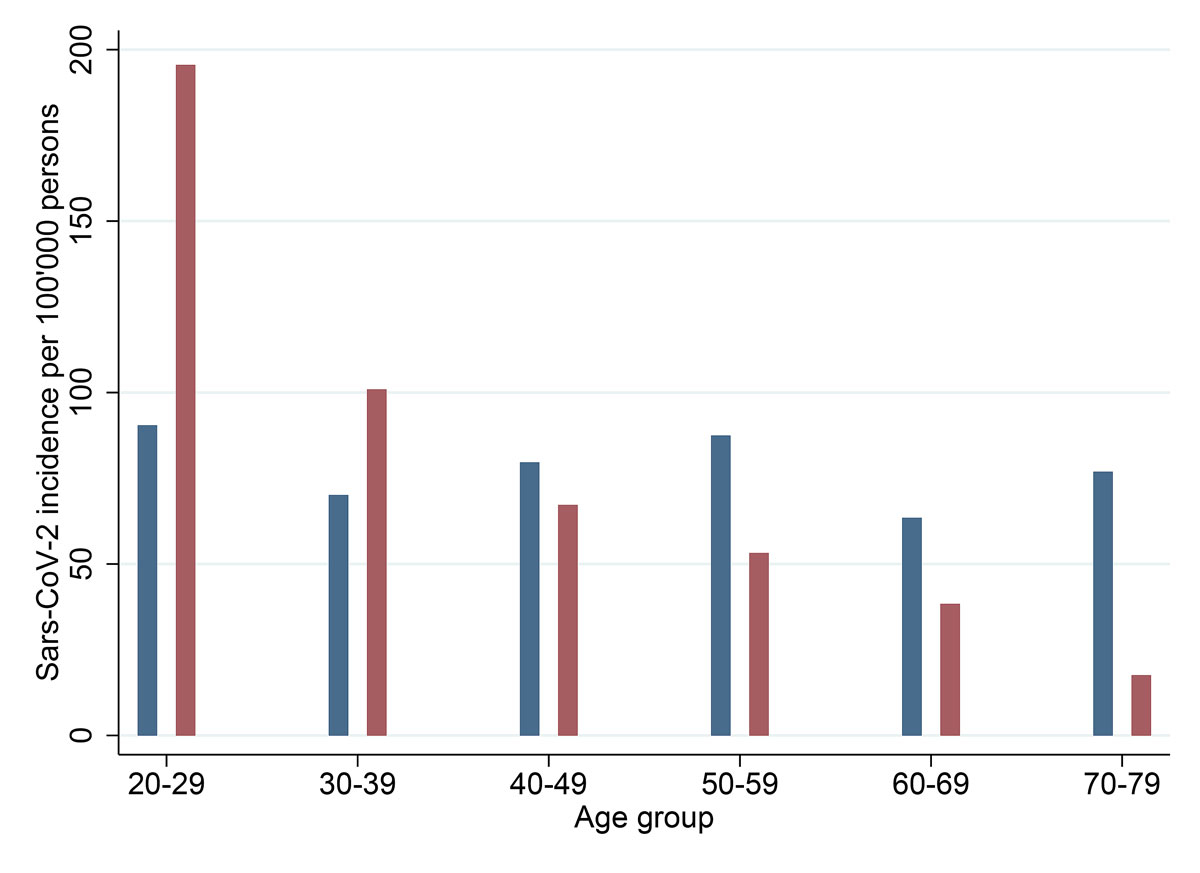
Figure 1 SARS-Cov-2 incidence per 100,000 individuals across different age groups between 4 and 20 April 2020 (blue), and 1 and 27 August 2020 (red). Source: Federal Office of Public Health [1].
DOI: https://doi.org/10.4414/smw.2020.20416
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic reached Switzerland in spring 2020, leading to a nationwide lockdown between the 23 March and 16 April 2020. This first wave of infections was followed by a temporary decrease in new infections to low levels, both in Switzerland and elsewhere in Europe. However, in August 2020 numbers of infections in many European countries began to rise again. Importantly, the dynamic of the pandemic in August and early September 2020 differed from the first wave in several important characteristics. First, it was characterised by an elevated incidence of infections among younger individuals (fig. 1 and fig. S1 in appendix 1). Second, the number of hospitalisations or deaths related to SARS-CoV-2 was substantially lower than the number of infections in spring 2020 [2]. However, at the end of October 2020 the dynamic of the second wave in Switzerland largely resembled the pattern of the first wave as infection rates started to rise again among all age groups.
