Figure 1 Flow chart.
DOI: https://doi.org/10.4414/smw.2020.20368
confidence interval
creatine kinase
creatine kinase muscle brain type
emergency medical service
emergency room
European Society of Cardiology
Fribourg STEMI Fast Track Registry
first medical contact to revascularisation
hazard ratio
interquartile range
left anterior descending
major adverse cardiac events
myocardial infarction
odds ratio
percutaneous coronary intervention
right coronary artery
ST-segment elevation myocardial infarction
Incidence rates of ST-segment elevation myocardial infarction (STEMI) are decreasing. The advent of primary percutaneous coronary intervention (PCI), potent platelet inhibitors and the implementation of STEMI networks have substantially decreased mortality after STEMI [1–3]. However, in-hospital mortality remains high, at an estimated 4–12%, and 1-year mortality as assessed in angiography registries is estimated at around 10% [4–6].
Several factors may impact clinical outcomes after STEMI. Time delays are one factor that can be modified by healthcare providers. Based on data from large registries, the 2012 European Society of Cardiology (ESC) STEMI guidelines set clear quality targets for STEMI networks, with recommended delays of <90 minutes from first medical contact and of <12 hours from symptom onset to primary PCI in all patients with a diagnosis of STEMI [7]. The 2017 guidelines reinforced the importance of system-dependent delays, with primary PCI recommended within 90 minutes of diagnosis, and within 60 minutes in cases of direct presentation to a primary PCI centre. Fibrinolysis is still recommended when delays between diagnosis and reperfusion exceed 120 minutes [7].
We undertook a formal analysis of the system-dependent component of our local STEMI network and sought to identify predictors and potentially modifiable factors of treatment delays. We then aimed to compare the clinical outcomes at 3 years between patients treated within the ESC-recommended interval of first medical contact (FMC) to PCI of <90 minutes and those presenting with longer intervals.
EVALFAST is a retrospective and prospective single centre registry. Data were collected retrospectively from 2008, and prospectively from 2010 onwards. All patients with a suspected diagnosis of STEMI who were referred to the University and Hospital Fribourg via the local STEMI network were eligible. Patients in whom the definite diagnosis was not STEMI and those unwilling or unable to provide written informed consent or to participate in follow-up were excluded. Baseline patient and procedural characteristics, as well as time delays, were collected. Clinical follow-up was performed by phone or clinic visit at 1 month, 1 year, and yearly up to 5 years. The study complied with the Declaration of Helsinki and was approved by the local ethics committee at University and Hospital Fribourg (protocol no 001-R-CER-FR). The study population includes all patients enrolled from June 2008 to December 2014 in whom the FMC time was known. Data for this analysis were extracted from the EVALFAST registry in 2018.
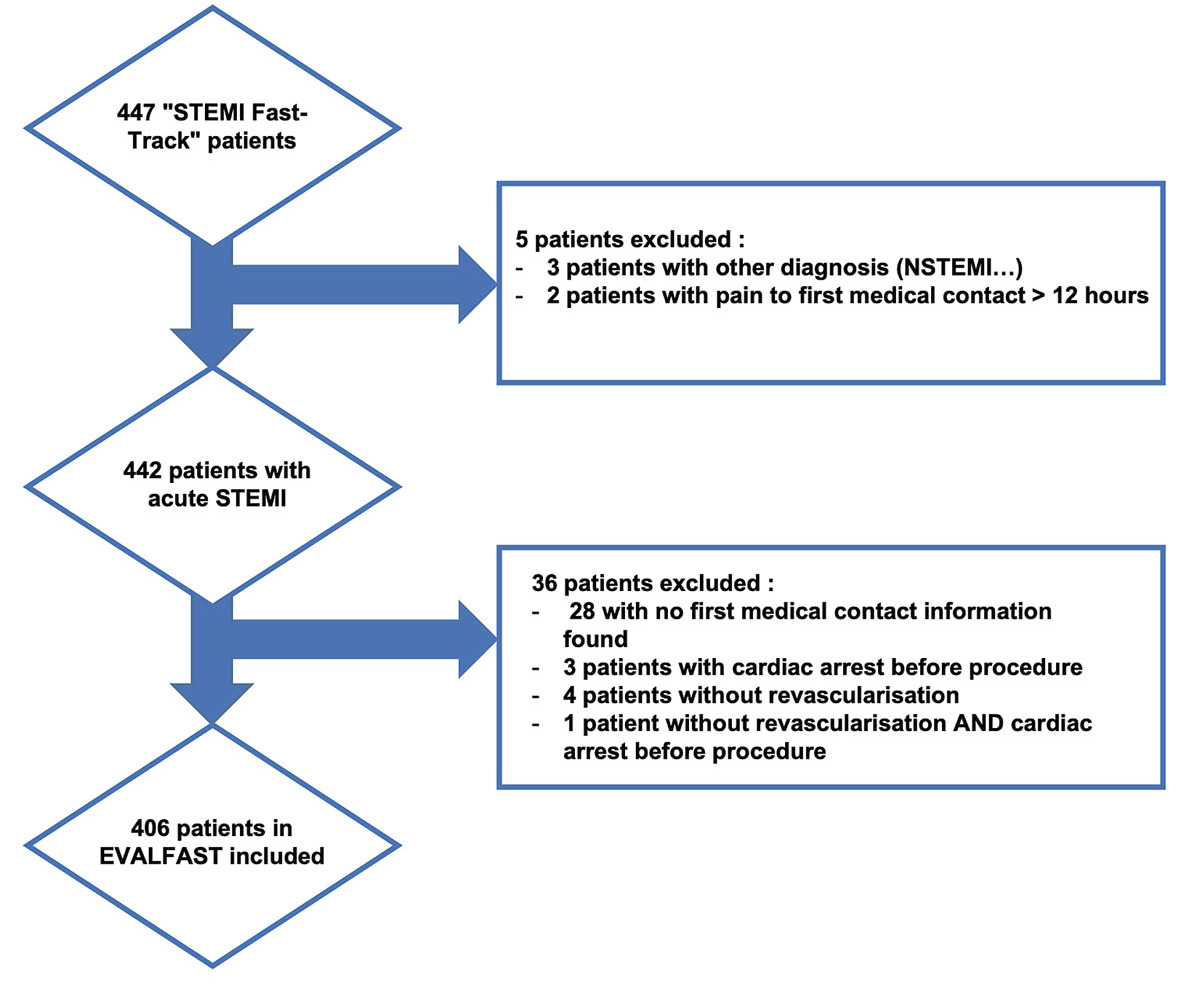
The STEMI Fast Track Network Fribourg began in June 2008. It includes one catheterisation laboratory facility providing 24h/7d primary PCI to six referring hospitals, covering a population of 320,000 inhabitants over 1,600 km2. In case of symptoms suggestive of myocardial infarction and typical electrocardiogram signs (ST elevation, presumed new left bundle branch block or ST depression in leads V1-V3 at FMC), STEMI was to be suspected, and the fast track procedure initiated (see fig. 1). The referring hospital, ambulance emergency medical service or the general practitioner (GP) contacted the on-call intensive care physician who triaged, confirming or not the diagnosis of STEMI, in collaboration with the on-call interventional cardiologist.
Patients with confirmed STEMI were transferred directly to the catheterisation laboratory of the University and Hospital Fribourg, bypassing the emergency room (ER). Medical treatment was given as soon as STEMI was suspected. From 2008 to 2009, clopidogrel was administered as a second antiplatelet agent in addition to aspirin. From 2009, ticagrelor and prasugrel were available, and these were preferentially prescribed over clopidogrel [8, 9]. As the patients were enrolled between June 2008 and December 2014, primary PCI was performed according to the 2008 ESC recommendations for the management of acute myocardial infarction in patients presenting with persistent ST-segment elevation [10]. Manual thrombectomy was performed whenever deemed necessary by the interventional cardiologist [11].
