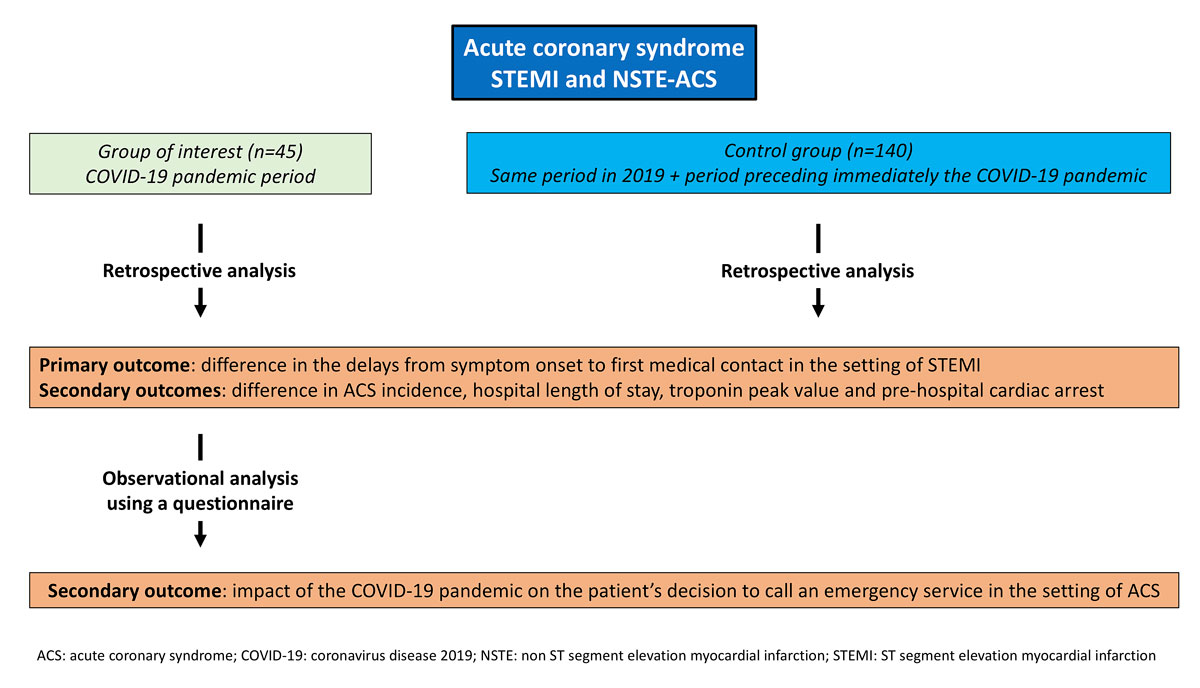
Figure 1 Study flowchart
DOI: https://doi.org/10.4414/smw.2020.20448
Coronavirus disease 2019 (COVID-19) is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and has been the cause of an unprecedented worldwide healthcare challenge. In early March 2020, the World Health Organization classified the disease as a pandemic [1] and strict social containment measures were implemented in most European countries to limit its spread [1]. On 13 March 2020, the Swiss Federal Council imposed nationwide measures to reduce the risk of COVID-19 transmission [2], including the cancellation of all non-urgent medical and surgical interventions [2]. Within Switzerland, the Geneva canton was among the most impacted by the disease [3].
The management of medical emergencies, such as ST-segment elevation myocardial infarction (STEMI), may have been affected at multiple levels by the COVID-19 pandemic, including an increase in patients’ threshold to calling emergency medical services, decreased availability of ambulances, increased waiting time in the emergency departments, and time delay in percutaneous coronary intervention (PCI) due to the implementation of personal protective measures [4]. In addition, a decrease in hospital admissions for acute coronary syndromes (ACS) in regions highly affected by COVID-19 has been reported[5].
Therefore, we hypothesised that changes in the perception of urgent care during the COVID-19 pandemic increased the delay between symptom onset and first medical contact in patients with STEMI. Moreover, we wanted to investigate whether people’s fear of getting infected or to inappropriately overloading the emergency departments would affect the decision to call emergency medical services during the first wave of the pandemic. Thus, we planned to assess whether the delay from symptom onset to first medical contact increased among patients treated for STEMI at the Geneva University Hospitals during the peak of the COVID-19 pandemic. In addition, we investigated whether there were COVID-19-related reasons for delaying first medical contact. Finally, we assessed whether there was a change in the incidence of ACS patients undergoing PCI during the first wave of the COVID pandemic.
The study was investigator-initiated and divided into two parts (fig. 1). The first part consisted of a retrospective analysis of inpatient data and the second part was an observational analysis using a questionnaire. The protocol was submitted and accepted by the local ethics committee.