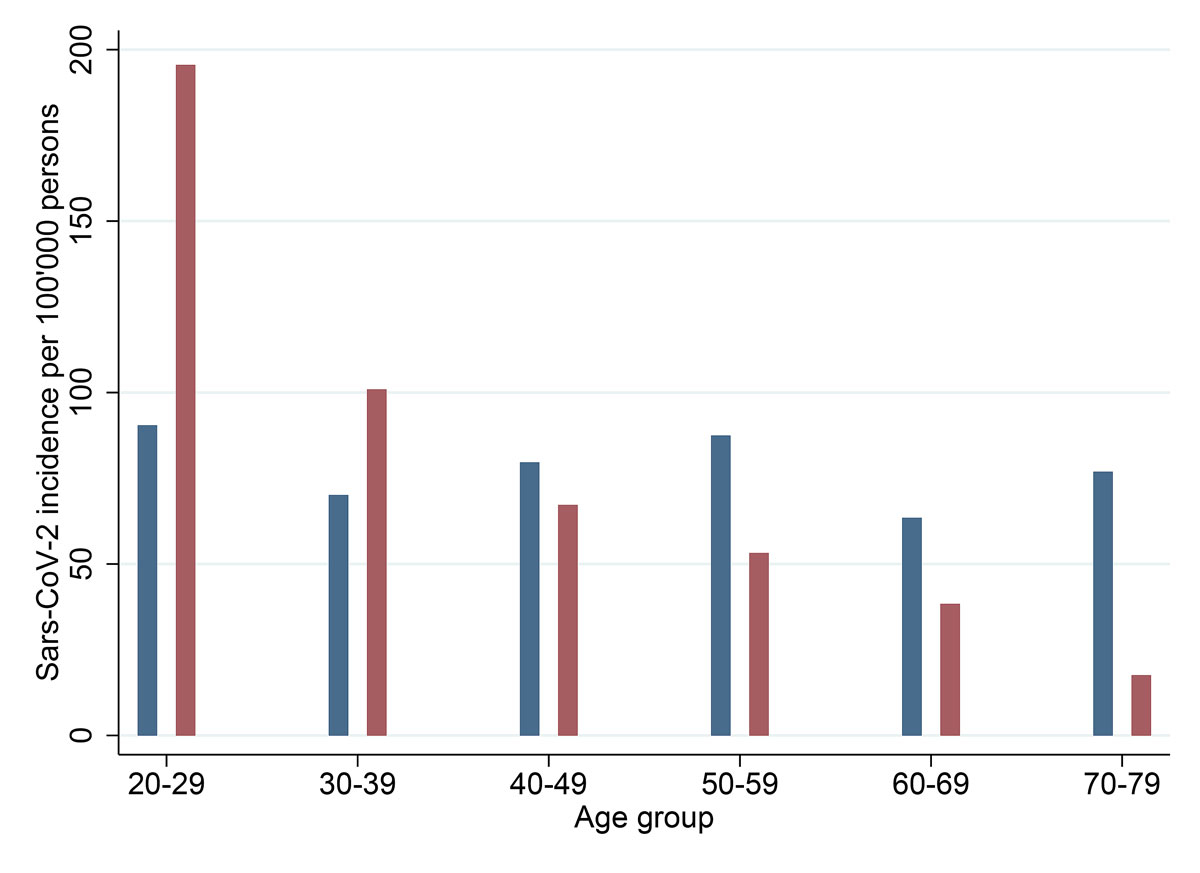
Figure 1 SARS-Cov-2 incidence per 100,000 individuals across different age groups between 4 and 20 April 2020 (blue), and 1 and 27 August 2020 (red). Source: Federal Office of Public Health [1].
This expansion of infections from younger to older age groups was not unforeseeable. Indeed, observations from different regions of the world indicate that local transmissions of SARS-CoV-2 do not seem to stay confined to specific age segments such as younger persons. Findings from a study conducted in the state of Florida revealed that the pandemic initially mainly circulated among younger individuals, but then infections spread to all age groups [3]. Since infected individuals’ age consistently emerged as one of the central predictors for a more severe course of the infection, for hospitalisation, need for ventilation, or mortality [3], the protection of vulnerable persons with chronic co-morbidities and of higher age are key in pandemic mitigation measures. In this context, nursing homes and other institutions for the elderly are of particular concern as many potentially vulnerable persons live in close proximity [4] with high mortality in the case of infectious outbreaks [5].
Hence, a deeper understanding of risk exposure and the epidemic transmissions across different age groups is crucial for our understanding of the infection dynamics and for planning prevention efforts. With regard to the transmission of infections across age groups, “social mixing” has received increasing attention as a key mechanism. As revealed by modelling studies, social mixing constitutes an important driver of transmission or, in reverse, an effective possible means for mitigation [6]. As a consequence, interactions between different age groups (e.g., grand-parents and grand-children), as well as compliance with recommended measures (e.g., keeping distance, mask wearing) require particular attention. Because, for most people, the majority of social contacts are with person groups of approximately similar age, transmissions within age groups may eventually also lead to self-propagating sub-epidemics along the social networks of persons of older age [7].
The present research aimed to contribute to deeper insight into the potential impact of “social mixing” of different age groups on possible SARS-CoV-2 exposure risks for persons aged 65 years and older. An understanding of such transmission dynamics will be key for managing the pandemic in time to come. To this end, the study focused on the transitional phase between the first and the second pandemic wave of SARS-CoV-2 in Switzerland in order to anticipate future pandemic dynamics. We defined exposure risks as a combination of numerous social contacts and low or only partial adherence to preventive measures. To examine the exposure risks, we analysed data from a longitudinal online panel on health and social behaviour during the SARS-CoV-2 pandemic in Switzerland. The present study examined the following research questions:
The present study examined persons aged 65 years and older using longitudinal panel data from the Swiss COVID-19 Social Monitor [8]. In brief, the Swiss COVID-19 Social Monitor comprises a cohort of randomly selected participants of an existing online panel population (that is, a stratified sample with regard to age, gender and linguistic region) who receive an invitation every 2 to 6 weeks to complete a survey pertaining to SARS-CoV-2. The first survey of the Social Monitor started 2 weeks after the lockdown in Switzerland (from 30 March to 6 April 2020). To make the Social Monitor samples representative for the overall Swiss population, it was weighted with regard to education, age, gender and region. So far, nine questionnaires with an average response of 1500 to 1700 persons have been completed. Participants are well-described with respect to demographics, attitudes towards SARS-CoV-2, health status, the number of social contacts, potential risks for SARS-CoV-2 infections and adherence to preventive measures for COVID-19. The most recent assessment (survey “August”) was implemented between 17 and 25 August 2020 (n = 1508 respondents). For research question one, which pertained to changes in social mixing and prevention, data from survey “August” were compared with the survey that was implemented between 11 and 18 May 2020 (survey “May”). “Survey “May” thus captures the time period following 11 May when the most severe lockdown measures had just been lifted (such as re-opening of schools, restaurants or shops). The Swiss COVID-19 Social Monitor has received a waiver from the cantonal Ethics Committee of Zurich (BASEC-Nr. Req-2020-00323) that it does not fall under the Swiss Human Research Law so that no informed consent was necessary.
