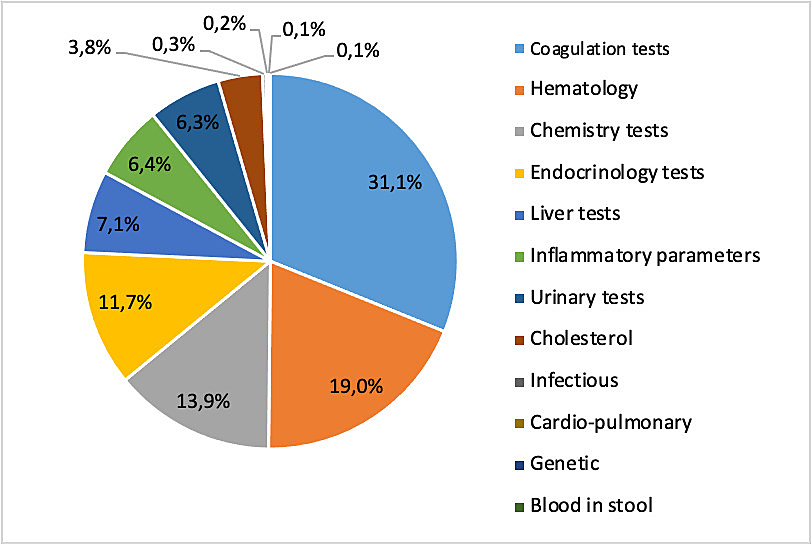
Figure 1 Type of laboratory tests billed during home visits, n = 72,159.
DOI: https://doi.org/10.4414/smw.2021.20396
We are observing a worldwide trend of aging of the population [1] and Switzerland is no exception. The proportion of older individuals is even expected to increase in the next decades [2], which will stretch existing resources in terms of nursing homes, homecare and health services. This is indeed a challenge for both social and health services, and most countries are in the process of designing new models of care to guarantee a good quality of care.
Home visits could be part of the measures that help maintain older people at home, thereby relieving pressure on nursing homes. Traditional home visits by family physicians used to be the main mode of home care delivery [3]. However, despite population aging, the number of physician home visits is declining worldwide [4]. In western Switzerland, the number of home visits by physicians has decreased by 40% in the last 10 years [5].
Increasingly, home visiting programmes are undertaken by nurses or multidisciplinary teams [6], which tend to replace the physician. Indeed, the private or public multidisciplinary teams receive a mandate for home visits with specific missions, including clinical check-ups, nursing care, drug treatments or meal delivery, prescribed by family physicians and sometimes by hospitals to reduce hospitalisation durations. And other organisations like palliative, geriatric or psychiatric mobile teams are also worth mentioning as healthcare professionals making home visits, generally in collaboration with the family physician as referent [7]. Furthermore, preventive home visits (visits pursuing various prevention and care activities, not solely devoted to addressing acute health issues) may help older people stay at home longer [8, 9] and maintain health-related quality-of-life [10], although their impact on preserving independence is still a matter of debate [11].
Several studies have evaluated trends and impact of home visits made by family physicians [12–14], but there are no studies describing the actual type of activities carried out during the visits [15]. A better understanding of home visit content may shed light on the specific contribution of family physicians in this action and may help in anticipating future needs and designing adapted services. The aim of this study therefore, was to describe the diversity of medical services provided by family physicians during home visits and analyse the evolution of these activities between 2006 and 2015.
This was a retrospective observational descriptive study, based on billing data. The source population was the general population of the canton of Vaud, the largest canton in French-speaking Switzerland, which accounted 767,497 individuals in 2015, with 16.4% of them older than 65 years of age [16].
The dataset used for this study consisted of all home visits billed by family physicians in the canton of Vaud between 2006 and 2015, collected by the cantonal trust centre. Billed visits could include different items according to the specific coding systems. In Switzerland, billing of medical services uses the Tarmed price-scale fixing system [17] and billing of laboratory items the analysis list annually approved by the Federal Office of Public Health [18]. Billing items can also be entered as free text (for example, a medication or medical material). Note that remuneration of Swiss family physicians is based on a fee and time-for-service system, for which the health insurance refunds patients for medical activities.
