Ventilatory weaning and early rehabilitation in COVID-19-related acute respiratory distress syndrome: the experience at Locarno hospital, canton of Ticino, Switzerland
DOI: https://doi.org/10.4414/smw.2020.20397
Ruben
Forniab, Tea
Besanac, Antonio
Amitranod, Camelia
Voineae, Adam
Ognaf
aCreoc Physical Therapy Service,
b
cSpeech Therapy Service,
dSpeech Therapy Service,
eRespiratory Medicine Service,
fRespiratory Medicine Service, La Carità Hospital, Locarno,
Ventilatory weaning and early rehabilitation in COVID-19-related acute respiratory distress syndrome: the experience at Locarno hospital, canton of Ticino, Switzerland
Introduction
At the end of February 2020, COVID-19 made its first appearance in the southern part of Switzerland. Without protection from the Alps, and because of its proximity to Lombardy and the gatherings of people during the carnival period, the canton of Ticino witnessed a rapid and alarming epidemic. Within three months, numbers had rocketed: 3321 positive cases, 350 fatalities and 908 hospital discharges in a population of about 360,000 [1, 2]. The local public health situation reflected what was happening on a worldwide scale: the ability of clinics and health facilities to provide intensive care to patients in need of mechanical respiratory support was critically challenged.
Such an emergency made it necessary to rapidly reorganise the whole health system. One of the most successful strategies was the recruitment of the rehabilitation sector in order to reduce pressure on intensive care units.
Physiotherapists, occupational therapists and speech therapists were engaged, along with pulmonologists, in the creation of a new tracheotomy ward. Patients who had undergone percutaneous tracheotomy were transferred there and ventilated in invasive ways by means of devices normally used for ventilation at home. New protocols were defined for the management of tracheotomies, decannulation and feeding recovery.
We are currently witnessing a recrudescence of infections, and a growing number of political and medical appeals to act responsibly by applying everything we learned during the first wave. Therefore, we want to share our clinical experience in the hope that the targeted solutions which allowed us to achieve positive results will be useful.
The COVID Research Database currently contains over 111,000 articles [3]. The number of publications has increased in proportion with the pandemic’s development, leading to calls for the use of artificial intelligence to guide researchers through the remarkably rapidly growing number of works, many of which are based on the guidelines developed by other healthcare professionals. The present article describes the experiences of a heterogeneous group of rehabilitators who treated tracheostomised patients with acute respiratory distress syndrome due to COVID-19 in the period immediately following their stay in the intensive care unit (ICU). Designated as a COVID-19 centre on 11 March 2020, La Carità Hospital, Locarno (ODL) was at the forefront of the fight against COVID-19 in the Ticino in the southern part of Switzerland.
This article presents the protocols developed to support the process of weaning patients from tracheotomy and the reprisal of feeding by mouth. Critical issues in the daily management of patients and practical solutions are also described.
Methods
Cantonal organisation and internal management of the hospital
At a time when guidelines and directives had not yet been published, decisions made at all levels (political, medical and health strategic) influenced the management of the COVID-19 pandemic in Ticino and led to operational lines of conduct aimed at preventing the intensive care units’ maximum capacity from being exceeded. The canton of Ticino is served by seven public hospitals, each part of the multi-site cantonal hospital Ente Ospedaliero Cantonale (EOC), with an overall capacity of 800 beds. The ODL, with about 180 beds and an ICU which was expanded from 8 to 45 ventilator-equipped beds, was dedicated entirely to COVID-19 patients. Concentrating the COVID-19 patients together in one hospital made it possible to centralise materials and specialised staff, who faced the overwhelming amount of work in 12-hour (instead of 8-hour) shifts. In addition, on 17 March 17 2020, one of the internal medicine wards (Medicine B) of the ODL began to be converted into a tracheotomy ward with a capacity of 24 beds, whose first patient was admitted on 20 March 2020. The transfer of post-tracheotomy patients in a relatively stable condition – but still needing ventilatory aid – to the tracheotomy ward relieved the pressure on the ICU, which never reached its saturation point. The lack of specialist staff led to the adoption of instruments normally used for home ventilation, mostly of the bilevel positive airway pressure (BiPAP) type. Since the patients transferred to the tracheotomy ward needed constant surveillance, cameras connected to the monitors were installed. Vital parameters (saturation, pressure, heart rate and respiratory rate) were regularly verified through monitors and frequent medical and nursing checks.
