In the eye of the hurricane: the Swiss COVID-19 pandemic stepwise shutdown approach in organ donation and transplantation
DOI: https://doi.org/10.4414/smw.2020.20447
Franz F
Immera, Christian
Bendenab, Andreas
Elmera, Nathalie
Krügela, Susanne
Nyfelerc, Mathias
Nebikerd, Markus J
Wilhelmbe, Cédric
Hirzelf, National Committee for Organ Donation (CNDO), Medical Committee (CM), Swisstransplant Infectious Diseases Working Group (STAI)
a Swisstransplant, Berne, Switzerland
b University of Zurich Faculty of Medicine, Zurich, Switzerland
c Federal Office of Public Health, Berne, Switzerland
d Department of Intensive Care, Berne University Hospital, University of Berne, Switzerland
e Department of Cardiac Surgery, University Hospital Zurich, Switzerland
f Department of Infectious Diseases, Berne University Hospital, University of Berne, Switzerland
Summary
AIMS OF THE STUDY
Coronavirus disease 2019 (COVID-19) pandemic has an ongoing severe impact on health care, but there is a lack of information on COVID-19 and its effect on organ donation and solid organ transplantation. Early in the pandemic, Swisstransplant, the Swiss National Foundation for Organ Donation and Transplantation, set up a national stepwise shutdown approach to avoid a collapse of transplant activities during phases of the pandemic with sufficient available healthcare capacities. The approach allowed regional adaptation of transplant-associated activities depending on available healthcare capacities, instead of implementing a rigid centralistic system. The aim of this study was to describe the stepwise shutdown approach and to determine whether this flexible approach would be helpful for avoiding complete cessation of transplant activities during a pandemic.
METHODS
A retrospective nationwide study was conducted to evaluate donor procurement and solid organ transplantation activity in Switzerland during the COVID-19 pandemic (1 January to 31 May 2020). To assess the impact of the flexible stepwise shutdown plan on overall transplantation activity in Switzerland, we compared total and individual numbers of transplanted organs during the first wave of the pandemic with the transplant activity immediately before the pandemic.
RESULTS
The pandemic evolved heterogeneously across Swiss cantons, severely affecting western cantons and the Ticino. Overall, there was a reduction in deceased donor transplants in Switzerland of 16.7% in March and April 2020 (during the pandemic) compared with January and February 2020 (prior to the pandemic), the decline mostly driven by kidney transplants (−27.6%) and to a lesser extent by transplants of vital organs (heart, lungs, liver) (−5.9%). In May 2020, solid organ transplantation activity in Switzerland again exceeded the average of pre-pandemic months (January and February), with 35 transplanted organs, but the increase from April to May 2020 was exclusively driven by liver and kidney transplants.
CONCLUSION
The Swiss stepwise shutdown approach in organ donation and transplantation helped to maintain a limited national organ procurement and vital organ transplant activity, avoiding a complete nationwide shutdown of organ donation and transplant activity. We therefore propose a flexible shutdown approach that regulates transplant activities dependent on regional healthcare resources rather than uniform centralistic regulations. This approach proved to be especially useful during a regional heterogeneously evolving pandemic.
Introduction
In December 2019, a novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), emerged in Wuhan, in the Chinese Province of Hubei, causing an unprecedented pandemic [1, 2]. The World Health Organization (WHO) labelled the disease caused by SARS-CoV-2 coronavirus disease 2019 (COVID-19), and declared COVID-19 a public health emergency of international concern on 30 January 2020 [2]. The COVID-19 pandemic has so far had a tremendous impact worldwide, with major consequences for health care, the world economy and social affairs. There is a massive impact on healthcare resources, in particular, the need for intensive care unit (ICU) beds and mechanical ventilatory support [2]. However, it was unknown how COVID-19 effects organ donation and solid organ transplantation in the future [3]. Recently, Loupy et al published data that quantified the contemporary impact of the COVID-19 pandemic on organ donation and transplantation in France and the USA, showing a strong association between the increase of COVID-19 infections and the reduction in transplant activity [4]. Deceased organ transplant procedures dropped after the start of the COVID-19 pandemic by 90.6% in France and by 51.1% in the USA [4]. Further, the authors reported a significant decline in solid organ transplantation rates even in regions with a low COVID-19 prevalence [4].
In Europe, Italy was the first country severely struck by the pandemic [5]. Given the fact that thousands of Northern Italian citizens daily cross the Italian-Swiss border to the Canton of Ticino, the southernmost canton of Switzerland to commute to work, it was expected that Switzerland would face a similar healthcare crisis to Italy. On 25 February 2020, the first SARS-CoV-2 positive individual was diagnosed in the Swiss Canton of Ticino [6]. Like Italy, where mainly the northern part and particularly Lombardy were affected, the COVID-19 pandemic in Switzerland also evolved heterogeneously in different regions. Of the 8,570,000 Swiss citizens, two thirds populate the German-speaking areas in the north and north-east, just over 20% live in the predominately French-speaking cantons in western Switzerland, and less than 10% inhabit the Italian-speaking Canton of Ticino in south Switzerland on the border with Italy. By far the highest incidences of SARS-CoV-2 infection were recorded in the French- and Italian- speaking cantons, with an incidence of more than 100 confirmed cases per 10,000 inhabitants in the Canton of Geneva, closely followed by the Canton of Ticino with more than 90 cases per 10,000 inhabitants from March to May 2020 [7]. The peak of the pandemic in terms of hospitalisations occurred on 2 April 2020 [7].
When the pandemic hit Switzerland, resources for organ donation and transplantation had to be evaluated. Swisstransplant, the Swiss National Foundation for Organ Donation and Transplantation with headquarters in Berne, decided to establish a nationwide stepwise shutdown approach, which allows adaption of transplant-associated activities regionally, dependent on local healthcare capacities. The major goal was to coordinate transplant activities in a structured manner in order to provide a continuous opportunity for critically ill patients on the national transplant waiting list to receive a life-saving transplantation. Furthermore, guidelines were established on how to proceed with deceased and living organ and tissue donors, guided by infectious diseases specialists from all Swiss transplant centres.