We manually separated all items received by the cantonal trust centre into five categories: medical services, laboratory, medications, medical material and vaccines. These categories were further refined into thematic subcategories. For example, we separated medical service items into consultation time, travel time, emergency supplements, physical examination, medical procedures, reports, and additional investigations. Then we further divided certain of these subcategories into subgroups; for example, physical examination could be billed as limited, complete, neurological, rheumatologic/orthopaedic, dermatological, gynaecological or mental health examinations [17]. Limited physical examinations included at least one of the following: weight/height measurement, heart rate and blood pressure measurement, skin/mouth/teeth/pharynx/throat examination, thoracic organ examination or abdominal examination. Complete examination included at least a limited examination plus a complete neurological examination or four of the following: eye inspection, visual acuity and field examination (colour vision and stereoscopy if appropriate), hearing examination, anterior rhinoscopy, otoscopy, partial neurological examination, joint examination, blood vessel examination, lymphatic nodes and thyroid examination, external genital examination or rectal/prostatic examination.
For items not retrieved in Tarmed or in the analysis list for laboratory analyses, we searched additional glossaries [19, 20]. We grouped free text items such as medications manually and by categories (for example nonsteroidal anti-inflammatory drugs). We could not categorise some items because we did not find a matching code in any of the glossaries used; we chose not to consider items that were billed less than 10 times during the study period.
We compared billing patterns between emergency and routine visits, with emergency visits including both urgent and pressing visits. In Tarmed, pressing visits are defined as visits that need to be made within 2 hours, during or outside of working hours, whereas urgent visits are visits that are made immediately [17]. We divided urgent visits into three types. Visits during working hours (Monday to Friday 7:00 to 19:00 and Saturday 7:00 to 12:00); visits outside of working hours during the evening or week-end (from Monday to Sunday 19:00 to 22:00, Saturday 12:00 to 19:00 and Sunday 7:00 to 19:00 and visits during the night (from Monday to Sunday from 22:00 to 7:00).
We conducted data analyses using the free software R, “RandomLCA” (Beath et al.) packages, and the Stata software (version 15.1, College Station, USA). We described the number of items billed per visit and the proportion of visits where specific item categories and subcategories appeared. We compared category frequencies between emergency and routine visits using the Pearson chi-square test.
To reduce the computational burden given the very large sample size and number of variables, we retained only the medical items having a prevalence of at least one per thousand (thereby reducing the number of indicator variables to 48), and then selected a random sub-sample of size of 10%. To ensure we did not lose too much information regarding the variables in the procedure, we verified that the prevalence computed in the sub-sample was similar to that we obtained during all the observations (see table S1 in appendix 1).
We used a clustering method that relied on discrete mixture models [21–24] and aimed to cluster visits solely based on the profile of medical service use.
For the case of continuous variables, various quality indexes of clustering exist (c_index, dunn, gamma, tau, silhouette, AIC, BIC, etc.) [25–27], but to the best of our knowledge for the binary variable setting, no such indexes exist. Therefore, to determine to what extent the indexes used to assess the quality of clustering for continuous variables might be useful for binary variables, we carried out a simulation study. For this purpose, we generated data arising from a mixture of three multivariate binary vectors of dimension 50 with mixture proportions of 1/3, 1/2 and 1/6. Simulation results showed that with binary data, none of the indexes (commonly) used for continuous variables perform well in identifying the correct number of clusters. Therefore, to select the number of clusters we relied mainly on visual inspection of the outcome probability plot and on the scatter plot of the data points (labelled and coloured according to their cluster membership) in the principal components space.
To end up with interpretable results and because of the absence of an appropriate index, we limited the search to a setting between two and six clusters (or classes).
After convergence of the clustering algorithm, we plotted the estimated outcome probabilities of each cluster as different symbols and colours on the same graph (probability plot) to visualise the profiles. We computed the posterior probabilities of belonging to the classes for each visit and retained the class with the highest probability. To help interpret the clusters found, we computed the mean of the following variables, age, gender, cost, duration, number of medical services, and of the indicator variable for an emergency intervention in each cluster.
We investigated the evolution over time of the cluster classes of home visits and presented the results in a graph.
From 2006 to 2015, 631 family physicians billed 451,634 (100%) home visits, which represented 2.5% of all consultations and a mean annual proportion of beneficiaries of 2.1% among the total resident population. The mean age of home visit beneficiaries was 67.1 years (standard deviation [SD] 23.3) with 72.3% of them older than 65 years and 34.3% older than 85 years. During these home visits, physicians billed 3880 different items, with a median of 5 items billed per visit (range from 2 to 95). Five hundred and seven items were not found in any of the glossaries and 2106 items were not considered as each appeared in fewer than 10 visits. In total, the non-retrieved items corresponded to less than 2% of all items (42,381/2,521,611).