Data were analysed using descriptive statistical methods. For the comparison of preventive behaviours and social contacts, categorical data were summarised as n (%) and median (interquartile range).
For research question one, the following self-reported questionnaire variables were compared across the two surveys: age, gender, linguistic region, household income, education, smoking status, presence of chronic illnesses, application of preventive measures for SARS-Cov-2 (see below) in the past 7 days, activities outside own house/flat, number of personal interactions in past 7 days, and the perceived risk for a SARS-Cov-2 infection on a scale from 0 to 100 percent.
For research question two, we sought to group the elderly participants from survey “August” with respect to similarity of social contact patterns and preventive behaviours. More specifically, we attempted to identify groups of persons who may be at a higher risk for a SARS-Cov-2 infection because they have many social contacts but apply recommended preventive measures only partially. To this end, we conducted an exploratory factor analysis using polychoric correlations as this analysis strategy allows us to distinguish between different groups with relatively homogenous patterns of behaviour and adherence to preventive measures.
For the analysis we considered the following categorical variables, which capture risks and preventive behaviours by assessing different reasons why individuals left the house over the course of the past 7 days: left the house to visits friends (indoor), to visit friends (outdoor), for shopping, for medical appointments, or for leisure and sports. Furthermore, the adherence to different preventive measures was assessed over the past 7 days using a 5-item scale including “never”, “rarely”, “sometimes”, “often”, and “always”. The following measures were included: using disinfectants, hand washing, avoiding leaving one’s home for non-essential tasks, avoiding personal contacts with persons aged 65 years or older, avoiding indoor visits in general, wearing masks, avoiding public transportation, keeping distance. To reduce the number of categories, “never” and “rarely”, as well as “often” and “always” were each collapsed into single categories. Furthermore, the use of the SwissCovid app and more than seven personal contacts (corresponding to the median) over the past 7 days were included as binary variables (yes/no) in the factor analysis.
Following the initial analysis two factor dimensions were retained as indicated by the eigenvalue scree plot. Furthermore, the following variables were retained (based on a minimal absolute factor loading 0.4 [9]): avoiding indoor visits, keeping distance, avoiding public transportation, avoiding non-essential outside activities, meeting friends indoors, meeting friends outdoors, and having more than seven personal contacts. Next, factor predictions were derived from the final model and clustered using the k-means algorithm. The derivation of the optimal number of k-means clusters was based on the Pseudo-F index, which yielded a maximum value of four clusters. All analyses were performed using Stata 13.1 (Stata Corp., College Station TX, US). Given the descriptive, exploratory nature of our study we did not implement statistical significance testing.
In summary, 270 persons (survey “May”: n = 1673 respondents in total) and 256 (survey “August”: n = 1532 respondents in total) aged 65 years and older were analysed for the present study. Of those, 235 individuals participated in both surveys. Summary data on demographic characteristics and adherence to recommended preventive measures are presented in table 1. The median age was 70 years (both surveys) and 45.6% (survey “May”) and 45.3% (survey “August”) of the respondents were female. Individuals participating in survey “May” and survey “August” did not differ substantially with regard to demographic characteristics.
Table 1 Demographic characteristics and adherence to recommended preventive measures in the Swiss COVID-19 Social Monitor assessed at survey “May” and survey “August” of persons aged 65 years or older.
