Figure 1 Inclusion process.
DOI: https://doi.org/10.4414/smw.2020.20398
Non-pharmaceutical interventions, including social distancing, wearing masks and lockdown measures, have been at the forefront of outbreak control during the COVID-19 pandemic. Although effective at containing viral spread, lockdown measures can have devastating consequences on society, causing businesses to stop operating [1], a loss of learning [2], and indirect deleterious health-related outcomes [3]. Immunity certificates from anti-SARS-CoV-2 serological testing, and eventually vaccination certificates, have been proposed as alternative solutions to lockdown measures in certain contexts. Serological testing is based on the identification of anti-SARS-CoV-2 antibodies, which a person would theoretically develop after contracting the disease. Some countries, including Germany [4], the UK [5] and Chile [6], have suggested the use of certificates as a path out of the current measures while ensuring public health safety. However, attempts to put such a system in place have been discouraged by low overall seroprevalence estimates of anti-SARS-CoV-2 antibodies around the world [7, 8]. The World Health Organization (WHO) [9] and other international bodies [10] have also cautioned against their use prior to obtaining answers on the interpretability of serological testing and the ethical and privacy aspects around disclosing or requesting serological information.
Viewpoints have been published about immunity certificates, but to date no clear consensus has been reached. Persad et al. [11] argued that immunity-based licenses are not unethical in principle, while Hall et al. [12] raised concerns about potential risks of discrimination, fraud and lack of standardisation. Notably, there is to date no population-based data available on perceptions of immunity certificates.
Recognising this, we conducted a survey within the framework of the SEROCoV-POP study, a population-based anti-SARS-CoV-2 IgG serosurvey in Geneva, Switzerland [7], to assess the social and individual perceptions of immunity and vaccination certificates, taking into account potential socio-demographic characteristics.
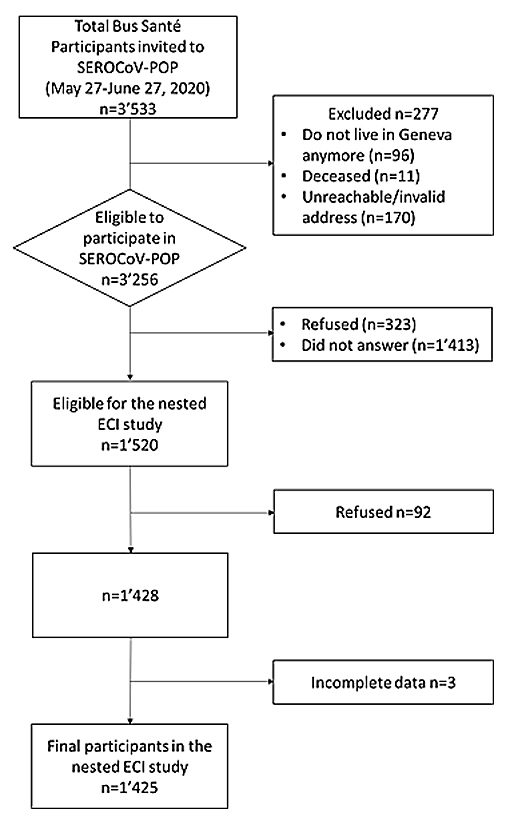
From May 27 to June 27, 2020, a self-administered questionnaire (ECI: survey on immunity certificates, “étude sur les certificats immunitaires”) was proposed to all individuals 18 years and older participating in the SEROCoV-POP study [7]. The SEROCoV-POP study participants were recruited from the Bus Santé study [13] (an annual health examination survey of a sample representative of the Geneva population). All individuals gave their consent and the study was approved by the Cantonal Research Ethics Commission of Geneva, Switzerland (CER 16-363). As information collected from subjects who consented to participate in a seroprevalence study may be influenced by participation bias, the questionnaire was also, over the same period, sent to individuals from the Bus Santé study who were invited to participate in the SEROCoV-POP study but refused or did not respond. The questionnaire (supplementary table S1 in appendix 2) was collaboratively constructed by physicians (IG, MN), epidemiologists (IG, SS), a sociologist (CBJ) and an ethicist (SH). The questionnaire covered the reasons for undergoing serological testing, contexts where immunity certificates would be useful, perceived risks of immunity certificates, and potential future uses of immunity certificates if a vaccine became available. The questionnaire also included an introduction explaining the lack of current data on the interpretability of serology testing. Answers were based on a 5-point Likert scale with the following categories: “strongly agree”, “agree”, “neutral”, “disagree”, and “strongly disagree”. The categories “strongly agree” and “agree” were later combined, as were “strongly disagree” and “disagree”. Results are reported as percentages, and only comparisons with statistically significant differences are mentioned (p <0.05).