We assumed that Swiss organ donation is structured in a similar way to that of France, with a centrally organised national organ allocation, and that we would therefore see similar consequences. Given the recently published detrimental French data on organ procurement and transplantation, we aimed at analysing the effect of the COVID-19 pandemic on the organ donation rate and solid organ transplantation in Switzerland. With this in mind, we looked at whether the Swiss stepwise shutdown approach allowed transplant activities to be maintained at an acceptable level during the pandemic. We were interested to learn if our new approach enabled at least transplantation of vital organs for critically ill patients to be maintained. Briefly, in Switzerland, there are six transplant centres, two in the French speaking part (Geneva and Lausanne) and four in the German speaking part (Basel, Berne, St Gallen and Zurich). Transplant centres in Basel and St Gallen offer kidney transplantation only; whole pancreas and islet transplantation is available only in Geneva and Zurich. Organ procurements are made at the level of the five university hospitals and in nine tertiary hospitals. Of these tertiary hospitals, there are three hospitals in the French-speaking part (Fribourg, Sion and Neuchâtel), five hospitals in the German speaking part (Aarau, Chur, Luzern, St Gallen and Winterthur) and one hospital in the Italian speaking part (Lugano).
Patients and methods
A retrospective nationwide study was conducted to evaluate donor procurement and solid organ transplantation activity in Switzerland during the COVID-19 pandemic (from 1 January 2020 to 31 May 2020) under a newly developed stepwise shutdown approach for procurement hospitals and transplant services.
Measures to address safety of solid organ transplantation started with implementation of a nationwide stepwise shutdown approach for organ procurement that allowed regional adaption of transplant-associated activities dependent on local healthcare capacities. The goal was to avoid a complete cessation of organ donation after brain death (DBD) and donation after circulatory death (DCD) (table 1
).
Table 1 The steps of the “Swiss COVID-19 pandemic stepwise shutdown approach” that were applied to organ donation and procurement programmes.
|
Step
|
Action
|
Result
|
| 1 |
National case-by-case triage |
Centralised donor evaluation by the Medical Director of Swisstransplant based on quality of organs, transplant centre resources and recipients medical urgency. |
| 2 |
Stop DCD programme |
Detection and procurement of DCD donors stopped. |
| 3 |
Stop DBD programme |
Donor detection and procurement no longer available. |
The availability of donor detection and organ procurement was checked by daily e-mail correspondence among the heads of the five regional donor procurement networks and lead intensive care unit (ICU) physicians at hospitals with procurement facilities. The daily update provided a national overview on decisions taken by the procurement hospitals and transplant centres in charge.
The stepwise shutdown approach was put into operation during the pandemic at all Swiss transplant centres as of 13 March 2020. It covered living donor transplantation and deceased donor detection in Switzerland, and also the modality of acceptance and availability of potential procurement of offers from outside Switzerland by transplant teams at each centre. For living and deceased donors, we implemented the following steps in order to avoid a complete shutdown and to give a national overview on the availability of regional resources as shown in table 2.
Table 2 The steps of the “Swiss COVID-19 pandemic stepwise shutdown approach” that were applied to organ transplant programmes.
|
Step
|
Action
|
Result
|
| 1 |
Stop all living donation transplantation |
Elective transplantations from living donors no longer available |
| 2 |
Stop pancreas and islets transplantation |
Pancreas/islets transplantation from deceased donors no longer available |
| 3 |
Stop kidney transplantation |
Kidney transplantation from deceased donors no longer available, including kidney/pancreas and kidney/islets |
| 4 |
Tailored approach for vital organs and/or urgent status recipients |
Only elective transplantations of vital organs or urgent transplantations to be performed |
| 5 |
Stop all non-urgent transplantations |
Only urgent transplantations to be performed (heart, kidney, liver, lung) |
| 6 |
Stop all transplantation activity |
Transplantation no longer available |
As of 17 March 2020, all possible/potential donors were reported to Swisstransplant. The case-to-case triage carried out by the medical advisor of Swisstransplant led to the enrolment of potential donors based on the actual situation on the waiting list and the availabilities of transplant programmes.
Furthermore, a special “Swiss Pandemic Urgent Status” was accepted by the three liver transplantation centres and the Swiss Federal Office of Public Health (FOPH) in the limited time period of the national lockdown. Since the Model for End-stage Liver Disease (MELD) criteria are rather weak in selecting patients, the Swiss Pandemic Urgent Status was mainly applied to patients at high risk (mortality) and expected short stay on the ICU and then selected, mainly based on the actual MELD or Standard Exceptions(SE)-MELD value.
Swisstransplant remained actively involved on an international level, with the intention to facilitate cross-border organ sharing. Team availabilities and logistic facilities were checked daily, and the interest of Switzerland in accepting foreign donor organs was communicated to international partners weekly.
For foreign donor organ offers, we defined stepwise measures as presented in table 3. Even though centres aimed to avoid travel of the procurement teams, in multiple cases (i.e., heart and lung procurement), Swiss teams went to the foreign donor hospital for procurement.
Table 3 The steps of the “Swiss COVID-19 pandemic stepwise shutdown approach” that were applied to cross-border organ exchange.
|
Step
|
Action
|
Result
|
| 1 |
Stop all cross-border living donation transplantation |
Elective transplantations from cross-border living donors no longer available |
| 2 |
Stop import of pancreas/islets and small bowel |
Pancreas/islets and small bowel transplantation from cross-border deceased donors no longer available |
| 3 |
Stop import of kidney grafts |
Kidney transplantation from cross-border deceased donors no longer available, including kidney/pancreas and kidney/islets |
| 4 |
Selected import of vital organs only |
Only elective transplantations of foreign vital organs |
| 5 |
Selected import of vital organs for patients in urgent status only |
Only life-saving transplantations of foreign organs to be performed (heart, liver, lung) in patients in urgent status. |
| 6 |
Complete stop of foreign donor organ import |
Transplantation utilizing foreign donor organs no longer available |
Further administrative and organisational steps were introduced. ICU donor coordinators, on the Swisstransplant payroll, were secondarily enrolled at the level of hospitals and partly exempt from their tasks on the donor procurement side. In addition, the national coordination team (mostly ICU-trained nurse specialists) were partly enrolled at the level of hospital ICUs to provide staff support, aiming to avoid cancellation of transplant activity due to shortness of specialised staff. Subsidiarity between individual transplant teams due to the local pandemic situation was discussed, i.e., in Geneva, where all transplant activities were halted, except for urgent cases only [8]. Swiss liver transplant centres collaborated and ensured that any centre not being able to perform transplants for COVID-19-related logistical reasons would be supported, even by potentially transferring patients to the other two still operating centres for the transplant procedure.
Statistical analysis
Epidemiological data on COVID-19 in Switzerland were extracted from www.corona-data.ch. The COVID-19 prevalence (cases per 10,000 permanent resident population) in each canton was used to visualise the spread of COVID-19 across Switzerland. We analysed organ procurement and transplantation activity according to the Swisstransplant stepwise shutdown approach for the period of 17 March 2020 to 11 May 2020 (data were updated daily from 17 March 2020 to 4 April 2020, and weekly from 29 April 2020 to 5 May 2020). Only publicly available information was used for analysis, hence not requiring additional institutional review board approval. To show the targeted application of the stepwise shutdown, the status according to the three approaches for all 14 hospitals providing organ procurement and/or transplantation programmes is presented.