|
Survey “May”
(n = 270) |
Survey “August”
(n = 256) |
|
|---|---|---|
| Age, median (IQR) | 70 (68–74) | 70 (68–74) |
| Female gender | 123 (45.6) | 116 (45.3) |
| Has a partner | ||
| No partner | 66 (24.4) | 63 (24.6) |
| Living with partner | 191 (70.7) | 179 (69.9) |
| Not living with partner | 13 (4.8) | 14 (5.5) |
| Citizenship | ||
| Swiss | 243 (90.0) | 229 (89.5) |
| Swiss and other | 11 (4.1) | 10 (3.9) |
| Non-Swiss | 16 (5.9) | 17 (6.6) |
| Linguistic region | ||
| German | 178 (65.9) | 174 (68.0) |
| French | 58 (21.5) | 53 (20.7) |
| Italian | 34 (12.6) | 29 (11.3) |
| Education | ||
| Compulsory education only | 15 (5.6) | 12 (4.7) |
| Achieved higher education degree | 139 (51.5) | 130 (50.8) |
| University, university of applied sciences | 116 (43.0) | 114 (44.5) |
| Currently not working | 238 (88.1) | 231 (90.2) |
| Monthly household income | ||
| ≤CHF 6000 | 97 (35.9) | 91 (35.5) |
| CHF 6000 to CHF 10000 | 101 (37.4) | 94 (36.7) |
| >CHF 10000 | 35 (13.0) | 37 (14.5) |
| No answer | 37 (13.7) | 34 (13.3) |
| Smoker | 51 (18.9) | 43 (16.8) |
| Self-reported chronic illness* | 116 (43.0) | 111 (43.4) |
| Use of protective masks | ||
| Always or most of the time | 64 (23.8) | 140 (54.7) |
| Sometimes | 119 (44.2) | 97 (37.9) |
| Rarely or never | 86 (32.0) | 19 (7.4) |
| Staying at home except for essential tasks | ||
| Always or most of the time | 198 (73.6) | 84 (32.8) |
| Sometimes | 57 (21.2) | 97 (37.9) |
| Rarely or never | 14 (5.2) | 75 (29.3) |
| Using disinfectants | ||
| Always or most of the time | 212 (79.1) | 214 (83.6) |
| Sometimes | 47 (17.5) | 39 (15.2) |
| Rarely or never | 9 (3.4) | 3 (1.2) |
| Keeping recommended distance (1.5/2 m) | ||
| Always or most of the time | 264 (98.1) | 227 (88.7) |
| Sometimes | 5 (1.9) | 25 (9.8) |
| Rarely or never | 0 (0.0) | 4 (1.6) |
| Avoiding private visits | ||
| Always or most of the time | 228 (84.8) | 77 (30.1) |
| Sometimes | 32 (11.9) | 112 (43.8) |
| Rarely or never | 9 (3.3) | 67 (26.2) |
| Avoiding public transport | ||
| Always or most of the time | 247 (91.8) | 178 (69.5) |
| Sometimes | 16 (5.9) | 47 (18.4) |
| Rarely or never | 6 (2.2) | 31 (12.1) |
| Sneezing/coughing into elbow/handkerchief | ||
| Always or most of the time | 240 (89.6) | 226 (88.6) |
| Sometimes | 16 (6.0) | 18 (7.1) |
| Rarely or never | 12 (4.5) | 11 (4.3) |
| No meetings with 65+-year-olds | ||
| Always or most of the time | 181 (67.0) | 49 (19.1) |
| Sometimes | 47 (17.4) | 64 (25.0) |
| Rarely or never | 42 (15.6) | 143 (55.9) |
| Frequent hand-washing | ||
| Always or most of the time | 264 (97.8) | 248 (96.9) |
| Sometimes | 5 (1.9) | 7 (2.7) |
| Rarely or never | 1 (0.4) | 1 (0.4) |
| Number of persons seen personally in past 7 days | 5 (3, 8) | 7 (4, 11) |
| Activities outside home during last 7 days | ||
| Seeing friends inside | 40 (14.8) | 87 (34.0) |
| Seeing friends outside | 97 (35.9) | 147 (57.4) |
| Shopping | 209 (77.4) | 234 (91.4) |
| Leisure, sports | 74 (27.4) | 115 (44.9) |
| Medical appointments | 103 (38.1) | 101 (39.5) |
| Using SwissCovid app | 0 (0.0) | 116 (45.3) |
| Perceived risk for infection with SARS-CoV-2 (%); median (IQR) | 5 (2–14) | 5 (2–12) |
IQR = interquartile range * Presence of chronic illnesses was defined based on self-report of at least one of the following conditions: asthma, chronic obstructive pulmonary disease (COPD), diabetes, hypertension, cardiovascular disease, stroke, cancer.
Established preventive measures such as frequent hand washing (survey “May”: 98%; survey “August”: 97%), use of disinfectants (survey “May”: 79%; survey “August”: 84%) and sneezing into the elbow (survey “May”: 90%; survey “August”: 89%) were reported at similar frequencies across the two surveys. In contrast, adherence to preventive measures pertaining to social contacts decreased substantially from survey “May” to survey “August”. More specifically, this concerned avoiding visits (%-point difference between survey “August” and survey “May”: −55%) and keeping distance (−9%). Consistently, survey “August”-participants more frequently reported inside visits of friends (+9%-points), outside visits of friends (+21%-points) or going outside for shopping (+14%-points) or leisure activities (+14%-points), and the median number of persons seen increased from five to seven between the two surveys. Of additional relevance, the SwissCovid proximity tracing app was released after survey “May” and 45% of respondents reported use of the app at survey “August”. Further, we observed that the median number of social contacts differed across linguistic regions: it was lowest in the German-speaking regions (7, IQR 4–10), followed by the French-speaking part (8, IQR 4–12), and highest in the Italian-speaking region (11, IQR 5–13)). Concordantly, the frequency of persons who indicated always or often keeping the recommended physical distance ranked in the same order (92%, 83% and 79%).
To identify at-risk individuals among elderly persons the combined factor/k-means clustering analysis of survey “August” data yielded four distinct groups of elderly individuals in terms of different patterns of adherence to recommended preventive measures (table 2): a larger group of individuals with many social contacts but high self-reported adherence to preventive measures (group 1, n = 86); a small group with many social contacts and overall lower adherence (group 2, n = 26); a group with comparatively few contacts and few social activities (group 3, n = 66); and a group which differed from latter through fewer contacts but more social activities than (group 4, n = 78). Sociodemographic characteristics and risk perception with regard to SARS-CoV-2 infections did not differ in a relevant way across the four groups.