A flow chart of patients included in and excluded from the SEROCoV-POP study as well as the nested study reported here is presented in figure 1.
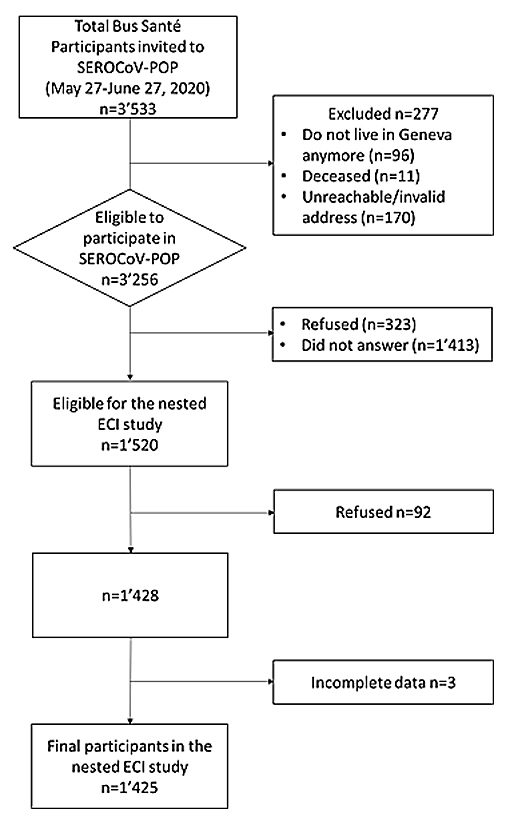
Figure 1 Inclusion process.
Overall, 1425 SEROCoV-POP participants completed the questionnaire (response rate 93%). Mean age was 52 ± 15.1 (standard deviation, SD) years and 51.9% of the participants were women. The participants’ characteristics are shown in table 1, and results and stratifications are available in the supplementary material. Additionally, as part of a separate analysis to explore potential participation bias, the questionnaire was sent to 1,736 individuals who did not participate in the SEROCoV-POP study, of which 270 answered the questionnaire (response rate 15.6%). These 270 had a mean age of 56.1 ± 15.2 (SD) years, and 46.3% were women (further characteristics in table S2, appendix 2).
Table 1 Participant characteristics.
| n = 1425 | |
|---|---|
| Age | |
| Mean ± SD (years) | 52.0 ± 15.1 |
| n (%) | |
| Age categories (years) | |
| Less than 40 | 303 (21.3) |
| 40–64 | 811 (56.9) |
| 65 and above | 311 (21.8) |
| Gender | |
| Female | 740 (51.9) |
| Male | 685 (48.1) |
| Education level | |
| Compulsory education | 73 (5.1) |
| Apprenticeship | 221 (15.5) |
| Upper secondary education | 263 (18.5) |
| University | 721 (50.7) |
| Doctorate | 83 (5.8) |
| Does not wish to answer | NA |
| No diploma | NA |
| Other | 61 (4.3) |
| Work status | |
| Retired | 338 (23.8) |
| Student | 97 (6.8) |
| Salaried | 746 (52.5) |
| Independent | 127 (8.9) |
| Unemployed | 95 (6.7) |
| Disability | NA |
| Other | 19 (1.3) |
| NA = not applicable; SD = standard deviation | |
Subjects who had participated in the SEROCoV-POP study had mostly done so to help advance research (78.3%), and only 4.8% reported having symptoms as a reason for participating in the serology testing.
Overall perceptions of serology testing and immunity certificates are summarised in figure 2. Results stratified by age, gender, education level and work status are presented in table S3 in appendix 2.