Tracheotomy interventions
Due to the need to free up the ICU beds while continuing to perform invasive ventilation, percutaneous tracheotomy was systematically performed by surgeons supported by pneumologists.
Tracheostomy was performed as soon as the respiratory situation of the patient was stable, with no more need for prone positioning and with the possibility of decreasing the positive end-expiratory pressure to values ≤10 cm H2O. Contraindications to tracheostomy were a coagulation disorder or hemodynamic instability requiring increasing doses of vasoactive drugs. The mean (± standard deviation) time from intubation to tracheostomy was 12.6 (±5.7) days.
The percutaneous technique was preferred to the surgical one for its rapidity and relative simplicity, together with the rarity of bleeding episodes [4–6]. Furthermore, percutaneous tracheotomy can be executed at the patient’s bed, thus avoiding risky displacements and any further interventions to close the ostomy.
Managing the tracheotomy
The ongoing care emergency didn’t allow the implementation of a regular training plan for health care staff not trained to manage tracheotomies. Thus, the creation of a simple operative protocol allowed us to monitor a patient’s progression towards weaning and to avoid mistakes while managing the tracheal cannula. The protocol shown in table 1 describes tracheal cannula settings at levels to be implemented at different times of the day. Every change in level and each modification of the tracheal cannula setting was carried out exclusively by the speech therapist or by other professionals with specific skills, such as physiotherapists specialised in respiratory physiotherapy.
Table 1 Tracheo level index (TLI)
| |
Tracheal cannula configuration
|
When
|
| Level 1 (baseline) |
Closed inner cannula, inflated cuff |
Always |
| Level 2 |
Closed inner cannula, deflated cuff |
If patient is awake, sitting or in bed |
| Level 3 |
Fenestrated inner cannula, deflated cuff |
If patient is awake, sitting or in bed |
| Level 4 |
Fenestrated inner cannula, deflated cuff and speaking valve |
If patient is awake, sitting or in bed |
Removal of tracheotomy
Choosing the ideal time to remove the tracheotomy was of major importance because it was not possible to rely on intermediate steps such as a Mini-Trach cannula, and also because avoiding returns to the ICU was essential. Therefore, pneumologists created the score illustrated in table 2. The table shows the prerequisites that patients had to meet for decannulation to be considered. Decannulation was only performed when they reached a total of four points upon the medical team assessing their complete clinical picture.
Table 2 Tracheo score index (TSI).
| 1 point |
Patient oriented |
| 1 point |
Patient can stay 24 h with the artificial nose without ventilation |
| 1 point |
Good cough reflex, patient can stay with deflated cuff and speaking valve or artificial nose without any aspiration |
| 1 point |
Patient does not need deep tracheal aspirations |
In addition to its rapidity and simplicity, the above protocol allows the physician to obtain a picture of the patient’s clinical state over a 24-hour period and not only at the time of the daily visit.
