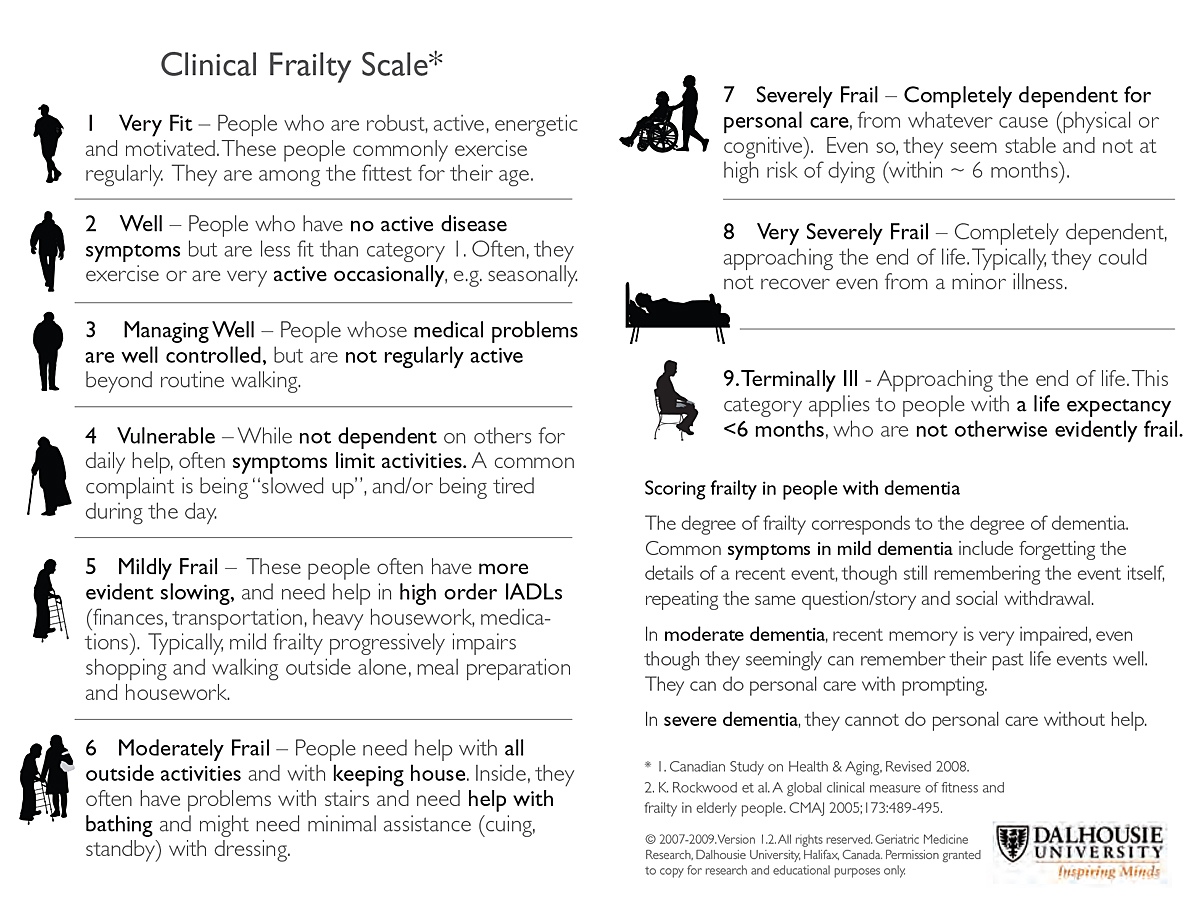
Figure 1 Clinical Frailty Scale.
DOI: https://doi.org/10.4414/smw.2020.20401
Guidance on the application of Section 9.3 of the SAMS Guidelines “ Intensive-care interventions ” (2013)
This document is available in English, French, German and Italian, cf. sams.ch/en/coronavirus . The German text is the authentic version.
