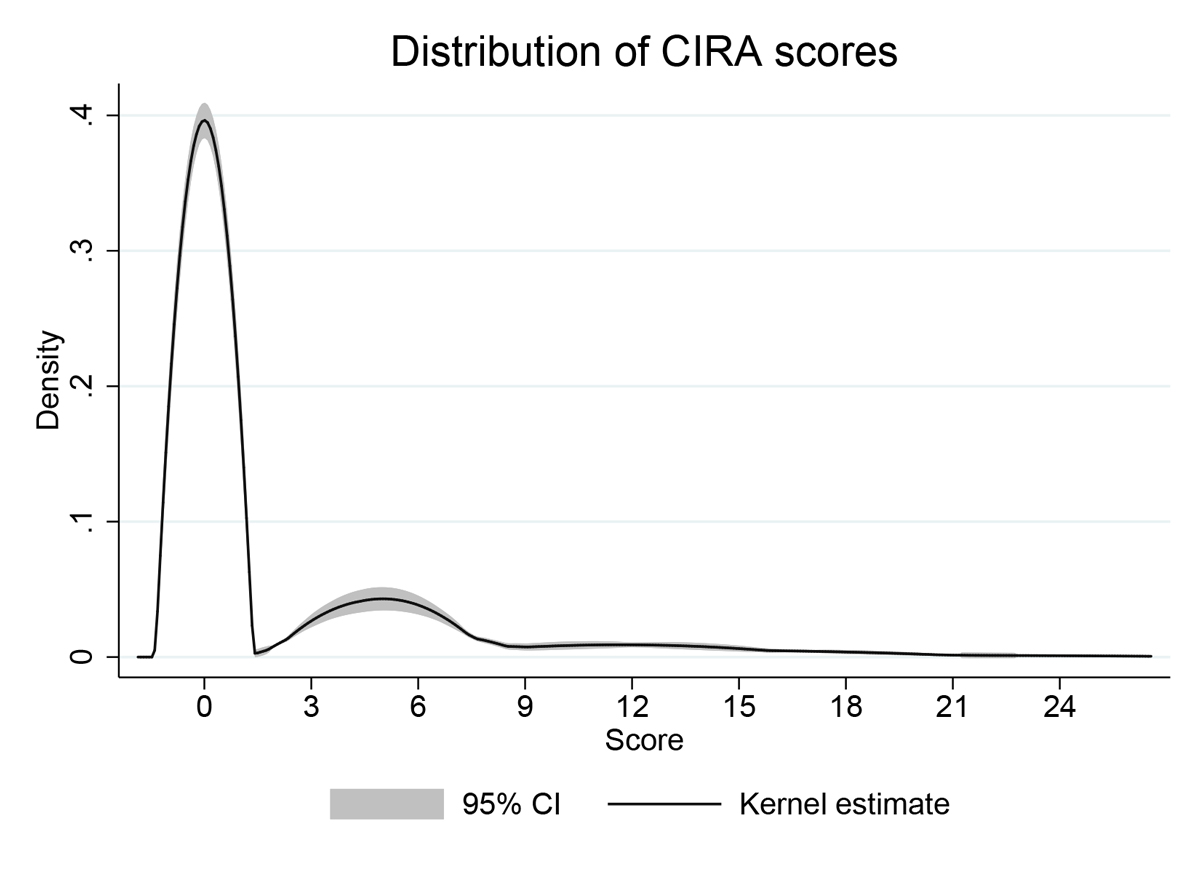
Figure 1 Distribution of CIRA scores in the development sample (n = 365). Kernel density with adaptive estimator.
DOI: https://doi.org/10.4414/smw.2021.20471
The current situation related to SARS-CoV-2 and its associated disease (COVID-19) poses critical challenges in prison settings [1]. Prisons are environments characterised by unsanitary conditions, insufficient provision of healthcare and promiscuity [2, 3]. All these factors can favour the spread of the disease [4]. Furthermore, detained persons tend to have a poorer health status than the general population [5–7]. Therefore, they may be more vulnerable to severe COVID-19 after infection. Protecting persons living in prison from infection is a state responsibility and, therefore, public health guidance for prison authorities and healthcare practitioners is crucial.
One way to protect detained persons is through the early identification of those at increased mortality risk from COVID-19 and measures to prevent initial infection. The World Health Organization (WHO) [8] and the Swiss Federal Office of Public Health (FOPH) [9] suggest that older age, cancer, cardiovascular disease, chronic respiratory diseases, immunodeficiency, diabetes and hypertension are risk factors for becoming severely ill after SARS-CoV-2 infection. The relevance of these risk factors has been supported in several meta-analyses [10–14] and early primary empirical studies from various countries including China [15], the United States [16], Italy [17] and Switzerland [18].