The primary clinical endpoint was survival free from major adverse cardiac events (MACE), defined as the composite of cardiac death, nonfatal myocardial infarction and any unplanned revascularisation. Secondary endpoints were all-cause mortality, the individual components of the primary endpoint, peak creatine kinase (CK) and creatine kinase muscle brain type (CK-MB), and length of stay in days.
The onset of pain was defined as the beginning of symptoms. FMC was defined as the first assessment by a medical professional. Revascularisation time was defined as the time point of the guidewire passage through the culprit lesion. Total ischaemic time was defined as the time from symptom onset to revascularisation. Death was classified as either cardiac or non-cardiac, according to the Academic Research Consortium definition [6]. Deaths that could not be classified were considered cardiac. Unplanned revascularisation was defined as any repeat percutaneous or surgical revascularisation, regardless of location. Stent thrombosis was either definite or probable, according to the Academic Research Consortium definition [6].
Analyses were performed using SPSS software 26.0 (SPSS Inc, Chicago, IL, USA) and STATA 14 MP. Continuous variables are expressed as mean ± standard deviation or median with interquartile range (IQR). Categorical variables are expressed as counts and percentages. For continuous variables, histograms were checked for normal distribution. For the univariate analysis, baseline and procedural characteristics as well as clinical outcome were compared between patients presenting a delay from first medical contact to revascularisation (FMC-R) of <90 minutes (short) and patients presenting a delay of ≥ 90 minutes (long) using a chi-square test for categorical variables, an unpaired t-test for continuous variables with a normal distribution, and non-parametric tests such as the Wilcoxon rank sum test or the Mann-Whitney U-test for continuous variables with a non-Gaussian distribution.
To find the correlation of normally distributed variables, the Pearson product-moment correlation coefficient was calculated. For variables with a non-Gaussian distribution, Spearman's rank correlation coefficient was computed.
Crude estimates of clinical outcomes were assessed using the Kaplan-Meier method. Cox regression was used to adjust for baseline imbalances between patients with an FMC-R interval <90 minutes and patients with an FMC-R delay ≥90 minutes. To identify independent predictors of the occurrence of MACE, a statistical model was computed using Cox proportional hazards. All variables that showed a significant difference between the groups, as well as clinically relevant variables (age, gender, diabetes, treatment during working hours, three-vessel disease, presentation at ER of PCI centre, transfer from GP, total ischaemic time) were forced into the model. In an explorative analysis, we created age categories. Patients in the same decade were considered as belonging to the same age category. Patients <40 years were pooled into the same category, as were patients >90 years.
A total of 447 patients were admitted with STEMI, of whom 406 were included in the present study. The patient flowchart is depicted in figure 1. Patients were divided into two groups according to their FMC-R delay: those treated after <90 minutes (“short” group; n = 187) and those with a delay ≥90 minutes (“long” group, n = 219). Baseline characteristics are presented in table 1. All patients were considered for primary PCI. No patient received thrombolysis. Mean age was 63 ± 12 years and was significantly lower in the short vs the long group (61 ± 12 vs 65 ± 12, p = 0.001), 75% (n = 306) were men (short: 78% (n = 145) vs long: 74% (n = 161), p = 0.36). Diabetes mellitus was present in 13% (n = 25) of patients in the “short” group and in 19% (n = 41) of patients in the “long” group (p = 0.14). Patients with previous myocardial infarction were equally distributed in both groups (short: 11% (n = 20) vs long: 19% (n = 22), p = 0.83). Patients admitted during working hours were less likely to be treated early (short: 41% (n = 76) vs long: 59% (n = 130), p <0.001).