Table 2 Demographic characteristics of four distinct groups of elderly persons with regard to their adherence to recommended preventive measures derived from an exploratory factor analysis.
|
Group 1
(n = 86) |
Group 2
(n = 26) |
Group 3
(n = 66) |
Group 4
(n = 78) |
|
|---|---|---|---|---|
| Age (mean) | 70.6 (69.8–71.5) | 70.9 (69.2–72.7) | 71.7 (70.7–72.7) | 70.9 (70.1–71.7) |
| Female gender | 52.3 (41.3–63.2) | 50.0 (29.9–70.1) | 31.8 (20.9–44.4) | 47.4 (36.0–59.1) |
| Has a partner | ||||
| No partner | 26.7 (17.8–37.4) | 38.5 (20.2–59.4) | 18.2 (9.8–29.6) | 23.1 (14.3–34.0) |
| Living with partner | 67.4 (56.5–77.2) | 57.7 (36.9–76.6) | 78.8 (67.0–87.9) | 69.2 (57.8–79.2) |
| Not living with partner | 5.8 (1.9–13.0) | 3.8 (0.1–19.6) | 3.0 (0.4–10.5) | 7.7 (2.9–16.0) |
| Citizenship | ||||
| Swiss | 88.4 (79.7–94.3) | 73.1 (52.2–88.4) | 89.4 (79.4–95.6) | 96.2 (89.2–99.2) |
| Swiss and other | 3.5 (0.7–9.9) | 11.5 (2.4–30.2) | 4.5 (0.9–12.7) | 1.3 (0.0–6.9) |
| Non-Swiss | 8.1 (3.3–16.1) | 15.4 (4.4–34.9) | 6.1 (1.7–14.8) | 2.6 (0.3–9.0) |
| Linguistic region | ||||
| German | 67.4 (56.5–77.2) | 42.3 (23.4–63.1) | 71.2 (58.7–81.7) | 74.4 (63.2–83.6) |
| French | 18.6 (11.0–28.4) | 34.6 (17.2–55.7) | 22.7 (13.3–34.7) | 16.7 (9.2–26.8) |
| Italian | 14.0 (7.4–23.1) | 23.1 (9.0–43.6) | 6.1 (1.7–14.8) | 9.0 (3.7–17.6) |
| Education | ||||
| Compulsory education only | 2.3 (0.3–8.1) | 11.5 (2.4–30.2) | 6.1 (1.7–14.8) | 3.8 (0.8–10.8) |
| Achieved higher education degree | 53.5 (42.4–64.3) | 42.3 (23.4–63.1) | 50.0 (37.4–62.6) | 51.3 (39.7–62.8) |
| University, university of applied sciences | 44.2 (33.5–55.3) | 46.2 (26.6–66.6) | 43.9 (31.7–56.7) | 44.9 (33.6–56.6) |
| Currently not working | 90.7 (82.5–95.9) | 92.3 (74.9–99.1) | 87.9 (77.5–94.6) | 91.0 (82.4–96.3) |
| Monthly household income | ||||
| ≤CHF 6000 | 34.9 (24.9–45.9) | 42.3 (23.4–63.1) | 31.8 (20.9–44.4) | 37.2 (26.5–48.9) |
| CHF 6000 to CHF 10000 | 38.4 (28.1–49.5) | 30.8 (14.3–51.8) | 43.9 (31.7–56.7) | 30.8 (20.8–42.2) |
| >CHF 10000 | 14.0 (7.4–23.1) | 11.5 (2.4–30.2) | 12.1 (5.4–22.5) | 17.9 (10.2–28.3) |
| No answer | 12.8 (6.6–21.7) | 15.4 (4.4–34.9) | 12.1 (5.4–22.5) | 14.1 (7.3–23.8) |
| Smoker | 14.0 (7.4–23.1) | 15.4 (4.4–34.9) | 16.7 (8.6–27.9) | 20.5 (12.2–31.2) |
| Self-reported chronic illness* | 43.0 (32.4–54.2) | 46.2 (26.6–66.6) | 42.4 (30.3–55.2) | 43.6 (32.4–55.3) |
| Use of protective masks† | ||||
| Always or most of the time | 59.3 (48.2–69.8) | 19.2 (6.6–39.4) | 62.1 (49.3–73.8) | 55.1 (43.4–66.4) |
| Staying at home except for essential tasks† | ||||
| Always or most of the time | 4.7 (1.3–11.5) | 11.5 (2.4–30.2) | 83.3 (72.1–91.4) | 28.2 (18.6–39.5) |
| Keeping recommended distance (1.5 m / 2 m) † | ||||
| Always or most of the time | 98.8 (93.7–100.0) | 0.0 (0.0–13.2) | 97.0 (89.5–99.6) | 100.0 (95.4–100.0) |
| Avoiding private visits† | ||||