Although medical doctors make evaluations of COVID-19 mortality risk in certain custodial settings, there is no available tool to quantify prisoners’ vulnerability and classify them into risk categories. Such an instrument could support prison managers and staff in prioritising cases and courses of action (e.g., testing, separation) with an economical and valid assessment method. This is particularly relevant since the disease can spread quicker in custodial settings than in the general population [1, 2]. Furthermore, available resources are more limited in prison settings than in the community [3, 4], which can further jeopardise the health and living conditions of detained persons.
To address this gap and assist custodial staff taking early measures to protect detained persons, the present study collected data from the two largest prisons in Switzerland to (1) develop a screening tool ‒ named the COVID-19 Inmate Risk Appraisal (CIRA) ‒ to identify detained persons at increased mortality risk and to classify them in risk categories, and (2) test its validity when compared with national recommendations and clinical evaluation of COVID-19 vulnerability. We hypothesised that (1) the CIRA would be useful for separating detained persons into different groups regarding their vulnerability to COVID-19, and that (2) the CIRA would be a valid assessment of COVID-19 vulnerability.
This cross-sectional study included two purposive samples (there were 102 prisons in Switzerland by 2019), selected by different sampling procedures (see below). The first was used for the development of CIRA scores and risk categories. The second served to test the criterion validity of CIRA risk categories. There was no exclusion criterion in any of the samples. Data were collected by prison medical staff from prisoners’ medical files.
This study was considered as falling outside of the scope of the Swiss legislation regulating research on human subjects, so that the need for local ethics committee approval was waived (Req-2020-01037). Specifically, ethical approval was not required because data were fully anonymised, in accordance with Article 2, alinea 2, of the Federal Act on Research involving Human Beings (HRA), Switzerland [19]. There were no issues with confidentiality, anonymity and safety of the data collected.
The development sample included all persons detained in the Pöschwies prison (Zurich, Switzerland) on 23 March 2020. Pöschwies has 397 places for post-trial detention (occupation rate = 92%) and includes all kinds of prison regimes (e.g., common, open, maximum security). A total of 365 males were included (mean age 41 years, standard deviation [SD] 13, range 20–83).
The validation sample included 192 male persons detained in the Champ-Dollon prison (Geneva, Switzerland) on March 15, 2020 (mean age 37 years, SD 11, range 19–74). Champ-Dollon has 398 places for pre-trial and post-trial detention. At the time of data collection, 650 people were detained in Champ-Dollon (occupation rate 163%). The sample included all people clinically classified as vulnerable for COVID-19 (n = 45), identified after a first medical screening of the whole prison population, and a random selection of 147 of those classified as non-vulnerable (matching 1:3 for severe course of COVID-19, see section “Variables”).
The CIRA focuses on risk factors identified by the WHO [8] and the FOPH [9] as risk factors for severe COVID-19, based on laboratory cases in China. It includes seven factors: age ≥60 and six medical conditions – cardiovascular disease, diabetes, hypertension, chronic respiratory disease, immunodeficiency (the WHO and FOPH removed immunodeficiency from their lists of risk factors for severe COVID-19, when the present paper was already under revision; obesity was added to the list of risk factors during this period) and cancer. Although the FOPH suggests age ≥65 as a risk factor, because of the higher vulnerability of persons residing in prison [20], the threshold was conservatively reduced to 60 years to take into account the correctional context. Older age in prison is frequently considered even lower (from 50 years of age), since detained persons of all ages tend to have a worse health status than persons in the general population [21].
The CIRA combines these seven risk factors to derive an absolute risk increase in mortality rate. If a risk factor is absent, its score is 0. If a risk factor is present, a score ranging from 3.7 (for cancer) to 8.9 (for cardiovascular disease) is assigned. Scores correspond to the increased risk of COVID-19 death relative to the death rate among persons for whom the risk factor is absent. Death rates were extracted from the study of the Novel Coronavirus Pneumonia Emergency Response Epidemiology Team (NCPERET) [15], which includes information on 72,314 cases of COVID-19 in China and was the most complete data available at the time of collection. Since the study did not provide death rates among patients with immunodeficiency, the increased death risk for any comorbidity (i.e., combined; 4.1) was assigned for this risk factor. The sum of the risk factor scores is the CIRA score, which ranges from 0.0 to 36.9, with higher values representing higher mortality risk.
Seven risk factors were collected: age, cardiovascular disease, chronic respiratory diseases, immunodeficiency, diabetes, hypertension and cancer.
We derived a binary criterion of being vulnerable as defined by the FOPH [9], which considers detained persons vulnerable if they are aged ≥65 years and/or if they have any of the underlying medical conditions listed above.
