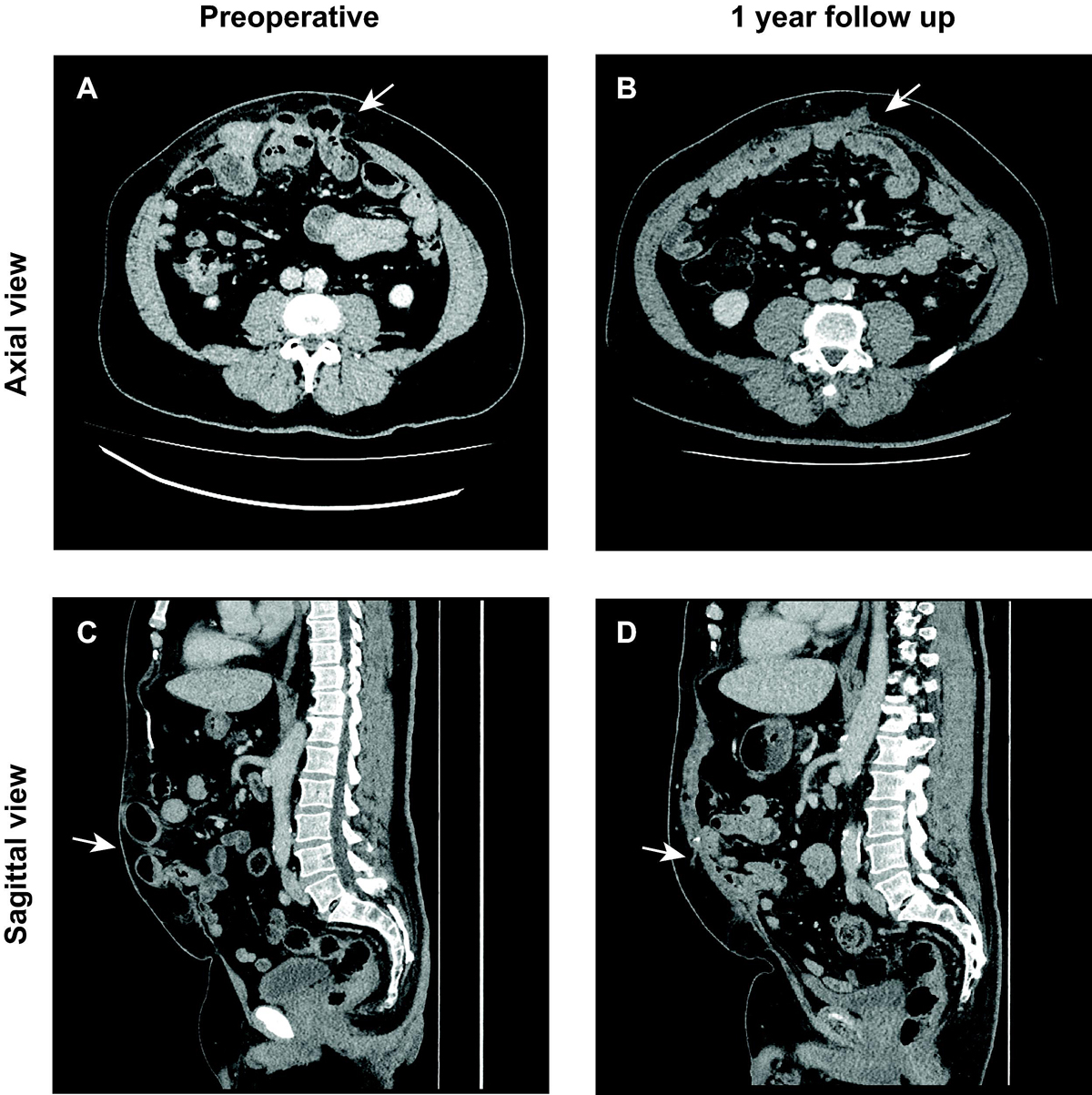
Figure 1 Abdominal computed tomography (CT) scan of the strangulated hernia in axial (a) and sagittal (c) views. Abdominal CT at 1-year follow up in axial (b) and the sagittal (d) views.
