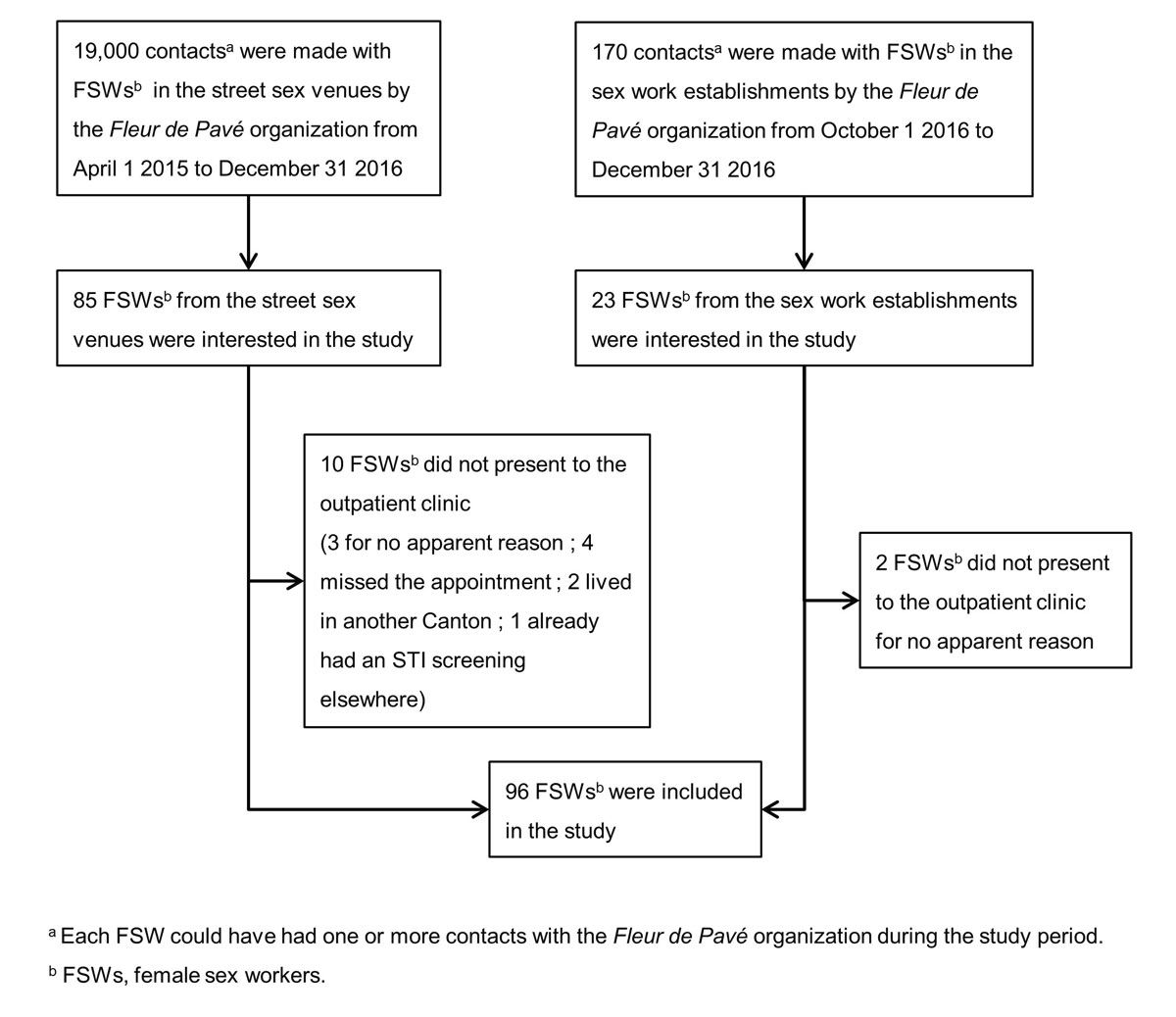
Figure 1 Study flow chart. The study was performed from 1 April 2015 to 31 December 2016 in Lausanne, Switzerland.
DOI: https://doi.org/10.4414/smw.2020.20357
Sex work is diverse and occurs in various contexts around the world, but people who engage in sex work tend to bear disproportionately high risks and burdens of sexually transmitted infections (STIs) due to multiple factors, such as exposure to multiple sex partners, inconsistent condom use, social marginalisation and stigmatisation [1]. Most sex workers are female [2] and it is estimated that female sex workers are 14 times more likely to be living with human immunodeficiency virus (HIV) than other women of similar reproductive age in the same general population [3], with the highest rates of HIV infection in female sex workers in sub-Saharan Africa and Eastern Europe [4]. However, there is substantial heterogeneity in STI prevalence among female sex workers across and within different regions around the world. This is generally attributed to variations in the methodologies used in studies, but also to social, political, economic, structural and cultural factors [2]. In high-income countries, data on STI prevalence in the female sex worker population are scarce [1, 5–7], and some studies have reported higher prevalences of HIV [8], active hepatitis B [8], Chlamydia trachomatis [9] and human papillomavirus [10, 11] infections among female sex workers compared to other women from the same population.
