
Figure 1 Marginal probability of overall IAE occurrence in ambulatory anaesthesia between 2000 and 2016.
Notice that the origin of the y-axis does not start at 0.
DOI: https://doi.org/10.4414/smw.2020.20365
Over the last three decades, the popularity of outpatient surgery (same-day, day-case) has been steadily increasing [1–3]. In the USA, the number of procedures being performed in ambulatory surgical centres increased from 380,000 in 1983 to 31.5 million in 1996 [4], and in Switzerland, the proportion of outpatient procedures increased by 13.4% between 2006 and 2010 [5–7].
There are several reasons for this transition from inpatient to outpatient. First, the development of novel anaesthetic agents that enable patients to regain consciousness more quickly and with fewer side effects has reduced the time frame of anaesthesia and post-anaesthetic monitoring [2]. Second, the emergence of new minimally invasive surgical procedures has reduced the duration of surgical procedures [8]. These two technical factors have made it possible to carry out more and more ambulatory procedures. Third, the savings achieved by reducing the length of stay in the hospital has been an important catalyst [6]. Previous research shows that outpatient interventions are often cheaper than hospitalisation to perform the same surgical procedures [6].
Simultaneously, there has been an inciting movement to assess and improve the quality and safety of healthcare [9–11]. Anaesthesiologists have been leaders in improving patient safety [8]. Indeed, anaesthesia-related mortality has outstandingly decreased over the last 50 years [5]. At the end of the 20th century, 1/900 patients died because of anaesthesia [9]. In the late 1950s, anaesthesia-related mortality was much lower and ranged from 3.1/10,000 to 6.4/10,000 [10, 11]. During the last three decades, mortality figures associated with anaesthesia have dropped to 0.04–0.07/10,000 anesthetised patients [12, 13].
Nevertheless, although anaesthesia can claim successes in mortality reduction, anaesthesia-related morbidity remains significant [13]. For example, in a number of specific techniques such as airway control, hoarseness of voice following tracheal intubation has been reported in 14–50% of patients [14], or in epidural anaesthesia, accidental dural perforations occurred in 0.5–0.6% of interventions [15–17]. Arrhythmia due to insufficient analgesia is the most common event in regional anaesthesia [18]. The overall incidence of minor anaesthesia-related perioperative incidents, such as hypotension or arrhythmia, was found to be between 18% and 22% [18, 19]. Therefore, it is fundamental to strive to continuously improve the practice of anaesthesia. For this purpose, the Anaesthesia Databank Switzerland (ADS), a voluntary data registry, was set up in 1996 in Switzerland [5]. Between 1996 and 2016, the ADS provided internal and external benchmark comparisons to the (up to 40) departments who participated.
We used ADS data to assess the overall incidence and time trend of intraoperative adverse events (IAEs) in ambulatory surgical interventions carried out between 2000 and 2016 in Switzerland. The secondary goal was to investigate the specific incidence and evolution of technical, cardiovascular, organisational, respiratory, and general sub-categories of IAE.
The ADS registry aims at improving the quality and safety of anaesthetic procedures through regular activity reporting of participating anaesthesia services. Participation was open to any public and private hospitals of various sizes and types in Switzerland [5]. In this study, we considered only hospitals providing information on IAEs [5]. Our inclusion criteria were all anaesthetic procedures performed for surgical intervention on outpatients aged ≥18 years. We included all procedures performed between 1 January 2000 and 31 December 2016.
We excluded procedures with missing values in the variables: age, gender, American Society of Anesthesiologists (ASA) physical status, comorbidities, surgery emergency status, hospitalisation type, anaesthesia type or type of surgical procedure. We also excluded cardiac, obstetrics, transplants, radiology, radiotherapy acts, pre-anaesthetic consultations, and other non-surgical procedures (such as pain treatment), as well as procedures in ASA 5 and 6 patients (a flowchart of included and excluded patients is provided in supplementary figure S1 in appendix 1).
An adverse event was defined as “a particular event requiring either one or more measures to be taken to avoid further deterioration or to treat a situation that is currently or potentially serious, and which does not routinely occur during the conduct of anaesthesia” [20].
For this study, we focused only on adverse events occurring between the arrival of the patient in the operating room and their exit to the recovery room, defined as IAEs. The primary outcome was the occurrence of any IAE (irrespective of the severity grading of the individual events as this information was not available), and the secondary outcomes were the occurrence of technical, cardiovascular, organisational, respiratory, and general events. A detailed list and definitions of these events are available in previously published works [5, 21] and were summarised in tables S1 and S4 in appendix 1.
