of laparoscopic and Lichtenstein inguinal hernia repair. Br J Surg. 2010;97(4):600–8. doi:.https://doi.org/10.1002/bjs.6904
12 Sadowski B , Rodriguez J , Symmonds R , Roberts J , Song J , Rajab MH , et al.; Scott and White Outcomes and Effectiveness Registry Group. Comparison of polypropylene versus polyester mesh in the Lichtenstein hernia repair with respect to chronic pain and discomfort. Hernia. 2011;15(6):643–54. doi:.https://doi.org/10.1007/s10029-011-0841-x
13 Verhagen T , Zwaans WAR , Loos MJA , Charbon JA , Scheltinga MR , Roumen RM . Randomized clinical trial comparing self-gripping mesh with a standard polypropylene mesh for open inguinal hernia repair. Br J Surg. 2016;103(7):812–8. doi:.https://doi.org/10.1002/bjs.10178
14 Chastan P . Tension-free open hernia repair using an innovative self-gripping semi-resorbable mesh. Hernia. 2009;13(2):137–42. doi:.https://doi.org/10.1007/s10029-008-0451-4
15 Pierides G , Scheinin T , Remes V , Hermunen K , Vironen J . Randomized comparison of self-fixating and sutured mesh in open inguinal hernia repair. Br J Surg. 2012;99(5):630–6. doi:.https://doi.org/10.1002/bjs.8705
16 Rönkä K , Vironen J , Kössi J , Hulmi T , Silvasti S , Hakala T , et al. Randomized Multicenter Trial Comparing Glue Fixation, Self-gripping Mesh, and Suture Fixation of Mesh in Lichtenstein Hernia Repair (FinnMesh Study). Ann Surg. 2015;262(5):714–20. doi:.https://doi.org/10.1097/SLA.0000000000001458
17 Kim-Fuchs C , Angst E , Vorburger S , Helbling C , Candinas D , Schlumpf R . Prospective randomized trial comparing sutured with sutureless mesh fixation for Lichtenstein hernia repair: long-term results. Hernia. 2012;16(1):21–7. doi:.https://doi.org/10.1007/s10029-011-0856-3
18 von Elm E , Altman DG , Egger M , Pocock SJ , Gøtzsche PC , Vandenbroucke JP ; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7. doi:.https://doi.org/10.1016/S0140-6736(07)61602-X
19 Chastan P . Tension free open inguinal hernia repair using an innovative self gripping semi-resorbable mesh. J Minim Access Surg. 2006;2(3):139–43. doi:.https://doi.org/10.4103/0972-9941.27726
20 Slankamenac K , Graf R , Barkun J , Puhan MA , Clavien PA . The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg. 2013;258(1):1–7. doi:.https://doi.org/10.1097/SLA.0b013e318296c732
21 Lederhuber H , Hanßke B , Dahlstrand U . Impact of trainee participation on inguinal hernia repair outcome – a study based on the Swedish Hernia Register. Ann Surg. 2019;Publish Ahead of Print. doi:.https://doi.org/10.1097/SLA.0000000000003497
22 Nienhuijs SW , Boelens OBA , Strobbe LJA . Pain after anterior mesh hernia repair. J Am Coll Surg. 2005;200(6):885–9. doi:.https://doi.org/10.1016/j.jamcollsurg.2005.02.005
23 Droeser RA , Dell-Kuster S , Kurmann A , Rosenthal R , Zuber M , Metzger J , et al. Long-term follow-up of a randomized controlled trial of Lichtenstein’s operation versus mesh plug repair for inguinal hernia. Ann Surg. 2014;259(5):966–72. doi:.https://doi.org/10.1097/SLA.0000000000000297
24 Sanders DL , Nienhuijs S , Ziprin P , Miserez M , Gingell-Littlejohn M , Smeds S . Randomized clinical trial comparing self-gripping mesh with suture fixation of lightweight polypropylene mesh in open inguinal hernia repair. Br J Surg. 2014;101(11):1373–82, discussion 1382. doi:.https://doi.org/10.1002/bjs.9598
25 Molegraaf MJ , Grotenhuis B , Torensma B , de Ridder V , Lange JF , Swank DJ . The HIPPO Trial, a randomized double-blind trial comparing self-gripping Parietex Progrip mesh and sutured Parietex mesh in Lichtenstein hernioplasty – A long-term follow-up Study. Ann Surg. 2017;266(6):939–45. doi:.https://doi.org/10.1097/SLA.0000000000002169
26 Ismail A , Abushouk AI , Elmaraezy A , Abdelkarim AH , Shehata M , Abozaid M , et al. Self-gripping versus sutured mesh fixation methods for open inguinal hernia repair: A systematic review of clinical trials and observational studies. Surgery. 2017;162(1):18–36. doi:.https://doi.org/10.1016/j.surg.2016.12.028
27 EU Hernia Trialists Collaboration. Repair of groin hernia with synthetic mesh: meta-analysis of randomized controlled trials. Ann Surg. 2002;235(3):322–32. doi:.https://doi.org/10.1097/00000658-200203000-00003
28 Zwaans WAR , Verhagen T , Wouters L , Loos MJA , Roumen RMH , Scheltinga MRM . Groin pain characteristics and recurrence rates – three-year results of a randomized controlled trial comparing self-gripping Progrip mesh and sutured polypropylene mesh for open inguinal hernia repair. Ann Surg. 2018;267(6):1028–33. doi:.https://doi.org/10.1097/SLA.0000000000002331
29 Callesen T , Bech K , Kehlet H . Prospective study of chronic pain after groin hernia repair. Br J Surg. 1999;86(12):1528–31. doi:.https://doi.org/10.1046/j.1365-2168.1999.01320.x
30 Smeds S , Löfström L , Eriksson O . Influence of nerve identification and the resection of nerves ‘at risk’ on postoperative pain in open inguinal hernia repair. Hernia. 2010;14(3):265–70. doi:.https://doi.org/10.1007/s10029-010-0632-9
No financial support and no potential conflict of interest relevant to this article was reported.