In Switzerland, sex work is legal from age 18 years and older. Each of the 26 cantons is responsible for adapting the national recommendations regarding sex work regulations according to its regional context and legislation. In the canton of Vaud, where this study was conducted, immigrant sex workers must declare their work activity to the local authorities, allowing them in most cases to obtain a three-month temporary residence permit and to work legally in designated street sex venues and formal sex work establishments [12]. While it is estimated that 100 to 250 female sex workers are registered annually in local authorities’ records, these numbers are most likely an underestimate, according to local non-governmental organisations (NGOs) and police authorities. Despite the laws and regulations, many female sex workers continue to work in illegal conditions. Moreover, accessing health care services is difficult, as it requires financial coverage through healthcare insurance. Access to free-of-charge testing for STIs is not available to female sex workers Switzerland.
In its 2011–2017 National Programme on HIV and other STIs, the Swiss Federal Office of Public Health assumed that sex workers in Switzerland may be at higher risk of contracting STIs than the general population. Therefore, the Swiss Federal Office of Public Health advocated for targeted interventions aimed at improving STI prevention, diagnosis and treatment in this group [13]. However, data on STI epidemiology in female sex workers is lacking in Switzerland. To our knowledge, the only data on this comes from a pilot project in Western Switzerland in which 92 female sex workers, predominantly documented immigrants from South America, were tested for HIV from 2011 to 2013, and none tested positive for HIV [14]. The main objective of the present study was to contribute to filling this data gap by evaluating the prevalence of six STIs (HIV, hepatitis B, hepatitis C, C. trachomatis, Neisseria gonorrhoeae and syphilis) among local adult female sex workers in the urban area of Lausanne in Western Switzerland, an area that had a population of more than 350,000 residents in 2014 [15]. The secondary objectives were to document the sociodemographic, behavioural and basic medical characteristics, including the hepatitis vaccination coverage, of a selection of female sex workers. Moreover, from a public health perspective, the analysis of the study results may help the development of appropriate and enhanced screening programs for the female sex worker population.
A local, exploratory, cross-sectional study was conducted from 1 April 2015 to 31 December 2016 on a convenience sample of female sex workers in Lausanne, one of the five major cities in Switzerland and the capital city of the canton of Vaud. For years, social workers from a local non-governmental organisation called “Fleur de Pavé” have conducted outreach interventions from a bus located in the area where sex work is authorised by the city government every evening from Monday to Friday. Fleur de Pavé is an organisation dedicated to providing social support and legal advice to sex workers in the canton of Vaud. During the study period, adult (≥18 years) female sex workers who worked in the street sex venues were approached for recruitment by social workers from Fleur de Pavé during their outreach interventions in the streets of Lausanne. In addition, from 1 October to 31 December 2016, adult female sex workers who worked in formal sex work establishments were recruited from massage parlours and brothels in Lausanne by the Fleur de Pavé organisation. Male and transgender sex workers, as well as female sex workers under 18 years of age or who had severe cognitive impairments, were excluded from the study.
All female sex workers who were interested in the study were invited to present at the outpatient clinic of the Lausanne University Hospital, where an anonymous, multiple-choice format questionnaire was given to each participant. The questionnaire explored a selection of socio-demographic, behavioural and basic medical characteristics. The questionnaire was delivered to participants during a face-to-face interview with a nurse, using a secured computer program. Fleur de Pavé offered all participants support in the form of translation and social services when required. Since Fleur de Pavé’s social workers knew at least one of the languages spoken by each of the participants, the use by the nurses of a professional interpreting service by telephone was not necessary. Participants were asked to describe their age, country of birth, residential status in Switzerland and health care insurance coverage. They were also asked about their sexual orientation, sexual and illegal substance use risk behaviours, history of condom use, history of imprisonment, personal history of STI testing and diagnosis, history of hepatitis B vaccination, pregnancy status and any symptoms of STIs at the time of recruitment. The latter included fever, unusual fatigue, skin rash, papules or itching, vaginal discharge, painful urination, pain during sexual intercourse, heavy menstrual bleeding or bleeding between periods, anal itching or pain, sore throat and swollen lymph nodes. Finally, participants were asked whether or not they would agree to have a throat, vaginal and/or anal swab as part of an STI screening, and how much they would hypothetically agree to pay for an STI screening.