Recovery of feeding by mouth
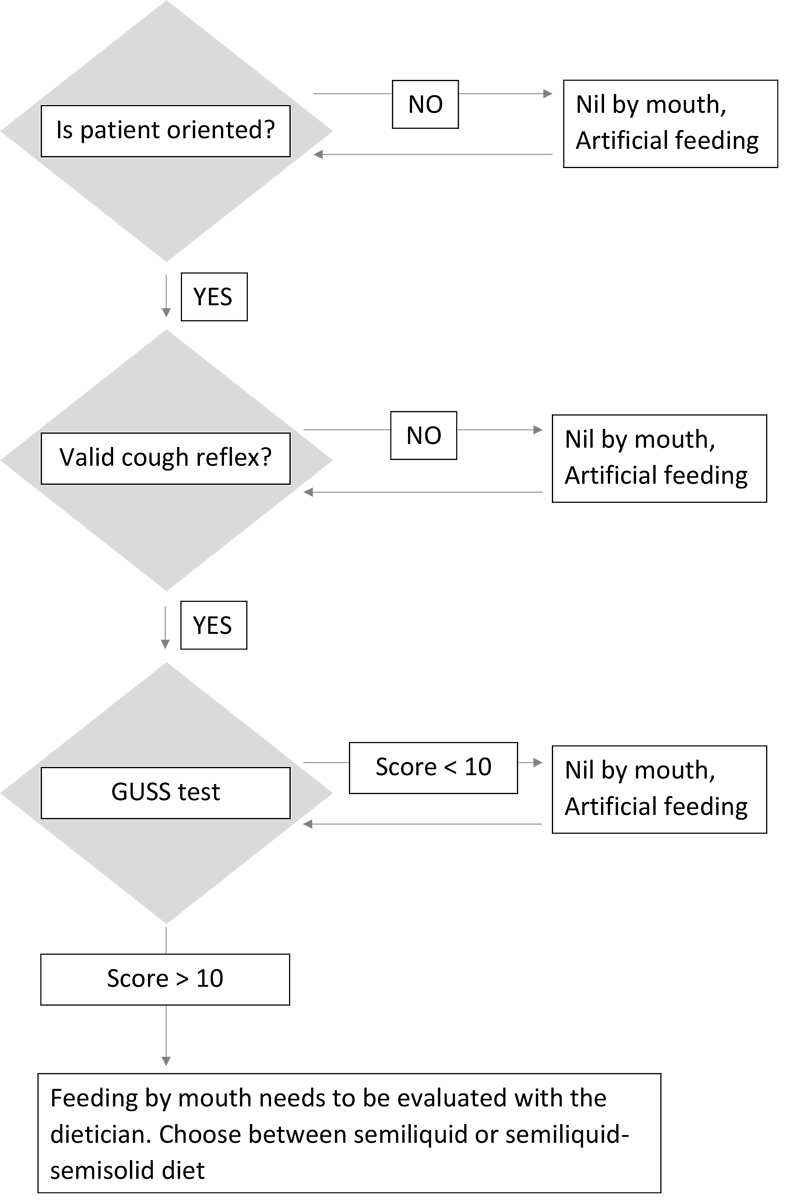
All patients transferred to the tracheotomy ward were fed enterally through a nasogastric tube. To avoid problems due to prolonged use of the nasogastric tube, once a patient’s respiratory condition was stable, an evaluation of their swallowing was carried out in order to verify the possibility of weaning from enteral feeding [7]. The pandemic context and the human and technical resources available made diagnosing dysphagia instrumentally by means of a fibreoptic endoscopic evaluation of swallowing only possible in rare and exceptional cases. A non-instrumental clinical swallowing examination protocol based on a precise bedside evaluation of swallowing was adopted. In order to avoid aspirations and related pulmonary complications for patients already in a critical respiratory condition [7], the clinical swallowing examination was carried out by the speech therapist or the swallowing therapist, who were the most specialised and experienced staff. To proceed to the evaluation of swallowing by means of the meshed, single-use, inner cannula and the phonatory valve, the patients had to be sitting in an armchair, with the cuff having been deflated for at least 30 minutes, and have normal vital parameters. Otherwise, they had to retain a non-meshed cannula and an artificial nasal tube. If the patient was fully conscious with a normal cough reflex, a Gugging Swallowing Screen (GUSS) test [8, 9] was carried out. Thus, at least as a first evaluation, the test with solid food was omitted, with semi-solid and liquid foods preferred (respectively, Acqua Gel by Nutricia Nutilis and still water). This method was adopted to shorten the time of food administration, consequently reducing the health care workers’ time of exposure and thus the risk of contagion. The assessment of swallowing is in fact subject to the production of droplets and aerosols. The results of the GUSS test determined the choice of nutritional modality. Patients who scored above 10 points could proceed to weaning on a semi-solid and semi-liquid diet and hydration by Acqua Gel, whereas scores under 10 points required further evaluation and confirmed feeding by tube. The flowchart in figure 1 shows the complete protocol adopted.
Results
Despite the high number of cases and the staff’s working conditions, the results were excellent.