3rd, updated version of 4 November 2020. The 2nd version was published in the Swiss Medical Weekly in March 2020 (Swiss Med Wkly. 2020;150:w20229, DOI: https://doi.org/10.4414/smw.2020.20229 )
In March 2020, owing to the rapid spread of the coronavirus (SARS-CoV-2), an extraordinary situation was declared,1 and for several weeks acute hospitals experienced a massive influx of patients. In view of this situation, the Swiss Academy of Medical Sciences (SAMS) and the Swiss Society of Intensive Care Medicine (SSICM) issued guidelines on triage for intensive-care treatment under resource scarcity. In this first wave of COVID-19, the restriction of elective procedures2 and an increase in ICU (particularly ventilator-equipped) beds, together with public health (behavioural) measures ordered by the federal government, were enough to prevent a situation of resource scarcity from arising at the national level. It was therefore not necessary for the SAMS guidelines to be applied. Given the development of the pandemic in October, the guidelines now need to be revised and updated in the light of the experience accumulated since March. There has been no change in the guiding principle that uniform criteria for intensive-care unit (ICU) admission and continued occupancy should be applied throughout Switzerland. The present guidelines provide the necessary basis.
In collaboration with health system stakeholders, the Coordinated Medical Services of the Swiss Armed Forces has established a system for national coordination of ICUs. A central coordination body is to ensure that optimum use is made of all ICU treatment capacity available across Switzerland.3
As specified in the document «National coordination in the event of a massive influx of patients to ICUs during the COVID-19 pandemic»4, responsibility for patient triage lies with the individual hospital/ICU. The SAMS and the SSICM hereby propose that the national coordination body should be responsible for determining at what point the situation in Switzerland is such that triage decisions – in accordance with the criteria set out here – are unavoidable. This would ensure that the best possible use is made of resources across Switzerland before triage decisions are required at individual hospitals. The coordination body should also be responsible for deciding on the threshold at which the application of these guidelines is to be triggered at the national level.
The guidelines will be adapted by the issuing authority if experience in practice and new scientific findings so require. The latest version is available at: sams.ch/en/coronavirus
The following guidelines concerning the criteria for ICU triage are applicable for the point in time at which resource scarcity arises and rationing decisions have to be made. They are applicable to all patient categories. Patients with COVID-19 and other patients requiring intensive care are treated according to the same criteria.
The guidelines supplement the SAMS Guidelines «Intensive-care interventions» and thus concern only a small proportion of patients infected with the coronavirus, namely the group of severely ill patients requiring intensive care.
The four widely recognised principles of medical ethics (beneficence, non-maleficence, respect for autonomy and equity) are also crucial under conditions of resource scarcity. It is important that the patient’s wishes with regard to emergency treatment and intensive care are ascertained at an early stage, especially for individuals belonging to a risk group. Scarce resources must never be employed for treatments which a patient does not wish to receive.
If the resources available are insufficient to enable all patients to receive the ideally required treatment, then these fundamental principles are to be applied in accordance with the following rules of precedence:6
Equity: Available resources are to be allocated without discrimination – i.e. without unjustified unequal treatment on grounds of age, sex, residence7, nationality, religious affiliation, social or insurance status, or chronic disability. The allocation procedure must be fair, objectively justified and transparent. With a fair allocation procedure, arbitrary decisions, in particular, can be avoided.
Preserving as many lives as possible: Under conditions of acute scarcity, all measures are guided by the aim of minimising the number of deaths. Decisions should be made in such a way as to ensure that as few people as possible become severely ill or die.
Protection of the professionals involved: These individuals8 are at particular risk of infection with the coronavirus. If they are unable to work owing to infection, more deaths will occur under conditions of acute scarcity. They are therefore to be protected as far as possible against infection, but also against excessive physical and psychological stress. Professionals whose health is at greater risk in the event of infection with the coronavirus are to be especially protected and should not be deployed in the care of patients with COVID-19.