All participants were then offered free screening for HIV, syphilis, hepatitis B and hepatitis C using rapid, point-of-care tests (INSTI™ for HIV, OnSite Rapid Test™ for syphilis, VIKIA HBsAg™ for hepatitis B and OraQuick HCV™ for hepatitis C). C. trachomatis and N. gonorrhoeae were tested for by analysing urine samples using a specific, real-time, quantitative duplex polymerase chain reaction assay [16, 17]. Capillary blood was used for the HIV, syphilis and hepatitis B rapid tests, and saliva was used for the HCV rapid test. In cases of a positive point-of-care rapid test, a confirmation serology test was performed (Treponema pallidum haemagglutination test and rapid plasma reagin test for syphilis; anti-HIV-1 and anti-HIV-2 antibodies and p24 Ag for HIV; HBsAg, anti-HBs and anti-HBc antibodies for hepatitis B; anti-HCV antibodies for hepatitis C). Antibiotics were prescribed to those female sex workers diagnosed with bacterial STIs, while female sex workers diagnosed with viral STIs were sent to local infectious diseases specialists for treatment and follow-up. Referrals for care and follow-up required the identification of the female sex workers, which was only done after obtaining their consent. Female sex workers who had no history of hepatitis B vaccination or infection were offered the first dose of a combined vaccine against hepatitis A and B (Twinrix®) free of charge. Vaccinated participants were encouraged to come back to the outpatient clinic or to consult any other healthcare services to complete their vaccination plan. When needed, free translation and social support services were provided to the participants by social workers from the Fleur de Pavé organisation.
Each participant received an individual identification number. Data were collected in a secured electronic database. Descriptive statistics, such as frequencies and proportions, were obtained using Excel™.
This research was approved by the Ethics Committee of the Lausanne University (reference number 77/15). We obtained written consent from all study participants. Participants were given no incentives to participate. All participants were informed that our research would be published and consented to this. The ethics approval was obtained prior to commencing the study.
Ninety-six female sex workers were included during the study period, as shown in the flow chart in figure 1. Of these, 75 (78%) were recruited from street sex venues and 21 (22%) from formal sex work establishments. Participants were predominantly undocumented immigrants (60%) from sub-Saharan Africa and Eastern Europe; only one participant was Swiss born. Most participants had no health insurance coverage (72%). Demographic information is shown in table 1.