A full description of the independent variables used in the analyses is provided in table S1 (appendix 1). They can be grouped as factors related to patient, anaesthesia, surgery, and hospital. Patient-related factors comprised age, divided into five quantiles, gender, ASA physical status from 1 to 4, and comorbidities (grouped into six categories: none, cardiovascular, respiratory, general, risk factors, others, see table S1 for details). Factors related to anaesthesia contained information about the type of anaesthesia performed and the duration of the procedure (divided into six categories). Surgery-related factors contained information about the surgical procedures (grouped in seven surgical specialties) and the surgery emergency status. Factors related to the hospital specified the year of the procedures and an indicator variable for each hospital.
Descriptive data are shown as numbers and percentages for categorical variables, mean and standard deviation (SD) when symmetrically distributed, and median and interquartile range (IQR) when skewed. To compare outpatients with inpatients, Student’s t-test, the chi-square test and Wilcoxon rank-sum test were used, depending on the variable type. The data have a complex multi-level structure, with crossed effects and multiple memberships (patients are nested within the cross-classification of procedures and hospitals, and a patient may have several procedures). Therefore, primary and secondary endpoints were modelled using multi-level logistic regression models with fixed effects [22]. At each level, potentially confounding variables were included. Variables at the first level were related to patients (age, gender, ASA status, comorbidities), interventions (degree of emergency, duration of anaesthesia) and anaesthesia (general, loco-regional, combined and standby); and those at the second cross-classified levels were related to procedure and hospital characteristics. All these variables were included in all the models estimated and no variable selection was performed. The variable “year” was included in the regression models using a cubic polynomial to assess the time trend on the probabilities (i.e., to assess whether there was some kind of “technical” progress over time). The marginal probability of each outcome at years 2000, 2004, 2008, 2012, and 2016 was computed and plotted to visualise the time trend. The goodness of fit of the model was assessed by the Hosmer-Lemeshow test and the calibration belt (when the power of the test was too high due to the very large sample sizes), and the discriminatory power by the area under the receiver operating characteristic (ROC) curve [23, 24]. Given the size of our data sample, the focus should be on effect sizes and 95% confidence intervals (CIs) rather than on p-values. All analyses were performed using Stata version 15.1 (StataCorp, College Station, TX, USA).
From 1 January 2000 to 31 December 2016, 3,496,201 anaesthesia procedures were conducted in the 32 hospitals participating in the IAE data collection of the ADS project. After applying our exclusion criteria, 1,066,049 procedures remained for the descriptive analysis and 289,948 (27%) were outpatient procedures (fig. S1 in appendix 1).
Inpatients were older than outpatients (58 vs 51 years; table S2 in appendix 1). Twenty-two percent of inpatients were classified as ASA 1 versus 35% of outpatients, whereas 27% of inpatients had an ASA score above 3 vs 13% in outpatients (p <0.001). Over the 17 years, the yearly distribution of the ASA scores remained quite uniform, with ASA 1–2 cases representing between 85% and 90%, ASA 3 cases between 10% and 14%, and ASA 4 cases between 0.4% and 1.4%.
General anaesthesia was more frequently performed in inpatients than in outpatients (61% vs 48%), whereas regional anaesthesia and stand-by / monitored anaesthesia care (MAC) was used more for outpatients than inpatients (50% vs 30%, p <0.001). The mean duration of anaesthetic procedures was longer in inpatients than in outpatients (137 vs 74 min, p <0.001). Urology and general surgeries were performed more frequently in inpatients than outpatients, whereas gynaecology, ophthalmology and ear-nose-throat (ENT) procedures were performed more in outpatients than inpatients, p <0.001.
No IAE occurred in most (91.4%) of the procedures carried out on ambulatory patients (table S3). When comparing characteristics of ambulatory patients with and without IAE, we observed that patients who had IAEs had a higher ASA score, more comorbidities, more frequently underwent a general or combined anaesthesia, an ENT or orthopaedic surgical procedure, and had longer durations of anaesthetic procedures.