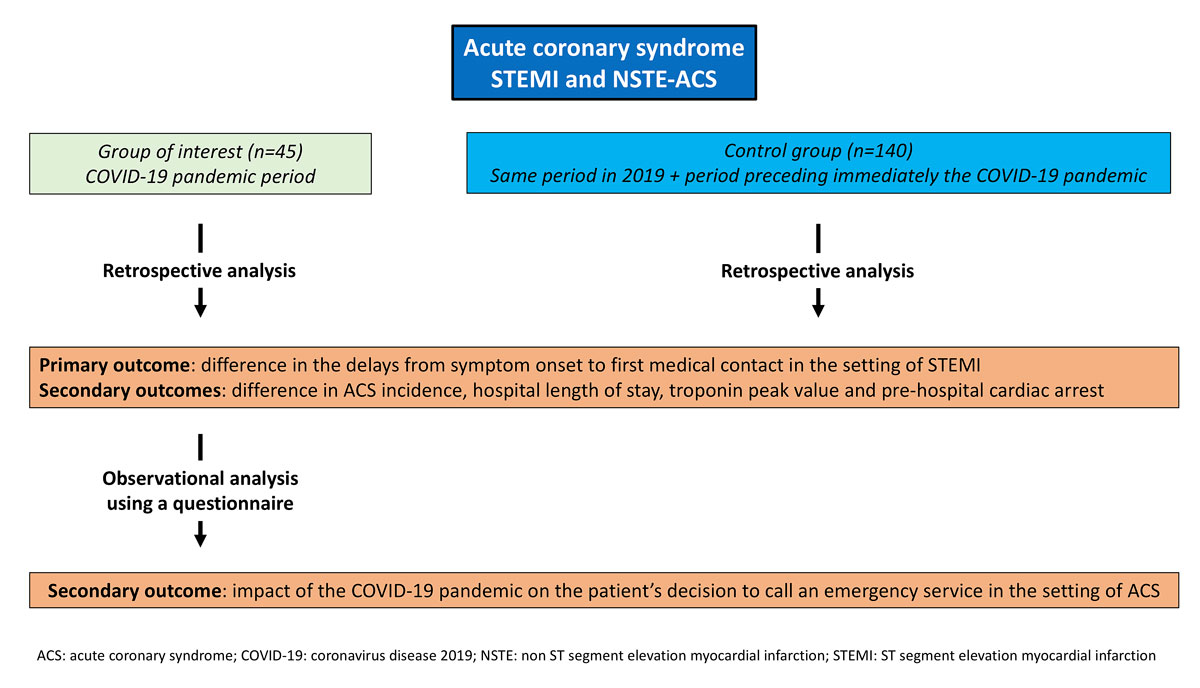
Figure 1 Study flowchart
All patients treated at the Geneva University Hospitals with PCI for ACS, as defined by European Society of Cardiology [6, 7], during one of the three periods of interest were included in the retrospective analysis (fig. 1). For the purpose of this study, the first wave of the COVID-19 pandemic, described hereafter as the COVID-19 period, was defined as the time from 13 March 2020 (the day on which the Swiss Federal Council imposed nationwide measures to be implemented to reduce the risk of transmission of this disease) to 30 April 2020, which corresponded to the end of the acute phase of COVID-19 hospitalisations. During this period, the prevalence of COVID-19 was at its highest, as were the social restrictive measures dictated by the Swiss Federal Council. As a consequence, all non-urgent medical and surgical interventions at Geneva University Hospitals were cancelled or postponed. The control periods were defined as the same period in 2019 (13 March to 30 April 2019) and a same length period immediately preceding the first diagnosed case of COVID-19 in Switzerland (7 January to 24 February 2020). Acute myocardial infarction incidence during these two time periods should not have been significantly impacted by seasonal variation as only a slight non-significant reduction in incidence between winter and spring is reported [8–10]. According to their clinical presentation, patients were divided into STEMI and non-ST-elevation ACS (NSTE-ACS).
Only patients included in the COVID-19 period who signed and returned the written informed consent form were included in the second observational part of the study (fig. 1).
Baseline and study-related characteristics were retrospectively collected from the patients’ hospital electronic medical records. Delays from symptom onset to first medical contact were derived either from the pre-hospital intervention forms or the emergency department medical records.
In order to assess the impact of the COVID-19 pandemic on the patient’s decision to call an emergency service, we used a questionnaire (appendix 1) completed directly by the patient and addressing three main points:
Answers to the questions were rated according to the Likert scale to measure the degree to which patients agreed or disagreed with the statement. To quantify anxiety and depression, we used the validated Hospital Anxiety and Depression Scale (HADS) [11], referring to the seven days preceding the start of the ACS symptoms. Briefly, this score is composed of 14 questions separated into 7 questions related to anxiety symptoms and 7 questions to depression. For each of the two parts, patients with a score of less or equal to 7 points are considered as asymptomatic, between 8 and 10 points as borderline, and more or equal than 11 points as symptomatic. Patients who did not return the completed questionnaire after a delay of 4 weeks were contacted by telephone and encouraged to do so. Questions were not asked by telephone because the score has not been validated in that setting.