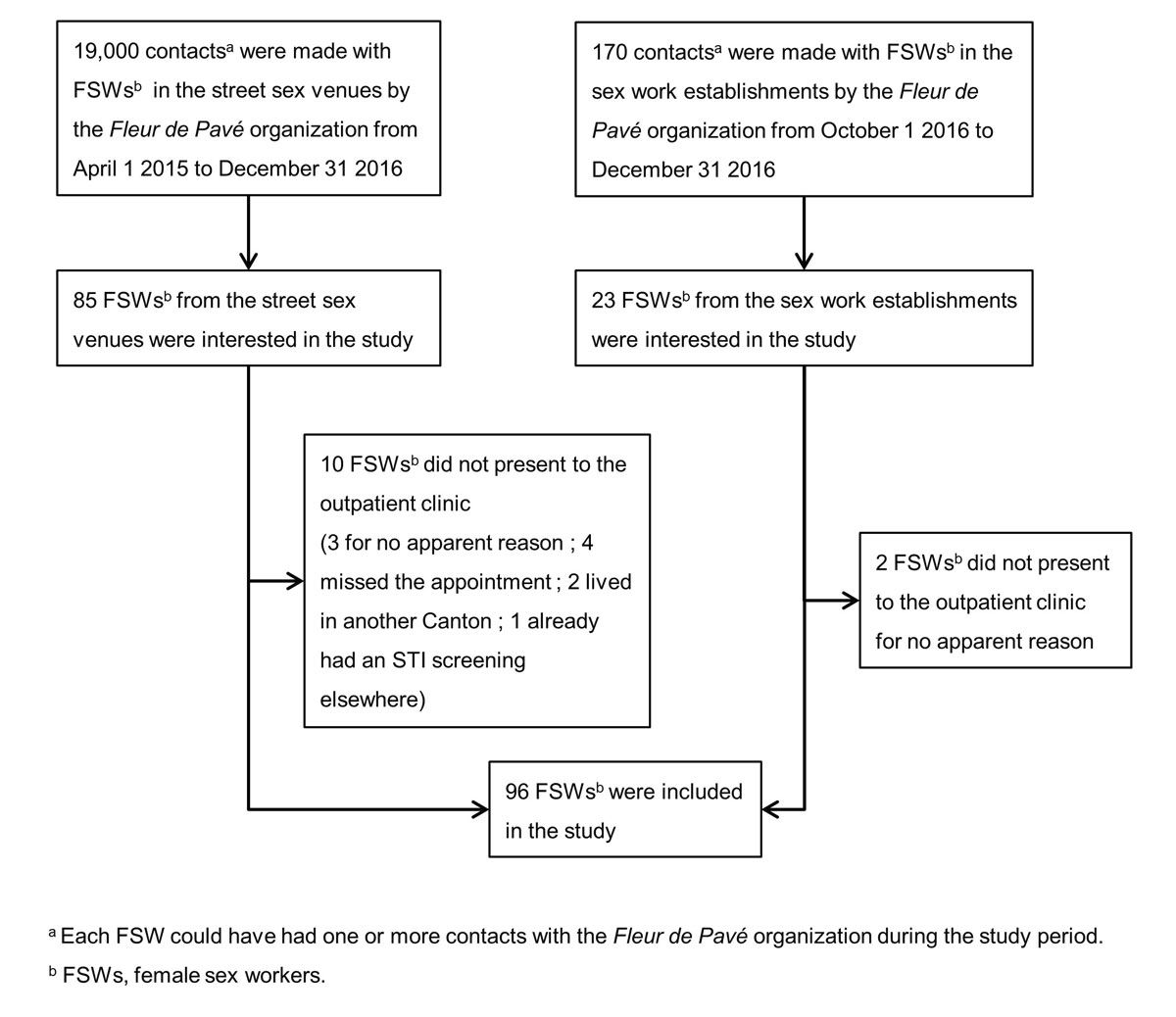
Figure 1 Study flow chart. The study was performed from 1 April 2015 to 31 December 2016 in Lausanne, Switzerland.
Table 1 Demographic characteristics of participants. The study was performed from 1 April 2015 to 31 December 2016 in Lausanne, Switzerland.
| Characteristic |
Participants, no. (%)
(N = 96) |
|---|---|
| Place of work | |
| Street sex venues | 75 (78) |
| Sex work establishments | 21 (22) |
| Age (years) | |
| 18–30 | 42 (44) |
| 31–40 | 34 (35) |
| 41–50 | 16 (17) |
| 51–60 | 4 (4) |
| Countries of birth regrouped by continent | |
| Africa (including Nigeria, Cameroun, Ghana, Democratic Republic of the Congo, Equatorial Guinea) | 60 (62) |
| South America (including Colombia, Brazil, Bolivia, Paraguay) | 10 (11) |
| Europe (including Romania, Spain, Bulgaria, Switzerland) | 26 (27) |
| Residential Status | |
| No permit | 58 (60) |
| “90 days” residential permit* | 19 (20) |
| Residential B permit† | 14 (15) |
| No response | 3 (3) |
| Swiss resident | 2 (2) |
| Healthcare insurance | |
| Yes | 27 (28) |
| No | 69 (72) |
* Short-term residential permit (3-month permit) † Long-term residential permit
The behavioural characteristics and basic medical information of the participants are presented in table 2. All the participants but one were heterosexual and fewer than a third (28%) always had protected sex (oral, vaginal and anal sex) with their clients or partners. Few participants had a history of illegal intravenous drug use (3%) or imprisonment (7%). According to the questionnaire, most (72%) had a history of STI screening, performed predominantly in other European countries, and 12% had already been diagnosed with one or more STIs during their lifetime. At the time of recruitment, four participants (4%) had a history of pregnancy and 10% had a history of symptoms of STIs. Most participants would agree to receive a throat, vaginal or anal swab (respectively 64%, 65% and 51%). The vast majority (91%) would want the STI screening to be totally free of charge.
Table 2 Risk factors and basic medical information of the participants and their willingness to undergo a sexually transmitted infection (STI) screening. The study was performed from 1 April 2015 to 31 December 2016 in Lausanne, Switzerland.