The prevalence of IAEs overall (8.6%) and by category of IAE is provided in table S4. The category with the highest prevalence of IAEs was cardiovascular incidents (2.32%), followed by technical incidents (1.89%), and organisational incidents (1.42%). The categories with the least IAEs were general (0.96%) and respiratory incidents (0.78%). Since the incident type in the “others” category was unknown, this category was not included in our secondary analyses. Unavailable surgeon was the most frequent IAE (1.14%), followed by insufficient sedation (0.87%), hypotension (0.81%), technical problems (0.74%) and delayed wake-up (0.71%). In contrast, the least prevalent IAEs were oliguria (<0.01%), dental lesions (0.01%), myocardial ischaemia (0.01%) and resuscitation (0.01%).
Results of the multilevel logistic regression analysis of the primary outcome (i.e., any IAE) are provided in table S5. Increasing age, ASA score, duration of anaesthetic procedures and comorbidities (except respiratory factors) increased the risk of IAE occurrence. Women were less at risk than men. Regarding the type of anaesthetic procedure, combined procedures were associated with an increased risk of IAEs (with respect to general anaesthesia), while loco-regional anaesthesia and stand-by/MAC were at a lower risk. Regarding surgical procedures, urology, ophthalmology, and ENT were associated with an increased risk of IAE. There was no association between the degree of emergency of surgery and IAE occurrence. To ease the interpretation of the results in table S5 and allow one to visualise the time trends, the marginal probabilities of IAEs have been plotted in figures S2–S8 in appendix 1.
The fitted cubic polynomial of time showed that there was a clear decreasing time trend in the overall incidence IAEs between 2000 and 2016 (fig.1).

Figure 1 Marginal probability of overall IAE occurrence in ambulatory anaesthesia between 2000 and 2016.
Notice that the origin of the y-axis does not start at 0.
The marginal probability of IAEs decreased from 10.8% in the year 2000 to 6.3% in 2016.
As regards secondary outcomes, figure 2 illustrates that the marginal probabilities of specific IAEs also decreased over the 2000–2016 period, except for the category of general incidents.
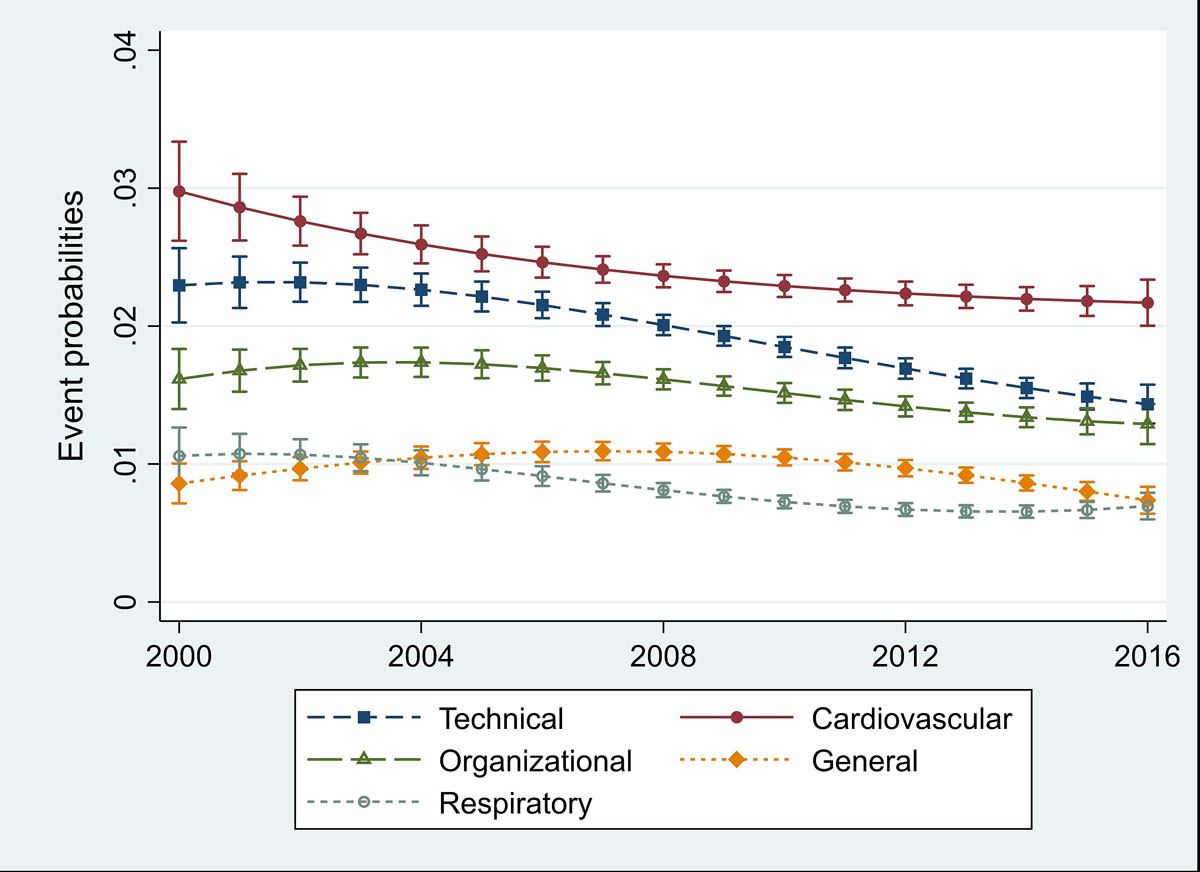
Figure 2 Marginal probability of specific IAE occurrence in ambulatory anaesthesia between 2000 and 2016.