Out of all the home visits, 157,921 (35%) were considered emergency visits, with 54.7% pressing visits (86,435) and 45.3% urgent visits (58,387). For the emergency visits, 69,419 (43.9%) were pressing visits during working hours and 17,016 (10.8%) outside working hours, whereas 31,440 (19.9%) urgent visits were during working hours, 26,947 (17.1%) outside working hours and 14,450 (9.1%) during the night.
For items from the Tarmed catalogue (table 1), consultation time was always billed (100.0%), travelling expenses were billed in 417,733 visits (92.5%), physical examinations in 66,229 visits (14.7%), medico-surgical procedures in 25,522 visits (5.7%), reports in 4547 visits (1.0%) and additional investigations in 2084 visits (0.5%).
Table 1 Proportion of items billed during home visits and by emergency or non-emergency.
|
Total
(n = 451,634) |
Emergency
(n = 157,921) |
Non-emergency
(n = 293,713) |
p-value | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Physical examination | 66 229 | 14.7 | 27 786 | 17.6 | 38 443 | 13.1 | <0.001 |
| Laboratory | 43 197 | 9.6 | 6 319 | 7.0 | 36 878 | 10.2 | <0.001 |
| Medico-surgical procedures | 25 522 | 5.7 | 8 454 | 5.4 | 17 068 | 5.8 | <0.001 |
| Reports | 4 547 | 1.0 | 2 125 | 1.4 | 2 422 | 0.8 | <0.001 |
| Medications | 3 093 | 0.7 | 1 499 | 1.7 | 1 594 | 0.4 | <0.001 |
| Vaccines | 2 678 | 0.6 | 83 | 0.1 | 2 595 | 0.7 | <0.001 |
| Additional investigations | 2 084 | 0.5 | 1 177 | 0.8 | 907 | 0.3 | <0.001 |
| Material use | 744 | 0.2 | 265 | 0.3 | 479 | 0.1 | <0.001 |
Home visits also included rare items (<1% of visits) such as forensic examination (401), manual medicine (254), psychiatric evaluation (253) and rheumatological (109), infectious (98) and complementary medicine-related (88) appointments.
Physical examination included limited (60,050, 13.3%) and complete examinations (5655, 1.3%) and neurological (454, 0.1%), rheumatological/orthopaedic (351), dermatological (277), gynaecological (141) and mental health (128) examinations. Medico-surgical procedures consisted mainly of venous and capillary punctures (16,829, 3.7%), injections and infusions (5514, 1.2%), wound care (1265, 0.3%), articular punctures (1174, 0.3%) and urinary catheterisations (493, 0.1%). Additional investigations performed were ECG (792, 1.7%), monitoring (270), Holter/Doppler/Remler (54) and spirometry (22).
There were 72,159 laboratory tests billed in 43,197 visits (9.6%) (fig. 1). The most frequent laboratory tests performed in home visits were coagulation tests, blood counts and chemistry tests.
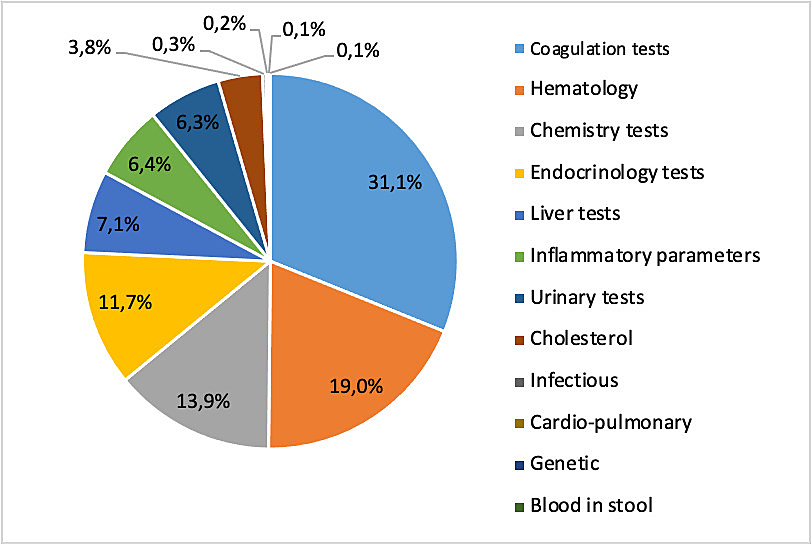
Figure 1 Type of laboratory tests billed during home visits, n = 72,159.