| Characteristic |
Participants, no. (%)
(N = 96) |
|---|---|
| Sexual orientation | |
| Heterosexual | 95 (99) |
| Bisexual | 1 (1) |
| History of unprotected sex | |
| Yes, in the last year | 32 (33) |
| Yes, more than 1 year ago | 37 (39) |
| No | 27 (28) |
| History of intravenous drug use | |
| Yes | 3 (3) |
| No | 92 (96) |
| No response | 1 (1) |
| History of imprisonment | |
| Yes | 7 (7) |
| No | 85 (89) |
| No response | 4 (4) |
| History of STI screening | |
| Yes | 69 (72) |
| No | 25 (25) |
| No response | 3 (3) |
| History of STI diagnosis | |
| None | 84 (88) |
| C. trachomatis alone | 5 (5) |
| N. gonorrhoeae alone | 2 (2) |
| Syphilis alone | 2 (2) |
| Syphilis and hepatitis B | 1 (1) |
| Syphilis and C. trachomatis | 1 (1) |
| Syphilis and N. gonorrhoeae | 1 (1) |
| History of hepatitis B vaccination | |
| Yes | 19 (20) |
| No | 61 (63) |
| Does not know | 16 (17) |
| History of pregnancy at recruitment | |
| Yes | 4 (4) |
| No | 87 (91) |
| Does not know | 5 (5) |
| History of symptoms of STI at recruitment | |
| Yes | 10 (10) |
| No | 85 (89) |
| No response | 1 (1) |
| Willingness to undergo, as part of an STI screening | |
| A throat swab: | |
| – Yes | 61 (64) |
| – No | 35 (36) |
| A vaginal swab: | |
| – Yes | 62 (65) |
| – No | 34 (35) |
| An anal swab: | |
| – Yes | 49 (51) |
| – No | 47 (49) |
| Willingness to pay for an STI screening | |
| 0 USD | 87 (91) |
| Less than 200 USD | 1 (1) |
| Between 200 and 300 USD | 4 (4) |
| More than 300 USD | 4 (4) |
Fifteen (16%; 95%CI 9-23%) female sex workers tested positive for an STI and none had more than one STI (see Table 3). Six (6%) tested positive for C. trachomatis, five (5%; 95% confidence interval [CI] 0.6–9%) for latent syphilis (of unknown time of exposure) and four (4%; 95% CI 0.1–8) for hepatitis B (three chronic active infections and one past exposure). No participants tested positive for HIV, N. gonorrhoeae or hepatitis C. Eleven (11%) female sex workers received antibiotics, three (3%) were sent to an infectious disease specialist for treatment or follow-up and one female sex worker with chronic active hepatitis B was lost to follow-up. Nineteen (20%) participants were already vaccinated against hepatitis B, and 73 participants (76%) initiated the vaccination against hepatitis A and hepatitis B during the study.
Table 3 Prevalence of sexually transmitted infection (STIs) among female sex worker participants – Lausanne, Switzerland, 2015-16.
| Newly confirmed STI diagnosis* |
Participants, no. (%)
(N = 96) |
|---|---|
| Total number of STIs | 15 (16) |
| C. trachomatis infection | 6 (6) |
| Latent syphilis (TPHA positive; RPR negative) | 5 (5) |
| Hepatitis B | 4 (4) |
| – Chronic active hepatitis B infection (HBsAg positive) | 3 (3) |
| – Past exposure to hepatitis B (HBsAg negative; anti-HBc positive) | 1 (1) |
TPHA = Treponema pallidum hemagglutination test; RPR = rapid plasma reagin test * All were also tested for HIV, HCV and N. gonorrhoeae, but all these tests were negative.
Finally, 44 (46%) female sex workers required the support of social workers in the form of translation and social support. The medical and social interventions performed during the study are summarised in table 4.
Table 4 Medical and social interventions provided during the study. The study was performed from 1 April 2015 to 31 December 2016 in Lausanne, Switzerland.
| Intervention |
Participants, no. (%)
(N = 96) |
|---|---|
| Received first dose of a combined vaccine against hepatitis A and hepatitis B | |
| Yes | 73 (76) |
| Not needed | 23 (24) |
| STI treatment provided | |
| Antibiotics | 11 (12) |
| Sent to an infectious disease specialist | 3 (3) |
| Did not receive treatment because lost to follow-up | 1 (1) |
| Translation and social support provided by social workers | |
| Yes | 44 (46) |
| Not needed | 52 (54) |
The prevalence of new STIs among female sex workers in this study was 16% (95% CI 9–23%). None of the female sex workers had more than one STI at a time. Available data among female sex workers are still scarce, and the STI epidemiology in that population seems to vary across Europe, with the highest prevalences of STIs found in Eastern Europe [7]. In the present study, the highest positive test rate was for C. trachomatis infections (6%; 95%CI 1-11%), although one might have expected the prevalence of C. trachomatis among the participants to be higher than this. This rate is similar to the one (6%) documented in 2012 among 1090 females and 80 males less than 31 years old from the general population in the canton of Vaud, Switzerland [18]. One explanation could be that C. trachomatis infection in oropharyngeal and anorectal locations may have been underestimated in our study, as the female sex workers were tested using urine samples only. No N. gonorrhoeae infections were documented in our study sample, whereas the number of new cases reported in the Swiss general population has increased significantly over the last decade (>3000 new cases in 2018, corresponding to an 11% increase compared to the previous year). However, this STI seems to predominantly affect the men who have sex with men population (almost half the new cases reported in Switzerland in 2018 were among men who have sex with men) [19]. We obtained positive test rates of 5% (95% CI 0.6–9%) for syphilis and 4% (95% CI 0.1–8%) for hepatitis B. In the Swiss general population, prevalence estimates for syphilis and HBsAg carriers are respectively <0.02% [20] and 0.3% [21]. All participants in this study were tested for HIV and no female sex workers were newly diagnosed with HIV. Moreover, no participants were known to be HIV positive prior to this study. Platt et al. suggest that injection drug use and having a history of imprisonment, two characteristics that were uncommon in our study, were the main factors statistically associated with HIV seropositivity among female sex workers in Europe (see table 2) [7]. It is worth mentioning that Switzerland is a country with a low prevalence of HIV (0.4%), and the local client population may be at low risk for HIV [22]. While acknowledging the limitations inherent to our study design, it is worth noting the higher positivity rates for syphilis and hepatitis B found in our study sample compared with the prevalence estimates for the Swiss general population. The rates found in our study