COVID-19 and cardiovascular disease: what have we learned?
DOI: https://doi.org/10.4414/smw.2020.20452
Elena
Tessitore, Philippe
Meyer
Cardiology Service, Geneva University Hospitals, Geneva, Switzerland
At the very beginning of 2020, before coronavirus disease 2019 (COVID-19) had officially reached Europe, the first data describing the clinical features of patients with COVID-19 were published [1, 2]. Patients with hypertension, diabetes or any pre-existing cardiovascular disease were then considered at risk for severe infections [2]. Acute cardiac injury, present in 12% of patients [1], was interpreted by many clinicians as acute myocarditis. Finally, caution was recommended regarding the use of renin-angiotensin-aldosterone system (RAAS) inhibitors, since coronaviruses were already known to enter host cells via angiotensin-converting enzyme 2 (ACE2) receptor binding [3].
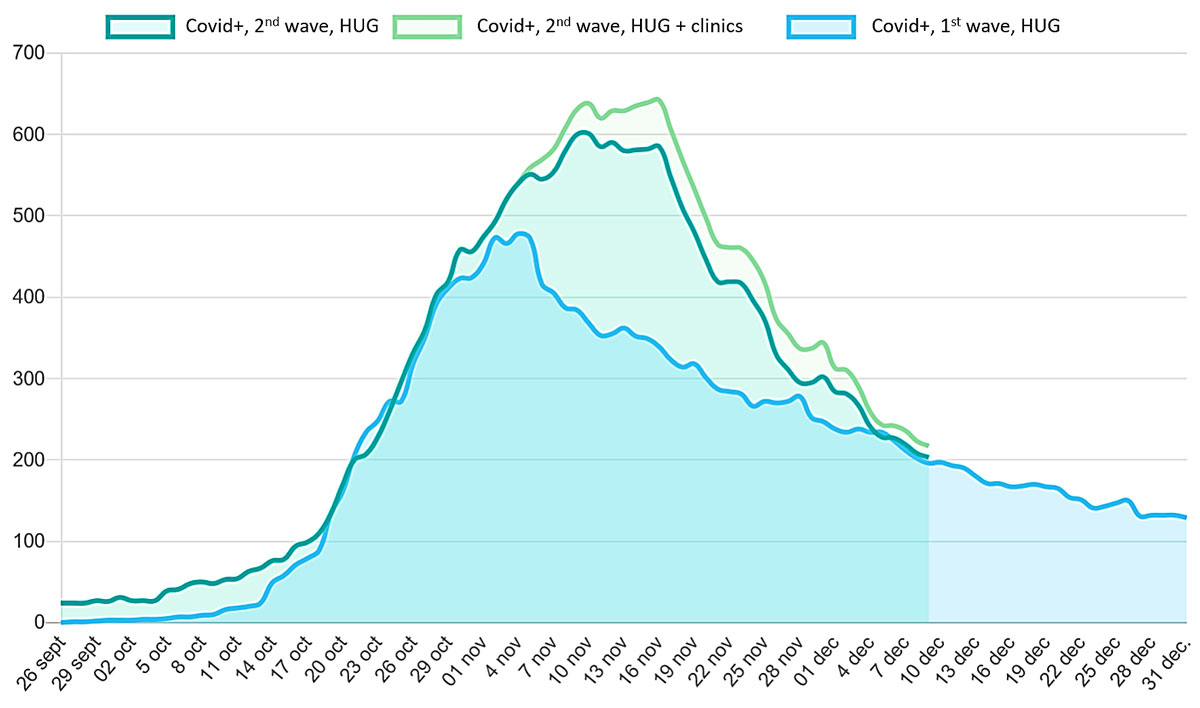
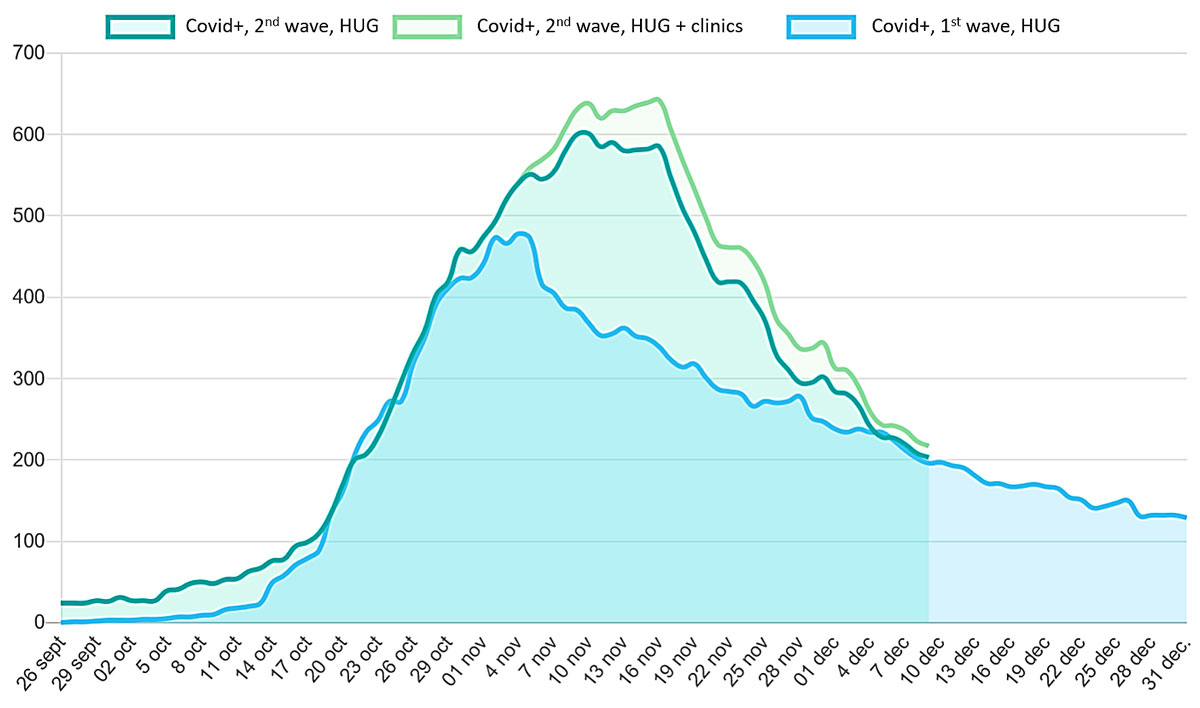
After the first reported case in Switzerland on 25 February 2020, the COVID-19 epidemic spread rapidly in our country, reaching the highest reported cumulative prevalence per head of population in the world in March. The Geneva canton was severely hit and initially the Geneva University Hospitals (HUG) were selected as the only COVID-19 referral centre in the region. During the first wave, the COVID-19 peak hospitalisation number was 478, with a peak of 67 intubated patients. Since October, we are facing even a bigger second wave and Geneva is again one of the most severely affected region in Europe (fig. 1), with a peak of 642 hospitalisations on 16 November 2020 and a peak of 32 intubated patients [4]. As of 10 December, a total of 605 cumulative deaths due to COVID-19 have been reported in the Geneva canton [5].
Since the beginning of the pandemic, an unprecedented number of scientific papers on COVID-19 have been published in frenetic agitation, with record times between submission and publication, sometimes at the expense of lesser research quality standards [6]. As of 10 December, 82,127 citations were found in PubMed on COVID-19 and 5285 when “COVID-19 and cardiovascular disease” were used as search words. Many cardiovascular societies have also released statements regarding COVID-19. The European Society of Cardiology has notably published a 98-page guidance document (excluding the reference section containing 276 citations) [7].
What have we learned from this incredible scientific excitement?