Physicians prescribed 4020 drugs during 3093 visits (0.7%) (fig. 2). Nonsteroidal anti-inflammatory drugs, corticoids and opiates were the most frequently billed drugs.
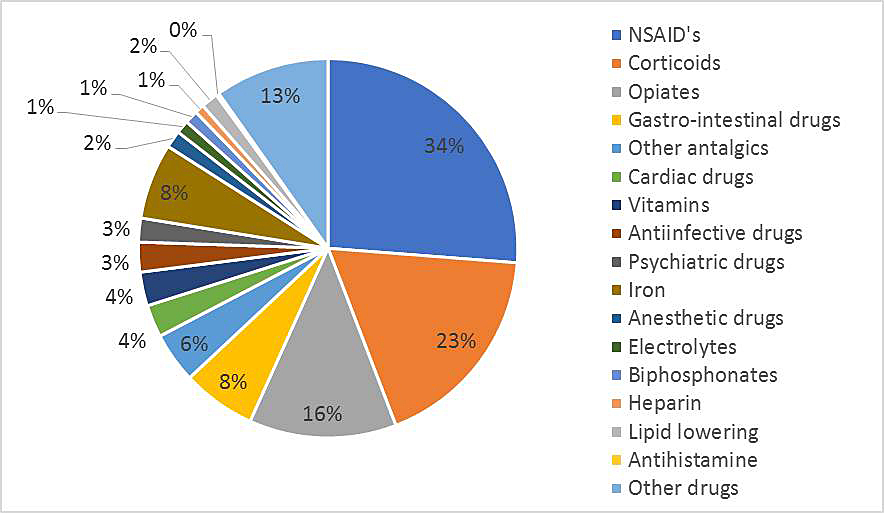
Figure 2 Medications prescribed during home visits, n = 4020.
Various materials were used in 1027 visits (0.2%), consisting of infusion sets (229 visits), wound dressings (198), other sets (141), suture packages (111), urological material (121), protection (95) and orthopaedic material (45).
Vaccines were administered in 2678 visits (0.6%), mostly influenza vaccines (2465 visits, 0.5%).
Comparison of emergency and routine visits showed that the proportions of visits that included physical examination (17.6 vs 13.1%, p <0.001), prescribed medication (1.7 vs 0.4%, p <0.001) and material use (0.3 vs 0.1%, p <0.001) were higher in emergency visits, whereas there were more laboratory tests (7.0 vs 10.2%) and vaccinations (0.1 vs 0.7%, p <0.001) performed during routine visits.
Figure 3 shows the correlation between billed items, which helped to identify clusters of home visits. This figure illustrates that, for the most part, medical services selected for the cluster analysis were not associated. Grouping the visits into four cluster classes appeared to be the best combination.
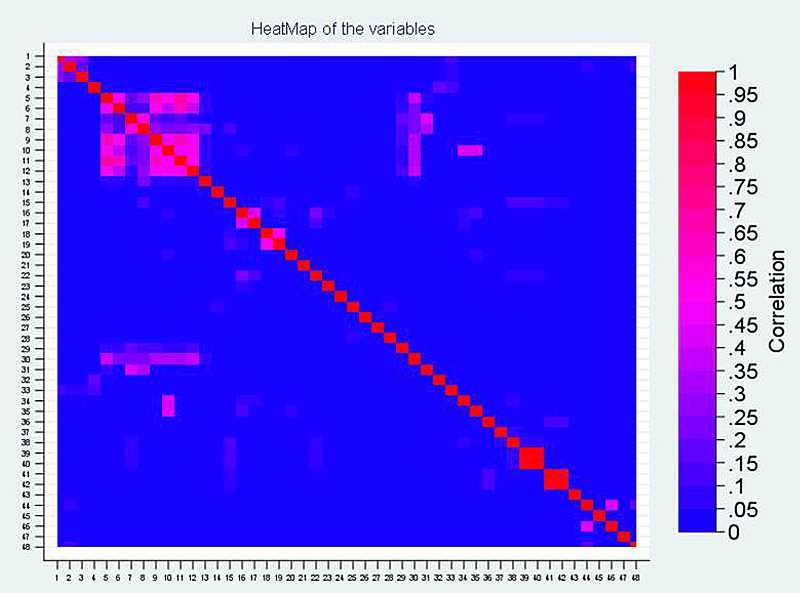
Figure 3 Correlation between items.