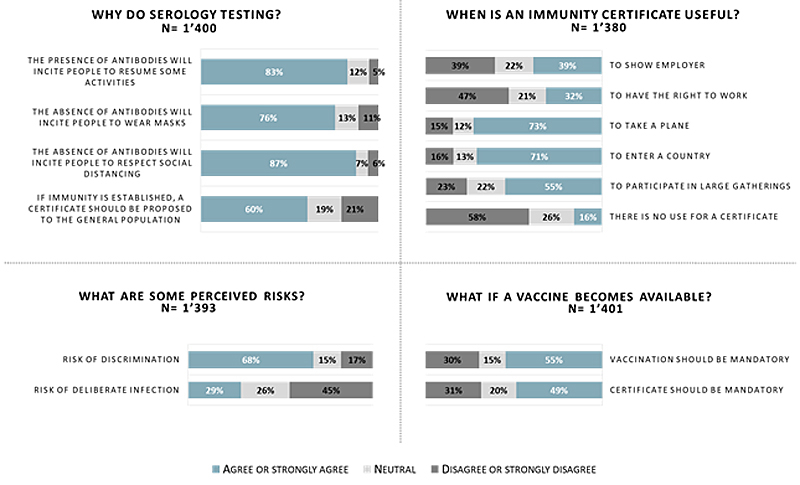
Figure 2 Overall serology testing and immunity certificate perceptions.
When asked about why serological testing would be useful, about 80% agreed that the presence of antibodies would encourage people to resume activities they had otherwise foregone, while 76% of subjects agreed that the absence of antibodies would encourage people to wear masks (80.8% of individuals 65 years and older, 76.2% of individuals 40-64 years old and 69% of individuals less than 40 years old; p = 0.01). Similarly, 87.4% of subjects agreed that the absence of antibodies would encourage people to respect social distancing measures (89.3% in individuals 65 years and older, 88.7% in individuals 40-64 years old and 82% in individuals less than 40 years old; p = 0.01)
About two thirds of the participants reported that certificates should be offered to the general population if immunity was established. The contexts where immunity certificates were perceived as potentially most useful were taking a plane (73% of participants) and entering a country (72%), while fewer participants agreed with certificates being useful for participating in large gatherings (55%) or for the right to work (32%). When stratified by occupational status, a lower proportion of participants who were (or were eligible to be) in the workforce agreed with certificates being useful for the right to work: 29.3% of salaried and 27.7% of unemployed individuals versus 44.2% of students and 34.9% of retirees (p <0.001).
When asked about perceived risks relating to immunity certificates, 67.7% of participants agreed that there is a risk of discrimination against those without immunity and 28.6% agreed that there is a risk of deliberate infection in order to acquire immunity. The perception of a risk of discrimination was more common in younger individuals (75.7% in subjects less than 40 years old, 67.9% in subjects 40–64 years old and 59.2% in subjects 65 years and older; p <0.001). The perception of a risk of discrimination was also more common in participants with a higher level of education (73% in subjects with a university or doctorate degree versus 59.7% in subjects with compulsory education, an apprenticeship or upper secondary education; p <0.001). More students agreed that there was a risk of deliberate infection (58%) compared to other groups.
When asked about future uses of immunity certificates if an effective vaccine became available, 55% of participants agreed that vaccination should be mandatory (62.3% of men versus 47.9% of women, p <0.001; and 62.7% of individuals 65 years and older, 51.9% of individuals 40–64 years old and 54.3% of individuals less than 40 years old, p = 0.003). About half of participants (49%) agreed that a vaccination certificate should be mandatory (54.1% of men vs 43.8% of women, p <0.001; and 58.6% of individuals 65 years and older, 46% of individuals 40–64 years old and 46% of individuals less than 40 years old, p <0.001).
Of the subjects who had not participated in the SEROCoV-POP study but who answered this questionnaire (n = 270), three of the main reasons for not participating in the serology testing were lack of time (30.8%), that the subjects did not think they were infected (12.5%), or that they did not want to get out of lockdown (8.7%) (table S4, appendix 2). Subjects in this group had similar results to the rest of the participants: 74.8% agreed that the presence of antibodies would encourage people to resume activities they had foregone, 86.7% agreed that the absence of antibodies would encourage people to wear masks, and 88.8% agreed that the absence of antibodies would encourage people to respect social distancing. Also, 73% agreed that certificates would be useful for taking a plane, 74.6% for entering a country, 57.3% for participating in large gatherings and 48.6% for the right to work. Fewer subjects in this group agreed that there was a risk of discrimination (51.7% vs 67.7% in the serosurvey participants; p <0.001), or of deliberate infection (20.7% vs 28.6% in the serosurvey participants; p = 0.02). If an effective vaccine were established, 59.3% of these subjects agreed that vaccination should be mandatory, and 53% agreed that a vaccination certificate should be mandatory.