| Always or most of the time | 1.2 (0.0–6.3) | 0.0 (0.0–13.2) | 84.8 (73.9–92.5) | 25.6 (16.4–36.8) |
| Avoiding public transport† | ||||
| Always or most of the time | 53.5 (42.4–64.3) | 53.8 (33.4–73.4) | 92.4 (83.2–97.5) | 73.1 (61.8–82.5) |
| No meetings with 65+ year olds | ||||
| Always or most of the time | 4.7 (1.3–11.5) | 3.8 (0.1–19.6) | 53.0 (40.3–65.4) | 11.5 (5.4–20.8) |
| More than seven persons seen† | 76.7 (66.4–85.2) | 57.7 (36.9–76.6) | 15.2 (7.5–26.1) | 34.6 (24.2–46.2) |
| Number of persons seen personally in past 7 days | 12.2 (10.3–14.2) | 8.2 (6.1–10.3) | 5.2 (4.3–6.0) | 8.7 (6.6–10.8) |
| Activities outside home during last 7 days | ||||
| Seeing friends inside | 64.0 (52.9–74.0) | 34.6 (17.2–55.7) | 16.7 (8.6–27.9) | 15.4 (8.2–25.3) |
| Seeing friends outside | 83.7 (74.2–90.8) | 65.4 (44.3–82.8) | 24.2 (14.5–36.4) | 53.8 (42.2–65.2) |
| Shopping | 98.8 (93.7–100.0) | 100.0 (86.8–100.0) | 78.8 (67.0–87.9) | 91.0 (82.4–96.3) |
| Leisure, sports | 52.3 (41.3–63.2) | 38.5 (20.2–59.4) | 28.8 (18.3–41.3) | 52.6 (40.9–64.0) |
| Medical appointments | 40.7 (30.2–51.8) | 34.6 (17.2–55.7) | 34.8 (23.5–47.6) | 43.6 (32.4–55.3) |
| Using SwissCovid app | 43.0 (32.4–54.2) | 23.1 (9.0–43.6) | 51.5 (38.9–64.0) | 50.0 (38.5–61.5) |
| Perceived risk for infection with SARS-CoV-2 (%); mean | 7.9 (5.5–10.3) | 10.0 (5.9–14.1) | 12.8 (8.1–17.5) | 10.2 (6.7–13.7) |
Numbers in parentheses are 95% confidence intervals of point estimates. The four groups were derived from an exploratory factor analysis. Overall, they can be characterised as follows: ‘good adherence to preventive measures’ (group 1), ‘many social contacts and relatively low adherence' (group 2), ‘few contacts and few social activities’ (group 3), ‘few contacts but more social activities’ (group 4). * Presence of chronic illnesses was defined based on self-report of at least one of the following conditions: asthma, chronic obstructive pulmonary disease (COPD), diabetes, hypertension, cardiovascular disease, stroke, cancer. † included in factorial analysis
A radar plot visualising the behaviour patterns of the four distinct groups is presented in figure 2. Values closer to the centre indicate that in a given group less persons reported possible risk exposure.
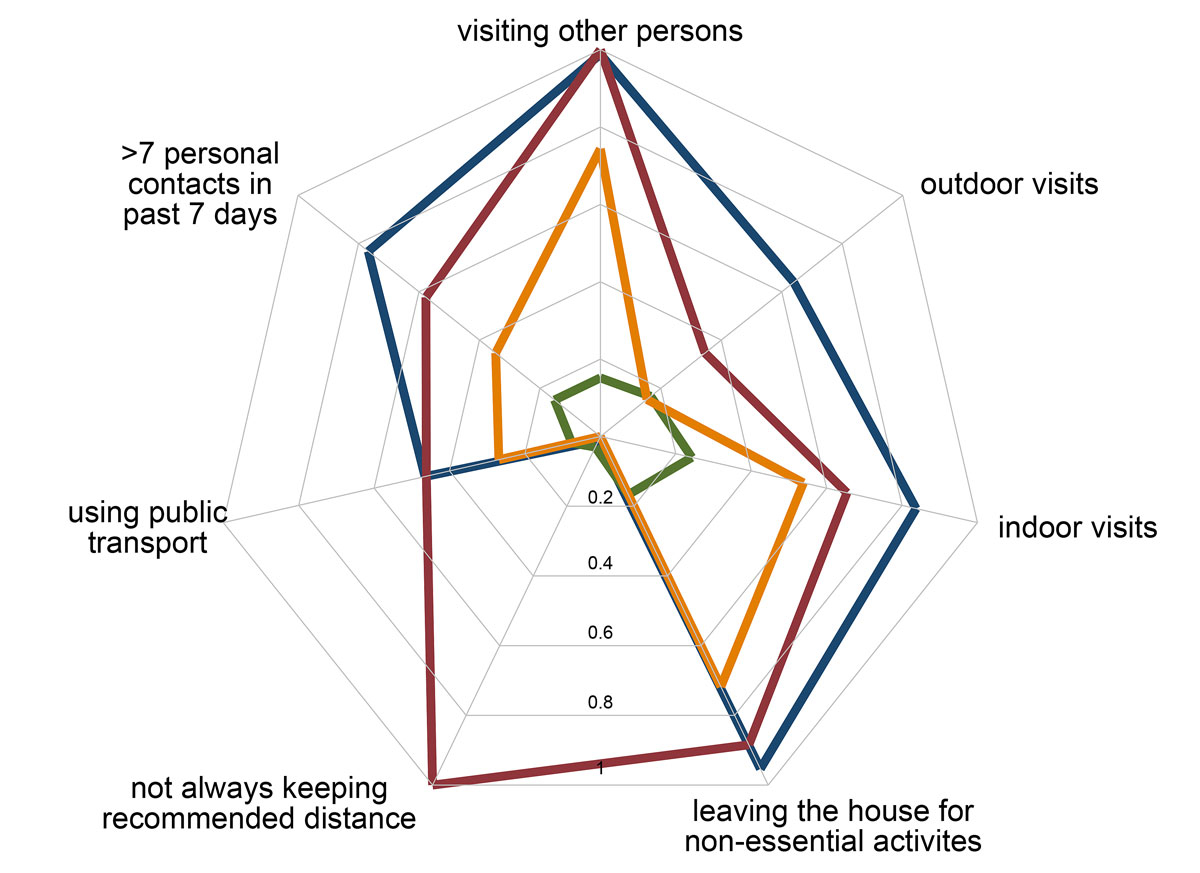
Figure 2 Radar plot visualising findings from an exploratory factor analysis on self-reported adherence to recommended preventive measures among elderly persons in Switzerland. Colours correspond to the four distinct groups presented in table 2: “good adherence to preventive measures” (blue; group 1, n = 86), “many social contacts and relatively low adherence” (red; group 2, n = 26), “few contacts and few social activities” (green; group 3, n = 66), “few contacts but more social activities” (yellow; group 4, n = 78). Lower values correspond to lower adherence to the specific prevention measure and, thereby, to a higher risk for an infection.