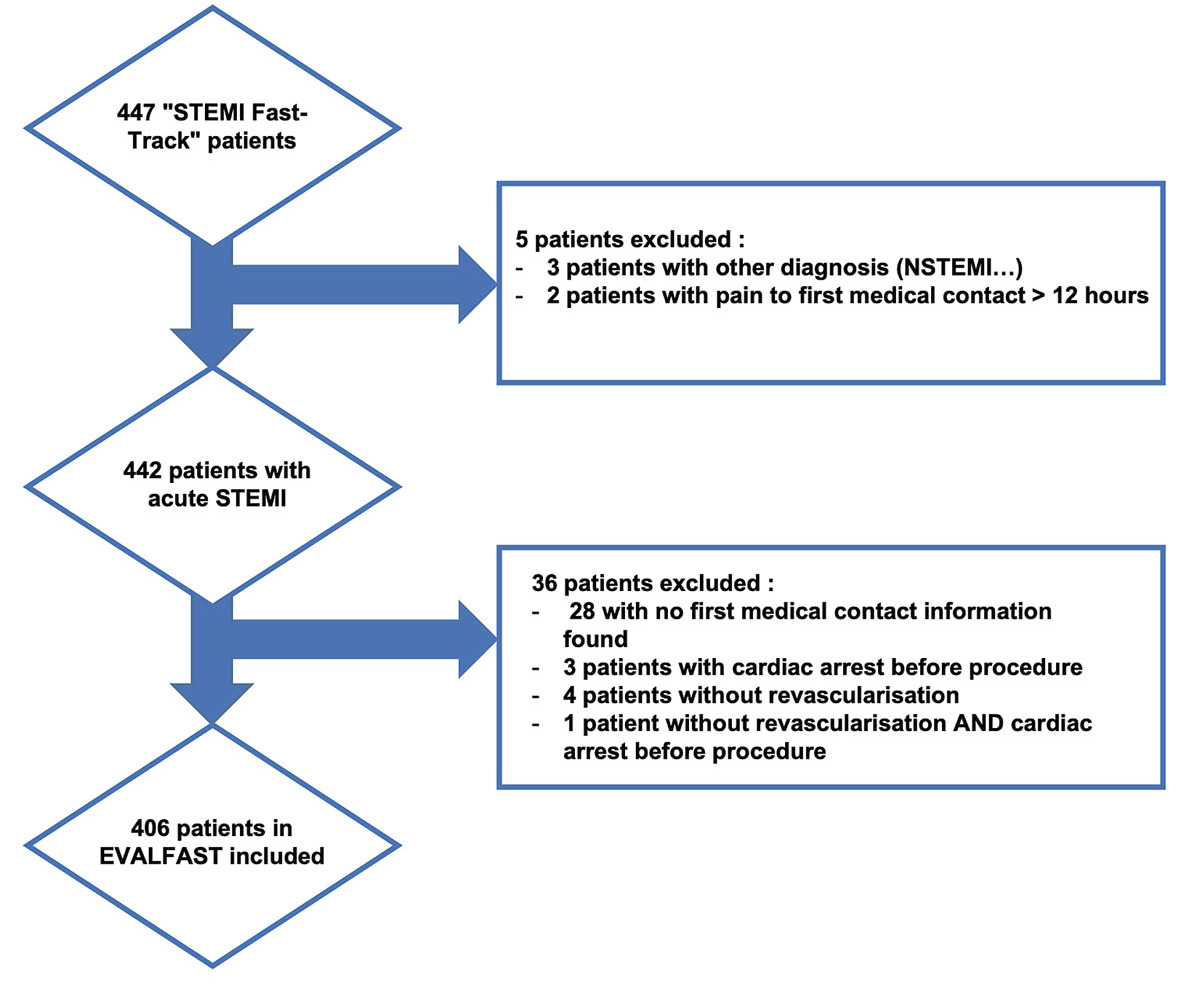
Figure 1 Flow chart.
Table 1 Baseline patient characteristics.