A senior medical doctor (LG) derived a four-level classification of vulnerability according to the definition provided by the Division of Prison Health of the Geneva University Hospitals (DPHGUH; see table S1 in appendix 1). This classification was employed by the medical staff in Champ-Dollon to identify vulnerable persons and served to test the validity of CIRA, a mechanical alternative to this method. The criteria were developed according to (1) national recommendations from the FOPH [9], (2) literature reviews on risk factors for a severe course of COVID-19 [10–14], and (3) consensus of medical doctors from the DPHGUH on factors to consider.
The seven risk factors were used to describe the prevalence of the diseases and comorbidities in the development sample. Furthermore, they were combined to generate CIRA scores. Subsequently, the distribution of CIRA scores was used to establish the cut-points for CIRA risk categories.
In a second step, CIRA risk categories in the validation sample were used as an independent variable in the inferential analyses. Vulnerability according to national recommendations (FOPH) and clinical evaluation (DPHGUH) were considered as dependent variables to test the concurrent validity of CIRA.
Although the purpose of CIRA was to provide an absolute risk increase in mortality rate after infection from COVID-19, CIRA could not be validated using this outcome since at the time the instrument was developed no detained person had died because of this disease and very few had been infected.
To detect a sensitivity or specificity of 95% with significance level of 5% and precision of 3%, 103 participants were required [22]. This number was set as the minimum sample size in the validation sample. However, this threshold was exceeded (n = 192) owing to the sampling procedure (matching 1:3 subject for severe course of disease), in order to increase statistical power and confidence in the results.
In the development sample, we first computed the prevalence rate of risk factors with 95% confidence intervals (CIs). We also calculated correlations between risk factors (phi-coefficient) and their significance. Then, we applied the CIRA algorithm to derive CIRA scores. We summarised the distribution of scores based on kernel density estimation and percentiles, which served to derive CIRA risk categories. By last, the proportions of persons in each risk category with 95% CI was presented.
In the validation sample, we tested whether the CIRA was valid (criterion validity) by comparing its risk categories to (1) the national recommendations of the FOPH (see section on “Vulnerability according to national recommendations” above) and (2) the clinical evaluation of medical staff of the DPHGUH (see “Vulnerability according to clinical evaluation”). For the clinical evaluation, we first used “vulnerable” versus “non-vulnerable” detained persons (to test the discriminative ability of CIRA “elevated risk” category) and then the highest risk category ("extremely vulnerable") versus other risk categories (to test the discriminative ability of CIRA "high risk" category). We used area under the curve (AUC) and defined the best threshold categories based on the Youden J statistic that maximised sensitivity and specificity. Analyses were conducted in Stata 15.0.
In the development sample, regarding the prevalence rate of risk factors for COVID-19 mortality, 10.7% (95% CI 7.9–14.3%, n = 39) of the subjects were age 60 or older. The most prevalent medical condition was hypertension (11.8%, 95% CI 8.8–15.5%, n = 43), followed by cardiovascular disease (5.5%, 95% CI 3.6–8.4%, n = 20), diabetes and chronic respiratory disease (both 3.8%, 95% CI 2.3–6.4%, n = 14), and immunodeficiency (3.0%, 95% CI1.7–5.4%, n = 11). Cancer was less common (0.5%, 95% CI 0.1–2.2, n = 2). The correlations between risk factors are presented in table 1. Age ≥60 was significantly correlated with hypertension (r = 0 .29, p <0.001) and cardiovascular disease (r = 0.23, p <0.001). Cardiovascular disease was also significantly correlated with hypertension (r = 0.36, p <0.001) and diabetes (r = 0.20, p <0.001). In addition, hypertension was correlated with diabetes (r = 0.15, p = 0.005).
Table 1 Correlation between risk factors.
| Risk factor | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Age 60+ | – | |||||
| 2. Cardiovascular | 0.23 (<0.001) |
– | ||||
| 3. Diabetes | 0.02 (0.658) |
0.20 (<0.001) |
– | |||
| 4. Hypertension | 0.29 (<0.001) |
0.36 (<0.001) |
0.15 (0.005) |
– | ||
| 5. Respiratory | –0.02 (0.663) |
–0.05 (0.360) |
0.03 (0.513) |
–0.03 (0.584) |
– | |
| 6. Immunodeficiency | 0.04 (0.415) |
0.03 (0.594) |
–0.04 (0.503) |
0.04 (0.505) |
–0.04 (0.503) |
– |
| 7. Cancer | –0.03 (0.625) |
–0.02 (0.734) |
–0.01 (0.778) |
–0.03 (0.606) |
–0.01 (0.778) |
–0.01 (0.803) |
Pearson correlations (phi-coefficient), p-values in parentheses, N = 365.