To assess the impact of the COVID-19 pandemic on the overall transplantation activity in Switzerland, we compared total and individual numbers of transplanted organs with the total number of ascertained COVID-19 cases over the period from 1 January 2020 to 31 May 2020. Data on transplanted organs from deceased donors were accessed by an automated database query in the Swiss Organ Allocation System (SOAS) and arranged using the freely available software R (version 3.6.0). Numbers were grouped by organ and month. Multi-organ transplantation counted to each of the respective organ and “double transplantations” (i.e., both kidneys to the same recipient) counted as two organs.
Results
Availability of organ donor detection and procurement, and transplant programme availability during the pandemic
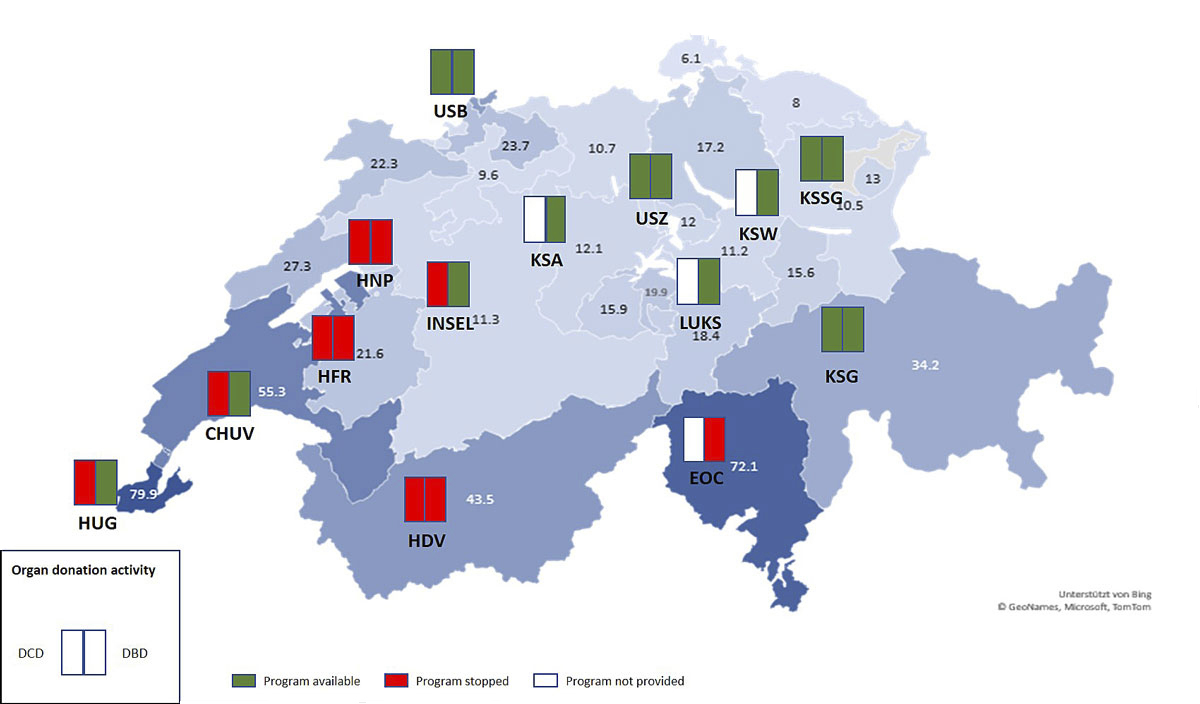
Under normal circumstances prior to the pandemic, a total of 14 centres (university hospitals and tertiary hospitals) provide identification of potential deceased organ donors and procurement services. Figure 1 represents a snapshot of the availability of deceased organ donor procurement across Switzerland on 6 April 2020, during the peak of the pandemic. In north-eastern cantons of Switzerland, where COVID-19 prevalence was below the national average, identification of potential deceased organ donors and procurement service was available as usual in all hospitals, whereas in the western and southern cantons all existing DCD programmes were completely discontinued. The DBD programmes in the western and southern cantons remained available only in the three large university hospitals of Geneva (University Hospital Geneva, HUG), Lausanne (University Hospital Lausanne, CHUV), and Berne (Inselspital, University Hospital Berne).
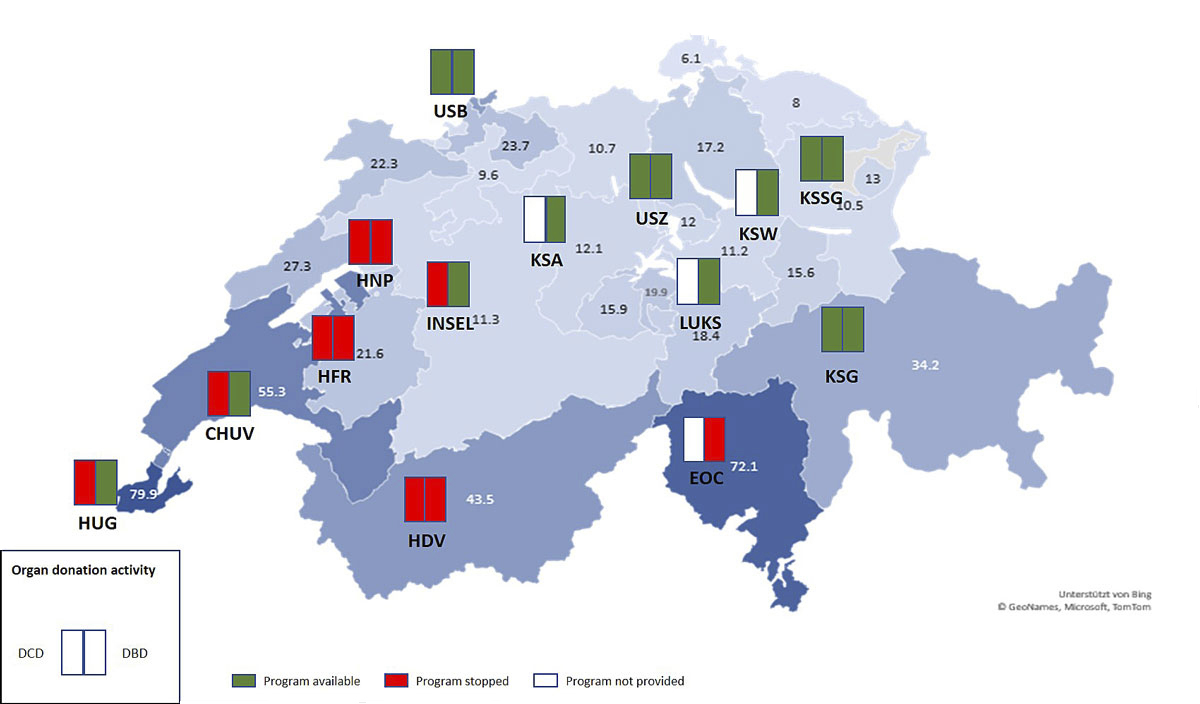
Figure 1 Availability of DCD programmes (left column) and DBD programmes (right column) in the 14 procurement centres in Switzerland on 16 April 2020, according to the stepwise shutdown approach for organ procurement described in “Patients and methods” (table 1). The prevalence of COVID-19 for each Swiss canton is shown per 10,000 inhabitants on 6 April 2020 (www.corona-data.ch). In all active procurement programmes, a centralised national case-by-case triage was applied between 17 March and 11 May 2020 (step 1, not shown).