|
All patients
(n = 406) |
Short
(n = 187) |
Long
(n = 219) |
p-value | |
|---|---|---|---|---|
| Age (years), mean ± SD | 63 ± 12 | 61 ± 12 | 65 ± 12 | 0.001 |
| Male, n (%) | 306 (75) | 145 (78) | 161 (74) | 0.36 |
| BMI (kg/m2), mean ± SD | 26.8 ± 4.1 | 26.6 ± 4.0 | 27.0 ± 4.1 | 0.27 |
| Diabetes mellitus, n (%) | 66 (16) | 25 (13) | 41 (19) | 0.14 |
| Smoking, n (%) | 181 (45) | 86 (46) | 95 (43) | 0.62 |
| Hypertension, n (%) | 190 (47) | 92 (49) | 98 (45) | 0.37 |
| Dyslipidaemia, n (%) | 153 (38) | 69 (37) | 84 (38) | 0.76 |
| Family history, n (%) | 94 (23) | 42 (23) | 52 (24) | 0.76 |
| Previous MI, n (%) | 42 (10) | 20 (11) | 22 (10) | 0.83 |
| Previous PCI, n (%) | 59 (15) | 30 (16) | 29 (13) | 0.42 |
| Previous CABG, n (%) | 8 (2) | 2 (1) | 6 (3) | 0.23 |
| Renal failure, n (%) | 17 (4) | 7 (4) | 10 (5) | 0.68 |
| Admitted during working hours, n (%) | 206 (51) | 76 (41) | 130 (59) | <0.001 |
| Cardiogenic shock, n (%) | 21 (5) | 10 (5) | 11 (5) | 0.88 |
| Coronary artery disease | ||||
| – Single-vessel, n (%) | 160 (39) | 78 (42) | 82 (37) | 0.38 |
| – Two-vessel, n (%) | 135 (34) | 64 (34) | 71 (32) | 0.70 |
| – Three-vessel, n (%) | 111 (27) | 45 (24) | 66 (30) | 0.17 |
| Culprit lesion | ||||
| – Left main, n (%) | 3 (1) | 2 (1) | 1 (1) | 0.48 |
| – LAD, n (%) | 179 (44) | 84 (45) | 95 (43) | 0.76 |
| – LCX, n (%) | 50 (12) | 20 (11) | 30 (14) | 0.34 |
| – RCA, n (%) | 170 (42) | 81 (43) | 89 (41) | 0.64 |
| Provenance | ||||
| – Walk-in to ER of PCI centre, n (%) | 72 (18) | 41 (22) | 31 (14) | 0.05 |
| – Transfer Riaz, n (%) | 56 (14) | 25 (13) | 31 (14) | 0.81 |
| – Transfer Tafers, n (%) | 40 (10) | 19 (10) | 21 (10) | 0.84 |
| – Transfer Payerne, n (%) | 56 (14) | 22 (12) | 34 (16) | 0.27 |
| – Transfer Meyriez, n (%) | 11 (3) | 3 (2) | 8 (4) | 0.20 |
| – Transfer Estavayer, n (%) | 2 (1) | 1 (1) | 1(1) | 0.90 |
| – Referral from GP, n (%) | 22 (5) | 7 (4) | 15 (7) | 0.16 |
| – EMS, n (%) | 120 (30) | 52 (28) | 68 (31) | 0.47 |
| – Other, n (%) | 9 (2) | 5 (3) | 4 (2) | 0.56 |
| – Unknown, n (%) | 16 (4) | 11 (6) | 5 (2) | 0.06 |
BMI = body mass index; CABG = coronary artery bypass graft; EMS = emergency medical services; ER = emergency room; GP = general practitioner; LAD = left anterior descending artery; LCX = left circumflex artery; MI = myocardial infarction; PCI = percutaneous coronary intervention
Treatment delays are outlined in supplementary table S1 in appendix 1 . Overall, the median FMC-R time was 94 minutes (IQR 71–120 minutes). The shortest FMC-R time was seen in patients presenting directly to the ER of the PCI centre (86 minutes [IQR 58–110 minutes]), whereas patients referred from their GP had the longest FMC-R interval (129 minutes [IQR 74–164 minutes]). Total ischaemic time was shortest in patients referred by emergency medical services (152 minutes [IQR 108–235 minutes]). Median total ischaemic time was significantly shorter in patients with a short compared to patients with a long FMC-R delay (148 minutes [IQR 110–220 minutes] vs 226 minutes [IQR 154–345 minutes], p <0.001).
There were no differences in peak CK or CK-MB levels between the groups (table S2). Median length of stay was 5 days (IQR 2–7), and similar between short and long FMC-R delays.
There were no differences in lesion or procedural characteristics between the two groups (table S3). Overall, 546 lesions were treated in 406 patients. Predilatation was performed in 438 cases (80%) (short vs long: n = 194 (79%) vs n = 244 (81%), p = 0.39). There were 404 (74%) complex lesions (short v. long: n = 185 (76%) vs n = 219 (73%), p = 0.51). Thrombus aspiration was performed in 210 (38%) lesions (short vs long: n = 103 (42%) vs n = 107 (36%), p = 0.13). Post-procedural TIMI 3 flow was present in 517 cases (94%) (short vs long: n = 234 (96%) and n = 283 (94%), p = 0.44).
Overall, binary logistic regression identified age as the only predictor of prolonged FMC-R delay (per additional year, odds ratio: 1.03, 95% confidence interval [CI]: 1.01 – 1.05, p = 0.001; table 2). table S4 shows the proportion of patients with short and long delays according to age category. Supplementary figure S1 depicts the distribution of age according to short or long treatment delays. Figure S2 shows the proportion of patients with long treatment delays for each age category.
Table 2 Predictors for first medical contact to revascularisation >90 minutes.
| Variable | Odds ratio (95% confidence interval) | p-value |
|---|---|---|
| Walk-in to ER of PCI centre | 0.61 (0.36–1.03) | 0.06 |
| Age (per additional year) | 1.03 (1.01–1.05) | 0.001 |
ER = emergency room; PCI = percutaneous coronary intervention
Clinical outcomes are provided in table 3. At 3 years, MACE rates were significantly higher in patients with “long’’ FMC-R intervals (24.6% vs 15.0%, hazard ratio [HR] 1.80, 95% CI 1.10–2.94; p = 0.02). This difference was driven by a higher rate of repeat revascularisation (14.2% vs 10.2%, HR 1.65, 95% CI 0.89–3.0; p = 0.11), and an increased incidence of cardiac death (7.8% vs 3.2%, HR 2.55, 95% CI 0.91–7.15; p = 0.08). Kaplan-Meier curves for the primary endpoint are presented in figure 2. One patient in the “short” group died 607 days after STEMI from sudden death at home, which was considered a cardiac death. One patient in the “long” group died suddenly 233 days after STEMI, which was also considered a cardiac death. No other ambiguous or otherwise unclassified deaths occurred.