The present study expands the scope of previous SARS-CoV-2-related research in Switzerland by providing insight into “social mixing” and adherence to recommended preventive measures among elderly persons during the transitional phase between two pandemic waves. In the light of the most recent pandemic developments, a comprehensive understanding of the transmission dynamics preceding the second wave will be key for anticipating future developments and for managing the pandemic in the time to come. To examine changes in preventive behaviours and social contacts, the present research focused on the time period between the end of the Swiss lockdown and late August 2020 using longitudinal online panel data. The study revealed two key findings. First, mobility and social interactions overall increased from May to August 2020 in elderly persons, whereas simultaneously adherence to recommended preventive measures decreased overall. Second, we identified four distinct groups with regard to their risk for potential infections as indicated by their self-reported adherence to recommended preventive measures. We found that about one quarter of all elderly were still strictly adhering to social distancing and preventive measures. In contrast, a minority of 10% of the elderly in our sample had many social contacts and were lacking adherence to preventive measures. The remaining groups seemed to fall in between: while they did have multiple personal contacts, they still maintained the recommended distance.
Our first research question pertained to potential changes in mobility, social interactions and adherence to recommended preventive measures during the time period between the release of the lockdown in Switzerland in May to late August 2020. Even though adherence to preventive measures in elderly persons decreased overall, it is important to consider that our data revealed substantial heterogeneity of different behaviour patterns. Importantly, the specific time period covered in the present study was characterised by a release in lockdown measures (re-opening of shops, schools and other public institutions) and a short phase with low double-digit SARS-CoV-2 case numbers, finally followed by an increase in new infections to over 400 new cases per day in August. As such, following a relaxation of the overall situation in Switzerland in July an increasing number of persons started to resume a near-normal life or travelled for their vacation. However, in early August, case numbers started to increase substantially, and so called local “superspreading events” received increasing attention in the media. However, there was then no escalation of preventive measures and mandates, and the Federal Office of Public Health and cantonal health authorities only issued warnings and called on self-responsibility. Against this backdrop, the heterogeneity with respect to social behaviour and adherence to preventive measures observed in our survey “August” questionnaire is not surprising.
Our second research question aimed to provide insight into differences among elderly individuals with regard to their risk for a potential infection in the light of their adherence to recommended preventive measures. Among the four groups identified by a factor analysis, two groups stood out as they constituted two extremes of a spectrum: a relatively small group (10%) with an overall higher amount of social contacts and simultaneously low adherence to recommended preventive measures (e.g., distance keeping), and a larger group (25%) with comparatively few contacts and high adherence. Interestingly, there were few differences in terms of sociodemographic characteristic or presence of chronic illnesses.
The two groups reporting an elevated number of social contacts (that is, groups 1 and 2) were slightly more frequent in the French- and Italian-speaking parts of Switzerland, such that they might possibly also reflect cultural differences (such as differences in the usual amount of social contact in everyday life). Indeed, we observed that the amount of social contacts seemed to differ across linguistic regions. The median number of persons seen in the past 7 days was lowest in the German-speaking region and highest in the Italian-speaking region. This pattern was also reflected in individuals’ adherence to keeping the recommended physical distance. These observations, if confirmed, may imply that prevention messages specific to the linguistic region may be warranted.
The present study, which was conducted in Switzerland, is in line with international research into social contacts, mobility, and adherence to preventive measures in elderly persons. A survey conducted in the UK with a similar sample size of 1356 participants revealed a 74% reduction of social contacts during the lockdown in March 2020. Importantly, elderly individuals (aged 70 years and older) had on average of 2.5 contacts per day during the lockdown and 7.6 contacts during a pre-pandemic baseline [10]. Using mathematical models, the same authors demonstrated that the basic reproductive number (R0) of the SARS-CoV-2 epidemic could be reduced to a value below 1 (which is needed for a self-sustained epidemic) by physical distancing. A study from Luxemburg reported a daily average of 1.7 contacts during and 4.7 contacts after the lockdown for persons aged 64 years or older [11]. Similar data are also available from the Netherlands [12]. The average number of contacts in Switzerland following the release of the lockdown were slightly higher (survey “May”: 6.2; survey “August”: 8.9). This divergence is likely to be linked to the longer time period covered by the Social Monitor (7 days) rather than reflecting a real difference. As such, our study expands findings from other countries by examining both social contacts and the adherence to preventive measures simultaneously.