Tracheotomy
The choice of percutaneous tracheotomy was confirmed to be successful, as bleeding episodes calling for surgical intervention were limited to 5% of patients. All decannulations were carried out at the patient’s bed, fairly rapidly and without complications. Droplet and aerosol management turned out to be effective, with a COVID-19-positive case rate among staff similar to that in non-COVID-19 hospitals.
Management and removal of tracheotomy
The use of the protocols TLI (table 1) and TSI (table 2) proved effective. All 50 patients of the tracheotomy ward were weaned from ventilation and decannulated before discharge and transfer to rehabilitation clinics. None of the decannulated patients in the tracheotomy ward needed a further cannulation.
Resumption of feeding by mouth
All patients hospitalised in the tracheotomy ward had been weaned off enteral nutrition and had already begun to feed by mouth upon discharge. The process of nutritional therapy through evaluation with a “modified GUSS test” led to positive outcomes. None of the patients of the tracheotomy ward showed pulmonary complications due to aspiration. All of them could start to feed and hydrate by mouth safely.
Discussion
During the peak of the pandemic in April and May 2020, the ODL cared for 466 patients, 97 of whom were treated in the ICU. A total of 86 fatalities were recorded in the hospital. Of the 53 patients who underwent tracheostomy, 3 (5.7%) died in the ICU before being transferred to the tracheotomy ward and 5 (9.4%) died after being transferred to the tracheotomy ward.
The average hospital stay was 13 days for all patients, and 21 days for patients requiring intensive care.
Taking care of these patients’ respiratory problems with home ventilation devices proved to be an effective solution. First of all, they turned out to be easy to operate, even for untrained nursing staff. In addition, the possibility of monitoring ventilation through secure digital (SD) cards allowed fast and accurate interventions and corrections. Only three cases of readmission (bounce back) to the ICU were recorded, mostly due to infectious complications that could not be managed by the tracheotomy ward.
The excellent results regarding resumption of oral feeding were largely due to the fact that dysphagia in patients affected by COVID-19 is often the result of post-extubation dysphagia [10]. Many studies have shown that prolonged orotracheal intubation has negative effects on swallowing ability, such as changes in the anatomic conformation of the glottis, atrophy of the muscles involved during swallowing, decreased sensibility and decreased cough reflex [11]. In our case, dysphagia might have been a transitory symptom due to the fact that tracheotomy was performed quickly and patients were intubated for a relatively short period. Nonetheless, in the tracheotomy ward dysphagia was attentively monitored and approached according to physiological recovery times, thus preventing negative effects of early or late weaning. Some patients’ dysphagia was related to a general asthenia which affected orofacial muscular structures, thus leading to particularly weak tongue thrusting. Given the emergency context and the particular setting, it was impossible to provide personalised therapy for all patients. Therefore, a programme of oral motricity stimulation was adopted, along with a specific set of exercises that patients could carry out autonomously [12].
In these patients, a recovery of a good oral motricity has been recorded along with an increase in tongue strength, with the consequent improvement and efficiency of the oral phase. Some cases showed a critical laryngeal desensitisation, likely due to prolonged intubation and the necessity of keeping the cuffed cannula in use. The possibility of using the uncuffed cannula led to a remarkable improvement in this respect.
According to our experience, the GUSS test [8, 9] proved satisfactory for screening for dysphagia in a non-neurological population, although it was tested in a neurological population.
Conclusion
Our experience, although limited, allows us to draw some important conclusions which may become useful in the current context of increasing numbers of COVID-19 patients needing hospitalisation.
Concentrating the COVID-19 patients in one hospital and the creation of a tracheotomy ward simplified the work on a logistical level, as well as simplifying the allocation of available resources. In the case of excessive pressure on the ICU, undertaking percutaneous tracheotomy on patients subsequently transferred to adapted subacute wards proved to be a successful solution, which freed up beds in the ICU.
Percutaneous tracheotomy provided good results and allowed surgeons to adapt to a technique that was normally used by pneumologists and intensivists. Patients with percutaneous tracheotomy can be ventilated efficiently by means of instruments normally used for home ventilation, such as BiPAP (for example ResMed Stellar), which are simpler than the conventional ventilators in use in the ICU. These devices can be successfully handled by nursing staff who are not specialised in the ICU as long as they are provided with correct instructions.