Table 3 Primary clinical end point and overall mortality at 30 days, 1 year and 3 years according to treatment delay.
|
Total
(n = 406) |
Short
(n = 187) |
Long
(n = 219) |
HR (95% CI) | p-value | |
|---|---|---|---|---|---|
| 30-day MACE, n (%) | 23 (5.7) | 5 (2.7) | 18 (8.2) | 2.61 (0.91–7.49) | 0.07 |
| – Cardiac death, n (%) | 15 (3.7) | 4 (2.1) | 11 (5.0) | 2.41 (0.63–7.29) | 0.22 |
| – Nonfatal MI, n (%) | 1 (0.2) | 0 (0.0) | 1 (0.5) | – | – |
| – Repeat revascularisation, n (%) | 7 (1.7) | 1 (0.5) | 6 (2.7) | 4.79 (0.46–49.59) | 0.19 |
| 1-year MACE, n (%) | 55 (13.5) | 16 (8.5) | 39 (17.8) | 2.05 (1.11–3.80) | 0.02 |
| – Cardiac death, n (%) | 19 (4.7) | 4 (2.1) | 15 (6.9) | 2.64 (0.84–8.26) | 0.09 |
| – Nonfatal MI, n (%) | 3 (0.7) | 0 (0.0) | 3 (1.4) | – | – |
| – Repeat revascularisation, n (%) | 33 (8.1) | 12 (6.4) | 21 (9.6) | 1.76 (0.82–3.81) | 0.15 |
| 3-year MACE, n (%) | 82 (20.2) | 28 (15.0) | 54 (24.6) | 1.80 (1.10–2.94) | 0.02 |
| – Cardiac death, n (%) | 23 (5.7) | 6 (3.2) | 17 (7.8) | 2.55 (0.91–7.15) | 0.08 |
| – Nonfatal MI, n (%) | 9 (2.2) | 3 (1.6) | 6 (2.7) | 1.46 (0.31–6.86) | 0.64 |
| – Repeat revascularisation, n (%) | 50 (12.3) | 19 (10.2) | 31 (14.2) | 1.65 (0.89–3.04) | 0.11 |
| 30-day mortality n (%) | 12 (3.0) | 3 (1.6) | 9 (4.1) | 2.57 (0.69–9.51) | 0.15 |
| 1-year mortality, n (%) | 22 (5.4) | 4 (2.1) | 18 (8.2) | 3.9 (1.33–11.5) | 0.01 |
| 3-year mortality, n (%) | 39 (9.6) | 13 (7.0) | 26 (11.9) | 1.79 (0.92–3.48) | 0.08 |
CI = confidence interval; HR = hazard ratio; MACE = major adverse cardiac events; MI = myocardial infarction
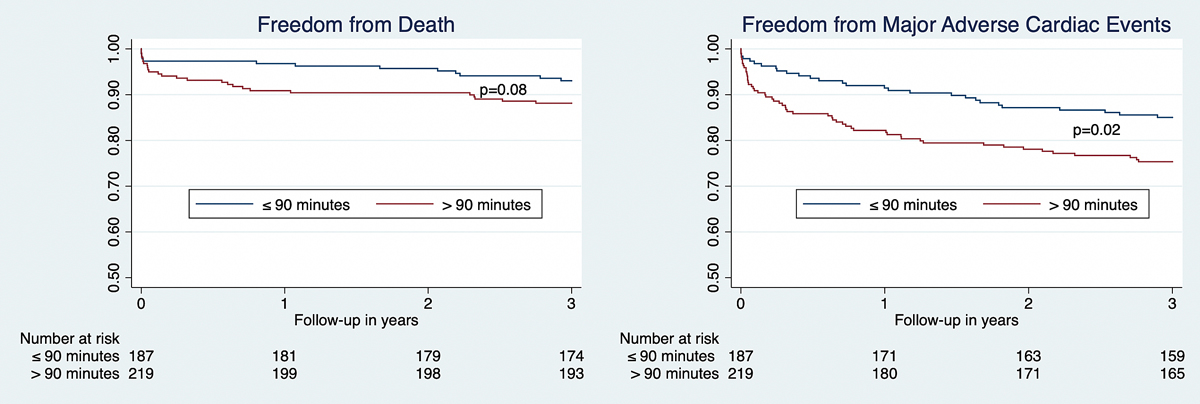
Figure 2 Kaplan-Meier curves for survival free from the occurrence of major adverse cardiac events and death.
Information on all-cause mortality is also provided in table 3. Mortality at 1 year was higher in the “long’’ than in the “short’’ group (8.2% vs 2.1%, HR 3.90, 95% CI 1.33–11.5; p = 0.01). However, at the 3-year follow-up, the difference in mortality was no longer statistically significant (11.9% vs 7.0%, HR 1.79, 95% CI 0.92–3.48, p = 0.08; fig. 2).
The main findings of the present study are [1]: age negatively impacts the delay between first medical contact and revascularisation in STEMI patients [2]; the system-dependent delay in our center complies with the new ESC quality target in 50% of patients [3]; patients revascularised within 90 minutes after first medical contact have lower MACE rates at 3 years.