As long as sufficient resources are available, patients requiring intensive care are to be admitted and treated in accordance with established criteria. Particularly resource-intensive interventions should only be undertaken in cases in which the benefits thereof have been unequivocally demonstrated. For patients with COVID-19, ECMO9 should only be used in particular situations, as specified in the SSICM guidelines, after careful assessment of the personnel resources required.10
It is important to discuss in advance – with all patients capable of doing so – the patients’ wishes in the event of possible complications (resuscitation status and extent of intensive care). If intensive-care interventions are withheld, comprehensive palliative care must be provided.11
If ICU capacity is exhausted and not all patients who require intensive care can be admitted, the short-term prognosis is decisive for purposes of triage. For ICU admission, highest priority is to be accorded to those patients whose prognosis12 with regard to hospital discharge is good with intensive care, but poor without it – i.e. the patients who will benefit most from intensive care.
Age, disability or dementia in themselves are not to be applied as criteria, as this would be to accord less value to older or disabled people, thus infringing the constitutional prohibition on discrimination. These factors are, however, indirectly taken into account under the main criterion «short-term prognosis», since older people more frequently suffer from comorbidity, and the short-term prognosis may also be adversely affected by dementia and certain disabilities. In connection with COVID-19, age, disability and dementia are risk factors for mortality and must be taken into account like all the other independent risk factors identified since March 2020.
Frailty is an important criterion to consider in a situation of resource scarcity. Of the various tools proposed for the evaluation of frailty, the best validated is the Clinical Frailty Scale (CFS, figure 1).13
Consideration of additional criteria. In the literature,14 additional criteria are discussed, such as lotteries, «first come, first served» and prioritisation according to social usefulness. These criteria are not to be applied.
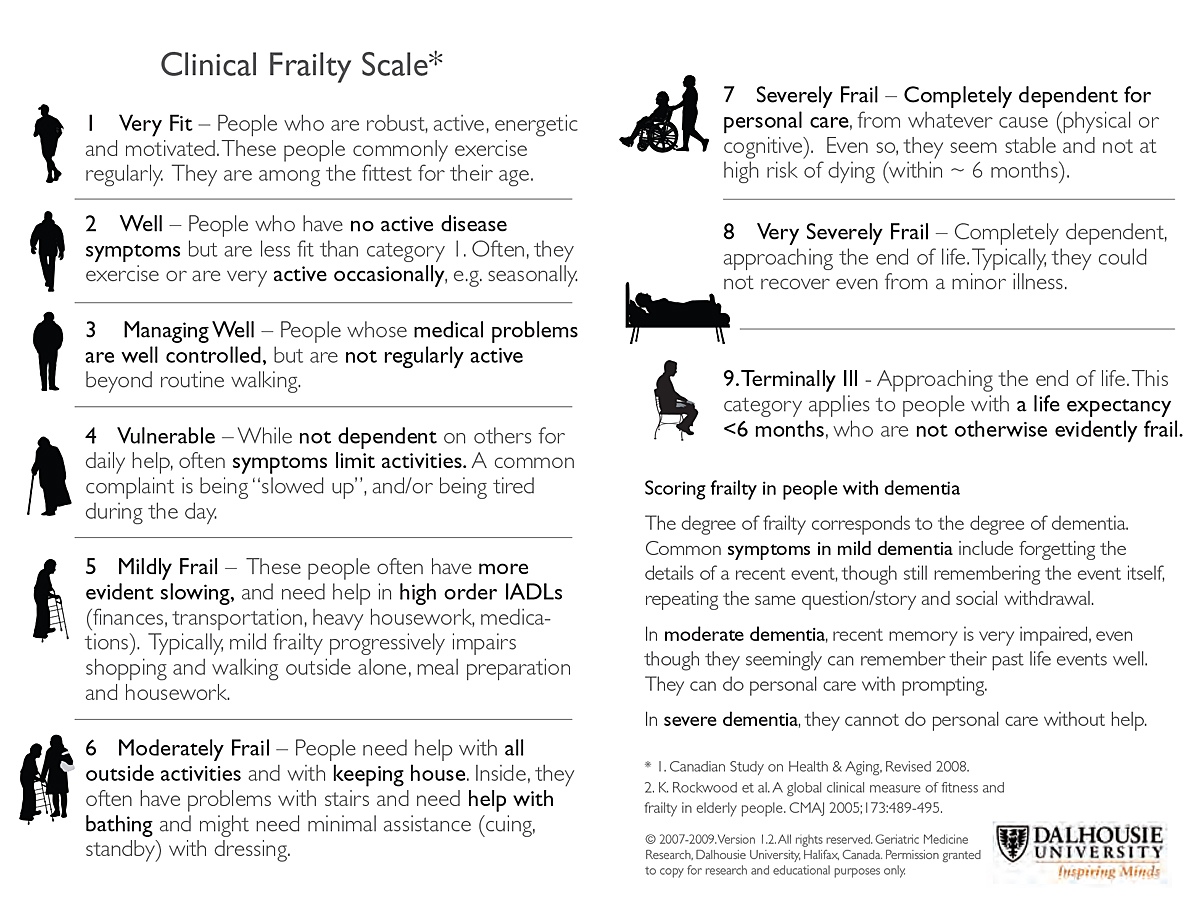
Figure 1 Clinical Frailty Scale.
If, in spite of additional external beds, ICU capacity is no longer sufficient to allow all patients requiring intensive care to be treated, the first measure is to make the short-term prognosis criterion more stringent. The aim is to maximise benefits for the individual patient and for patients collectively – i.e. to make decisions in such a way as to save the largest possible number of lives. The good short‑term prognosis criterion thus becomes (even) more central.