DOI: https://doi.org/10.4414/smw.2021.20423
Abdominal wall hernia is defined as an aponeurotic defect that lets an organ protrude from its original cavity [1]. Several types of abdominal wall hernias have been described and they constitute one of the most common surgical conditions.
Incisional hernias are caused by a defect in the abdominal wall following a laparotomy and their reported incidence is as high as 22.4% at 3 years after surgery, with some reports as high as 36% [2, 3]. Incarcerated hernia is a condition encountered by every general surgeon, with a rate of emergency operation of about 10–15% [4–6].
A strangulated hernia is a surgical emergency, with a higher rate of postoperative complications than elective surgery for non-incarcerated hernias, and a greater impact on mortality and morbidity [3]. Although laparotomy is the classical technique used for emergency hernia repair, laparoscopic approaches are being explored and have been described as safe and feasible techniques [7, 8].
Recently, a laparoscopic technique developed in 2017 by Dr Belyansky, called the enhanced-view totally extraperitoneal approach (eTEP), has been described for elective repair of ventral hernias, with the same indications as the classical Rives-Stoppa technique. This procedure can be complemented by the transversus abdominis release (TAR) procedure to reduce the tension of the posterior rectus sheath in order to close the defect [9, 10]. However the use of eTEP surgery with or without TAR in the case of a strangulated ventral hernia has not yet been described. It would be interesting to determine whether the eTEP surgery can be performed for an emergency hernia repair. Thus, we present the case of a patient with a strangulated incisional hernia operated with the eTEP technique.
A 57-year-old Caucasian male with a history of multiple abdominal surgeries was admitted in the emergency department with faecal vomiting and periumbilical pain for 3 days. His medical history included type 2 non-insulin dependent diabetes, hypercholesterolaemia, depressive anxiety disorder and a history of ischaemic heart disease in 2016. His medication included an oral antidiabetic, a beta-blocker and aspirin for cardiovascular prevention.
His surgical history included a Hartmann’s intervention via laparotomy for a perforated sigmoid colon, in 1996. In the same year, colon continuity was re-established and in 2010, he underwent surgery for an incisional hernia, without mesh implantation, which was performed by another surgical team. After this procedure for incisional hernia, he developed a recurrence of the hernia that was deemed too challenging to operate on because of multiple defects in the abdominal wall.
On clinical examination, the patient presented a strangulated incisional umbilical hernia with local cellulitis and tenderness in the left iliac fossa. Abdominal sounds were decreased.
His blood tests on presentation did not show a significant inflammatory syndrome, with a leucocyte count of 10 G/l and C-reactive protein level of 74 mg/l. Abdominal computed tomography showed a supra-umbilical incisional hernia with multiple defects of the abdominal wall associated with a strangulated hernia of the small intestine at the site of previous stoma, with signs of tissue damage (fig 1a,c). Following this finding, a nasogastric tube was inserted under smooth suction and the patient was admitted to the operating room for an emergency laparoscopic eTEP. This technique was indicated in this patient’s case because of the presence of multiple abdominal wall defects and in order to avoid the longer hospital stay and postoperative complications that might follow an open approach. The patient was placed in the French position under general anaesthesia. The strangulated hernia was reduced before incision after anaesthesia induction. Trocars were inserted into the left lower quadrant and an explorative laparoscopy was performed, which showed a total absence of intestinal ischaemia and widespread adhesions that required extensive adhesiolysis. After total adhesiolysis, the left preperitoneal retrorectus space was dissected, then crossover to the contralateral retrorectus space permitted the creation of operative space from the xiphoid to the pubis. Because tension on the posterior wall prevented closure, TAR was performed. There was a significant diastasis of the rectus abdominis, with a defect of 10 × 15 cm, as well as another 6 × 4 cm defect near the upper right quadrant. The posterior wall was closed and a 30 × 30 cm Versatex mesh was deployed without fixation. The operating time was around 6 hours.