For technical incidents, the probabilities decreased from 2.3% to 1.4%, for cardiovascular from 3.0% to 2.2%, for organisational from 1.6% to 1.3%, for respiratory from 1.1% to 0.7%, and for general incidents from 0.9% to 0.7%.
The goodness of fit analysis showed that the calibration and discriminatory power of all the models were good (for the primary outcome the area under the ROC curve = 0.74).
We studied 1,066,049 anaesthesia procedures performed in 32 Swiss anaesthesia departments, between 2000 and 2016. Out of these, 73% (776,101) were inpatient and 27% (289,948) were outpatient. Our study showed that over this period the average incidence of IAEs was 16.1% in inpatients and 8.6% in outpatients, and that technical incidents and cardiovascular incidents were the most prevalent IAEs among outpatients. However, the incidence of IAEs was not constant and showed a continuously decreasing trend over the seventeen years of study analysis.
We found a higher rate of IAEs (8.6%) than Chung et al. [25] (3.95%). This difference might be explained by the change in outpatient practice since the Chung et al. study was published two decades ago. With the ongoing transition from inpatient to outpatient, many surgical procedures that required hospitalisation, such as carpal tunnel release, vein ligations, or cataract surgery, are now more commonly performed in outpatient settings [26, 27]. In particular, there is an increasing number of older and more at-risk patients treated in ambulatory. This more at-risk case mix could temporarily lead to an increase in IAEs when shifting from inpatient to outpatient surgery setting, but over time the incidence should decline with management/technical improvements (such as the deployment of monitoring equipment) and staff training (such as nontechnical skills development) [28–30]. To ensure patient safety, risk assessment procedures are nowadays implemented prior to the anaesthesia, according to available guidelines. High-risk patients will be eligible for ambulatory surgery only if appropriate resources are provided. Fecho et al. explored the occurrence of IAEs between 2004 and 2005 [30]. They reported a rate of 1.45% in outpatients [30]. This is quite a lot lower than in our study during the same period (7.3%). This difference can be explained by the criteria used to define IAEs. In their study, they focused on serious perioperative complications, whereas in our study we included a broader array of intraoperative complications.
In the multilevel regression analyses, we found a clear decreasing time trend in the overall incidence of IAEs, as well as in the incidence of most of the specific IAEs. Given the adjustment for many potential confounders and, importantly, for hospital effect, under the assumption that reporting quality varied across institutions but remained more or less constant over time within an institution/team, this time trend may be interpreted as some kind of “technical progress”, possibly due to improvements in techniques used, drugs, training, management, etc. Unfortunately, given the limited information recorded in the registry, we were not able to identify the precise reasons for this diminishing trend. The fact that the occurrence of IAEs varied substantially across hospitals (there was a ratio of 18 between the smallest and largest odds ratios), despite adjustment for many potential confounders, might be explained by residual confounding but also by the “safety culture” (i.e., some teams may have recorded an adverse event as soon as it occurred, even if it was a minor event, whereas others may have coded only events that persisted for a long time or those that were severe). Also, the interpretation and use of the definitions of adverse events might have varied across the hospitals [31–33]. Nevertheless, given that our analyses were adjusted for the hospital effect, in addition to numerous patients, anaesthesia and surgery characteristics, the observed decreasing time trend may not be attributable to the differences across hospitals (including in the reporting of incidents) but rather to the above-mentioned “technical progress”.