The primary outcome measure was delay from symptom onset to first medical contact in the setting of STEMI during the COVID-19 period as compared with the control period. This delay was not assessed for NSTE-ACS patients because of the difficulty in determining symptom onset as well as the lack of impact of this parameter on outcomes in this patient population. Time from symptom onset to first medical contact was defined as the time of onset of chest discomfort or other ACS-related symptoms, as reported by the patient, to first medical contact. Based on this measure, STEMI patients were divided into early (<6 hours), delayed (between 6–12 hours) and late (>12 hours) presenters.
Secondary outcome measures included the difference in ACS incidence between the COVID-19 period and the control period, and the impact of the COVID-19 pandemic on the patient’s decision to call emergency services, evaluated using the questionnaire described above. After excluding the patients who were transferred to another hospital following revascularisation or those presenting their highest troponin value in the initial blood sample, we also analysed the hospital length of stay and troponin peak value. Peak troponin value was defined as the maximum troponin value when this value was preceded and followed by a lower value. High sensitive cardiac troponin assays were used.
Normally distributed variables are presented as means ± standard deviations and differences compared using the Student’s t-test. Non-normally distributed variables are presented as medians (interquartile ranges [IQRs]) and differences are compared using the Wilcoxon rank-sum test, as appropriate. Categorical data are expressed as numbers and frequencies (%) and compared using the Fisher’s exact test or Pearson’s chi-square test as appropriate. The incidence of ACS is presented as daily new admissions during the COVID-19 and control period and was calculated by dividing the number of ACS patients by the number of days in each period of interest. Incidence rates are expressed per 1000 person-years assuming a population of 500,000 inhabitants for Geneva. Incidence rate ratios were calculated between the active and the control period.
Of the 45 patients admitted for an ACS at the Geneva University Hospitals during the COVID-19 period, 20% were females; the mean age was 63.8 ± 9.2 years. Two thirds of the patients presented typical chest pain. Baseline characteristics are presented in table 1. There was no statistically significant difference in terms of baseline characteristics of ACS patients between the COVID-19 period (n = 45) and the control period (n = 140). The supplementary tables S1–S3 in appendix 2 present the control group divided into two periods comprising the same period in 2019 and the period immediately preceding the first case of COVID-19 in Switzerland.
Table 1 Baseline characteristics of all acute coronary syndrome patients. Values are presented as mean (± standard deviation) or number (percentage).
|
COVID-19
n = 45 |
Pre-COVID-19
n = 140 |
p-value | |
|---|---|---|---|
| Age | 63.8 ± 11.6 | 68.0 ± 13.9 | 0.07 |
| Female | 9 (20.0) | 35 (25.0) | 0.5 |
| BMI | 26.9 ± 3.8 | 26.4 ± 4.6 | 0.6 |
| Smoking (past or active) | 17 (37.8) | 50 (35.7) | 0.8 |
| Diabetes | 10 (22.2) | 44 (31.4) | 0.2 |
| Hypertension | 18 (40.0) | 76 (54.3) | 0.08 |
| Dyslipidaemia | 12 (26.7) | 58 (41.4) | 0.08 |
| Prior PCI | 8 (17.8) | 11 (7.9) | 0.06 |
| Prior CABG | 1 (2.3) | 1 (0.7) | 0.4 |
| Typical chest pain | 29 (65.9) | 105 (75.0) | 0.2 |
| SARS-CoV-2 tested/positive | 32 (71.1)/4 (8.9) | - | - |
BMI = body mass index; CABG = coronary artery bypass graft; PCI = percutaneous coronary intervention; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2.
Results are for the entire ACS population as well as stratified according to STEMI or NSTE-ACS presentation (tables 2, 3 and 4 ). The median delay from symptom onset to first medical contact was significantly longer among patients suffering from a STEMI in the COVID-19 period than the control period (112 min vs 60 min, p = 0.049), with data available in 94.0% and 83.3% of the patients, respectively. Delayed (between 6 and 12 hours) or late (>12 hours) presentations were reported in 18.2% and 9% of patients in the COVID-19 and control periods, respectively (p = 0.3) (fig. 2). The incidence rate of ACS was lower during the COVID-19 period than the control period (0.7 vs 1.1 per 1000 person-years, p <0.01) with an incidence rate ratio of 0.6 (95% confidence interval [CI] 0.449–0.905). This difference was driven by lower incidence rates among NSTE-ACS patients (incidence rate ratio 0.324, 95% CI 0.160–0.601) during the COVID-19 period, with no difference in incidence rates among STEMI patients (incidence rate ratio 1, 95% CI 0.638–1.541).