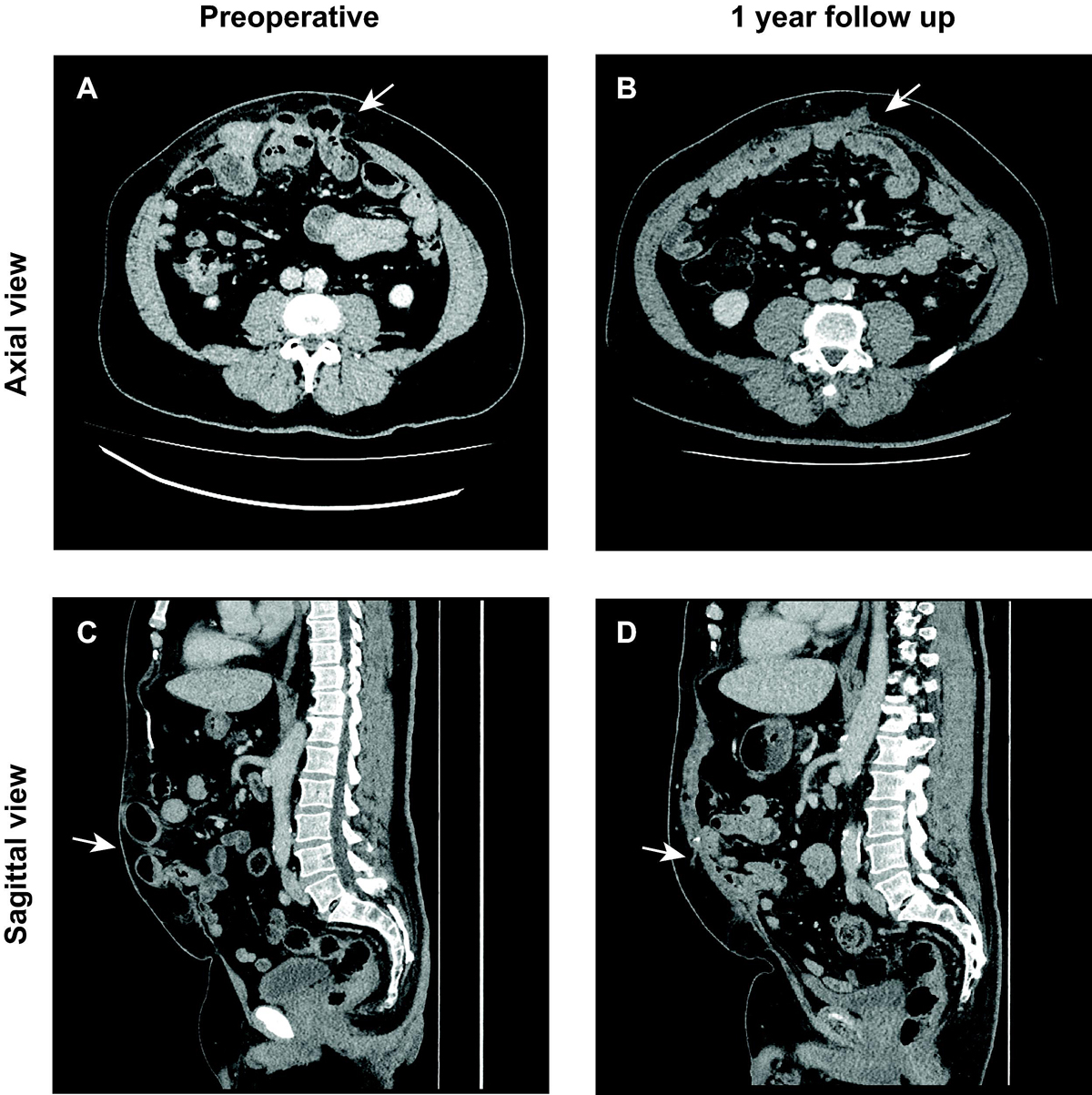
Figure 1 Abdominal computed tomography (CT) scan of the strangulated hernia in axial (a) and sagittal (c) views. Abdominal CT at 1-year follow up in axial (b) and the sagittal (d) views.
No drain was placed during the procedure and the patient remained hospitalised for 5 days, where the immediate postoperative period was uncomplicated. However, at the 30th post-operative day, there was a symptomatic seroma causing pain in the surgical site, which needed surgical evacuation, but was completely resolved at 1-year follow-up with no symptoms at all (fig.1b,d). Bacteriological culture of the seroma was negative.