Figure 4 shows the probability of having an item when belonging to a specific cluster class. Cluster class 1 (red ‘x’ letters) represented standard home visits, consisting mainly of consultation time. It also included travel expenses, physical examination, instructions to patients and emergencies during working hours. Cluster class 1 was the most frequent type of visit (table 2), representing 83.5% of all visits. It concerned mainly older patients (mean age 79.8 years), with a majority of women (69.5%). Cluster class 2 (blue dots) represented standard home visits as in cluster class 1, but included also additional laboratory tests or forensic examination. It also concerned mainly older adults, and more often women. This cluster class showed the highest mean number of home visits per patient, with 7.8 visits/patient. The mean billed amount was also slightly higher compared with cluster class 1. The remaining cluster classes represented emergency visits, either during the day (during and outside working hours) for cluster class 3 (pink triangles) or at night for cluster class 4 (green crosses). Emergency visits were rare (6.0 and 3.3%, respectively, of day and night visits). Emergency visits also occasionally included blood drawing, medico-legal examination, physical examination and psychotherapeutic consultation. Cluster class 4 (emergency visits at night) had the youngest patients (mean age 53.7 years) and was most balanced with respect to gender (52.2% men). It represented also the most expensive billing.

Figure 4 Specific billing items corresponding to the four cluster classes of home visits.
Table 2 Cluster class characteristics.
| Cluster class | Type of home visit | % | % Emer-gency | Mean age | Mean n of visits / patient | % men |
Mean billed sum
(CHF) |
Mean duration (min) | Mean n of items |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Routine | 83.5 | 12.4 | 79.8 | 6.8 | 30.5 | 148.5 | 22.5 | 3.6 |
| 2 | Routine with lab. tests | 7.2 | 8.6 | 82.8 | 7.8 | 32.9 | 180.1 | 23.5 | 6.7 |
| 3 | Emergency visits (day) | 6 | 100 | 67.5 | 2.3 | 39.0 | 299.4 | 25.7 | 5.6 |
| 4 | Emergency visits (night) | 3.3 | 100 | 53.7 | 1.8 | 52.2 | 390.3 | 24.7 | 5.6 |
As shown in figure 5, we saw a decrease in the proportion of cluster classes 1, 3 and 4 over the observation period whereas cluster class 2 (routine visits with laboratory tests), appeared stable.
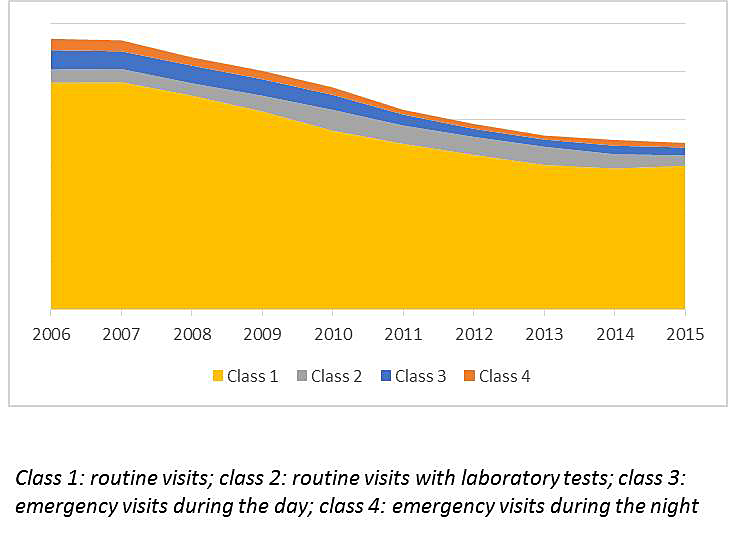
Figure 5 Evolution over time of the different home visit cluster classes.
Home visits may help older people to stay at home longer, but we observed a decrease in the number of home visits made by family physicians between 2006 and 2015 [5]. We aimed to describe the content and typology of home visits over this time.
We found that routine home visits to older people, consisting mainly of consultation time, were the most frequent type of family physician home visit in the canton of Vaud, followed by routine home visits with laboratory tests, which were considerably less frequent but concerned very old people with the highest rate of visits per person. In contrast to routine home visits, emergency home visits, regarding younger adults, were infrequent. We can thus consider that the main purpose of home visits in the canton of Vaud is to maintain older people at home, probably with preventive visits [15].