Table 2 Outcome measures in all acute coronary syndromes patients. Values are presented as medians (interquartile ranges), numbers (percentage) and ratios.
|
COVID-19
n = 45 |
Pre-COVID-19
n = 140 |
p-value | |
|---|---|---|---|
| LVEF (%) | 55 (43–60) | 50 (40–60) | 0.70 |
| Peak hs-cTn (ng/l) | 2247 (975–5200) | 1076 (402–3799) | 0.02 |
| Hospital LoS (days) | 6 (5–7) | 7 (5–11) | 0.03 |
| Out-of-hospital cardiac arrest | 10 (22.2) | 10 (7.1) | <0.01 |
| Number of daily admissions | 0.9 | 1.5 | – |
| Incidence rate for 1000 person-years | 0.7 | 1.1 | <0.01 |
hs-cTn= highly sensitive cardiac troponin; LoS = length of stay; LVEF left ventricular ejection fraction
Table 3 Outcome measures in ST-segment elevation myocardial infarction patients. Values are presented as medians (interquartile ranges), numbers (percentage) and ratios.
|
COVID-19
n = 33 |
Pre-COVID-19
n = 66 |
p-value | |
|---|---|---|---|
| Symptom onset to first medical contact (minutes) | 112 (16–211) | 60 (20–165) | 0.049 |
| LVEF (%) | 53 (37–59) | 48 (40–58) | 0.68 |
| Peak hs-cTn (ng/l) | 4102 (1684–6108) | 3753 (1509–8960) | 0.84 |
| Hospital LoS (days) | 6.5 (5–7) | 7 (6–12) | 0.02 |
| Out-of-hospital cardiac arrest | 9 (27.2) | 9 (13.6) | 0.10 |
| Number of daily admissions | 0.7 | 0.7 | – |
| Incidence rate for 1000 person-years | 0.5 | 0.5 | 1.0 |
hs-cTn = highly sensitive cardiac troponin; LoS = length of stay; LVEF = left ventricular ejection fraction
Table 4 Outcome measures in non-ST-segment elevation-acute coronary syndrome patients. Values are presented as medians (interquartile ranges), numbers (percentage) and ratios.
|
COVID-19
n = 12 |
Pre-COVID-19
n = 74 |
p-value | |
|---|---|---|---|
| LVEF (%) | 58 (52–62) | 55 (45–63) | 0.42 |
| Peak hs-cTn (ng/l) | 1137 (764–2090) | 502 (213–1059) | 0.02 |
| Hospital LoS (days) | 5.5 (5–8) | 7 (4–10) | 0.42 |
| Out-of-hospital cardiac arrest | 1 (8.3) | 1 (1.4) | 0.11 |
| Number of daily admissions | 0.3 | 0.8 | – |
| Incidence rate for 1000 person-year | 0.2 | 0.6 | <0.01 |
hs-cTn = highly sensitive cardiac troponin; LoS = length of stay; LVEF = left ventricular ejection fraction
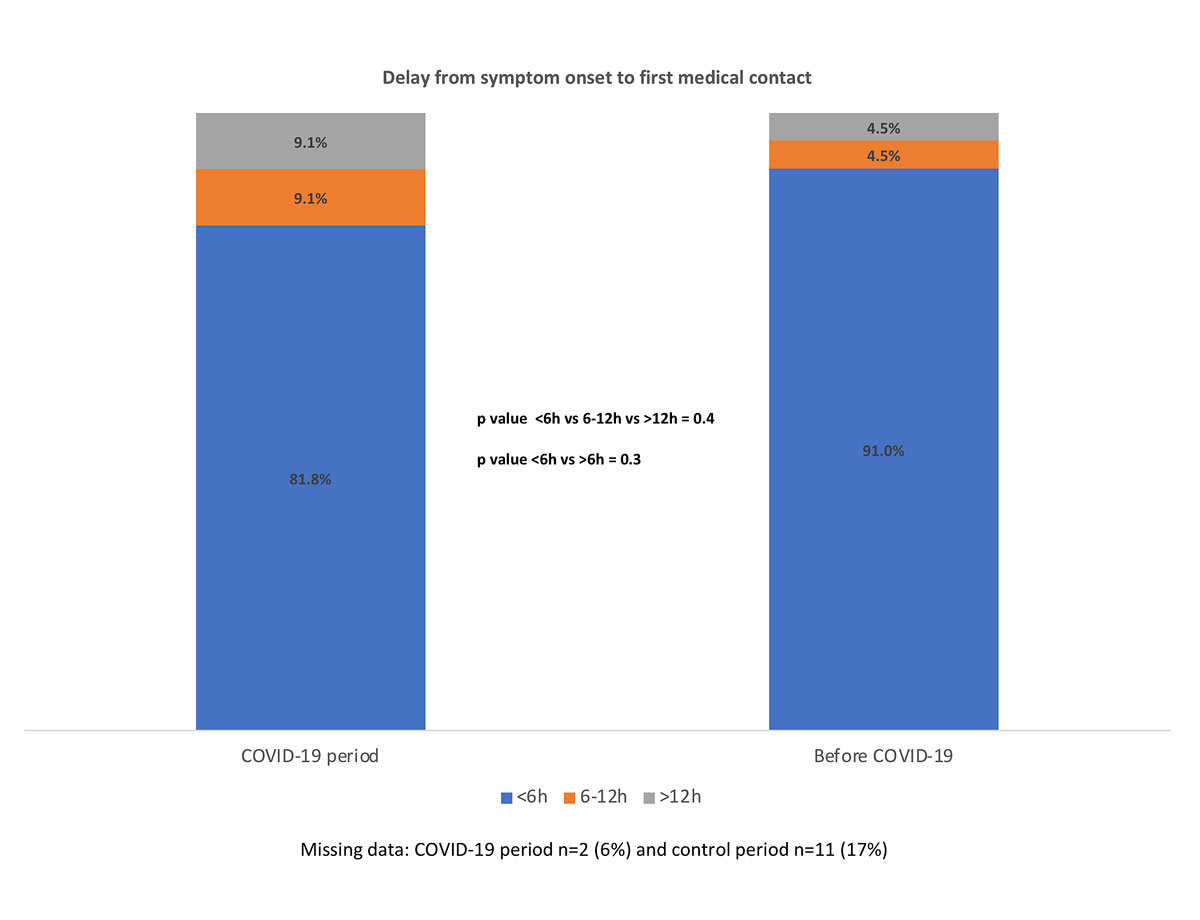
Figure 2 Delay from symptom onset to first medical contact.