In a persistent mass influx situation, only patients who require mechanical ventilation (or another specific intensive-care intervention, such as hemodynamic support with vasoactive agents or continuous renal replacement therapy) are to be admitted to the ICU, in accordance with the criteria defined below. In this situation, resuscitation following cardiac arrest is not recommended.15 All less intensive treatments should be carried out in intermediate (IMCUs) or standard care units.
Depending on the development of pressure on care facility capacity and the intensity of the patient influx, a decision may be required on the two stages A and B in relation to the triage decision criteria. The SAMS and the SSICM suggest that the national coordination body should be responsible for making such a decision (cf. section “Background”).
Stage A: ICU beds available, but national capacity limited, with a risk of ICU beds becoming unavailable in the next few days
→ Admission triage / Resource management through decisions on discontinuation of treatment
Stage B: No ICU beds available
→ Admission triage / Resource management through decisions on discontinuation of treatment
Step 1:
Does the patient have any of the following inclusion criteria?
If one of these inclusion criteria is fulfilled → Step 2
Step 2:
Does the patient have any of the following exclusion criteria?
Stage A (cf. 4.2.)
In the event of uncertainty, the 4C Mortality Score may additionally be employed.19 It must not, however, be used as the sole decision-making criterion. A score of >15 indicates high mortality.
Stage B (cf. 4.2.)
Here, the following additional criteria are applied:
If one of the exclusion criteria is fulfilled, the patient is not to be admitted to the ICU. In the event of uncertainty, the 4C Mortality Score may additionally be employed. It must not, however, be used as the sole decision-making criterion. A score of >15 indicates high mortality.
The following criteria are relevant for the continuation of ICU treatment:
Patients in the ICU are to be assessed daily and interprofessionally. Here, the utility of intensive care is be evaluated on the basis of the clinical course, so that a decision can be taken with regard to possible discontinuation of treatment and a transition to palliative care. This applies to all (i.e. both COVID-19 and non-COVID-19) patients receiving ICU treatment when resources are exhausted. The more acute resource scarcity becomes, the more stringently the following criteria are to be applied.