could be correlated with the prevalences found in many of the countries of origin of the examined female sex workers. In contrast to the national healthcare policies of other European countries such as the Netherlands or Germany, where free access to STI screening is usually provided to groups at high risk for acquiring STIs [1, 5], there is no such national policy in Switzerland. High proportions of the female sex workers in our sample had illegal status and lacked health insurance coverage. This may emphasise the need for local authorities and healthcare decision-makers and stakeholders in Switzerland to address structural barriers, such as access to care, costs for testing and communication barriers, by tailoring easily accessed interventions to the local needs, as advocated by researchers in the field [2, 3]. In our sample, these considerations may be particularly relevant as almost half the female sex workers (46%) required assistance for social support and translation purposes, while only a few of them (9%) would agree to pay for an STI screening.
Less than a third (28%) of female sex workers in this study reported always using condoms with their sexual partners when having oral, vaginal and anal sex. The low percentage of condom use could be because the questionnaire used in this study did not distinguish between oral, anal or vaginal sex. Moreover, we did not distinguish between commercial and non-commercial partners (e.g., intimate, steady partners or spouses), which limits our ability to interpret this figure.
Little is known about vaccine protection against hepatitis B status in the female sex worker population. In our study, only 20% of female sex workers were already vaccinated against hepatitis B at the time of recruitment, and all female sex workers that were not previously immune or infected agreed to initiate vaccination against hepatitis A and B. The decision to propose vaccination against hepatitis B was motivated by the high prevalence of this disease in many of the countries of birth of female sex workers who migrate to Switzerland. Vaccination against hepatitis A also seemed relevant, considering the unprotected oral and anal sexual practices frequently encountered in the female sex worker population [1].
This study is, to our knowledge, the first to investigate the prevalence of six common STIs in the female sex worker population in Switzerland. Other strengths are that the STI screening, hepatitis A and hepatitis B vaccination, and social and translation services were subsidised by local public health authorities, facilitating access to these interventions. In addition, this study tested with success the feasibility of a collaborative approach between local public health authorities, a university hospital and a non-governmental organisation to address the needs of the targeted population regarding STIs. As a result, most of the social and medical interventions proposed in the present study are expected to continue in the future, supported by the stakeholders and decision-makers who were involved in the program.
Limitations include the very small sample size, leading to less precise calculated STI prevalences and thus making comparisons with other studies more difficult. Moreover, our findings cannot be generalised to other areas of Switzerland, as female sex workers’ sociodemographic characteristics and the legal regulations regarding sex work are region-dependent and may change over time [12, 23]. Also, the female sex workers included in this study may be different from other female sex workers in Lausanne who were not approached or were not interested in participating in the study. For practical and organisational reasons, we were unable to document the proportion and characteristics of the female sex workers who were approached but were not interested in participating in the study. Therefore, our study sample is likely to be a very selective study population due to selection bias in the recruitment of participants. We can reasonably assume that many female sex workers did not access our programme because of one or more personal or structural obstacles (e.g., stigmatisation of the work, fear of the authorities, social isolation, financial difficulties, limitations in communication, etc.). It may be difficult to estimate the extent of this problem because of the persistent marginalisation of that population (e.g., many female sex workers still work without declaring their activities to the local authorities). The circumstances of the recruitment to the study were also not optimal: female sex workers were approached in the streets or in the bus by the Fleur de Pavé organisation during their routine work at night, i.e., between clients. Some illegal female sex workers expressed concerns about being exposed to the local authorities or the police, whereas other female sex workers mentioned that health problems were currently not their top priority. Contacts between female sex workers and Fleur de Pavé’s social workers were numerous, but the vast majority were very brief, as in most cases the female sex workers were seeking brief information or the shelter of Fleur de Pavé’s bus, where they could rest for a short period of time. Another potential limitation is that the setting where the tests were provided, i.e., a tertiary care unit (university hospital), could potentially be a very inaccessible place for marginalised persons, resulting in another selection bias. Moreover, male and transgender sex workers were not included, but their vulnerability to STI acquisition and transmission has been recognised in some parts of the world [4, 24]. Finally, the real impact of STIs in the female sex worker population may have been underestimated as we tested for C. trachomatis and N. gonorrhoeae using urine samples only. The reasons why we decided to collect urine samples only were: (1) the reluctance that female sex workers might have had regarding more invasive sampling methods (e.g. vaginal or anal swabs); (2) the difficulties in drawing valid conclusions from the results if the sampling was performed according to the female sex workers’ preferred method. A majority, but not all the female sex workers in this study said they would agree to receive oropharyngeal, vaginal and anal swabs for STI screening, with the anal sampling being the least accepted method.