We observed significantly more patients presenting with out-of-hospital cardiac arrest during the COVID-19 period compared with the control period (22.2% vs 7.1%, p <0.01). The median peak value of troponins in the overall ACS population was higher among patients in the COVID-19 period (data available for 73% of patients) than those in the control period (data available for 98% of the patients) (2247 ng/l, IQR 975–5200 vs 1076 ng/l, IQR 402–3799, p = 0.02), mostly driven by a significant difference in the NSTEMI patients (1137 ng/l, IQR 764–2090 vs 502 ng/l, IQR 213–1059, respectively, p = 0.02).
Among surviving ACS patients of the COVID-19 period, 18 (43%) returned the questionnaire and signed the written informed consent form. Eleven (61% of the respondents) did not recognise their symptoms as those of an acute myocardial infarction. None of the patients reported difficulty in reaching their family doctor as a cause of delaying their medical care. Six patients (33%) delayed their call to the emergency services because of fear of contracting or spreading the COVID-19 or fear of adding additional work to the healthcare system. Among them, four patients (22%) were afraid of contracting the SARS-COV-2 and four (22%) were afraid of spreading the disease to a relative in the event of hospital admission. Five patients (28%) delayed their call to the emergency services because of fear of adding additional work to a healthcare system already burdened by the pandemic (fig. 3). The median HADS score was 3.5 (IQR 2.0–7.5) for anxiety and 3 (IQR 1.0–5.5) for depression. Among the respondents, 27.8% and 22.2% presented at the least borderline features of anxiety or depression, respectively (fig. 4). There was no difference between respondents and non-respondents in baseline characteristics (with the exception of significantly more diabetes in the non-respondent group) or in terms of time delays in STEMI patients, left ventricular ejection fraction, troponin peak value or hospital length of stay (tables S4 and S5 in appendix 2).
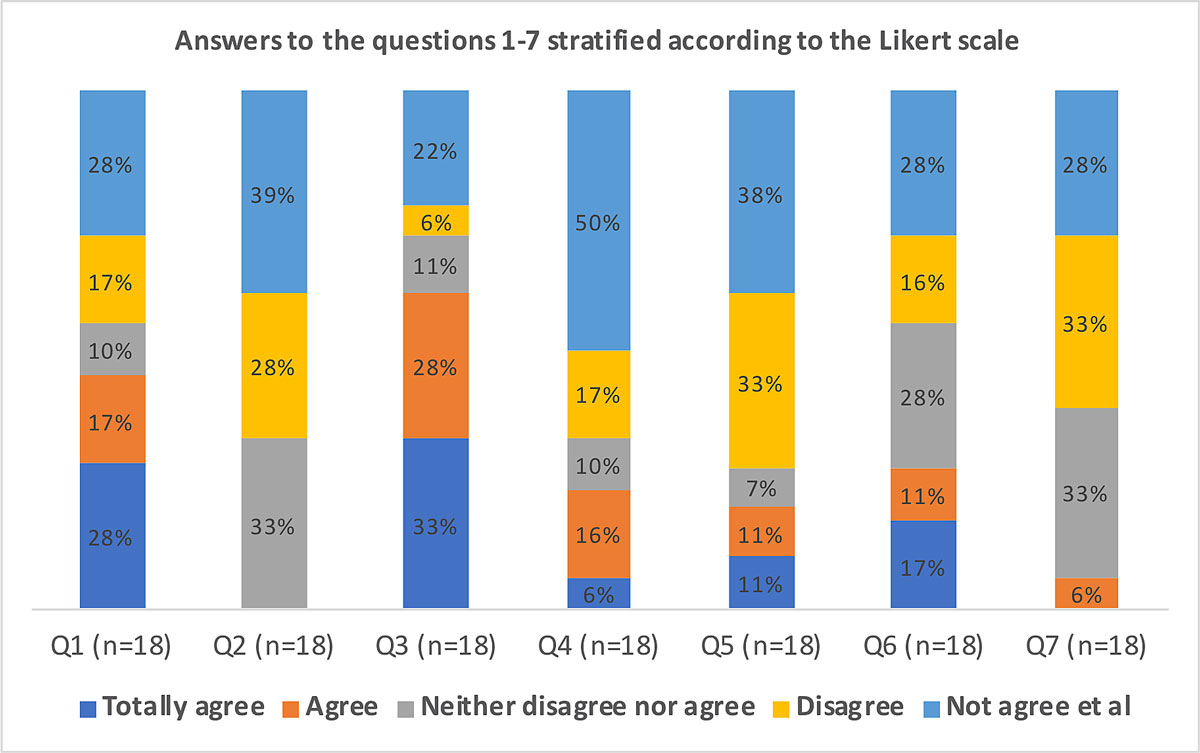
Figure 3 Answers to the questions 1–7 according to the Likert scale.