Figure 1 presents the distribution of CIRA scores. The distribution was skewed to the right. Although the mean was 2.2 (95% CI 1.7–2.6), scores ranged from 0.0 to 24.7. Percentiles 66, 75 and 90 corresponded to the scores 0.0, 4.1 and 5.7, respectively.
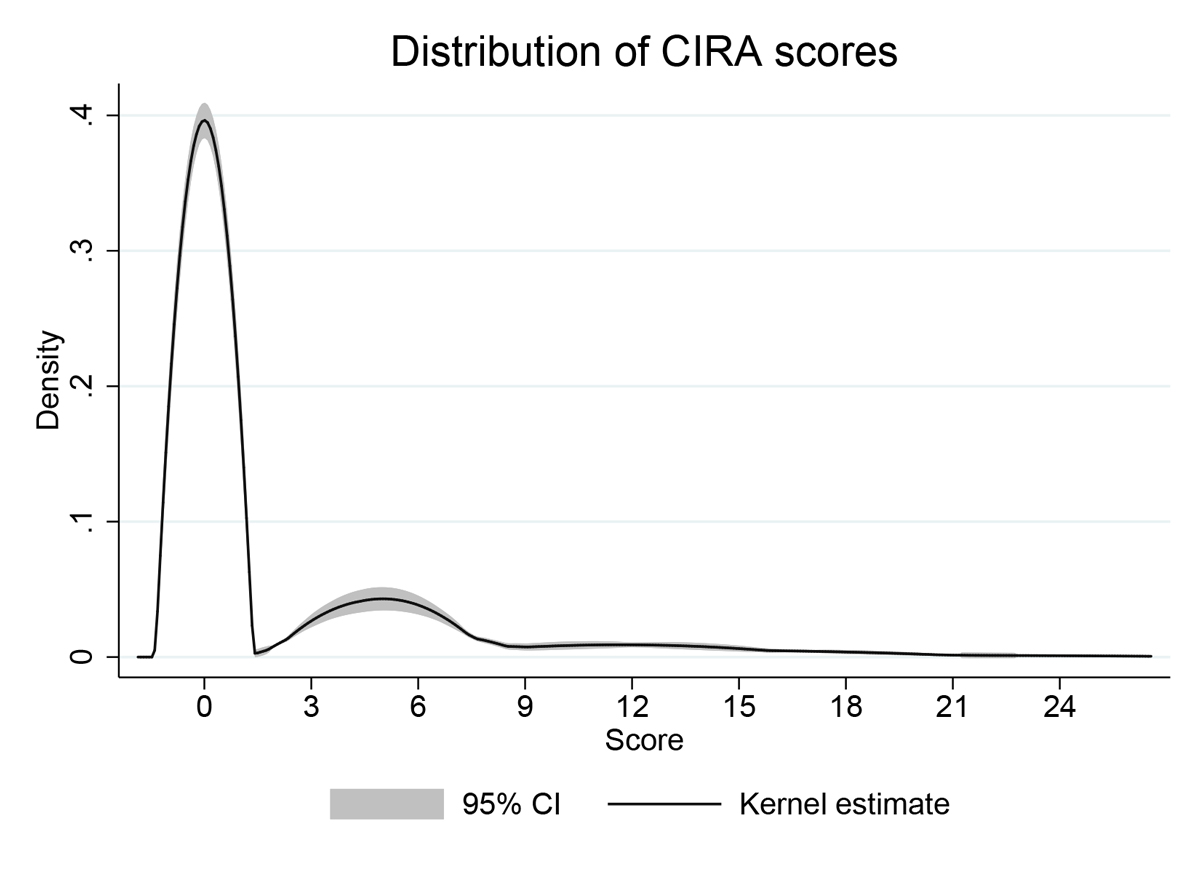
Figure 1 Distribution of CIRA scores in the development sample (n = 365). Kernel density with adaptive estimator.
Based on the distribution of CIRA scores and national recommendations (every person with one risk factor had to be considered at risk), we proposed a three-level classification of risk: average risk (<3.7), elevated risk (3.7–5.7) and high risk (>5.7; see table 2 for a complete description of CIRA risk factor scores and risk categories). Most detained persons had a score of 0.0 (72.6%, 95% CI 67.8–77.0%, n = 265) because they had no risk factor and were classified as “average risk”. Another group (17.5%, 95% CI 14.0–21.8%, n = 64) had scores between 3.7 and 8.8 and were classified as “elevated risk”. A smaller group (9.9%, 95% CI 7.2–13.4%, n = 36) had higher scores, spanning 8.9 to 24.7, and were classified as “high risk”.