We observed that the global number of home visits tended to decrease over the observation time, with routine and emergency visits both affected by this trend. However, the proportion of routine home visits with laboratory tests remained stable during the observation period. A part of the decrease in family physician home visits is from the rise in new healthcare organisations engaged in home visits in collaboration with the family physician. Indeed, in the last decade we have seen an increased number of hours billed for homecare from these systems [28] and their intervention may have an impact on the reduced frequency of family physician home visits. Another aspect is the increased number of emergency department (ED) consultations observed in Swiss hospitals over the same time period [29, 30], with both younger adults and older people concerned in this trend. But the cause and effect relationship with the decrease in home visits by family physicians is difficult to determine. Indeed, we may argue that the patients’ choice to directly visit the ED, leading to the increased ED consultations, is a cause of the decrease in family physicians’ home visits. However, it has been shown that access to primary care can be limited by different factors such as below-average income, immigrant status and chronic conditions [31]. Unfortunately, there are few detailed data on access to primary care in Switzerland, but a limited access to family physicians is one of the hypotheses that could explain an increased number of ED consultation.
Strengths of our study include bringing information on real-life practice on a large dataset. Indeed, the studied population contains patients evaluated by family physicians of the canton of Vaud. Moreover, we analysed an almost 10-year observation period having a high number of visits.
Due to the retrospective nature of the study, we did not collect data specifically for the purpose of the study, which has some limitations. First, in terms of billing, home visits also included visits to people who lived in nursing homes, as this was their permanent home. Thus, we cannot discriminate this population from population living in private homes. However, as discussed in a previous analysis [5] of the same study population, this phenomenon should be minor, as the mean age of home visit beneficiaries was much lower than the mean age of people in nursing homes. In addition, it is impossible to evaluate whether all family physicians billed their activities in the same way and whether billing data completely represent the real activity. These points may be illustrated by travel expenses billing, which appeared in 92.5% of home visit billings. However, theoretically, physicians should bill expenses for all home visits (100%), as the doctor goes to the patient’s home. We could explain this discrepancy by the fact that when family physicians make home visits for couples or multiple patients in nursing homes, they bill travel expenses for only one, generally the patient for whom a home visit is the most necessary.
There are some other limitations due to the billing data nature of the study. For example, billing data do not give precise information about a consultation’s reason or diagnosis. Similarly, physical examinations were billed in only 15% of home visits, but this percentage does not represent the reality. Indeed, many family physicians bill the physical examination as consultation time in their practice owing to Tarmed’s billing constraints.
Further, the impossibility to decode almost 638 items not found in any glossary is also a limitation. Finally, the manual process of recoding may have led to some coding errors, especially when free text items were recoded. For example, physicians often abbreviated medication names perhaps leading to some misinterpretation.
As previously said, there is no known study focusing on the description of home visits made by family physicians; therefore, the study brings valuable information. Indeed, insofar as most home visits consist only of consultation time without additional investigation, with a mean time of about 20 minutes, it is relevant to ask whether more family physician home visits could be delegated to other healthcare professionals. For example, routine home visits with no or minimal physical examination of patients in a relatively stable situation could be delegated to nurses or other healthcare professionals [32]. Such visits could also integrate preventive measures, especially for older individuals [8]. However, for vulnerable patients, or patients in unstable and/or palliative situations for which a rapid decision or adaptation of care has to be made, family physician home visits should be maintained. We can add that family physicians will continue to have a role to play in emergency home visits, which could contribute to reduce the number of hospital emergency visits.
This study suggests that recommendations for practice [33, 34] specifically for home visits, including the use of existing or new resources, may be a valuable aid to better define situations most suited to home visits, and the most appropriate healthcare professional to manage them. The future of practice is tending towards multidisciplinary team work on many scales [35] and a qualitative evaluation (patient surveys, for example) of people’s perception of care received at home from multidisciplinary teams may be interesting to assess the repartition of healthcare resources.
In conclusion, there is a high diversity among the content of family physician home visits, which are, however, mostly routine visits consisting of consultation time without additional investigations and concerning mainly older people. This suggests that the main purpose of home visits in the canton of Vaud is to maintain older people at home rather than managing emergency situations. The overall number of family physician home visits tended to decrease over the study time, but part of this trend may be attributed to the emergence of home-oriented healthcare organisations that work together with family physicians, and also the increased number of ED consultations. Thus, the future of maintaining older people at home may be multidisciplinary teamwork including family physicians and homecare services. The development of recommendations for the specific practice of home visits and qualitative patient surveys concerning non-family-physician home visits could be valuable in the process of a more adequate use of healthcare resources for home visits; with a relevant part of family physician home visits delegated to other healthcare professionals in the future.