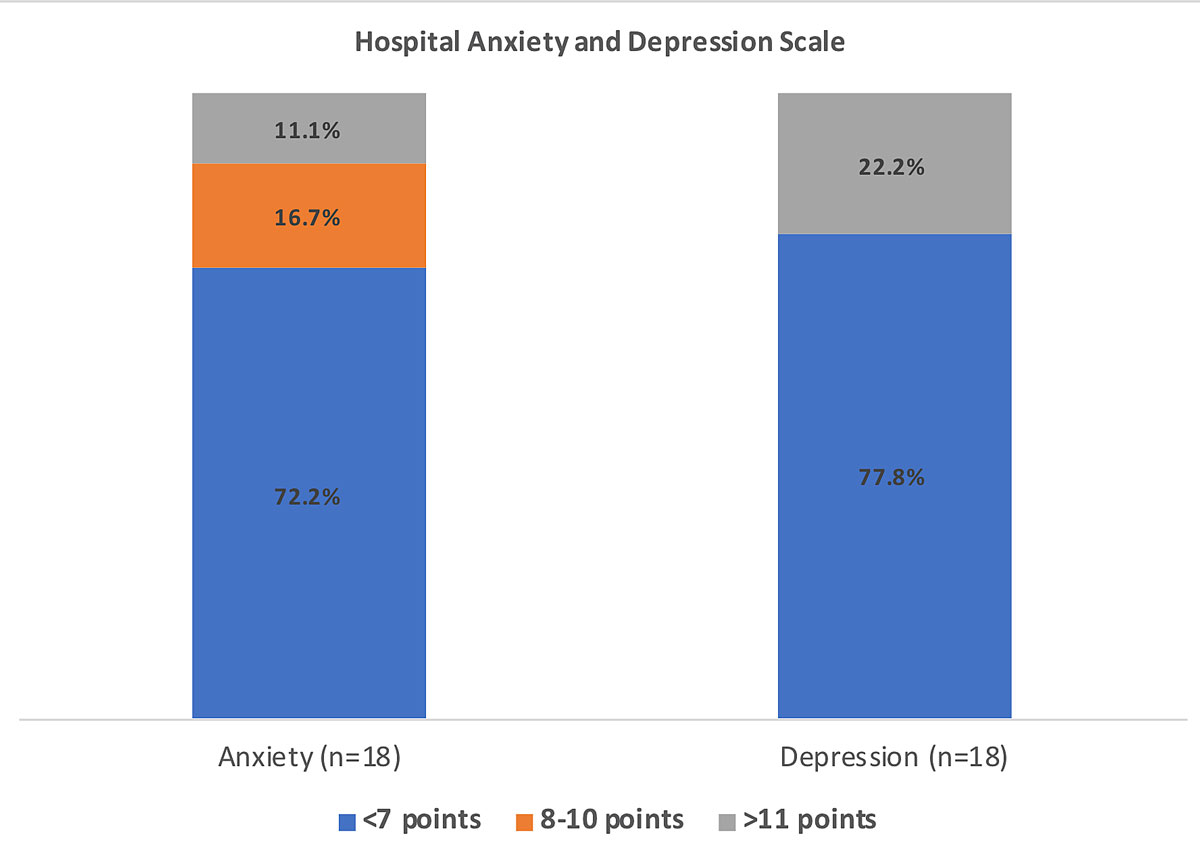
Figure 4 Hospital Anxiety and Depression Scale (HADS).
Among patients who spent the entire acute hospitalisation in our centre (78% and 95% in the COVID-19 period vs control period, respectively), hospital length of stay was statistically significantly shorter for the COVID-19 period as compared to the control period (6 vs 7 days, p = 0.03).