Incarcerated ventral hernia is a pathology known by all general surgeons and characterised by the impossibility of reducing the hernia content during the physical examination, due to a narrow opening in the abdominal wall or to adhesions between the content and the hernia sac [4].
Approximately 10–25% of ventral hernia repairs are performed as an emergency, with worse outcomes than elective repair [5]. Helgestrand and al. showed that the risk factors for emergency repair were female gender, older age, umbilical hernia defects between 2 and 7 cm and incisional hernia defects up to 7 cm [5].
Most studies comparing laparoscopic approaches and open surgery were done in the context of reducible hernias that are dealt with in elective procedures. Few studies have compared the different techniques in the setting of incarcerated or strangulated hernias. For example, Deeba et al. compared the use of laparoscopic approaches with laparotomy in the treatment of incarcerated and strangulated inguinal hernias and showed that it was comparably safe and with similar outcome [8, 11–13].
In 2017, Belyanski et al. presented a new extraperitoneal laparoscopic technique to treat ventral abdominal hernias, the enhanced-view totally extraperitoneal approach (eTEP) [9]. This technique combines the advantages of physiological reconstruction of the abdominal wall, as in open surgery, with those of laparoscopy, by avoiding the implantation of a prosthesis in the abdominal cavity. The retromuscular space (rectus abdominis) is accessed using a dissection balloon. With preservation of the anterior wall, contralateral access is prepared to tackle all hernia orifices, using the same principle as open surgery. This laparoscopic approach allows a check of the integrity of the midline and reduction of all hernias, curing the muscular diastases. In the case of large defects, a complementary TAR can be performed. After closure of the posterior aponeurosis, it is possible to implant a retromuscular and preperitoneal prosthesis, as in the Rives-Stoppa technique [14].
We presented here the case of a patient with a strangulated incisional hernia that we surgically treated using the laparoscopic eTEP technique. Several studies of this new technique show increasing evidence of better clinical outcome, shorter length of hospital stay, and decreased morbidity and mortality in elective abdominal wall hernia repair, as compared with open approaches such as Rives Stoppa [9].
However, there is no report of feasibility of the eTEP surgery in the setting of a strangulated incisional hernia requiring emergency surgical treatment. By presenting this case, we show for the first time that the aforementioned technique is feasible in an emergency setting. It now remains to be shown that it can be a promising approach to reduce the high morbidity and mortality of strangulated hernias [7].
This procedure was chosen because of the multiple defects in the abdominal wall found before the operation, a condition that influenced a previous rejection of surgical treatment for the pre-existing incisional hernia. An extensive defect of the abdominal wall associated with the benefits of minimally invasive surgery are indications for the use of the eTEP technique for abdominal wall repair.
In the literature, the debate about the use of a laparoscopic approach in the emergency setting for ventral hernia repair is ongoing. In our case, the eTEP technique treated all the wall defects and avoided a second intervention, and the patient benefited in terms of outcome.
Our case aims to show as a proof of concept that in selected patients where there is no sign of bowel necrosis or infection, which would be a contraindication, the eTEP technique is a feasible and safe procedure. Multiple or extensive wall defects are amenable to this procedure
The main limitation of the use of the eTEP technique in the setting of strangulated incisional hernia would occur if the bowel is not viable and required resection. In our case, the strangulation did not require bowel resection and therefore was compatible with the eTEP procedure. This means that the choice of technique will depend on the clinical presentation of the hernia and the viability of the bowels. Another major limitation of the eTEP technique in an emergency setting is its dependence on skilled and trained surgeons who are familiar with the technique and who might not be available round the clock in the hospital. The complexity of the procedure is reflected by the long operating time in our case. Indeed, it took 6 hours for the whole procedure, which is explained by the adhesive status found intraoperatively.
The eTEP procedure is a new promising technique that has shown better outcome, fewer postoperative complications and shorter length of hospital stay in the context of elective surgery.
Incarcerated and strangulated ventral hernias are still classically treated by laparotomy. Studies that compare laparotomy and laparoscopy are scarce and there is no study describing the use of the eTEP technique in emergency hernia repair. We hypothesise that this new procedure could be a promising approach to incarcerated and strangulated hernias, with the potential to have fewer postoperative complications and shorter hospital stays. More studies need to be done to confirm the feasibility of this approach in the emergency setting.