We found that in a general adult population sample from Geneva, Switzerland, anti-SARS-CoV-2 serological testing is perceived to be useful, and participants can envisage scenarios where immunity certificates would be applicable. While the interpretability of antibodies is yet to be determined, if they correlate well with immunity, our results suggest they could influence individuals’ behaviour. Younger individuals less frequently believed that the absence of antibodies would encourage people to wear masks, potentially a sign of more risk taking in this population, which suggests a targeted way to reinforce public health messaging.
Linking serological results to certain rights, as immunity certificates would intrinsically be designed to do, raises ethical and societal concerns [12, 14]. It could also, however, be useful for certain goals. Our results show that the general population does consider such certificates to have some utility in specific contexts, including travel and entering countries. Human rights aspects, as well as economic and social consequences, need to be balanced against the utility of public health measures in controlling outbreaks, so that the least restrictive path is chosen [15].
When addressing controversies surrounding immunity certificates, the issues of discrimination and privileging those with immunity are raised. Indeed, authors have argued that immunity certificates could create a world of haves and have-nots [16], a risk also perceived in our study. It is important to note, however, that lockdowns can also widen the societal gap, affecting those who are socio-economically vulnerable the most [17]. Immunity certificates also raise the issue of freedom of choice and decision-making at the individual level. As long as a vaccine is not available, individuals cannot choose to be immune, thus increasing the risks of discrimination and deliberate infection. Only a minority of participants agreed that there was a risk of deliberate infection, and only 55% agreed that a vaccine should be mandatory once established. This could be a reflection of a society that is less prone to accepting mandatory measures and that values freedom of choice. Of note, men seemed to be more in favour of vaccination and vaccination certificates than women, as did older individuals.
While some editorials have been published, to our knowledge this is the first population-based survey contributing information to the overall perceptions of immunity certificates, especially in the general public. Limitations include administering the questionnaire during a pandemic and immediately following a strict lockdown, which could create a higher degree of acceptance of any solution to controlling the disease while removing restrictions. As is usual in survey research, participants are unlikely to be aware of all the advantages and disadvantages of the studied intervention. While the answers from individuals who did not participate in the SEROCoV-POP study were very similar to those from individuals who did participate, the low response rate (15.6%) of subjects who did not participate in the SEROCoV-POP study means we cannot exclude the potential for participation bias. Stratification also showed that 51% of participants had a university degree, which may not be representative of the general population in terms of education level.
Seroprevalence estimates of anti-SARS-CoV-2 antibodies remain low [7] to date, and the interpretability of serological testing and immunity remains undefined. If the current scientific uncertainties were lifted, however, and governments or institutions chose to implement immunity or vaccination certificates, differences in the perceptions of such certificates based on the context and on socio-demographic characteristics should be taken into account to limit inequalities and mitigate risks. Implementation should be accompanied by the widespread availability of any solution (i.e., an effective vaccine), as well as awareness and education campaigns empowering individuals to selectively disclose and use their seroprevalence status to benefit both the individual and society.