We found that age, ASA score, patient’s comorbidities, gender, duration of the procedure, general and combined anaesthesia, were associated with the risk of IAEs. Others found similar associations [21, 25, 34–36], therefore confirming that these variables were important confounders to include in our regression analyses.
This study naturally has several limitations. First, this was an observational study of routinely collected data based on voluntary participation and coding quality may have differed across institutions. Nevertheless, given that the data were collected using a standardised protocol and that the very large number of observations allowed us to adjust for a large array of potential confounders, in addition to the hospital, we believe that the time trend found is real. Second, there were many missing values and the records of interventions were simply deleted (complete case analysis). Given the extremely large sample size, we did not envisage carrying out multiple imputations. Implicitly, this means that we assumed that data were missing completely at random. Third, it was not possible to take into account the severity grading of the adverse events, as this information was not available. Nevertheless, we believe that this is not of concern for assessing the overall time trend of events. Fourth, using a standardised protocol is naturally limitative as some IAE may be difficult to catalogue. In addition, the list of adverse events was not exhaustive. Other events may have occurred and, since there was no corresponding code, anaesthesiologists coded them as "Others". This may explain the relatively high incidence of the "Others" category. Finally, as participation was voluntary one cannot exclude that the worst performing institutions may have not participated. Nevertheless, given the adjustment for the hospital effect in the analyses, this is not of concern regarding the time trend.
In sum, despite the above-mentioned limitations, given that we analysed data collected prospectively, from a large number of Swiss hospitals, over a relatively long period of 17 years, and that these routinely collected data reflect the daily activities of the hospital services participating in the project, as well as the problems they experienced in per- and postoperative setting, we believe that our results are illustrative of the “technical” progress made in anaesthesia in Switzerland during the period 2000-2016.
In conclusion, our study shows that the occurrence of IAE in ambulatory anaesthesia has been continuously decreasing between 2000 and 2016. This trend is essentially attributable to the reduction in the incidence of technical, cardiovascular, and organisational events, whereas the event rates of general and respiratory events were already very low and remained somewhat constant.
Table S1: Description of the dependent and independent variables.
Table S2: Characteristics of inpatients and outpatients.
Table S3: Comparison of outpatients with and without intraoperative adverse events.
Table S4: Prevalence of intraoperative adverse events in ambulatory surgery (n = 289,948).
Table S5: Multilevel logistic regression analysis of overall intraoperative adverse events in patients undergoing ambulatory anaesthesia.
Figure S1: Flowchart of included and excluded patients.
Figure S2: Probability of overall intraoperative adverse event occurrence by age.
Figure S3: Probability of overall intraoperative adverse event occurrence by gender.
Figure S4: Probability of overall intraoperative adverse event occurrence by ASA (American Society of Anesthesiologists) score.
Figure S5: Probability of overall intraoperative adverse event occurrence by comorbidity.
Figure S6: Probability of overall intraoperative adverse event occurrence by emergency status.
Figure S7: Probability of overall intraoperative adverse event occurrence by anaesthesia type.
Figure S8: Probability of overall intraoperative adverse event occurrence by surgical procedure type.
The appendix is available as a separate file at: https://smw.ch/article/doi/smw.2020.20365.
The authors are thankful to the ADS study group for allowing the use of the ADS database.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Kaafarani HMA , Rosen AK , Nebeker JR , Shimada S , Mull HJ , Rivard PE , et al. Development of trigger tools for surveillance of adverse events in ambulatory surgery. Qual Saf Health Care. 2010;19(5):425–9.
2 Kumar G , Stendall C , Mistry R , Gurusamy K , Walker D . A comparison of total intravenous anaesthesia using propofol with sevoflurane or desflurane in ambulatory surgery: systematic review and meta-analysis. Anaesthesia. 2014;69(10):1138–50. doi:.https://doi.org/10.1111/anae.12713
3 Gupta A , Stierer T , Zuckerman R , Sakima N , Parker SD , Fleisher LA . Comparison of recovery profile after ambulatory anesthesia with propofol, isoflurane, sevoflurane and desflurane: a systematic review. Anesth Analg. 2004;98(3):632–41. doi:.https://doi.org/10.1213/01.ANE.0000103187.70627.57
4 Cullen KA , Hall MJ , Golosinskiy A . Ambulatory surgery in the United States, 2006. Natl Health Stat Rep. 2009;11(11):1–25.