The main findings of the present study are:
Timely myocardial revascularisation in the context of STEMI is one of the pillars of treatment to improve patient outcomes [7], and a prolonged time to hospital admission has been associated with increased in-hospital mortality [12]. Therefore, great efforts have been made to reduce as much as possible pre-hospital and intra-hospital delays by implementing locally validated STEMI protocols. Patient might contribute to increased pre-hospital delays as a result of lack of prompt recognition of symptoms or unwillingness to immediately seek medical help.
The impact of the COVID-19 pandemic on the delays from symptom onset to first medical contact remains poorly investigated. To date, limited data from single centres suggest prolonged delays from symptom onset to first medical contact in STEMI patients [13, 14]. We observed an almost doubled time from symptom onset to first medical contact during the COVID-19 pandemic as compared with the control period (112 min vs 60 min, p <0.05).
Several reasons have been formulated to explain the prolonged delays during the COVID-19 pandemic, including the fear of getting or spreading the infection, unwillingness to overload the emergency medical systems or difficulty in getting a medical appointment [4]. However, to the best of our knowledge, objective questionnaire-based investigations of those delays have not been reported yet. In our study, the most prevalent reason for prolonged delays in calling the emergency services (58% of the respondents) was the misinterpretation of symptoms by the patients, even though two third of them presented typical chest pain. This might reflect either ineffective public health prevention messages or an altered patient behaviour driven by the COVID-19 pandemic. Other causes of prolonged delays identified were the fear of overloading a healthcare system already burdened by the pandemic (28% of respondents), as well as the fear of getting infected by the SARS-CoV-2 (22%) or contaminating relatives (22%) in the event of hospital admission. In addition, features of anxiety and depression, identified in approximately one quarter of the patients, may have contributed to patient-related delay.
Even though STEMI patients presented prolonged delays from symptom onset to first medical contact during the COVID-19 period, peak troponin and left ventricular ejection fraction were not different from the control group. This might be explained by the limited sample size. However, in the overall ACS population, driven by NSTE-ACS, we observed more extensive myocardial injury in the COVID-19 period as compared with the control period, with a two-fold higher high-sensitive cardiac troponin peak value (2247 ng/l vs 1076 ng/l, p = 0.02). This did not impact left ventricular ejection fraction, which remained similar in both groups probably as a result of the only modest, though significant from a statistical point of view, rise in high-sensitive cardiac troponins. In addition, we observed more ACS patients presenting with out-of-hospital cardiac arrest, possibly also reflecting more severe myocardial injury, even though the small number of events limits definitive conclusions.
Our results are in line with previous reports describing a significant reduction in ACS incidence during the COVID-19 pandemic [13, 15, 16], largely driven in our report by the fall in NSTE-ACS incidence (incidence rate ratio 0.324 for the COVID-19 period compared with the control period) whereas we did not find any significant reduction in STEMI incidence. A recent large analysis which included data from all patients admitted for ACS in England, showed similar results. Even though authors reported an overall 40% reduction in ACS incidence during the COVID-19 period, they noticed an almost two-fold greater decline in NSTE-ACS incidence in comparison with STEMI incidence (percent reduction 42% vs 23%) [17]. The lack of reduction in STEMI incidence in our study needs, however, to be interpreted cautiously owing to the limited sample size. The proximity and accessibility of the emergency services in our relatively small district (15.93 km2) might explain why patients with more severe symptoms (as is often the case during STEMI) were less reluctant to seek medical help.
Overall hospital length of stay for patients not prematurely transferred was shorter during the COVID-19 period than during the control period, likely because of the necessity to allow as many as possible hospital admissions for SARS-CoV-2 infected patients as our hospital was the designated COVID-19 hospital of the region.
For the ongoing second wave of the COVID-19 pandemic, reinforced health prevention campaigns would have been essential but did not occur. Public prevention messages should have raised awareness among the general population of the importance of rapidly seeking medical help in the case of ACS symptom onset despite the social restrictive measures.
The present study has several limitations. First, it was of single centre retrospective design with a limited number of patients included. Second, less than half of the eligible patients returned a completed version of the questionnaire. The extension of the results to the entire COVID-19 ACS population should thus be made with caution. Moreover, the results of the questionnaire were not compared between active and control groups. Third, peak troponin measurement and hospital length of stay were not available for a proportion of patients, as they were transferred early to other institutions to avoid saturation of our hospital.
In conclusion, during the COVID-19 period we observed prolonged delays from symptom onset to first medical contact in STEMI patients and a decline in overall ACS incidence driven by a lower incidence of NSTE-ACS patients. In addition, ACS patients presented with more extensive myocardial damage. Patient-related reasons for the increased delay in calling the emergency services included the fear of contracting or spreading COVID-19 in the event of hospital admission and reluctance to add additional burdens to the healthcare system. Public health campaigns should better address these issues for the potential next waves of the pandemic.
Questionnaire addressed to all surviving patients who presented an ACS during the COVID-19 period.
Table S1: Baseline characteristics of the two control groups.