CHUV = University Hospital Lausanne; DBD = donation after brain death; DCD = donation after circulatory death; EOC = Cantonal Hospital Lugano; HDF = Cantonal of Hospital of Valais; HFR = Cantonal Hospital Fribourg; HNP = Cantonal Hospital Neuchatel; HUG = University Hospital Geneva; Insel = University Hospital Berne; KSA = Cantonal Hospital Aarau; KSG = Cantonal Hospital of Graubünden; KSW = Cantonal Hospital Winterthur; KSSG = Cantonal Hospital St Gallen; LUKS = Cantonal of Hospital of Lucerne; USB = University Hospital Basel; USZ = University Hospital Zurich
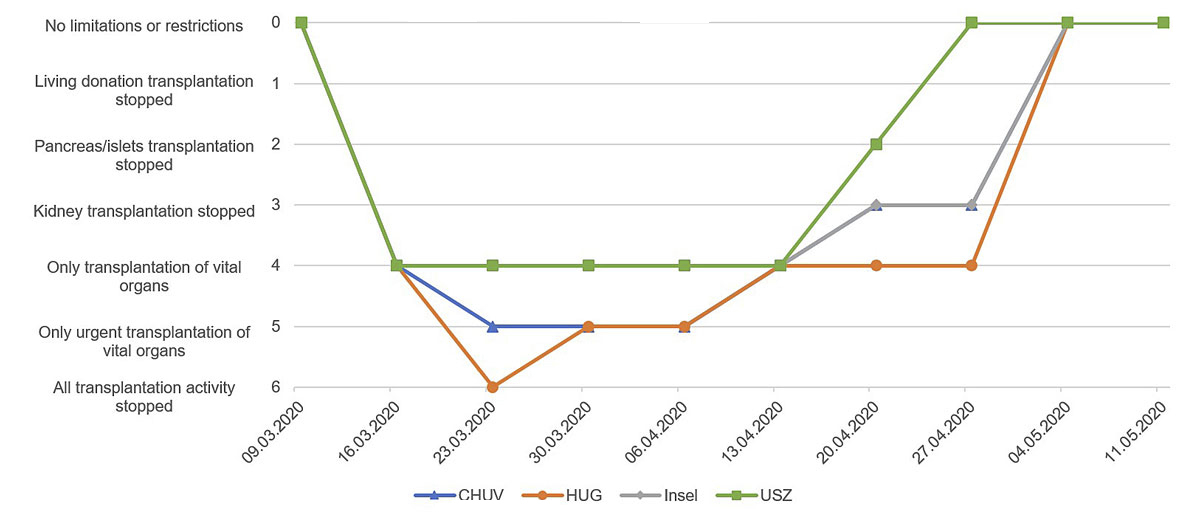
During normal conditions, a total of six university or tertiary hospitals provide transplant programmes for one or several organs, including kidney and liver transplantation from living donors. Figure 2 shows the availability of organ transplant programmes across Switzerland from 9 March 2020 to 11 May 2020, according to the stepwise shutdown approach used during the pandemic in Switzerland. Transplantation from living donors, pancreas/islets transplantation and kidney transplantation was stopped from 16 March to 13 April in all centres nationwide. At HUG in Geneva and CHUV in Lausanne – located in regions with the highest COVID-19 prevalence – transplantation was limited to vital organs and urgently listed patients only during the same period. At HUG, transplant activities even completely ceased for one week. From mid-April, transplant activities were resumed step-by-step, first at centres in the least affected eastern part of Switzerland (i.e., in Zurich), subsequently also at centres located elsewhere in Switzerland, and ultimately in Geneva.
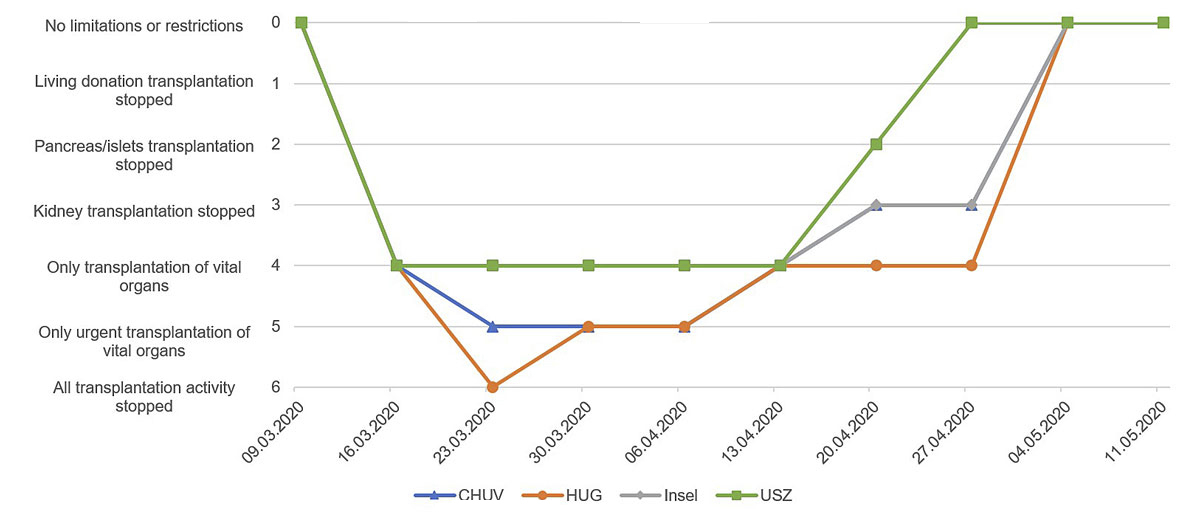
Figure 2 Availability of the four transplant centres with multiple organ transplant programmes in Switzerland according to the stepwise shutdown approach described in “Patients and methods” (table 2) over time. Shown here are weekly statuses from 9 March 11 to May 2020.