Table 2 CIRA risk factors, scores, and risk categories.
| No. | Risk factor | Coding |
Score
(if risk factor is present) |
|
|---|---|---|---|---|
| 1 | Age | 0 = <60, 1 = 60+ | 5.4 | |
| 2 | Cardiovascular disease | 0 = absent, 1 = present | 8.9 | |
| 3 | Diabetes | 0 = absent, 1 = present | 5.7 | |
| 4 | Hypertension | 0 = absent, 1 = present | 4.7 | |
| 5 | Chronic respiratory disease | 0 = absent, 1 = present | 4.4 | |
| 6 | Immunodeficiency | 0 = absent, 1 = present | 4.1 | |
| 7 | Cancer | 0 = absent, 1 = present | 3.7 | |
| CIRA score (sum of scores): | ||||
| Risk category: | Average (<3.7) / Elevated (3.7–5.7) / High (>5.7) | |||
CIRA = COVID-19 Inmate Risk Appraisal Scores represent the increased mortality compared to the group without the risk factor.
In the validation sample, based on the national recommendations, 21.4% (n = 41) of the persons were considered vulnerable for COVID-19 mortality. CIRA risk categories had a high capacity in discriminating vulnerable individuals (AUC = 0.99; 95% CI 0.98–1]). The category “elevated risk” maximised sensitivity (100%) and specificity (97.4%, J = 0.97). CIRA classification identified all individuals considered vulnerable by the national recommendations plus 4 (2.1%), due to the lower age threshold used by the tool.
CIRA had even higher capacity in discriminating vulnerable individuals according to clinical evaluation (AUC = 1; 95% CI 1–1). The category “elevated risk” maximised sensitivity and specificity (both 100%, J = 1). CIRA identified the same individuals as being vulnerable for COVID-19 mortality as the medical staff (n = 45). For the individuals classified as extremely high risk by medical staff (n = 9), the category “high risk” had a high discriminatory capacity (AUC = 0.97; 95% CI 0.95–1, J = 0.86, sensitivity = 0.89, specificity = 0.97).
Responding to the challenges that SARS-CoV-2 poses for people in prison and the government’s responsibility in protecting them from being infected, we developed a screening tool (CIRA) to identify detained people at increased risk for COVID-19 mortality. This article presents the development of the CIRA and its validation. In accordance with our research hypotheses, the CIRA was useful in separating detained persons according to their vulnerability to COVID-19 and appeared to be a valid assessment method.
Based on CIRA scores in the development sample, 72.6% of detained people were classified as “average risk”, 17.5% as “elevated risk”, and 9.9% as “high risk”. All detained persons with one or more risk factors (27.4%) were classified as elevated risk. Cardiovascular disease is the only risk factors that directly classifies people as high risk. This is justified since, besides having been identified as the most severe risk factor for COVID-19 mortality [15], cardiovascular disease is the leading cause of death worldwide [23]. However, the high risk category represents mostly individuals with comorbidities. Although this category constitutes a small proportion of the sample (9.9%), it is relevant because comorbidity is generally associated with worse health outcomes, more complex clinical management and increased health care costs [24, 25], thus being useful to identify more vulnerable cases.
Criterion validity analyses indicated that CIRA risk categories have a high discriminative ability. The CIRA category “elevated risk” identified all individuals considered as vulnerable by the national recommendations of the FOPH [9] which suggests that persons with any of the seven risk factors (see the section “Variables” above) are at increased risk for severe course of COVID-19. Furthermore, this category identified the same individuals as being vulnerable as the clinical evaluations of the medical staff of the DPHGUH. The CIRA category “high risk” most correctly classified high risk persons. Overall, the results indicate that CIRA is a valid tool.
Although other COVID-19 risk assessment tools exist, most are focused on symptom detection, patient tracking, or planning mass gatherings and events [26]. Those focused on indicators of COVID-19 vulnerability (e.g., Objective Risk Stratification) [27] were not developed among prison populations and therefore their cut-scores are not adapted to detained persons. Arguably, mortality risk after COVID-19 infection is higher among detained persons than in the community due to their poorer health status in general.
In addition, the development of the CIRA gave an accurate overview of the prevalence rate of risk factors for COVID-19 mortality in the development sample, which was composed of the whole population of the Pöschwies prison. More than one in four detained persons had a risk factor for COVID-19 and the most prevalent underlying medical condition was hypertension (11.8%). Other recent studies on COVID-19 have shown that hypertension was the most prevalent comorbidity in prisoner samples, and that detained persons tend to have more severe outcomes after infection, including a higher rate of admission, longer length of stay and death in intensive care units [28, 29]. As such, hypertension may play a particular role in COVID-19 course of disease among detained persons.
Age ≥60 was also a prevalent risk factor (10.7%). Elderly persons are the fastest-growing segment of the incarcerated population and experience an early onset of aging-related health conditions when compared with the general population [30, 31]. Furthermore, the death rate among COVID-19 cases is known to grow exponentially as age increases [8, 15]. Therefore, older people may require particular attention from prison staff.