We identified age as the only significant predictor for a treatment delay exceeding 90 minutes. Likewise, in a registry including 3832 patients, Ruiz et al. also identified age as an independent predictor for an FMC-R delay of >120 minutes [11]. This may be due to several factors. Firstly, atypical symptoms are more frequent with advancing age, thus rendering the diagnosis of STEMI more difficult [12]. Moreover, communication between the patient and the first medical responder may be impaired in the elderly. Secondly, comorbidities and frailty might prolong the time from diagnosis to treatment [13]. Lastly, in the very old, conservative treatment instead of primary PCI may be considered before activating established STEMI network pathways. Increased treatment delays for patient subsets presenting with atypical symptoms have been found previously. Roswell and colleagues found prolonged FMC-R delays in women and explained their finding by postulating atypical symptoms as the cause of this association [14–18]. In analysing 14,518 US patients with first medical contact at non-PCI-capable hospitals and requiring transfer for primary PCI, Dauerman et al. found a prolonged system-dependent delay in patient subsets with a propensity for atypical clinical presentation (women, elderly and diabetics). Interestingly, other potent predictors for short treatment delays in their analysis were white race and higher annual STEMI volume [19].
With an increasingly elderly population, more elderly patients are likely to be treated for STEMI, increasing the risk of misdiagnoses and adverse clinical outcomes. Future clinical research in this elderly population should not only concentrate on medical parameters such as risk factors, clinical and angiographic presentations, management and prognosis, but also, and most importantly, on ethical considerations, including patient autonomy and expectations.
Our analysis shows that the ESC-recommended system-dependent treatment delay of <90 minutes was achieved in approximately 50% of patients treated between 2008 and 2014. The maximum expected delay before choosing PCI over fibrinolysis (120 minutes) was achieved in 75% of patients. Many PCI centres, regional STEMI networks and national societies have reported their system-dependent treatment delay, showing large differences. In a cross-sectional, multicentre study including seven PCI-capable hospitals in the Netherlands, Tra and colleagues reported reaching the guideline-recommended target of <90 minutes in 78.7% of patients [20]. However, they defined the beginning of the system-dependent delay as the time of the first electrocardiogram and not the time of first medical contact, which likely explains their overall performance. Our results are in line with the treatment delays reported in GRACE and the HORIZONS-AMI trial, where reperfusion delays from first medical contact or from first hospital door threshold of <90 minutes were achieved in roughly 50% of patients [21, 22]. Short system-dependent delays have been recommended for a long time [23]. Interestingly, the 2012 ESC Guidelines recommendations of delays <90 and at most <120 minutes are derived from a post-hoc analysis of the DANAMI-2 trial and an analysis of the National Cardiovascular Data Registry in the US [24, 25]. While both studies suggested that shorter time delays were beneficial in terms of clinical outcomes, the question of whether or not the recommended delays were feasible was not addressed. The median system-dependent delay in DANAMI-2 was 127 minutes (IQR 98–157 minutes) for patients undergoing primary PCI. Nonetheless, achieving optimal treatment delays should be the ultimate objective of every STEMI network. Comparisons between countries, geographical regions, healthcare systems and cultures may be subject to biases. It is unclear whether there would be much room for improvement in extensive rural areas, remote from primary PCI-capable centres, in which access to primary healthcare is restricted. This may, in part, explain data from the United States, where only minimal improvements in treatment delays were observed from the late 1990s to the mid-2000s [26, 27]. Indeed, feasibility seems to be a key issue in this context. The overall treatment delay from symptom onset to reperfusion is dependent on a large number of variables. The patient-dependent component, governing the time from symptom onset to first medical contact, could possibly be modulated through public service announcements; these would have to be provided repeatedly. Geographic location, i.e., the distance to the nearest healthcare provider, seems to play an important role and is likely an unchangeable factor. The system-dependent component should be constantly analysed. Malfunctioning processes should be amended based on thorough analyses. Future research might focus on STEMI networks that perform well and on trying to understand whether the key reasons for a network’s success are transferrable to other systems with distinct socio-geographical attributes.
It is generally accepted that total ischaemic time and age are some of if not the most influential predictors for clinical outcome after STEMI. There is ample evidence of fewer mid- and long-term MACE in patients with shorter door-to-balloon or FMC-R times [24, 25]. In this analysis, we found significantly lower rates of MACE in patients with an FMC-R delay <90 minutes compared to patients with a delay exceeding 90 minutes. This difference was largely driven by lower rates of cardiac death occurring within the first year. At 3 years, the overall MACE rate was 20% and all-cause mortality was 9.6% for patients treated in the STEMI network of Fribourg.
Data on 3-year mortality after STEMI are limited. Hosseiny and colleagues recently reported an overall 3-year mortality rate of 11.6% in 1313 Australian STEMI patients [28].
All-cause mortality at 1 year has been reported at 11.4% in 2804 consecutive patients treated with primary PCI for STEMI in Denmark [4]. In contrast, 1-year mortality in our registry was 5.4%. This difference might be explained by the fact that patients in the Danish registry were included between 1998 and 2008, with inherent differences in the medical devices used (e.g., PCI with bare metal or first-generation drug-eluting stents). One-year all-cause mortality in the SCAAR study was reported at 9.4% between 2009 and 2010 [29]. In 2017, Garcia et al. reported a 2-year mortality of 8.5% in 1268 Catalan patients treated between 2002 and 2013 [30].
Our study has several limitations. The data collection from 2008 to 2010 was retrospective and may be subject to misclassification or information bias. Information on first medical contact was collected retrospectively and was missing in a minority of patients. Given our limited sample size, the statistical power for identifying predictors for a long FMC-R delay was likely low.