CHUV = University Hospital Lausanne; HUG = University Hospital Geneva; Insel = University Hospital Berne; USZ = University Hospital Zurich
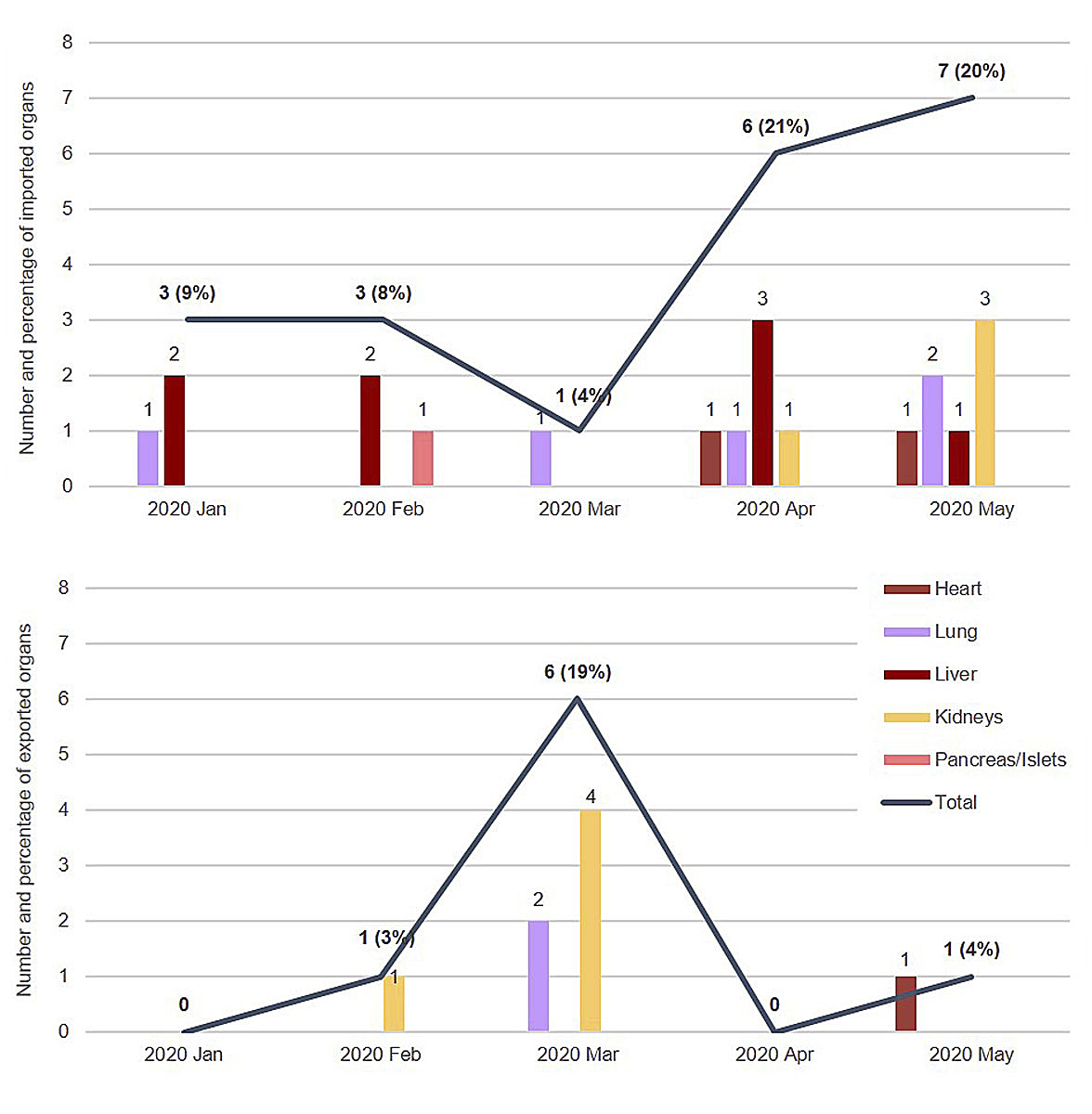
The limited availability of the Swiss organ transplant programmes, particularly in the month of March, is reflected in substantially reduced organ importation. In the months of April and May, organ importation increased strongly, reaching high figures (six imported organs in April and seven in May). Every fifth organ transplanted in Switzerland was retrieved at foreign procurement centres and imported to Switzerland in April and May 2020, whereas prior to the pandemic, in January and February 2020, the percentage of imported organs was below 10%. The number of exported organs shows an opposite development, with six organs (19%) exported in March 2020, which is clearly above the usual monthly average (1–5%). This reflects the maintained ability of donor detection and procurement activities in about half of the Swiss procurement centres even during the pandemic’s peak in Switzerland. Organs procured in Switzerland during this period were made available for patients in other European countries as transplant capacities were limited in Switzerland (fig. 3).