No financial support and no potential conflict of interest relevant to this article was reported.
The patient provided written consent to publish. A copy of the consent is available.
1 Reza Zahiri H , Belyansky I , Park A . Abdominal Wall Hernia. Curr Probl Surg. 2018;55(8):286–317. doi:.https://doi.org/10.1067/j.cpsurg.2018.08.005
2 Fink C , Baumann P , Wente MN , Knebel P , Bruckner T , Ulrich A , et al. Incisional hernia rate 3 years after midline laparotomy. Br J Surg. 2014;101(2):51–4. doi:.https://doi.org/10.1002/bjs.9364
3 Yang GPC . Laparoscopy in emergency hernia repair. Ann Laparosc Endosc Surg. 2017;2(6). Available at: http://ales.amegroups.com/article/view/4017. Accessed 2020 April 23.
4 Birindelli A , Sartelli M , Di Saverio S , Coccolini F , Ansaloni L , van Ramshorst GH , et al. 2017 update of the WSES guidelines for emergency repair of complicated abdominal wall hernias. World J Emerg Surg. 2017;12:37. doi:. https://doi.org/10.1186/s13017-017-0149-y
5 Helgstrand F , Rosenberg J , Kehlet H , Bisgaard T . Outcomes after emergency versus elective ventral hernia repair: a prospective nationwide study. World J Surg. 2013;37(10):2273–9. doi:.https://doi.org/10.1007/s00268-013-2123-5
6 Beadles CA , Meagher AD , Charles AG . Trends in emergent hernia repair in the United States. JAMA Surg. 2015;150(3):194–200. doi:.https://doi.org/10.1001/jamasurg.2014.1242
7 Turner PL , Park AE . Laparoscopic repair of ventral incisional hernias: pros and cons. Surg Clin North Am. 2008;88(1):85–100, viii. doi:.https://doi.org/10.1016/j.suc.2007.11.003
8 Deeba S , Purkayastha S , Paraskevas P , Athanasiou T , Darzi A , Zacharakis E . Laparoscopic approach to incarcerated and strangulated inguinal hernias. JSLS. 2009;13(3):327–31.
9 Belyansky I , Daes J , Radu VG , Balasubramanian R , Reza Zahiri H , Weltz AS , et al. A novel approach using the enhanced-view totally extraperitoneal (eTEP) technique for laparoscopic retromuscular hernia repair. Surg Endosc. 2018;32(3):1525–32. doi:.https://doi.org/10.1007/s00464-017-5840-2
10 Belyansky I , Zahiri HR , Park A . Laparoscopic Transversus Abdominis Release, a Novel Minimally Invasive Approach to Complex Abdominal Wall Reconstruction. Surg Innov. 2016;23(2):134–41. doi:.https://doi.org/10.1177/1553350615618290
11 Pechman DM , Cao L , Fong C , Thodiyil P , Surick B . Laparoscopic versus open emergent ventral hernia repair: utilization and outcomes analysis using the ACSNSQIP database. Surg Endosc. 2018;32(12):4999–5005. doi:.https://doi.org/10.1007/s00464-018-6312-z
12 Azin A , Hirpara D , Jackson T , Okrainec A , Elnahas A , Chadi SA , et al. Emergency laparoscopic and open repair of incarcerated ventral hernias: a multi-institutional comparative analysis with coarsened exact matching. Surg Endosc. 2019;33(9):2812–20. doi:.https://doi.org/10.1007/s00464-018-6573-6
13 Reinke CE , Matthews BD . What’s New in the Management of Incarcerated Hernia. J Gastrointest Surg. 2020;24(1):221–30. doi:.https://doi.org/10.1007/s11605-019-04352-4
14 Stoppa RE . The treatment of complicated groin and incisional hernias. World J Surg. 1989;13(5):545–54. doi:.https://doi.org/10.1007/BF01658869
Joint first authors
SN and FB contributed equally to this work; SN, FB and GH drafted the manuscript; GH revised the manuscript for important intellectual content; all authors have read and approved the final version of the manuscript to be published.
No financial support and no potential conflict of interest relevant to this article was reported.