Table S1 Proportion of items billed during home visits and for sub sample size 10%
| Studied population | Subsample size of 10% | |||
|---|---|---|---|---|
| n | % | n | % | |
| Consultation time | 451,634 | 100 | 45163 | 100 |
| Emergency | 157,921 | 35 | 20,166 | 44.65 |
| Physical examination | 66,229 | 14.7 | 6454 | 14.29 |
| Laboratory | 43,197 | 9.6 | 7468 | 16.54 |
| Medico-surgical procedures | 25,522 | 5.7 | 2328 | 5.15 |
| Reports | 4547 | 1.0 | 427 | 0.9 |
| Medications | 3093 | 0.7 | 223 | 0.49 |
| Vaccines | 2678 | 0.6 | 245 | 0.54 |
L. Herzig and T. Bischoff for initial study support and negotiations with the trust center.
Billing data made available by the trust centre (Centre de Confiance) of the Société Vaudoise de Médecine. This work was supported by a grant from the Avenir and Santé Foundation.
NS and SD are practicing GPs and members of the Société Vaudoise de Médecine, who are in charge of organising the duty service in the canton of Vaud.
1World Health Organization. Factsheet: Ageing and health. 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
2Kohli R, Babel J, Deplazes J. Les scénarios de l'évolution de la population de la Suisse et des cantons, de 2020 à 2050. Neuchâtel: Swiss Federal Statistical Office. 2020.
3 Kao H , Conant R , Soriano T , McCormick W . The past, present, and future of house calls. Clin Geriatr Med. 2009;25(1):19–34, v. doi:.https://doi.org/10.1016/j.cger.2008.10.005
4 Meyer GS , Gibbons RV . House calls to the elderly--a vanishing practice among physicians. N Engl J Med. 1997;337(25):1815–20. doi:.https://doi.org/10.1056/NEJM199712183372507
5 Mueller Y , David S , Cohidon C , Locatelli I , Senn N . Home visits made by general practitioners in the canton of Vaud between 2006 and 2015. Swiss Med Wkly. 2019;149:w20037. doi:.https://doi.org/10.4414/smw.2019.20037
6Association Vaudoise d’Aide et de Soins à Domicile. Dates-clés. 2012. Available from: http://www.avasad.ch/jcms/m_7022/fr/dates-cles
7 Efstathopoulou A , David S , Herzig L . [Home visits by GPs - Considerations in Europe and in Switzerland]. Rev Med Suisse. 2016;12(537):1874–8. Article in French.
8 Stuck AE , Egger M , Hammer A , Minder CE , Beck JC . Home visits to prevent nursing home admission and functional decline in elderly people: systematic review and meta-regression analysis. JAMA. 2002;287(8):1022–8. doi:.https://doi.org/10.1001/jama.287.8.1022
9 Elkan R , Kendrick D , Dewey M , Hewitt M , Robinson J , Blair M , et al. Effectiveness of home based support for older people: systematic review and meta-analysis. BMJ. 2001;323(7315):719–25. doi:.https://doi.org/10.1136/bmj.323.7315.719
10 Liimatta H , Lampela P , Laitinen-Parkkonen P , Pitkala KH . Effects of preventive home visits on health-related quality-of-life and mortality in home-dwelling older adults. Scand J Prim Health Care. 2019;37(1):90–7. doi:.https://doi.org/10.1080/02813432.2019.1569372
11 Mayo-Wilson E , Grant S , Burton J , Parsons A , Underhill K , Montgomery P . Preventive home visits for mortality, morbidity, and institutionalization in older adults: a systematic review and meta-analysis. PLoS One. 2014;9(3):e89257. doi:.https://doi.org/10.1371/journal.pone.0089257
12 Aylin P , Majeed FA , Cook DG . Home visiting by general practitioners in England and Wales. BMJ. 1996;313(7051):207–10. doi:.https://doi.org/10.1136/bmj.313.7051.207
13 Reuben DB , Fried TR , Wachtel TJ , Tinetti ME . When the patient cannot come to the doctor: a medical housecalls program. J Am Geriatr Soc. 1998;46(2):226–31. doi:.https://doi.org/10.1111/j.1532-5415.1998.tb02544.x
14 Peterson LE , Landers SH , Bazemore A . Trends in physician house calls to Medicare beneficiaries. J Am Board Fam Med. 2012;25(6):862–8. doi:.https://doi.org/10.3122/jabfm.2012.06.120046
15 Orup Larsen AS , Kristensen T , Lykkegaard J , Waldorff FB . Use of preventive home visits by general practitioners in patients diagnosed with dementia. Dan Med J. 2018;65(12):A5518.