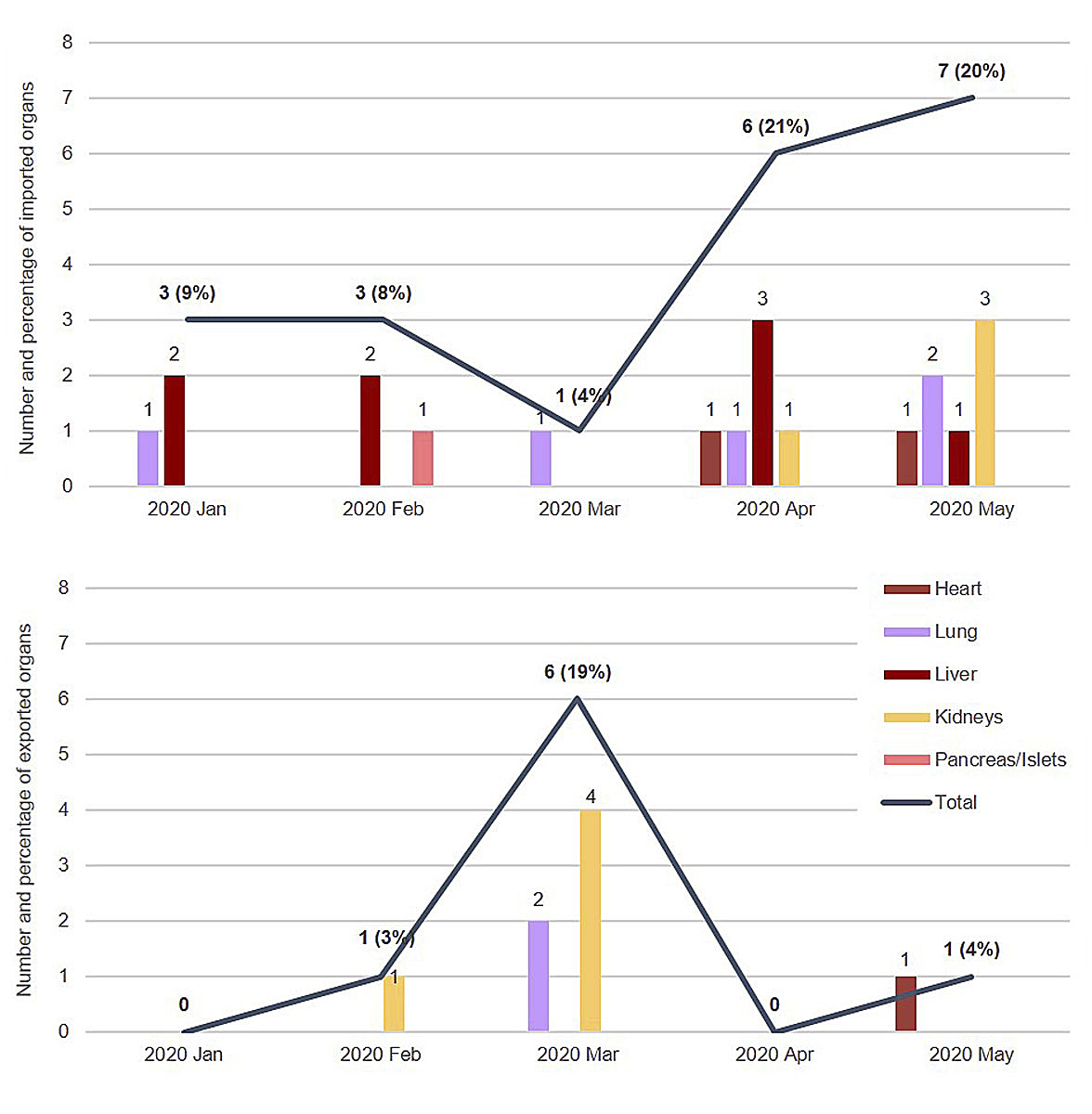
Figure 3 Number of foreign organs imported (upper chart) and exported (lower chart) over time. For total numbers, in brackets, import share in percent of all transplanted organs in Switzerland, and export share in percent of all transplanted organs from Swiss deceased donors, respectively, are given. From January to May 2020, organs were exchanged with France (18 organs), Italy (3 organs), Spain (2 organs), the United Kingdom (2 organs), and with Germany, Sweden, and Lithuania (1 organ each).
Impact on solid organ transplantation
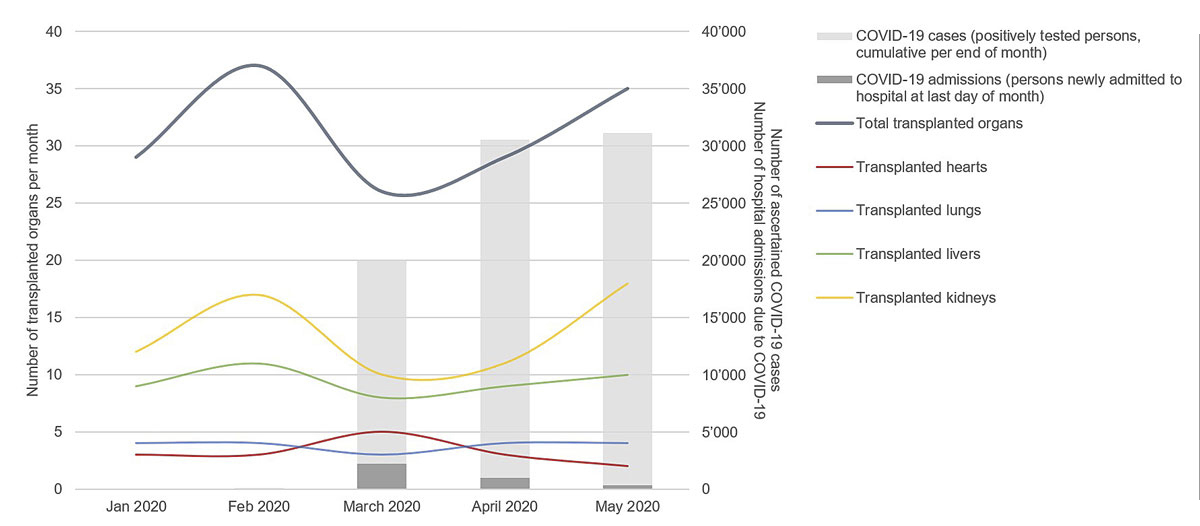
There was an overall reduction in deceased donor transplantation in Switzerland of 16.7%, when March and April 2020 (during the pandemic) were compared with January and February 2020 (prior to the pandemic). This decline was mostly driven by kidney transplantation (−27.6%) and to a lesser extent by transplants of the vital organs heart, lungs, and liver (−5.9%). In May 2020, solid organ transplantation activity in Switzerland exceeded the average of the pre-pandemic months January and February, with 35 transplanted organs. However, the increase from April to May 2020 was exclusively driven by liver and kidney transplantation (fig. 4).
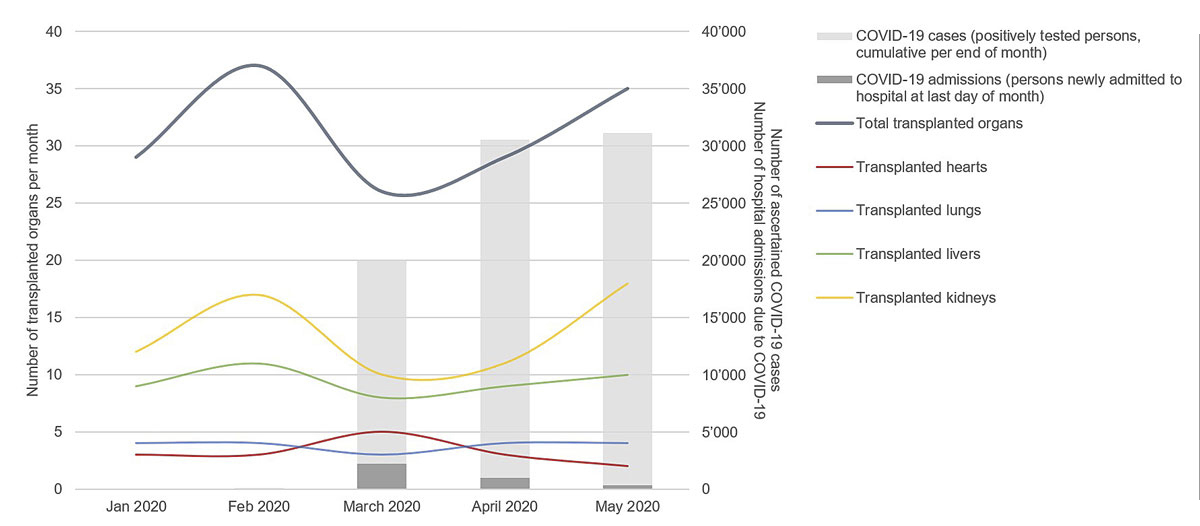
Figure 4 Trends in COVID-19 prevalence, COVID-19 hospital admissions, and solid organ transplants from deceased donors over time in Switzerland. COVID-19 = coronavirus disease 2019.