Because CIRA quantifies prisoners’ risk and classifies them in risk categories, based on the severity of risk factors and their comorbidity, the tool may assist prison managers prioritising cases and making intervention plans. Concretely, CIRA may serve to identify detained persons that should be tested (elevated-risk persons) or separated from the general prison population (high-risk persons). In conformity, high-risk detained persons could be subjected to more intense protective measures than persons with an elevated or moderated risk. For instance, for high-risk persons, measures such as allocation in a cell with other prisoners, walks with large groups and contact with symptomatic visitors should be avoided. Furthermore, using a screening tool can save time and resources to prison staff, reducing ambiguity in decision making at the same time (higher reliability) [32]. An algorithm to calculate scores and associated risk category is presented in table S2 (appendix 1).
The present study has several limitations. First, knowledge on risk factors for COVID-19 mortality is still limited and, therefore, important variables may not have been included in the guidelines of national and international organisations. Furthermore, after we had written the paper, the FOPH excluded immunodeficiency and included obesity in their list of risk factors for COVID-19 mortality. In addition, the CIRA scores assigned to risk factors relied on data from China. The WHO and the FOPH used the same data to provide recommendations regarding risk factors for severe COVID-19, and similar findings have been reported in other regions [16–18]. However, the applicability of the data to other countries is still uncertain. Therefore, the variables and scores used in CIRA should be considered preliminary and will need to be adjusted in the future [33].
Furthermore, although the correlations between risk factors in the present study were mostly weak, the mortality rates could be different when taking comorbidity between diseases into account. The mortality rates used in CIRA were extracted from a descriptive study [15], not a multivariable regression model, and therefore did not control for the covariance between variables. Another limitation is related to the fact that incarcerated persons are more likely to have unknown or poorly controlled chronic illnesses [5, 7]. The CIRA would classify these detained persons as having a low risk of severe COVID-19. Therefore, CIRA scores cannot be interpreted as mortality risk estimates, but rather as an indication of higher or lower vulnerability to COVID-19 among detained persons.
In addition, although vulnerability according to national recommendations and clinical evaluation were used for the validation of CIRA, these outcomes cannot be considered “gold standards” in terms of psychometric properties, because their validity and reliability are unknown. Finally, the empirical evidence for the cut-score of the high risk category is limited because of the small sample size (n = 9) in the highest clinical risk category. Nevertheless, a post-hoc power analysis revealed that, with the observed effect size (AUC = 0.97), the available sample provided a 100% power (one-tail) for the AUC analyses.
Underlying data will have to be updated regularly, since knowledge and policies regarding COVID-19 are changing rapidly in response to current developments and new findings. A website was created for this purpose (see www.prison-research.com) [34] and the algorithm to compute CIRA scores and associated risk categories will be updated according to new scientific evidence. In order to improve CIRA, further research on risk factors for COVID-19 and their relative risk, combining data from different countries and over a longer period is necessary. Besides, we believe that the CIRA can be used in custodial settings to help practitioners protecting detained persons from COVID-19.
Conceptualisation, methodology and validation: all authors; formal analysis: LCG and SB; investigation: AR and LG; data curation; LCG and LG; drafting – original draft preparation: LCG, SB, and MW; drafting – review and editing: LG, HW, JPS, AN, AR, AR, and JE; supervision: JE and HW; project administration: AR. All authors approved the final version of the manuscript.
All authors have completed the Unified Competing Interest form (available on request from the corresponding author) and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; and no other relationships or activities that could appear to have influenced the submitted work.