In our study, the prevalences of latent syphilis and hepatitis B in female sex workers were 5% and 4% respectively, while the prevalence of C. trachomatis (6%) may have been underestimated in our sample. No HIV infections were newly diagnosed among the participants. Most of the studied female sex workers were not protected against hepatitis B. Social deprivation and vulnerability were frequently encountered among participants: about 75% were uninsured and half the migrant female sex workers required support in the form of translation and social support. From a public health perspective, the results of the present study support the development of multidisciplinary programmes aimed at delivering more comprehensive services tailored to the social and medical needs of the female sex worker population.
The authors would like to thank the nurses and the financial and administrative staff of the STI and HIV consultation, as well as the social workers of the Fleur de Pavé organisation, for their substantial contributions to the acquisition and management of the data.
Financial support was received from the Department of Public Health in the canton of Vaud, Switzerland, to help with costs for screening tests and vaccines, as well as for the translation and social support. The funding source had no involvement in the study design; the collection, analysis and interpretation of data; the writing of the report; or the decision to submit the article for publication.
No conflict of interest was declared.
1 Verscheijden MMA , Woestenberg PJ , Götz HM , van Veen MG , Koedijk FDH , van Benthem BHB . Sexually transmitted infections among female sex workers tested at STI clinics in the Netherlands, 2006-2013. Emerg Themes Epidemiol. 2015;12(1):12. doi:.https://doi.org/10.1186/s12982-015-0034-7
2 Shannon K , Strathdee SA , Goldenberg SM , Duff P , Mwangi P , Rusakova M , et al. Global epidemiology of HIV among female sex workers: influence of structural determinants. Lancet. 2015;385(9962):55–71. doi:.https://doi.org/10.1016/S0140-6736(14)60931-4
3 Bekker LG , Johnson L , Cowan F , Overs C , Besada D , Hillier S , et al. Combination HIV prevention for female sex workers: what is the evidence? Lancet. 2015;385(9962):72–87. doi:.https://doi.org/10.1016/S0140-6736(14)60974-0
4 Beyrer C , Crago AL , Bekker LG , Butler J , Shannon K , Kerrigan D , et al. An action agenda for HIV and sex workers. Lancet. 2015;385(9964):287–301. doi:.https://doi.org/10.1016/S0140-6736(14)60933-8
5 Bremer V , Haar K , Gassowski M , Hamouda O , Nielsen S . STI tests and proportion of positive tests in female sex workers attending local public health departments in Germany in 2010/11. BMC Public Health. 2016;16(1):1175. doi:.https://doi.org/10.1186/s12889-016-3847-6
6 Almeida A , Brasileiro A , Costa J , Eusébio M , Fernandes R . Prevalence of and factors mediating HIV infection among sex workers in Lisbon, Portugal: the 5-year experience of a community organisation. Sex Transm Infect. 2014;90(6):497. doi:.https://doi.org/10.1136/sextrans-2014-051523
7 Platt L , Jolley E , Rhodes T , Hope V , Latypov A , Reynolds L , et al. Factors mediating HIV risk among female sex workers in Europe: a systematic review and ecological analysis. BMJ Open. 2013;3(7):e002836. doi:.https://doi.org/10.1136/bmjopen-2013-002836
8 Zermiani M , Mengoli C , Rimondo C , Galvan U , Cruciani M , Serpelloni G . Prevalence of sexually transmitted diseases and hepatitis C in a survey of female sex workers in the north-East of Italy. Open AIDS J. 2012;6(1):60–4. doi:.https://doi.org/10.2174/1874613601206010060
9 Mak RP , Van Renterghem L , Traen A . Chlamydia trachomatis in female sex workers in Belgium: 1998-2003. Sex Transm Infect. 2005;81(1):89–90. doi:.https://doi.org/10.1136/sti.2004.010272
10 Mak R , Van Renterghem L , Cuvelier C . Cervical smears and human papillomavirus typing in sex workers. Sex Transm Infect. 2004;80(2):118–20. doi:.https://doi.org/10.1136/sti.2002.003749
11 Marek E , Dergez T , D’cruz G , Bozsa S , Cseh A , Szilard I , et al. Human papillomavirus infections among Hungarian female sex workers. Eur J Cancer Care (Engl). 2014;23(1):65–75. doi:.https://doi.org/10.1111/ecc.12110
12Bugnon G, Chimienti M, Chiquet L. Marché du sexe en Suisse. Etat des connaissances, best practices et recommandations. Volet 2 – Cadre légal. Département de sociologie. Geneva: Université de Genève; 2009.