During the study period, no patient with respiratory failure secondary to severe COVID-19 underwent lung transplantation. Furthermore, no patient with COVID-19 underwent solid organ transplantation. To the authors’ knowledge, no transplant recipient developed COVID-19 in the early post-transplant stage during the study period; however, no systematic nationwide SARS-CoV-2 screening programme was in place.
Discussion
To the authors’ knowledge, we describe for the first time a nationwide stepwise shutdown approach for organ donation and transplantation in response to the COVID-19 pandemic. Our approach included a daily communication by email on the current availability of donation and transplantation programmes for each hospital, and the availability of cross-border organ exchange. We are convinced that this constant communication was crucial and helped to raise the awareness that hospital occupancy rates due to COVID-19 varied greatly from region to region, and thus the availability of resources for organ donation and transplantation also varied. We believe that our approach helped to maintain a reduced organ procurement activity in about half of the Swiss procurement centres. On a national level, our approach facilitated maintaining the transplantation activity for vital organs and urgently listed patients on the national waiting list, preventing a steeper decline of transplant numbers in Switzerland during the first wave of the COVID-19 pandemic.
In general, the deceased donor rate in Switzerland is rather low, with fewer than 20 deceased donors per million steady population [9]. In 2019, 36% of the deceased donors were DCD Maastricht III donors (awaiting cardiocirculatory death) [10]. French- and Italian-speaking parts of Switzerland contributed almost 40% to the total number of deceased donors in year 2019 [10]. However, the French- and Italian-speaking parts of Switzerland have were the areas mainly affected by the pandemic. Therefore, shutting down all DCD programmes and donor detection in four large procurement hospitals in these areas because of the COVID-19 pandemic had major implications for solid organ transplantation activity in Switzerland.
To date, data on the impact of the COVID-19 pandemic on worldwide organ donation and transplantation activity are limited. The negative impact of the pandemic on transplant activity in France and the USA was previously reported by Loupy and coworkers, revealing a more than 90% decline in deceased organ transplant procedures in France and more than 50% in the USA [4]. Switzerland has the higher COVID-19 prevalence at 27.7 compared with 18.6 and 22.1 in France and the USA, respectively. France and Switzerland have comparable healthcare systems and centrally organised national organ allocation. In contrast to other countries, it was possible to maintain transplant activities in Switzerland. We argue that the implementation of a flexible shutdown approach, which takes regional differences of healthcare capacities during a pandemic into account, was a crucial step to avoid dramatic decreases in transplant activity. The daily coordination by Swisstransplant, in close collaboration with the procurement hospitals and transplant centres, has been essential to this approach. The daily updates by Swisstransplant also provided an overview on national donation activity (number of donors evaluated/enrolled), foreign offers (cross-border organ exchange), as well as the situation on the national wait list (patients in urgent status, medical status of patients on the national wait list awaiting vital organ transplants) within the last 24 hours.
Due to the shutdown of the DCD programmes on the donor side in the French- and Italian-speaking parts of Switzerland on 18 March 2020, a case-by-case triage of potential donors (step 3) was implemented immediately. A careful selection of extended criteria organ donor offers was also essential in view of the limited resources in times of a pandemic, balanced with the need of ongoing transplantation of vital organs and urgently listed transplant candidates. This prompt and very close involvement of relevant national stakeholders by Swisstransplant on the donor and transplantation side was probably the main reason for the success of the stepwise shutdown approach. Swisstransplant’s lead role and the knowledge that in selected areas in Switzerland – mainly in the German speaking part – resources were available, was important. During this time, we experienced an impressive level of commitment and solidarity across the country, with increased continuous communication and real-time adaptation of procurement and transplant activity. As chair of the European Committee on Organ Transplantation (CD-P-TO), Swisstransplant initiated an exchange of relevant documents through the platform created by the European Directory for Quality of Medicine and Health Care (EDQM), which was used by many other European countries. In order not to discard good quality organs, Swisstransplant approached its partners through FOEDUS, the leading platform for facilitating exchange of organs in Europe (covering a population of 372 million inhabitants), to stimulate import and export, and overcome logistic issues during the pandemic.
In view of limited resources, Swisstransplant was able, with support by the FOPH, to review allocation modalities, introducing a timely limited “Swiss Pandemic Urgent Status” for liver transplant recipients, which allowed the experts to establish a tailored approach in patient selection and provided access to transplantation to those patients with a suspected high wait list mortality but hopefully a shorter post-transplantation ICU stay [8]. The effect of reduced donor volume on resource allocation has very recently been discussed for cardio-thoracic transplantation, also [10].
It is important to emphasise that the introduction of a stepwise shutdown approach, moving forward in different steps at individual centres also allowed potential re-opening of individual programmes to be to some degree anticipated, based on regional pandemic status and local resources. In this context, kidney transplantation has been re-launched very early in most centres, after almost 5 weeks of shutdown, reaching activities similar to those before the COVID-19 pandemic in May. Furthermore, donor procurement programmes were re-opened very fast as a result of the involvement of ICU staff at procurement centres and their willingness to respond to the need of donor organs for patients on the national wait list.
As mentioned before, the stepwise shut down approach also allowed a certain timely limited subsidiarity of donor coordinators (mostly trained ICU staff) and Swisstransplant medical staff to support local ICUs and transplant centres.