1 Yang H , Thompson JR . Fighting covid-19 outbreaks in prisons. BMJ. 2020;369:m1362. doi:.https://doi.org/10.1136/bmj.m1362
2 Kinner SA , Young JT , Snow K , Southalan L , Lopez-Acuña D , Ferreira-Borges C , et al. Prisons and custodial settings are part of a comprehensive response to COVID-19. Lancet Public Health. 2020;5(4):e188–9. doi:.https://doi.org/10.1016/S2468-2667(20)30058-X
3Penal Reform International. Coronavirus: Healthcare and human rights of people in prison - Penal Reform International. London, UK: Penal Reform International; 2020 Mar. Available from: https://www.penalreform.org/resource/coronavirus-healthcare-and-human-rights-of-people-in/ [accessed 2020 Apr 11]
4World Health Organization. Preparedness, prevention and control of COVID-19 in prisons and other places of detention. Interim guidance 15 March 2020. Copenhagen: WHO Regional Office for Europe; 2020 Mar. Available from: http://www.euro.who.int/__data/assets/pdf_file/0019/434026/Preparedness-prevention-and-control-of-COVID-19-in-prisons.pdf [accessed 2020 Apr 13]
5 Condon L , Gill H , Harris F . A review of prison health and its implications for primary care nursing in England and Wales: the research evidence. J Clin Nurs. 2007;16(7):1201–9. doi:.https://doi.org/10.1111/j.1365-2702.2007.01799.x
6 Watson R , Stimpson A , Hostick T . Prison health care: a review of the literature. Int J Nurs Stud. 2004;41(2):119–28. doi:.https://doi.org/10.1016/S0020-7489(03)00128-7
7 Wilper AP , Woolhandler S , Boyd JW , Lasser KE , McCormick D , Bor DH , et al. The health and health care of US prisoners: results of a nationwide survey. Am J Public Health. 2009;99(4):666–72. doi:.https://doi.org/10.2105/AJPH.2008.144279
8World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 2020 Feb. Available from: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf [accessed 2020 Apr 11]
9Federal Office of Public Health. People at especially high risk. 2020. Available from: https://www.bag.admin.ch/bag/en/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/besonders-gefaehrdete-menschen.html [accessed 2020 Apr 11]
10 Rodriguez-Morales AJ , Cardona-Ospina JA , Gutiérrez-Ocampo E , Villamizar-Peña R , Holguin-Rivera Y , Escalera-Antezana JP , et al.; Latin American Network of Coronavirus Disease 2019-COVID-19 Research (LANCOVID-19). Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. doi:.https://doi.org/10.1016/j.tmaid.2020.101623
11 Wang B , Li R , Lu Z , Huang Y . Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY). 2020;12(7):6049–57. doi:.https://doi.org/10.18632/aging.103000
12 Xu L , Mao Y , Chen G . Risk factors for severe corona virus disease 2019 (COVID-19) patients: A systematic review and meta analysis. medRxiv. 2020. doi:https://doi.org/10.1101/2020.03.30.20047415
13 Yang J , Zheng Y , Gou X , et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: A systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5.. doi:.https://doi.org/10.1016/j.ijid.2020.03.017
14 Zhao X , Zhang B , Li P , et al. Incidence, clinical characteristics and prognostic factor of patients with COVID-19: A systematic review and meta-analysis. medRxiv. 2020. Available from: https://www.medrxiv.org/content/10.1101/2020.03.17.20037572v1.full.pdf [accessed 2020 Apr 14]. doi:htps://doi.org/10.1101/2020.03.17.20037572
15 Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China] Article in Chinese. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(2):145–51. doi:.https://doi.org/10.3760/cma.j.issn.0254-6450.2020.02.003
16 Chow N , Fleming-Dutra K , Gierke R , Hall A , Hughes M , Pilishvili T , et al.; CDC COVID-19 Response Team. COVID-19 Response Team. Preliminary estimates of the prevalence of selected underlying health conditions among patients with Coronavirus disease 2019 — United States, February 12–March 28, 2020 MMWR Morb Mortal Wkly Rep. 2020;69(13):382–6. doi:.https://doi.org/10.15585/mmwr.mm6913e2
17COVID-19 Surveillance Group. Characteristics of COVID-19 patients dying in Italy. Rome, Italy: Istituto Superiore di Sanità; 2020 Mar. Available from: https://www.epicentro.iss.it/coronavirus/bollettino/Report-COVID-2019_20_marzo_eng.pdf [accessed 2020 Apr 14]
18Federal Office of Public Health. Maladie à coronavirus 2019 (COVID-19): Rapport sur la situation épidémiologique en Suisse et dans la Principauté de Liechtenstein. Berne, Switzerland: Federal Office of Public Health; 2020 Apr. French. Available from: https://www.bag.admin.ch/dam/bag/fr/dokumente/mt/k-und-i/aktuelle-ausbrueche-pandemien/2019-nCoV/covid-19-lagebericht.pdf.download.pdf/COVID-19_Situation_epidemiologique_en_Suisse.pdf&usg=AOvVaw096L-UcknWjmD7MoDXXDVg [accessed 2020 Apr 11]
19The Federal Council. Federal Act on Research involving Human Beings. Swiss Confederation 2020. Available from: https://www.admin.ch/opc/en/classified-compilation/20061313/index.html [accessed 2020 Nov 12]