The external validity and general transferability of our results are limited, as geographical, political and social factors are intertwined, and the results likely reflect the care provided in a small, high-income country with universal access to health care.
Increased age prolongs the delay to revascularisation after first medical contact in patients with STEMI. Patients with treatment delays of <90 minutes have significantly lower MACE rates at 3 years.
Table S1: Provenance and delay.
Table S2: Peak CK and length of stay.
Table S3: Lesion and procedural characteristics.
Table S4: FMC-R delay according to age category.
Figure S1: Distribution of age according to short or long treatment delays.
Figure S2: Proportion of patients with long treatment delays for each age category.
The appendix is available as a separate file at https://smw.ch/article/doi/smw.2020.20368.
This trial was an investigator-initiated study supported by an unrestricted grant from the Fonds Scientifique Cardiovasculaire (Fribourg, Switzerland). The funding sources had no role in the design of the study, data collection, data monitoring, data analysis, data interpretation, or writing of the report.
The authors declare no conflict of interest.
1 Puymirat E , Simon T , Steg PG , Schiele F , Guéret P , Blanchard D , et al.; USIK USIC 2000 Investigators; FAST MI Investigators. Association of changes in clinical characteristics and management with improvement in survival among patients with ST-elevation myocardial infarction. JAMA. 2012;308(10):998–1006. doi:.https://doi.org/10.1001/2012.jama.11348
2 Townsend N , Wilson L , Bhatnagar P , Wickramasinghe K , Rayner M , Nichols M . Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J. 2016;37(42):3232–45. doi:.https://doi.org/10.1093/eurheartj/ehw334
3 Quinn T , Johnsen S , Gale CP , Snooks H , McLean S , Woollard M , et al.; Myocardial Ischaemia National Audit Project (MINAP) Steering Group. Effects of prehospital 12-lead ECG on processes of care and mortality in acute coronary syndrome: a linked cohort study from the Myocardial Ischaemia National Audit Project. Heart. 2014;100(12):944–50. doi:.https://doi.org/10.1136/heartjnl-2013-304599
4 Pedersen F , Butrymovich V , Kelbæk H , Wachtell K , Helqvist S , Kastrup J , et al. Short- and long-term cause of death in patients treated with primary PCI for STEMI. J Am Coll Cardiol. 2014;64(20):2101–8. doi:.https://doi.org/10.1016/j.jacc.2014.08.037
5 McManus DD , Gore J , Yarzebski J , Spencer F , Lessard D , Goldberg RJ . Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;124(1):40–7. doi:.https://doi.org/10.1016/j.amjmed.2010.07.023
6 Canto JG , Rogers WJ , Goldberg RJ , Peterson ED , Wenger NK , Vaccarino V , et al.; NRMI Investigators. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA. 2012;307(8):813–22. doi:.https://doi.org/10.1001/jama.2012.199
7 Ibanez B , James S , Agewall S , Antunes MJ , Bucciarelli-Ducci C , Bueno H , et al.; ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77. doi:.https://doi.org/10.1093/eurheartj/ehx393
8 Wallentin L , Becker RC , Budaj A , Cannon CP , Emanuelsson H , Held C , et al.; PLATO Investigators. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045–57. doi:.https://doi.org/10.1056/NEJMoa0904327
9 Wiviott SD , Braunwald E , McCabe CH , Montalescot G , Ruzyllo W , Gottlieb S , et al.; TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357(20):2001–15. doi:.https://doi.org/10.1056/NEJMoa0706482
10 Van de Werf F , Bax J , Betriu A , Blomstrom-Lundqvist C , Crea F , Falk V , et al.; ESC Committee for Practice Guidelines (CPG). Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008;29(23):2909–45. doi:.https://doi.org/10.1093/eurheartj/ehn416
11 Carol Ruiz A , Masip Utset J , Ariza Solé A ; researchers of the Codi Infart registry of Catalonia. Predictors of Late Reperfusion in STEMI Patients Undergoing Primary Angioplasty. Impact of the Place of First Medical Contact. Rev Esp Cardiol (Engl Ed). 2017;70(3):162–9. doi:.https://doi.org/10.1016/j.rec.2016.11.030
12 Gregoratos G . Clinical manifestations of acute myocardial infarction in older patients. Am J Geriatr Cardiol. 2001;10(6):345–7. doi:.https://doi.org/10.1111/j.1076-7460.2001.00641.x
13 Mehta RH , Rathore SS , Radford MJ , Wang Y , Wang Y , Krumholz HM . Acute myocardial infarction in the elderly: differences by age. J Am Coll Cardiol. 2001;38(3):736–41. doi:.https://doi.org/10.1016/S0735-1097(01)01432-2
14 Bangalore S , Fonarow GC , Peterson ED , Hellkamp AS , Hernandez AF , Laskey W , et al.; Get with the Guidelines Steering Committee and Investigators. Age and gender differences in quality of care and outcomes for patients with ST-segment elevation myocardial infarction. Am J Med. 2012;125(10):1000–9. doi:.https://doi.org/10.1016/j.amjmed.2011.11.016
15 Collins SD , Ahmad S , Waksman R . Percutaneous revascularization in women with coronary artery disease: we’ve come so far, yet have so far to go. Nutr Metab Cardiovasc Dis. 2010;20(6):436–44. doi:.https://doi.org/10.1016/j.numecd.2010.02.014