Step 1:
Presence of a criterion for ICU discharge:
Step 2:
Following a period of stabilisation in accordance with the particular condition:
Presence of the following three criteria:
All three criteria must be met for ICU treatment to be continued.
Step 3:
Irrespective of the three criteria specified in Step 2, the presence of one of the following criteria should lead to the discontinuation of intensive care:
Stage A (cf. 4.2.)
Stage B (cf. 4.2.)
If one of these criteria is present, ICU treatment should be discontinued and the patient should receive palliative care.
In triage decisions, confidence must be maintained under the most difficult conditions. For this reason, fair rationing criteria and fair processes must be transparently applied at all times. Clear reasons for according (or failing to accord) priority must be documented and updated as the situation develops. The same applies to the processes whereby such decisions are made. Individual decisions must be amenable to examination: they must be documented in writing and include a statement of reasons and the name of the person responsible. Any deviation from the specified criteria must be similarly documented. In addition, mechanisms should be in place for subsequent review of conflicts.
The decision-making process must be managed by experienced professionals. Whenever possible, decisions must be made within an interprofessional team. Ultimately, however, responsibility is borne by the most senior intensive care specialist present. Bodies providing support for treatment teams (e.g. ethics support, multiprofessional team) may be helpful. However, the ICU must be able to make rapid, independent decisions at any time on patient admissions and transfers. The legal requirements21 concerning the duty to provide regular reports on the total number and occupancy of ICU beds are to be complied with.
If, owing to a triage situation, intensive care is not offered or is discontinued, this must be communicated in a transparent manner. It is not permissible to justify the treatment decision to the patient on the grounds that such treatment is not indicated, if a different decision would have been taken had sufficient resources been available. The patient with capacity, or the relatives authorised to represent a patient lacking capacity (Art. 378 Swiss Civil Code), are to be openly informed about the decision-making process, and if possible further support (e.g. hospital pastoral care) should be offered.
1 The Ordinance 2 of 13 March 2020 on Measures to Combat the Coronavirus (COVID-19) (COVID-19 Ordinance 2) (status as of 17 March 2020; since revoked) was based on Article 7 of the Epidemics Act (SR 818.101), which regulates the «extraordinary situation».
2 «Healthcare facilities such as hospitals and clinics, medical practices and dental practices must discontinue all non-urgent medical procedures and therapies» (Art. 10a para. 2 of the Ordinance cited in Footnote 1).
3 Further information and contact details can be found at: www.vtg.admin.ch/de/organisation/astab/san/ksd/nki.html (accessed on 3 November 2020).
4 Only available in German; accessed on 2 November 2020.
5 For a more detailed discussion of the ethical principles, see Section 2 of the SAMS Guidelines «Intensive‑care interventions».
6 Cf. also Swiss Influenza Pandemic Plan, Strategies and measures to prepare for an influenza pandemic, 5th edition 2018, Part II, Section 6.1, and especially Part III, Section 6 «Ethical issues».
7 Available ICU beds must be reported; cf. Art. 12 of the Ordinance of 19 June 2020 on Measures during the Special Situation to Combat the COVID-19 Epidemic (status as of 2 November 2020).
8 Naturally, the same applies for all persons exposed to a higher risk of infection as a result of their work (e.g. retail and pharmacy staff, as well as relatives caring for patients).
9 Extracorporeal membrane oxygenation.
10 Cf. Bartlett RH, Ogino MT, Brodie D, McMullan DM, Lorusso R, et al. Initial ELSO Guidance Document: ECMO for COVID-19 Patients with Severe Cardiopulmonary Failure. ASAIO J. 2020;66:472–4.
11 Cf. the palliative.ch guidelines: Therapeutische Massnahmen bei Patienten mit Covid-19 mit zu erwartender ungünstiger Prognose ( www.palliative.ch ).