5 Pittet V , Perret C , Moret V , Despond O , Burnand B ; ADS Study Group. Evolution of anaesthesia care and related events between 1996 and 2010 in Switzerland. Acta Anaesthesiol Scand. 2013;57(10):1275–86. doi:.https://doi.org/10.1111/aas.12177
6Roth S, Pellegrini S. Virage ambulatoire: transfert ou expansion de l’offre de soins? (in French) Swiss Health Observatory 2015. Available at https://www.obsan.admin.ch/sites/ default/files/publications/2015/obsan_68_rapport_0.pdf
7Prestations ambulatoires dans les hôpitaux et les cliniques (in French). Available at: https://www.hplus.ch/fileadmin/hplus.ch/public/Medien/Medienkonferenzen/JMK_2014/20.05.2014/20140520_Faktenblatt_F.pdf
8 Cooper JB , Gaba D . No myth: anesthesia is a model for addressing patient safety. Anesthesiology. 2002;97(6):1335–7. doi:.https://doi.org/10.1097/00000542-200212000-00003
9 Brown RH . Risk and Outcome in Anesthesia. Anesthesiology. 1992;77:839.
10 Beecher HK , Todd DP . A study of the deaths associated with anesthesia and surgery: based on a study of 599, 548 anesthesias in ten institutions 1948-1952, inclusive. Ann Surg. 1954;140(1):2–33. doi:.https://doi.org/10.1097/00000658-195407000-00001
11 Memery HN . Anesthesia mortality in private practice. A ten-year study. JAMA. 1965;194(11):1185–8. doi:.https://doi.org/10.1001/jama.1965.03090240019004
12 Arbous MS , Meursing AEE , van Kleef JW , de Lange JJ , Spoormans HHAJM , Touw P , et al. Impact of anesthesia management characteristics on severe morbidity and mortality. Anesthesiology. 2005;102(2):257–68, quiz 491–2. doi:.https://doi.org/10.1097/00000542-200502000-00005
13 Haller G , Laroche T , Clergue F . Morbidity in anaesthesia: today and tomorrow. Best Pract Res Clin Anaesthesiol. 2011;25(2):123–32. doi:.https://doi.org/10.1016/j.bpa.2011.02.008
14 McHardy FE , Chung F . Postoperative sore throat: cause, prevention and treatment. Anaesthesia. 1999;54(5):444–53. doi:.https://doi.org/10.1046/j.1365-2044.1999.00780.x
15 Lienhart A , Auroy Y , Péquignot F , Benhamou D , Warszawski J , Bovet M , et al. Survey of anesthesia-related mortality in France. Anesthesiology. 2006;105(6):1087–97. doi:.https://doi.org/10.1097/00000542-200612000-00008
16 Van de Velde M , Schepers R , Berends N , Vandermeersch E , De Buck F . Ten years of experience with accidental dural puncture and post-dural puncture headache in a tertiary obstetric anaesthesia department. Int J Obstet Anesth. 2008;17(4):329–35. doi:.https://doi.org/10.1016/j.ijoa.2007.04.009
17 Paech M , Banks S , Gurrin L . An audit of accidental dural puncture during epidural insertion of a Tuohy needle in obstetric patients. Int J Obstet Anesth. 2001;10(3):162–7. doi:.https://doi.org/10.1054/ijoa.2000.0825
18 Fasting S , Gisvold SE . Statistical process control methods allow the analysis and improvement of anesthesia care. Can J Anaesth. 2003;50(8):767–74. doi:.https://doi.org/10.1007/BF03019371
19 Bothner U , Georgieff M , Schwilk B . Building a large-scale perioperative anaesthesia outcome-tracking database: methodology, implementation, and experiences from one provider within the German quality project. Br J Anaesth. 2000;85(2):271–80. doi:.https://doi.org/10.1093/bja/85.2.271
20 Fasting S , Gisvold SE . Data recording of problems during anaesthesia: presentation of a well-functioning and simple system. Acta Anaesthesiol Scand. 1996;40(10):1173–83. doi:.https://doi.org/10.1111/j.1399-6576.1996.tb05547.x
21 Beyer K , Taffé P , Halfon P , Pittet V , Pichard S , Haller G , et al.; ADS study Group. Hypertension and intra-operative incidents: a multicentre study of 125,000 surgical procedures in Swiss hospitals. Anaesthesia. 2009;64(5):494–502. doi:.https://doi.org/10.1111/j.1365-2044.2008.05821.x
22 Lehtonen R . Multilevel Statistical Models. Harvey Goldstein. J Am Stat Assoc. 2005;100(469):353–4. doi:.https://doi.org/10.1198/jasa.2005.s9
23 Finazzi S , Poole D , Luciani D , Cogo PE , Bertolini G . Calibration belt for quality-of-care assessment based on dichotomous outcomes. PLoS One. 2011;6(2):e16110. doi:.https://doi.org/10.1371/journal.pone.0016110
24Hosmer DW, Lemeshow S. Applied logistic regression. 2nd edition. New York: Wiley; 2000.