Our study has several limitations which merit consideration. The Swiss COVID-19 Social Monitor is based on an online panel that is representative of the Swiss population with regard to key demographic characteristics [12]. However, there may be differences between panel participants and the general population with regard to health literacy or adherence to health-related recommendations. Furthermore, despite the implementation of the study in an online environment it is still possible that participants responded in a socially desirable way. Further, a recall bias pertaining to the accuracy of survey responses cannot be excluded. It is important to mention though that social contact data and reports regarding preventive measures were compared with data from the survey implemented in July for persons who participated both survey “May” and survey “August”. Overall, the responses were remarkably coherent across the two surveys (not presented in this paper). Finally, the sample size did not allow more detailed stratifications (e.g., by language region).
The present study has implications that might contribute to informing official recommendations pertaining to preventive measures and behaviours in Switzerland in elderly individuals. A key finding was that although many elderly persons adhered to prevention recommendations there was substantial heterogeneity in this group such that the elderly gradually differed with respect to their exposure risks. This heterogeneity with regard to the adherence to preventive measures is not surprising given the low incidence over the summer. However, the rapid and uncontrollable emergence of the second infection wave in October 2020 has emphasised the importance of preventive measures among all age groups. Our findings, in accordance with the resurgence of pandemic transmission among older age groups, imply that in order to protect vulnerable populations such as the elderly, pandemic containment among all age groups is essential. Furthermore, our results indicate that prevention and communication efforts during post-pandemic phases may benefit from being more tailored to local differences between linguistic regions in Switzerland.
The Swiss COVID-19 Social Monitor has received funding from the Federal Office of Public Health and from Health Promotion Switzerland. The funders had no influence on the design, conduct, analyses and publications.
The authors declare no conflict of interest with respect to this study, submission or publication of this manuscript
1Bundesamt für Gesundheit (BAG). Neues Coronavirus: Situation Schweiz. Available from: https://www.bag.admin.ch/bag/de/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/situation-schweiz-und-international.html.
2Bundesamt für Gesundheit. COVID-19 - Situation Schweiz: Verteilung nach Kanton, Alter und Geschlecht. Available from: https://covid-19-schweiz.bagapps.ch/de-1.html [accessed 2020 September 23].
3 Harris JE . Data from the COVID-19 epidemic in Florida suggest that younger cohorts have been transmitting their infections to less socially mobile older adults. Rev Econ Househ. 2020;1–19. Online ahead of print. doi:.https://doi.org/10.1007/s11150-020-09496-w
4 McMichael TM , Currie DW , Clark S , Pogosjans S , Kay M , Schwartz NG , et al.; Public Health–Seattle and King County, EvergreenHealth, and CDC COVID-19 Investigation Team. Epidemiology of Covid-19 in a Long-Term Care Facility in King County, Washington. N Engl J Med. 2020;382(21):2005–11. doi:.https://doi.org/10.1056/NEJMoa2005412
5 Patel MC , Chaisson LH , Borgetti S , Burdsall D , Chugh RK , Hoff CR , et al. Asymptomatic SARS-CoV-2 infection and COVID-19 mortality during an outbreak investigation in a skilled nursing facility. Clin Infect Dis. 2020:ciaa763. doi:.https://doi.org/10.1093/cid/ciaa763
6 Britton T , Ball F , Trapman P . A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2. Science. 2020;369(6505):846–9. doi:.https://doi.org/10.1126/science.abc6810
7 Ajrouch KJ , Blandon AY , Antonucci TC . Social networks among men and women: the effects of age and socioeconomic status. J Gerontol B Psychol Sci Soc Sci. 2005;60(6):S311–7. doi:.https://doi.org/10.1093/geronb/60.6.S311
8 Moser A , Carlander M , Wieser S , Hämmig O , Puhan MA , Höglinger M . The COVID-19 Social Monitor longitudinal online panel: Real-time monitoring of social and public health consequences of the COVID-19 emergency in Switzerland. PLoS One. 2020;15(11):e0242129. doi:.https://doi.org/10.1371/journal.pone.0242129
9 Howard MC . A Review of Exploratory Factor Analysis Decisions and Overview of Current Practices: What We Are Doing and How Can We Improve? Int J Hum Comput Interact. 2016;32(1):51–62. doi:.https://doi.org/10.1080/10447318.2015.1087664
10 Jarvis CI , Van Zandvoort K , Gimma A , Prem K , Klepac P , Rubin GJ , et al.; CMMID COVID-19 working group. Quantifying the impact of physical distance measures on the transmission of COVID-19 in the UK. BMC Med. 2020;18(1):124. doi:.https://doi.org/10.1186/s12916-020-01597-8
11 Latsuzbaia A , Herold M , Bertemes J-P , Mossong J . Evolving social contact patterns during the COVID-19 crisis in Luxembourg. PLoS One. 2020;15(8):e0237128. doi:.https://doi.org/10.1371/journal.pone.0237128
12 von Wyl V , Höglinger M , Sieber C , Kaufmann M , Moser A , et al. Are COVID-19 proximity tracing apps working under real-world conditions? Indicator development and assessment of drivers for app (non-)use. Epidemiology. 2020. (Preprint). doi:.https://doi.org/10.1101/2020.08.29.20184382
The Swiss COVID-19 Social Monitor has received funding from the Federal Office of Public Health and from Health Promotion Switzerland. The funders had no influence on the design, conduct, analyses and publications.
The authors declare no conflict of interest with respect to this study, submission or publication of this manuscript