12 For a more detailed discussion of prognosis, see Section 5.1 of the SAMS Guidelines «Intensive-care interventions» (2013).
13 Cf. Hewitt J, Carter B, Vilches-Moraga A, Quinn TJ, Braude P, et al. (COPE Study Collaborators). The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health. 2020 Aug;5(8):e444–51.
14 Cf., for example, Persad G, Wertheimer A, Emanuel E J. Principles for allocation of scarce medical interventions. Lancet. 2009;373:423–31.
15 See also the recommendations of the Swiss Society of Emergency and Rescue Medicine (SSERM) on pre‑hospital triage and care under conditions of resource scarcity in the hospital setting (specifically intensive care) during the COVID-19 pandemic. Cf. www.sgnor.ch/home/covid-19
16 Cf. Christian MD, Hawryluck L, Wax RS, et al. Development of a triage protocol for critical care during an influenza pandemic. CMAJ. 2006;175:1377–81.
17 Congenital and post-traumatic disabilities are excluded.
18 With regard to «age» and «CFS score» (dementia and disability) in Stages A and B, cf. the discussion of age, disability and dementia in Section 3.
19 Knight SR, Ho A, Pius R, Buchan I, Carson G, et al. on behalf of the ISARIC4C investigators. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ. Published online 9 September, 2020.
20 This is to be determined by the national coordination body in accordance with capacity at the two Burn Units (USZ and CHUV).
21 Cf. the Ordinance of 19 June 2020 on Measures during the Special Situation to Combat the COVID-19 Epidemic (status as of 2 November 2020).
Professor Daniel Scheidegger, SAMS Vice President, Arlesheim (lead)
Professor Thierry Fumeaux, SSICM Past President, Nyon
Bianca Schaffert, MSN, SAMS Central Ethics Committee Vice President, Schlieren
Professor Samia Hurst, University of Geneva
Professor Arnaud Perrier, HUG Chief Medical Officer, Geneva
lic. iur. Michelle Salathé, SAMS, Bern (until September 2020)
Dr Thomas Gruberski, SAMS, Bern
The SAMS and the SSICM thank the numerous experts who commented on these guidelines and provided valuable input.
The guidelines have been approved by the Central Ethics Committee (CEC), the Executive Board of the SAMS and the Board of the Swiss Intensive Care Medicine Society (SSICM); they are effective from 20 March 2020. The revised Version 3 was approved by the CEC and the Executive Board of the SAMS on 2 November 2020, and by the Board of the SSICM on 3 November 2020.
-Please note: The latest literature on SARS-CoV-2 is made available on the website of the Swiss Society of Intensive Care Medicine (SSICM) at www.sgi-ssmi.ch
- Bouadma L , Lescure FX , Lucet JC , Yazdanpanah Y , Timsit JF . Severe SARS-CoV-2 infections: practical considerations and management strategy for intensivists. Intensive Care Med. 2020;46(4):579–82; Epub ahead of print. doi:.https://doi.org/10.1007/s00134-020-05967-x
-Bundesamt für Gesundheit (BAG). Influenza-Pandemieplan Schweiz. Strategien und Massnahmen zur Vorbereitung auf eine Influenza-Pandemie, 5. Auflage 2018, Kap. 6.1. sowie insb. Teil II.I «Ethische Fragen des Influenza-Pandemieplan Schweiz 2006», Stellungnahme der Nationalen Ethikkommission NEK-CNE Nr. 12/2006. www.bag.admin.ch/dam/bag/de/dokumente/mt/k-und-i/hygiene-pandemiefall/influenza-pandemieplan-ch.pdf.download.pdf/bag-pandemieplan-influenza-ch.pdf