16 Jneid H , Fonarow GC , Cannon CP , Hernandez AF , Palacios IF , Maree AO , et al.; Get With the Guidelines Steering Committee and Investigators. Sex differences in medical care and early death after acute myocardial infarction. Circulation. 2008;118(25):2803–10. doi:.https://doi.org/10.1161/CIRCULATIONAHA.108.789800
17 Pagley PR , Yarzebski J , Goldberg R , Chen Z , Chiriboga D , Dalen P , et al. Gender differences in the treatment of patients with acute myocardial infarction. A multihospital, community-based perspective. Arch Intern Med. 1993;153(5):625–9. doi:.https://doi.org/10.1001/archinte.1993.00410050061008
18 Rezaee ME , Brown JR , Conley SM , Anderson TA , Caron RM , Niles NW . Sex disparities in pre-hospital and hospital treatment of ST-segment elevation myocardial infarction. Hosp Pract (1995). 2013;41(2):25–33. doi:.https://doi.org/10.3810/hp.2013.04.1023
19 Dauerman HL , Bates ER , Kontos MC , Li S , Garvey JL , Henry TD , et al. Nationwide Analysis of Patients With ST-Segment-Elevation Myocardial Infarction Transferred for Primary Percutaneous Intervention: Findings From the American Heart Association Mission: Lifeline Program. Circ Cardiovasc Interv. 2015;8(5):e002450. doi:.https://doi.org/10.1161/CIRCINTERVENTIONS.114.002450
20 Tra J , van der Wulp I , de Bruijne MC , Wagner C . Exploring the treatment delay in the care of patients with ST-elevation myocardial infarction undergoing acute percutaneous coronary intervention: a cross-sectional study. BMC Health Serv Res. 2015;15(1):340. doi:.https://doi.org/10.1186/s12913-015-0993-y
21 Blankenship JC , Skelding KA , Scott TD , Berger PB , Parise H , Brodie BR , et al. Predictors of reperfusion delay in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention from the HORIZONS-AMI trial. Am J Cardiol. 2010;106(11):1527–33. doi:.https://doi.org/10.1016/j.amjcard.2010.07.033
22 Spencer FA , Montalescot G , Fox KA , Goodman SG , Granger CB , Goldberg RJ , et al.; Global Registry of Acute Coronary Events (GRACE) Investigators. Delay to reperfusion in patients with acute myocardial infarction presenting to acute care hospitals: an international perspective. Eur Heart J. 2010;31(11):1328–36. doi:.https://doi.org/10.1093/eurheartj/ehq057
23 Hasdai D , Behar S , Wallentin L , Danchin N , Gitt AK , Boersma E , et al.; The Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS). A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin; the Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS). Eur Heart J. 2002;23(15):1190–201. doi:.https://doi.org/10.1053/euhj.2002.3193
24 Nielsen PH , Terkelsen CJ , Nielsen TT , Thuesen L , Krusell LR , Thayssen P , et al.; Danami-2 Investigators. System delay and timing of intervention in acute myocardial infarction (from the Danish Acute Myocardial Infarction-2 [DANAMI-2] trial). Am J Cardiol. 2011;108(6):776–81. doi:.https://doi.org/10.1016/j.amjcard.2011.05.007
25 Rathore SS , Curtis JP , Chen J , Wang Y , Nallamothu BK , Epstein AJ , et al.; National Cardiovascular Data Registry. Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ. 2009;338(may19 1):b1807. doi:.https://doi.org/10.1136/bmj.b1807
26 Chakrabarti A , Krumholz HM , Wang Y , Rumsfeld JS , Nallamothu BK ; National Cardiovascular Data Registry. Time-to-reperfusion in patients undergoing interhospital transfer for primary percutaneous coronary intervention in the U.S: an analysis of 2005 and 2006 data from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2008;51(25):2442–3. doi:.https://doi.org/10.1016/j.jacc.2008.02.071
27 Nallamothu BK , Bates ER , Herrin J , Wang Y , Bradley EH , Krumholz HM ; NRMI Investigators. Times to treatment in transfer patients undergoing primary percutaneous coronary intervention in the United States: National Registry of Myocardial Infarction (NRMI)-3/4 analysis. Circulation. 2005;111(6):761–7. doi:.https://doi.org/10.1161/01.CIR.0000155258.44268.F8
28 Doost Hosseiny A , Moloi S , Chandrasekhar J , Farshid A . Mortality pattern and cause of death in a long-term follow-up of patients with STEMI treated with primary PCI. Open Heart. 2016;3(1):e000405. doi:.https://doi.org/10.1136/openhrt-2016-000405
29 Fokkema ML , James SK , Albertsson P , Akerblom A , Calais F , Eriksson P , et al. Population trends in percutaneous coronary intervention: 20-year results from the SCAAR (Swedish Coronary Angiography and Angioplasty Registry). J Am Coll Cardiol. 2013;61(12):1222–30. doi:.https://doi.org/10.1016/j.jacc.2013.01.007
30 García-García C , Ribas N , Recasens LL , Meroño O , Subirana I , Fernández A , et al. In-hospital prognosis and long-term mortality of STEMI in a reperfusion network. “Head to head” analisys: invasive reperfusion vs optimal medical therapy. BMC Cardiovasc Disord. 2017;17(1):139. doi:.https://doi.org/10.1186/s12872-017-0574-6
Shared first authors
OR and AS take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
This trial was an investigator-initiated study supported by an unrestricted grant from the Fonds Scientifique Cardiovasculaire (Fribourg, Switzerland). The funding sources had no role in the design of the study, data collection, data monitoring, data analysis, data interpretation, or writing of the report.
The authors declare no conflict of interest.