13Swiss Federal Office of Public Health (FOPH). National Programme on HIV and other STI (NPHS) 2011–2017. Bern: Federal Office of Public Health; 2010.
14Wetzel D, With S, Durieux S. Mise en place d'une consultation d'information sur les IST et de dépistage du VIH pour les personnes exerçant la prostitution à Genève. Rapport d'activité de la phase pilote Novembre 2011-Mai 2013. 2013.
15Département des finances et des relations extérieures du canton de Vaud. Population résidente dans l'agglomération lausannoise, 1980-2014. Accessed on the web on May 30 2017: www.scris.vd.ch/Data_Dir/ElementsDir/3820/15/F/i99.01.02.xls.
16 Greub G , Sahli R , Brouillet R , Jaton K . Ten years of R&D and full automation in molecular diagnosis. Future Microbiol. 2016;11(3):403–25. doi:.https://doi.org/10.2217/fmb.15.152
17 Jaton K , Bille J , Greub G . A novel real-time PCR to detect Chlamydia trachomatis in first-void urine or genital swabs. J Med Microbiol. 2006;55(12):1667–74. doi:.https://doi.org/10.1099/jmm.0.46675-0
18 Bally F , Quach A , Greub G , Jaton K , Petignat C , Ambord C , et al. Opportunistic testing for urogenital infection with Chlamydia trachomatis in south-western Switzerland, 2012: a feasibility study. Euro Surveill. 2015;20(9):21051. doi:.https://doi.org/10.2807/1560-7917.ES2015.20.9.21051
19Office Fédéral de la Santé Publique (OFSP). Bulletin 41 du 7 octobre 2019. VIH, syphilis, gonorrhée et chlamydiose en Suisse en 2018: survol épidémiologique. Bern: Office Fédéral de la Santé Publique; 2019.
20Office Fédéral de la Santé Publique (OFSP). Bulletin 46 du 14 novembre 2016. VIH, syphilis, gonorrhée et chlamydiose en Suisse en 2015: survol épidémiologique. BAG-Bulletin 46 du 14 novembre 2016. Bern: Office Fédéral de la Santé Publique; 2016. pp. 12–36.
21 Fretz R , Negro F , Bruggmann P , Lavanchy D , De Gottardi A , Pache I , et al. Hepatitis B and C in Switzerland - healthcare provider initiated testing for chronic hepatitis B and C infection. Swiss Med Wkly. 2013;143:w13793. doi:.https://doi.org/10.4414/smw.2013.13793
22 Darling KE , Diserens EA , N’garambe C , Ansermet-Pagot A , Masserey E , Cavassini M , et al. A cross-sectional survey of attitudes to HIV risk and rapid HIV testing among clients of sex workers in Switzerland. Sex Transm Infect. 2012;88(6):462–4. doi:.https://doi.org/10.1136/sextrans-2012-050489
23Bugnon G, Chimienti M, Chiquet L. Marché du sexe en Suisse. Etat des connaissances, best practices et recommandations. Volet 3 – Mapping, contrôle et promotion de la santé dans le marché du sexe en Suisse. Geneva: Université de Genève; 2009.
24 Baral SD , Friedman MR , Geibel S , Rebe K , Bozhinov B , Diouf D , et al. Male sex workers: practices, contexts, and vulnerabilities for HIV acquisition and transmission. Lancet. 2015;385(9964):260–73. doi:.https://doi.org/10.1016/S0140-6736(14)60801-1
All authors read and agreed to the content of the present paper.
Financial support was received from the Department of Public Health in the canton of Vaud, Switzerland, to help with costs for screening tests and vaccines, as well as for the translation and social support. The funding source had no involvement in the study design; the collection, analysis and interpretation of data; the writing of the report; or the decision to submit the article for publication.
No conflict of interest was declared.