- Cheung WK , Myburgh J , Seppelt IM , Parr MJ , Blackwell N , Demonte S , et al.; Influenza Pandemic ICU Triage Study Investigators. A multicentre evaluation of two intensive care unit triage protocols for use in an influenza pandemic. Med J Aust. 2012;197(3):178–81. doi:.https://doi.org/10.5694/mja11.10926
- Christian MD , Hawryluck L , Wax RS , Cook T , Lazar NM , Herridge MS , et al. Development of a triage protocol for critical care during an influenza pandemic. CMAJ. 2006;175(11):1377–81. doi:.https://doi.org/10.1503/cmaj.060911
-The Hastings Center. Ethical Framework for Health Care Institutions Responding to Novel Coronavirus SARS-CoV-2 (COVID-19). Guidelines for Institutional Ethics Services Responding to COVID-19. Managing Uncertainty, Safeguarding Communities, Guiding Practice. March 16, 2020. www.thehastingscenter.org/wp-content/uploads/HastingsCenterCovidFramework2020.pdf
- Hewitt J , Carter B , Vilches-Moraga A , Quinn TJ , Braude P , Verduri A , et al.; COPE Study Collaborators. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health. 2020;5(8):e444–51. doi:.https://doi.org/10.1016/S2468-2667(20)30146-8
- Jöbges S , Vinay R , Luyckx VA , Biller-Andorno N . Recommendations on COVID-19 triage: international comparison and ethical analysis. Bioethics. Published online September 25, 2020. doi:.https://doi.org/10.1111/bioe.12805
- Knight SR , Ho A , Pius R , Buchan I , Carson G , et al. ISARIC4C investigators. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ. Published online September 9, 2020. doi:.https://doi.org/10.1136/bmj.m3339
- Liao X , Wang B , Kang Y . Novel coronavirus infection during the 2019-2020 epidemic: preparing intensive care units-the experience in Sichuan Province, China. Intensive Care Med. 2020;46(2):357–60. doi:.https://doi.org/10.1007/s00134-020-05954-2
- MacLaren G , Fisher D , Brodie D . Preparing for the Most Critically Ill Patients With COVID-19: The Potential Role of Extracorporeal Membrane Oxygenation. JAMA. 2020;323(13):1245–6. doi:.https://doi.org/10.1001/jama.2020.2342
-Murthy S, Gomersall CD, Fowler RA. Care for Critically Ill Patients With COVID-19. JAMA. 2020; .
- Ñamendys-Silva SA . Respiratory support for patients with COVID-19 infection. Lancet Respir Med. 2020;8(4):e18. doi:.https://doi.org/10.1016/S2213-2600(20)30110-7
-Österreichische Gesellschaft für Anaesthesiologie. Reanimation und Intensivmedizin (ÖGARI). Allokation intensivmedizinischer Ressourcen aus Anlass der Covid-19-Pandemie. Klinisch-ethische Empfehlungen für Beginn, Durchführung und Beendigung von Intensivtherapie bei Covid-19-PatientInnen. Statement der Arbeitsgruppe Ethik der ÖGARI vom 17.03.2020. www.oegari.at/web_files/cms_daten/covid-19_ressourcenallokation_gari-statement_v1.7_final_2020-03-17.pdf
- Persad G , Wertheimer A , Emanuel EJ . Principles for allocation of scarce medical interventions. Lancet. 2009;373(9661):423–31. doi:.https://doi.org/10.1016/S0140-6736(09)60137-9
- Swiss Academy Of Medical Sciences. COVID-19 pandemic: triage for intensive-care treatment under resource scarcity. Swiss Med Wkly. 2020;150:w20229.doi:https://doi.org/10.4414/smw.2020.20229
-Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;S2213-2600(20)30079-5 .
- Wu C , Chen X , Cai Y , Xia J , Zhou X , Xu S , et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):934–43; Epub ahead of print. doi:.https://doi.org/10.1001/jamainternmed.2020.0994
- Zhou F , Yu T , Du R , Fan G , Liu Y , Liu Z , et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62. doi:.https://doi.org/10.1016/S0140-6736(20)30566-3