Silvia Stringhinia,b,c, Idris Guessousa,b, Andrew S. Azmana,d,e, Hélène Bayssonb, Prune Collombeta,b, David De Ridderb, Paola d’Ippolitoa, Yaron Dibnera, Natalie Franciolia, Kailing Marcusa, Chantal Martineza, Natacha Noela, Francesco Pennacchioa, Dusan Petrovica,c, Attilio Picazioa, Giovanni Piumattia,h, Jane Portiera, Caroline Pugina, Barinjaka Rakotomiaramananaa, Aude Richarda,d, Stephanie Schrempfta, Maria-Eugenia Zaballaa, Ania Wisniaka,d, Antoine Flahaulta,b,d, Isabelle Arm Vernezi, Olivia Keiserd, Loan Matterap, Magdalena Schellongovab, Claudine Burton-Jeangrosm, Laurent Kaiserb,f,i,n, Pierre Lescuyerf, Géraldine Poulainf, Nicolas Vuilleumierb,f, Sabine Yerlyf,i, Sultan Bahtab, Jonathan Barbolinib, Rebecca Butzbergerb, Sophie Cattanib, Alioucha Davidovicb, Antoine Daenikerb, Eugénie de Weckq, Céline Dubasb, Joséphine Ducb, Céline Eelbodeb, Benoit Favreb, Alice Gilsonb, Julie Guérinb, Lina Hassarb, Aurélia Hepnerb, Francesca Hovagemyanb, Melis Kirb, Fanny-Blanche Lombardb, Amélie Machb, Eva Marchettib, Soraya Maretb, Kourosh Massihab, Virginie Mathey-Doretb, Tom Membrezb, Natacha Michelb, Emmanuelle Mohbatb, Hugo-Ken Ouleveyb, Irine Sakvarelidzeb, Milena Stimecb, Kor-Gaël Toruslub, Nawel Tounsib, Natacha Vincentb, Manon Willb, Alenka Zeballos Valleb, François Chappuisa,b, Delphine Courvoisiera, Nacira El Merjania, Laurent Gétaza,b, Mayssam Nehmea, Febronio Pardos, Guillemette Violott, Sylvie Welkera, Alison Chiovinia, Odile Desvachezp, Benjamin Emeryc, Acem Gonula, Samia Hurstg, Gaëlle Lamours, Yasmina Malima, Philippe Matutea, Jean-Michel Maugeys, Aleksandra Mitrovica, Didier Pittetl, Klara M. Posfay-Barbeb,j, Jean-François Pradeaus, Christiane Rocchia Finea, Lilas Salzmann-Bellarda, Mélanie Seixas Miranda, Michel Tacchinos, Sophie Theurillatr, Mélissa Tomasinia, Didier Tronok, Zoé Waldmannb
a Division of Primary Care, Geneva University Hospitals, Geneva, Switzerland
b Faculty of Medicine, University of Geneva, Geneva, Switzerland
c University Centre for General Medicine and Public Health, University of Lausanne, Switzerland
d Institute of Global Health, Faculty of Medicine, University of Geneva, Switzerland
e Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Baltimore, USA
f Division of Laboratory Medicine, Geneva University Hospitals, Geneva, Switzerland
g Institut Ethique, Histoire, Humanités, University of Geneva, Switzerland
h Faculty of BioMedicine, Università della Svizzera Italiana, Lugano, Switzerland
i Geneva Center for Emerging Viral Diseases and Laboratory of Virology, Geneva University Hospitals, Geneva, Switzerland
j Division of General Pediatrics, Geneva University Hospitals, Geneva, Switzerland
k School of Life Sciences, Ecole Polytechnique Fédérale de Lausanne (EPFL), Lausanne, Switzerland
l Infection Prevention and Control Program and World Health Organization (WHO) Collaborating Centre on Patient Safety, Geneva University Hospitals, Geneva, Switzerland
m Institute of Sociological Research, University of Geneva, Geneva, Switzerland
n Division of Infectious Diseases, Geneva University Hospitals, Geneva, Switzerland
o Division of Diagnostics, Geneva University Hospitals, Geneva, Switzerland
p Campus Biotech, Geneva, Switzerland
q Education Structure, University of Geneva, Geneva, Switzerland
r Human Resources Department, Geneva University Hospitals, Geneva, Switzerland
s Information Systems Division, Geneva University Hospitals, Geneva, Switzerland
t Division of Communication, Geneva University Hospitals, Geneva, Switzerland
Table S1: Survey instrument.
Table S2: Comparison of characteristics of subjects who participated and did not participate in SEROCoV-POP.
Table S3: Results stratified by age, gender, education level and work status (n = 1425).
Table S4: Comparison of results between subjects who participated and did not participate in SEROCoV-POP.
Appendix 2 is available as a separate file at: https://smw.ch/article/doi/smw.2020.20398.
There are no potential conflicts of interest, nor any significant financial contributions to this work. We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
We also confirm that any aspect of the work covered in this manuscript that involved human patients was conducted with the ethical approval of the Cantonal Research Ethics Commission of Geneva, Switzerland, and that such approvals are acknowledged within the manuscript.
1OECD. Evaluating the initial impact of COVID-19 containment measures on economic activity. OECD. Published June 2020. Available from: http://www.oecd.org/coronavirus/policy-responses/evaluating-the-initial-impact-of-covid-19-containment-measures-on-economic-activity-b1f6b68b/ [accessed 2020 July 18].