Table S2: Outcome measures in ST segment elevation myocardial infarction patients in the two control groups.
Table S3: Outcome measures in non-ST segment elevation myocardial infarction-acute coronary syndrome patients in the two control groups.
Table S4: Baseline characteristics of respondents and non-respondents to the questionnaire.
Table S5: Outcome measures among respondents and non-respondents to the questionnaire.
The appendices are available as separate files at https://smw.ch/article/doi/smw.2020.20448.
No financial support and no other potential conflict of interest relevant to this article was reported.
The data underlying this article will be shared on reasonable request to the corresponding author.
1WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
2 https://www.admin.ch/opc/en/classified-compilation/20200744/index.html.
4 Roffi M , Guagliumi G , Ibanez B . The Obstacle Course of Reperfusion for ST-Segment-Elevation Myocardial Infarction in the COVID-19 Pandemic. Circulation. 2020;141(24):1951–3. doi:.https://doi.org/10.1161/CIRCULATIONAHA.120.047523
5 De Filippo O , D’Ascenzo F , Angelini F , Bocchino PP , Conrotto F , Saglietto A , et al. Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy. N Engl J Med. 2020;383(1):88–9. doi:.https://doi.org/10.1056/NEJMc2009166
6 Roffi M , Patrono C , Collet JP , Mueller C , Valgimigli M , Andreotti F , et al.; ESC Scientific Document Group. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(3):267–315. Available at: https://academic.oup.com/eurheartj/article/37/3/267/2466099. doi:.https://doi.org/10.1093/eurheartj/ehv320
7 Ibanez B , James S , Agewall S , Antunes MJ , Bucciarelli-Ducci C , Bueno H , et al.; ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77. Available at: https://academic.oup.com/eurheartj/article/39/2/119/4095042. doi:.https://doi.org/10.1093/eurheartj/ehx393
8 Ornato JP , Peberdy MA , Chandra NC , Bush DE . Seasonal pattern of acute myocardial infarction in the National Registry of Myocardial Infarction. J Am Coll Cardiol. 1996;28(7):1684–8. doi:.https://doi.org/10.1016/S0735-1097(96)00411-1
9 Patel NJ , Pant S , Deshmukh AJ , Nalluri N , Badheka AO , Shah N , et al. Seasonal variation of acute myocardial infarction related hospitalizations in the United States: perspective over the last decade. Int J Cardiol. 2014;172(3):e441–2. doi:.https://doi.org/10.1016/j.ijcard.2013.12.319
10 González Hernández E , Cabadés O’Callaghan A , Cebrián Doménech J , López Merino V , Sanjuán Mañez R , Echánove Errazti I , et al.; Investigadores del estudio PRIMVAC. [Seasonal variations in admissions for acute myocardial infarction. The PRIMVAC study]. Rev Esp Cardiol. 2004;57(1):12–9. Available at: https://www.revespcardiol.org/en-seasonal-variations-in-admissions-for-articulo-13056528.
11 Zigmond AS , Snaith RP . The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70. doi:.https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
12 Ting HH , Bradley EH , Wang Y , Nallamothu BK , Gersh BJ , Roger VL , et al. Delay in presentation and reperfusion therapy in ST-elevation myocardial infarction. Am J Med. 2008;121(4):316–23. doi:.https://doi.org/10.1016/j.amjmed.2007.11.017
13 Wilson SJ , Connolly MJ , Elghamry Z , Cosgrove C , Firoozi S , Lim P , et al. Effect of the COVID-19 Pandemic on ST-Segment-Elevation Myocardial Infarction Presentations and In-Hospital Outcomes. Circ Cardiovasc Interv. 2020;13(7):e009438. doi:.https://doi.org/10.1161/CIRCINTERVENTIONS.120.009438
14 Tam CF , Cheung KS , Lam S , Wong A , Yung A , Sze M , et al. Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment-Elevation Myocardial Infarction Care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4):e006631. doi:.https://doi.org/10.1161/CIRCOUTCOMES.120.006631
15 Solomon MD , McNulty EJ , Rana JS , Leong TK , Lee C , Sung SH , et al. The Covid-19 Pandemic and the Incidence of Acute Myocardial Infarction. N Engl J Med. 2020 l;383(7):691–3. doi:.https://doi.org/10.1056/NEJMc2015630
16 Garcia S , Albaghdadi MS , Meraj PM , Schmidt C , Garberich R , Jaffer FA , et al. Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States During COVID-19 Pandemic. J Am Coll Cardiol. 2020;75(22):2871–2. doi:.https://doi.org/10.1016/j.jacc.2020.04.011
17 Mafham MM , Spata E , Goldacre R , Gair D , Curnow P , Bray M , et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396(10248):381–9. doi:.https://doi.org/10.1016/S0140-6736(20)31356-8
No financial support and no other potential conflict of interest relevant to this article was reported.
The data underlying this article will be shared on reasonable request to the corresponding author.