Strength and limitations
It is the strength of our study that it describes for the first time a nationwide stepwise shutdown approach for organ donation and transplantation in response to the COVID-19 pandemic. But our study has several limitations due to its retrospective design and small patient numbers. Given the descriptive nature of this national study, one cannot completely rule out that the development in organ donation and solid organ transplantation activity seen would have been different without the pandemic, thus a causative effect of our stepwise shutdown approach on organ donation and transplant activity is not proven. It also remains debatable if the complete shutdown of the nationwide kidney transplant activity in Switzerland was absolutely needed at the start of the pandemic. Even though this step helped to redirect resources within the healthcare system under pressure of the pandemic, the 27.6% fall in kidney transplant activity during the pandemic placed an extreme burden on patients on the national wait list for kidney transplantation. In the case of a second wave of the pandemic, relocation of (staff) resources among centres should probably be the preferred approach. Furthermore, the authors acknowledge that the Swiss healthcare system is somewhat unique; thus, comparisons with other countries are by some means limited. Despite the high incidence of SARS-CoV-2 infection in Switzerland in spring 2020, the Swiss healthcare system overall coped well, ICU beds were available throughout the pandemic, and plans for expanding ICU beds were in place.
Conclusion
In summary, the Swiss SARS-CoV-2 pandemic stepwise shutdown approach in organ donation and transplantation assisted to maintain – at least – limited organ procurement and vital organ transplantation, avoiding a complete national shutdown of organ donation and transplant activity in Switzerland. We propose our approach of a coordinated triage as a suitable tool also for other countries with comparable healthcare systems and a centrally organised national organ allocation system in times of a pandemic, despite certain limitations. Our approach may also be extended internationally, as Swisstransplant has successfully done through FOEDUS, avoiding loss of good quality organs due to a pandemic situation and lack of resources.
Acknowledgements
The authors acknowledge all the members of the Medical Committee (CM), the National Committee for Organ Donation (CNDO), and the Swisstransplant Infectious Diseases Working Group (STAI) for their collaborative efforts and collegial support during the SARS-CoV-2 pandemic as detailed below (in alphabetical order).
CNDO members: Markus Béchir (Hirslanden Clinic Aarau), Jeannine Bienz (Cantonal of Hospital of Lucerne), Christian Brunner (Cantonal of Hospital of Lucerne), Corinne Delalay (University Hospital Geneva), Susann Endermann (Cantonal Hospital St Gallen), Edith Fässler (Cantonal Hospital St Gallen), Adam-Scott Feiner (University Hospital Lausanne), Eva Ghanfili-Schellenberg (Cantonal Hospital Lugano), Cornelia Gumann (Cantonal Hospital St Gallen), Eric Hüttner (Hospital Center Biel), Renato Lenherr (University Hospital Zurich), Mathias Nebiker (Berne University Hospital), Lilian Penfornus (University Hospital Geneva), Marc Pfluger (Berne University Hospital), Deborah Pugin (University Hospital Geneva), Stefan Regenscheit (University Hospital Zurich), Jan Sprachta (University Hospital Basel), Kai Tisljar (University Hospital Basel), Martin Wendt (University Hospital Zurich).
CM members: Thierry Berney (University Hospital Geneva), Isabelle Binet (Cantonal Hospital St Gallen), Pierre-Alain Clavien (University Hospital Zurich), Michael Dickenmann (University Hospital Basel), Philippe Dutkowski (University Hospital Zurich), Cédric Hirzel (Berne University Hospital), Thorsten Krüger (University Hospital Lausanne), Michele Martinelli (Berne University Hospital), Maurice Matter (University Hospital Lausanne), Thomas Müller (University Hospital Zurich), Ramona Odermatt (University Hospital Zurich), Manuel Pascual (University Hospital Lausanne), Lilian Penfornus (University Hospital Geneva), Olivier De Rougemont (University Hospital Zurich), Urs Schanz (University Hospital Zurich), Jean Villard (University Hospital Geneva), Bruno Vogt (Berne University Hospital), Markus Wilhelm (University Hospital Zurich).
STAI Members: Christoph Berger (Children’s Hospital Zurich), Katia Boggian (Cantonal Hospital St Gallen), Cédric Hirzel (Berne University Hospital), Nina Khanna (University Hospital Basel), Christian Garzoni (Clinica Luganese Moncucco), Oriol Manuel (University Hospital Lausanne), Nicolas Müller (University Hospital Zürich), Christian van Delden (University Hospital Geneva), Laura Walti (Berne University Hospital).
References
1
Aslam
S
,
Mehra
MR
. COVID-19: Yet another coronavirus challenge in transplantation. J Heart Lung Transplant. 2020;39(5):408–9. doi:.https://doi.org/10.1016/j.healun.2020.03.007
2
Hage
R
,
Steinack
C
,
Benden
C
,
Schuurmans
MM
. COVID-19 in patients with solid organ transplantation: a systematic review. Transplantology. 2020;1(1):1–15. doi:.https://doi.org/10.3390/transplantology1010001
3
Woolley
AE
,
Mehra
MR
. Dilemma of organ donation in transplantation and the COVID-19 pandemic. J Heart Lung Transplant. 2020;39(5):410–1. doi:.https://doi.org/10.1016/j.healun.2020.03.017
4
Loupy
A
,
Aubert
O
,
Reese
PP
,
Bastien
O
,
Bayer
F
,
Jacquelinet
C
. Organ procurement and transplantation during the COVID-19 pandemic. Lancet. 2020;395(10237):e95–6. doi:.https://doi.org/10.1016/S0140-6736(20)31040-0
5
Distante
C
,
Piscitelli
P
,
Miani
A
. COVID-2019 outbreak progression in Italian regions: approaching the peak by the end of March in Northern Italy and first week of April in Southern Italy. Int J Environ Res Public Health. 2020;17(9):3025. doi:.https://doi.org/10.3390/ijerph17093025
6COVID-19 in Switzerland, 2020 February 24 [Online]. [Accessed 2020 July 10.] Available from: https://covid-19-schweiz.bagapps.ch/de-2.html
7COVID-19 information for Switzerland, 2020 May 29. [Online]. [Accessed 2020 May 29]. Available from: http://www.corona-data.ch
8
Moeckli
B
,
Peloso
A
,
Oldani
G
,
Orci
LA
,
Banz
V
,
Dutkowski
P
, et al.
The Swiss approach to the COVID-19 outbreak. Am J Transplant. 2020;20(7):1935–6. doi:.https://doi.org/10.1111/ajt.15939
9
Weiss
J
,
Elmer
A
,
Béchir
M
,
Brunner
C
,
Eckert
P
,
Endermann
S
, et al.; Comité National du Don d’Organes (CNDO). Deceased organ donation activity and efficiency in Switzerland between 2008 and 2017: achievements and future challenges. BMC Health Serv Res. 2018;18(1):876. doi:.https://doi.org/10.1186/s12913-018-3691-8
10
https://www.swisstransplant.org/fileadmin/user_upload/Swisstransplant/Jahresbericht/2019/Swisstransplant-Jahresbericht_2019.pdf