2Goldstein D. Research Shows Students Falling Months Behind During Virus Disruptions. The New York Times 2020 June 5. Available from: https://www.nytimes.com/2020/06/05/us/coronavirus-education-lost-learning.html [accessed 2020 July 21].
3 Roberton T , Carter ED , Chou VB , Stegmuller AR , Jackson BD , Tam Y , et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8(7):e901–8. doi:.https://doi.org/10.1016/S2214-109X(20)30229-1
4Miller J. Armed with Roche antibody test, Germany faces immunity passport dilemma. Reuters. Published 2020 May 4. Available from: https://www.reuters.com/article/health-coronavirus-germany-antibodies-idUSL1N2CM0WB [accessed 2020 July 20].
5Proctor K, Devlin H. Coronavirus UK: health passports “possible in months.” The Guardian 2020 May 4. Available from: https://www.theguardian.com/politics/2020/may/03/coronavirus-health-passports-for-uk-possible-in-months [accessed 2020 July 20].
6Laing A. Chile plans “release certificates” for recovered coronavirus patients. Reuters. Published 2020 April 9. Available from: https://www.reuters.com/article/us-health-coronavirus-chile-recovered-idUSKCN21R3EC [accessed 2020 July 20].
7 Stringhini S , Wisniak A , Piumatti G , Azman AS , Lauer SA , Baysson H , et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study. Lancet. 2020;396(10247):313–9. doi:.https://doi.org/10.1016/S0140-6736(20)31304-0
8 Havers FP , Reed C , Lim T , Montgomery JM , Klena JD , Hall AJ , et al. Seroprevalence of Antibodies to SARS-CoV-2 in 10 Sites in the United States, March 23-May 12, 2020. JAMA Intern Med. 2020;(July 21). Online ahead of print. doi:.https://doi.org/10.1001/jamainternmed.2020.4130
9World Health Organization. “Immunity passports” in the context of COVID-19. “Immunity passports” in the context of COVID-19. Published 2020 April 24. Available from: https://www.who.int/news-room/commentaries/detail/immunity-passports-in-the-context-of-covid-19 [accessed 2020 July 18].
10National COVID-19 Science Task Force (NCS-TF). Ethical, legal, and social issues associated with “serological passports.” April 2020. https://ncs-tf.ch/en/policy-briefs.
11 Persad G , Emanuel EJ . The Ethics of COVID-19 Immunity-Based Licenses (“Immunity Passports”). JAMA. 2020;323(22):2241–2. doi:.https://doi.org/10.1001/jama.2020.8102
12 Hall MA , Studdert DM . Privileges and Immunity Certification During the COVID-19 Pandemic. JAMA. 2020;323(22):2243–4. doi:.https://doi.org/10.1001/jama.2020.7712
13 de Mestral C , Stringhini S , Guessous I , Jornayvaz FR . Thirteen-year trends in the prevalence of diabetes in an urban region of Switzerland: a population-based study. Diabet Med. 2020;37(8):1374–8. doi:.https://doi.org/10.1111/dme.14206
14 Kofler N , Baylis F . Ten reasons why immunity passports are a bad idea. Nature. 2020;581(7809):379–81. doi:.https://doi.org/10.1038/d41586-020-01451-0
15 Childress JF , Faden RR , Gaare RD , Gostin LO , Kahn J , Bonnie RJ , et al. Public health ethics: mapping the terrain. J Law Med Ethics. 2002;30(2):170–8. doi:.https://doi.org/10.1111/j.1748-720X.2002.tb00384.x
16 Phelan AL . COVID-19 immunity passports and vaccination certificates: scientific, equitable, and legal challenges. Lancet. 2020;395(10237):1595–8. doi:.https://doi.org/10.1016/S0140-6736(20)31034-5
17 Wright L , Steptoe A , Fancourt D . Are we all in this together? Longitudinal assessment of cumulative adversities by socioeconomic position in the first 3 weeks of lockdown in the UK. J Epidemiol Community Health. 2020;74(9):683–8. doi:.https://doi.org/10.1136/jech-2020-214475
The members of the SEROCoV-POP study team are listed in appendix 1.
There are no potential conflicts of interest, nor any significant financial contributions to this work. We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
We also confirm that any aspect of the work covered in this manuscript that involved human patients was conducted with the ethical approval of the Cantonal Research Ethics Commission of Geneva, Switzerland, and that such approvals are acknowledged within the manuscript.