In an article now published in Swiss Medical Weekly, two cardiologists from the Triemli Hospital in Zurich, PD Dr. med. David Kurz and Professor Franz Robert Eberli give a comprehensive overview of current evidence about cardiovascular aspects of COVID-19, including the interactions with the RAAS, the impact of pre-existing cardiovascular disease, and cardiovascular consequences of the infection [8].
For our clinical practice, the most important messages regarding COVID-19 and cardiovascular disease can be summarised as follows:
- Male gender, advanced age and multi-morbidity are now universally considered as predictors of severe infections, but a single cardiovascular comorbidity, such as chronic ischaemic heart disease or atrial fibrillation does not seem to have such an impact [9].
- Angiotensin converting-enzyme inhibitors and angiotensin II receptor blockers can be continued without any hesitation as a regular treatment in patients with COVID-19 [10].
- Myocardial injury defined by increased cardiac troponin can be observed in about one fifth of patients, depending on COVID-19 severity, and reflects mainly various non-ischaemic myocardial processes, whereas confirmed myocarditis or true (type I) myocardial infarction have been very rarely reported [11].
However several questions remain still unsolved and currently under investigation, such as:
- Could RAAS inhibitors actually be protective in patients with COVID-19?
- Exactly what role does heart failure play in the COVID-19 pandemic?
- Are there any long-term consequences of COVID-19 on the cardiovascular system?
Finally, the figure accompanying this editorial begs another much broader and more urgent question: why have we so miserably failed to counter this second wave?
Author contributions
The two authors participated in writing and approved of the final manuscript.
References
1
Huang
C
,
Wang
Y
,
Li
X
,
Ren
L
,
Zhao
J
,
Hu
Y
, et al.
Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:.https://doi.org/10.1016/S0140-6736(20)30183-5
2
Wang
D
,
Hu
B
,
Hu
C
,
Zhu
F
,
Liu
X
,
Zhang
J
, et al.
Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–9. doi:.https://doi.org/10.1001/jama.2020.1585
3
Fang
L
,
Karakiulakis
G
,
Roth
M
. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?
Lancet Respir Med. 2020;8(4):e21. doi:.https://doi.org/10.1016/S2213-2600(20)30116-8
4
http://www.intrahug.ch/groupes/coronavirus-de-la-maladie-covid-19/group-news/covid-19-situation.
5
https://infocovid.smc.unige.ch.
6
Bramstedt
KA
. The carnage of substandard research during the COVID-19 pandemic: a call for quality. J Med Ethics. 2020;46(12):803–7. doi:.https://doi.org/10.1136/medethics-2020-106494
7
https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance.
8
Kurz
D
,
Eberli
FR
. Cardiovascular aspects of COVID-19. Swiss Med Wkly. 2020;150:w20417. doi:https://doi.org/10.44414/smw.2020.20417
9
Phelps
M
,
Christensen
DM
,
Gerds
T
,
Fosbøl
E
,
Torp-Pedersen
C
,
Schou
M
, et al.
Cardiovascular comorbidities as predictors for severe COVID-19 infection or death. Eur Heart J Qual Care Clin Outcomes. 2020;qcaa081. doi:.https://doi.org/10.1093/ehjqcco/qcaa081
10
de Abajo
FJ
,
Rodríguez-Martín
S
,
Lerma
V
,
Mejía-Abril
G
,
Aguilar
M
,
García-Luque
A
, et al.; MED-ACE2-COVID19 study group. Use of renin-angiotensin-aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study. Lancet. 2020;395(10238):1705–14. doi:.https://doi.org/10.1016/S0140-6736(20)31030-8
11
Sandoval
Y
,
Januzzi
JL, Jr
,
Jaffe
AS
. Cardiac Troponin for Assessment of Myocardial Injury in COVID-19: JACC Review Topic of the Week. J Am Coll Cardiol. 2020;76(10):1244–58. doi:.https://doi.org/10.1016/j.jacc.2020.06.068