20Centers for Disease Control and Prevention. Groups at higher risk for severe illness. Atlanta, GA: U.S. Department of Health & Human Services; 2020 Apr. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html [accessed 2020 Apr 11]
21Bretschneider W. Ageing prisoners and ethics behind bars: Law, human rights and health care - old (age) problems and new challenges [dissertation]. Basel, Switzerland: University of Basel; 2015. Available from: https://edoc.unibas.ch/38577/ [accessed 2020 Apr 13]. doi:https://doi.org/10.5451/unibas-006433969
22 Hajian-Tilaki K . Sample size estimation in diagnostic test studies of biomedical informatics. J Biomed Inform. 2014;48:193–204. doi:.https://doi.org/10.1016/j.jbi.2014.02.013
23World Health Organization. Cardiovascular diseases (CVDs). 2017. Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) [accessed 2020 Apr 14]
24 Guan WJ , Liang WH , Zhao Y , Liang HR , Chen ZS , Li YM , et al.; China Medical Treatment Expert Group for COVID-19. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547. doi:.https://doi.org/10.1183/13993003.00547-2020
25 Valderas JM , Starfield B , Sibbald B , Salisbury C , Roland M . Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009;7(4):357–63. doi:.https://doi.org/10.1370/afm.983
26 Chatterjee R , Bajwa S , Dwivedi D , Kanji R , Ahammed M , Shaw R . COVID-19 Risk Assessment Tool: Dual application of risk communication and risk governance. Progress in Disaster Science. 2020;7:100109. doi:.https://doi.org/10.1016/j.pdisas.2020.100109
27 English P , Friedman E , McKeown H , Rao M , Sethi S , Strain, WD . Risk Stratification tool for Healthcare workers during the CoViD-19 Pandemic; using published data on demographics, co-morbid disease and clinical domain in order to assign biological risk. MedRxiv. 2020. doi:https://doi.org/10.1101/2020.05.05.20091967
28 Ali K , Rao S , Berdine G , Test V , Nugent K . A retrospective analysis and comparison of prisoners and community-based patients with COVID-19 requiring intensive care during the first phase of the pandemic in West Texas. J Prim Care Community Health. 2020;11:2150132720954687. doi:.https://doi.org/10.1177/2150132720954687
29 Altibi A , et al. Comparative clinical outcomes and mortality in prisoner and non-prisoner populations hospitalized with COVID-19: A cohort from Michigan. MedRxiv. 2020. doi:https://doi.org/10.1101/2020.08.08.20170787
30Subjack J, Aguilar G, Titterington VB. Aging prison population: Factors to consider. In: Bruinsma G, Weisburd D (eds) Encyclopedia of Criminology and Criminal Justice. New York, NY: Springer; 2020. doi:https://doi.org/10.1007/978-1-4614-5690-2_522
31 Greene M , Ahalt C , Stijacic-Cenzer I , Metzger L , Williams B . Older adults in jail: high rates and early onset of geriatric conditions. Health Justice. 2018;6(1):3. doi:.https://doi.org/10.1186/s40352-018-0062-9
32 Wormith JS . Automated offender risk assessment. Criminol Public Policy. 2017;16(1):281–303. doi:.https://doi.org/10.1111/1745-9133.12277
33 Wynants L , Van Calster B , Collins GS , Riley RD , Heinze G , Schuit E , et al. Prediction models for diagnosis and prognosis of covid-19: systematic review and critical appraisal. BMJ. 2020;369:m1328. doi:.https://doi.org/10.1136/bmj.m1328
34Canton of Zurich. COVID-19 Inmate Risk Appraisal (CIRA). 2020. Available from: www.prison-research.com [accessed 2020 Apr 14]
Table S1 Criteria for COVID-19 Vulnerability and Risk Classification used by the Penitentiary Medicine Service of the Geneva University Hospitals (on 15 March 2020).
| Risk classification | Criteria | n |
|---|---|---|
| Extremely high | – Chronic pulmonary disease / pulmonary fibrosis – Age >60 and at least on vulnerability factor* – Human immunodeficiency virus with CD4 count <200 cell/mm3 |
9 |
| Very high | – Asthma – Diabetes – Heart disease – Stage 4 renal failure – Human immunodeficiency virus with CD4 count 200–500 cell/mm3 |
22 |
| High | – Age >60 without comorbidity – Human immunodeficiency virus with CD4 count >500 cell/mm3 |
6 |
| Moderate | – Hypertension | 8 |
Clinical risk classification applied in the validation sample (n = 192). * Cancer, immunodeficiency, chronic respiratory disease, diabetes, cardiovascular disease, and hypertension.
Table S2 Display of the algorithm to compute CIRA scores and risk categories.
| COVID-19 Inmate Risk Appraisal (CIRA) | ||
|---|---|---|
| Please select the appropriate category in “Coding”. | ||
| Risk factor | Coding | Score |
| Age | <60 | 0 |
| Cardiovascular disease | No | 0 |
| Diabetes | No | 0 |
| Hypertension | No | 0 |
| Chronic respiratory disease | No | 0 |
| Immunodeficiency | No | 0 |
| Cancer | No | 0 |
| CIRA score | 0 | |
| Risk | AVERAGE | |
Last update: 20 March 2020 Available from: www.prison-research.com [34]