These months of work at the ODL have shown us the complexity that treating COVID-19-affected patients entails, due to the patients’ fragility and the particular setting in which the work was carried out.
The positive outcome of this experience was guaranteed by excellent interprofessional cooperation, the real keyword of these last few months, which allowed us to provide adequate care to all patients. On the other hand, in the initial phase of the pandemic, when the tracheotomy ward was providing care to a large number of patients in an unstable condition, there were difficulties in defining the roles of the various therapists. At that particular time, the situation required a transprofessional rather than an interprofessional approach. The improvements in the patients’ condition allowed us to solve the problem, because it permitted the resumption of work in an interprofessional way.
Acknowledgments
We are grateful to Marco Pedroli, Careen Van Son, Brigitte Wehrli and Luca Scascighini for their valuable contributions to and support of this work.
Author contributions
The authors contributed equally to this work.
References
1Repubblica e Cantone del Ticino. Bollettino epidemiologico 05.06.2020. Published 2020. Available from: https://www4.ti.ch/dss/dsp/covid19/home/ [accessed 2020 July 3].
2Daniel P. COVID-19 Information for Switzerland. Published 2020. Available from: https://www.corona-data.ch/ [accessed 2020 July 3].
3World Health Organization. Global research on coronavirus disease (COVID-19). Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov [accessed 2020 July 5].
4
Esnault
P
,
D’Aranda
E
,
Montcriol
A
, et al.
Tracheotomia chirurgica e tracheotomia percutanea in rianimazione. EMC - Anestesia-Rianimazione. 2020. doi:https://doi.org/10.1016/s1283-0771(20)43679-5
5
Susanto
I
. Comparing percutaneous tracheostomy with open surgical tracheostomy. BMJ. 2002;324(7328):3–4. doi:.https://doi.org/10.1136/bmj.324.7328.3
6
Mallick
A
,
Bodenham
AR
. Tracheostomy in critically ill patients. Eur J Anaesthesiol. 2010;27(8):676–82. doi:.https://doi.org/10.1097/EJA.0b013e32833b1ba0
7
Fritz
MA
,
Howell
RJ
,
Brodsky
MB
,
Suiter
DM
,
Dhar
SI
,
Rameau
A
, et al.
Moving Forward with Dysphagia Care: Implementing Strategies during the COVID-19 Pandemic and Beyond. Dysphagia. 2020.Online ahead of print. doi:.https://doi.org/10.1007/s00455-020-10144-9
8
Trapl
M
,
Enderle
P
,
Nowotny
M
,
Teuschl
Y
,
Matz
K
,
Dachenhausen
A
, et al.
Dysphagia bedside screening for acute-stroke patients: the Gugging Swallowing Screen. Stroke. 2007;38(11):2948–52. doi:.https://doi.org/10.1161/STROKEAHA.107.483933
9
Trapl
M
,
Firlinger
B
,
Teuschl
Y
,
Dachenhausen
A
,
Brainin
M
. International dissemination and usage of the gugging swallowing screen (GUSS). A prospective cross sectional study. In: 6th ESSD Congress Milan 2016 Abstract Book. Dysphagia. 2017;32:126–207. doi:.https://doi.org/10.1007/s00455-016-9766-y
10
Brodsky
MB
,
Pandian
V
,
Needham
DM
. Post-extubation dysphagia: a problem needing multidisciplinary efforts. Intensive Care Med. 2020;46(1):93–6. doi:.https://doi.org/10.1007/s00134-019-05865-x
11
Brown
CVR
,
Hejl
K
,
Mandaville
AD
,
Chaney
PE
,
Stevenson
G
,
Smith
C
. Swallowing dysfunction after mechanical ventilation in trauma patients. J Crit Care. 2011;26(1):108.e9–13. doi:.https://doi.org/10.1016/j.jcrc.2010.05.036
12
Adams
V
,
Callister
R
,
Mathisen
B
. Using Tongue-Strengthening Exercise Programs in Dysphagia Intervention. Asia Pac J Speech Lang Hear. 2011;14(3):139–46. doi:.https://doi.org/10.1179/jslh.2011.14.3.139