25 Chung F , Mezei G , Tong D . Adverse events in ambulatory surgery. A comparison between elderly and younger patients. Can J Anaesth. 1999;46(4):309–21. doi:.https://doi.org/10.1007/BF03013221
26 Hull L , Arora S , Aggarwal R , Darzi A , Vincent C , Sevdalis N . The impact of nontechnical skills on technical performance in surgery: a systematic review. J Am Coll Surg. 2012;214(2):214–30. doi:.https://doi.org/10.1016/j.jamcollsurg.2011.10.016
27Etat des lieux 2015 sur l’activité de chirurgie ambulatoire Programme national chirurgie ambulatoire (in French). Available At: https://www.atih.sante.fr/sites/default/ files/public/content/1504/note_gdr_chirambu_2015.pdf
28 Catchpole K , Mishra A , Handa A , McCulloch P . Teamwork and error in the operating room: analysis of skills and roles. Ann Surg. 2008;247(4):699–706. doi:.https://doi.org/10.1097/SLA.0b013e3181642ec8
29 Parker SH , Flin R , McKinley A , Yule S . Factors influencing surgeons’ intraoperative leadership: video analysis of unanticipated events in the operating room. World J Surg. 2014;38(1):4–10. doi:.https://doi.org/10.1007/s00268-013-2241-0
30 Fecho K , Moore CG , Lunney AT , Rock P , Norfleet EA , Boysen PG . Anesthesia-related perioperative adverse events during in-patient and out-patient procedures. Int J Health Care Qual Assur. 2008;21(4):396–412. doi:.https://doi.org/10.1108/09526860810880207
31 Bothner U , Georgieff M , Schwilk B . Validation of routine incidence reporting of one anaesthesia provider institution within a nation-wide quality of process assessment program. J Clin Monit Comput. 1998;14(6):305–11. doi:.https://doi.org/10.1023/A:1009922313572
32 Benson M , Junger A , Fuchs C , Quinzio L , Böttger S , Jost A , et al. Using an anesthesia information management system to prove a deficit in voluntary reporting of adverse events in a quality assurance program. J Clin Monit Comput. 2000;16(3):211–7. doi:.https://doi.org/10.1023/A:1009977917319
33 Patel S , Rajkomar A , Harrison JD , Prasad PA , Valencia V , Ranji SR , et al. Next-generation audit and feedback for inpatient quality improvement using electronic health record data: a cluster randomised controlled trial. BMJ Qual Saf. 2018;27(9):691–9. doi:.https://doi.org/10.1136/bmjqs-2017-007393
34 Ansell GL , Montgomery JE . Outcome of ASA III patients undergoing day case surgery. Br J Anaesth. 2004;92(1):71–4. doi:.https://doi.org/10.1093/bja/aeh012
35 Fasting S , Gisvold SE . [Serious intraoperative problems--a five-year review of 83,844 anesthetics]. Can J Anaesth. 2002;49(6):545–53. doi:.https://doi.org/10.1007/BF03017379
36 Taffé P , Sicard N , Pittet V , Pichard S , Burnand B ; ADS study group. The occurrence of intra-operative hypotension varies between hospitals: observational analysis of more than 147,000 anaesthesia. Acta Anaesthesiol Scand. 2009;53(8):995–1005. doi:.https://doi.org/10.1111/j.1399-6576.2009.02032.x
No financial support and no other potential conflict of interest relevant to this article was reported.