16Statistique Vaud. Bilan démographique, grands groupes d'âges et population étrangère, par commune, Vaud, 2010–2018. 2019. Available from: http://www.scris.vd.ch/Default.aspx?DomId=1710
17TARMED. Navigateur tarifaire et banque de données. Bern: FMH Swiss Medical Association; 2019.
18Publique OFdlS. Liste des analyses (LA). 2019.
19 DoXmart. Arzneimittel-Informationen und Tipps für Sie und Ihre Praxis. DoXmedical. 2008;1:19–27.
20 SUVA. 2019.
21 Everitt BS . An introduction to finite mixture distributions. Stat Methods Med Res. 1996;5(2):107–27. doi:.https://doi.org/10.1177/096228029600500202
22 Govaert G , Nadif M . An EM algorithm for the block mixture model. IEEE Trans Pattern Anal Mach Intell. 2005;27(4):643–7. doi:.https://doi.org/10.1109/TPAMI.2005.69
23 Carreira-Perpinan MA , Renals S . Practical identifiability of finite mixtures of multivariate bernoulli distributions. Neural Comput. 2000;12(1):141–52. doi:.https://doi.org/10.1162/089976600300015925
24 KJ. B. RandomLCA: An R package for Latent Class with Random Effects Analysis. J Stat Softw. 2017;81(13):1–25.
25Grün B. Model-based clustering, in Handbook of Mixture Analysis. GC Sylvia Fruhwirth-Schnatter, Christian P Robert Editors. Chapman & Hall / CRC Press. 2019.
26 Locatelli I , Monod S , Cornuz J , Büla CJ , Senn N . A prospective study assessing agreement and reliability of a geriatric evaluation. BMC Geriatr. 2017;17(1):153. doi:.https://doi.org/10.1186/s12877-017-0546-9
27 Charrad M , Ghazzali N , Boiteau V , Niknafs A . NbClust: An R package for determining the relevant number of clusters in a data set. J Stat Softw. 2014;61(6):1–36. doi:.https://doi.org/10.18637/jss.v061.i06
28Santé et soins: chiffres-clés. In: Publique, SdlS, Editor. 2018.
29Clémence Merçay O. Le recours aux services d'urgence en Suisse - Description des différences cantonales. Obsan dossier 64. Neuchâtel: Obsan; 2018.
30 Sanchez B , Hirzel AH , Bingisser R , Ciurea A , Exadaktylos A , Lehmann B , et al. State of Emergency Medicine in Switzerland: a national profile of emergency departments in 2006. Int J Emerg Med. 2013;6(1):23. doi:.https://doi.org/10.1186/1865-1380-6-23
31 Corscadden L , Levesque JF , Lewis V , Strumpf E , Breton M , Russell G . Factors associated with multiple barriers to access to primary care: an international analysis. Int J Equity Health. 2018;17(1):28. doi:.https://doi.org/10.1186/s12939-018-0740-1
32 van den Berg N , Meinke C , Matzke M , Heymann R , Flessa S , Hoffmann W . Delegation of GP-home visits to qualified practice assistants: assessment of economic effects in an ambulatory healthcare centre. BMC Health Serv Res. 2010;10(1):155. doi:.https://doi.org/10.1186/1472-6963-10-155
33 Herzig L , Chappuis A , Camain JY , Burnand B , Jotterand S . [Adaptation of clinical practice guidelines--the example of cantonal Diabetes Program]. Rev Med Suisse. 2012;8(341):1049–53.
34 Aebischer O , Rochat M , Méan M . [Use of clinical practice guidelines in medicine : what’s new? ]. Rev Med Suisse. 2017;13(584):2036–9.
35 Favale R , Al-Sultan S , Gavinio R . [From permanence to the group practice and then to the health center: New frameworks for new roles and skills of the primary care physician]. Rev Med Suisse. 2018;14(620):1695–7.
Billing data made available by the trust centre (Centre de Confiance) of the Société Vaudoise de Médecine. This work was supported by a grant from the Avenir and Santé Foundation.
NS and SD are practicing GPs and members of the Société Vaudoise de Médecine, who are in charge of organising the duty service in the canton of Vaud.