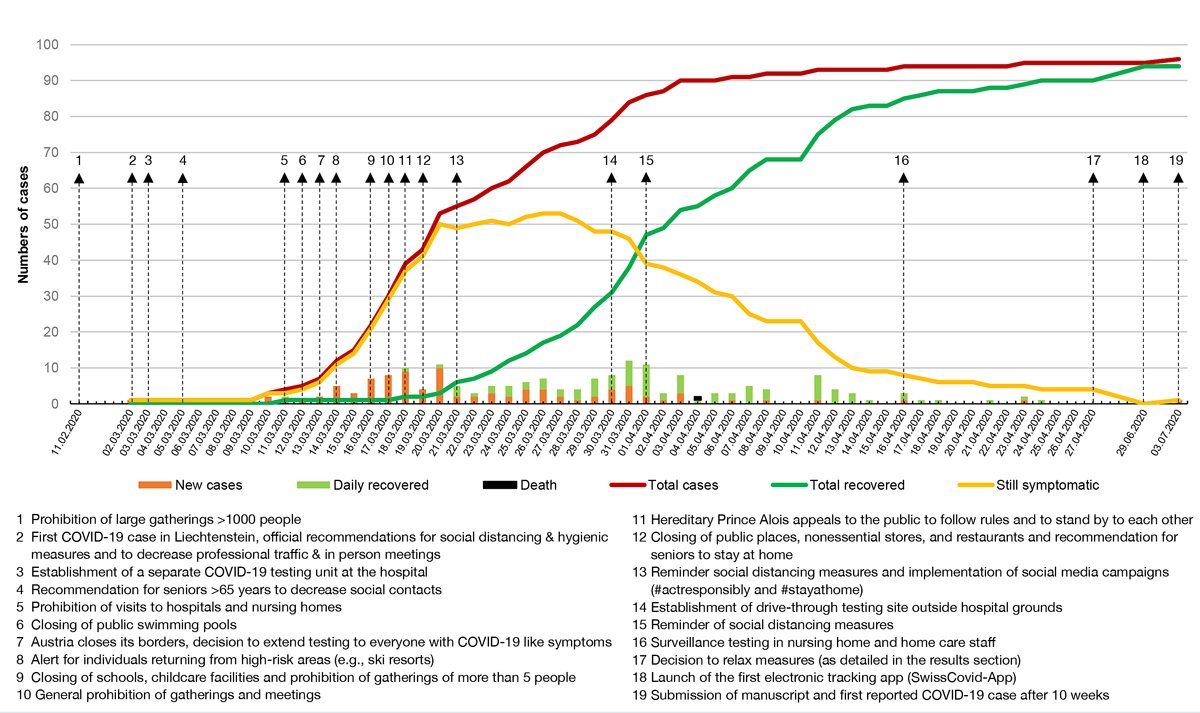
Figure 1 Timeline of PCR-confirmed COVID-19 cases in Liechtenstein with reference to public health measures taken during the first wave.
DOI: https://doi.org/10.4414/smw.2020.20361
SARS-CoV-2, the new coronavirus responsible for the “coronavirus disease 2019” (COVID-19) pandemic, was first reported in Wuhan, Hubei Province, China, in December 2019 [1]. SARS-CoV-2 causes COVID-19, an acute respiratory distress syndrome with a great variety of possible symptoms. The most common symptoms include coughing, fever, headache, fatigue, anosmia and ageusia [2–4].
After the initial outbreak in Wuhan could not be contained, the virus quickly spread across the globe and was declared a pandemic by the World Health Organization (WHO) on 11 March 2020.
In response to the pandemic, different recommendations and measures to mitigate the spread of the disease were implemented. The main aim was to decrease the number of patients who required hospitalisation or intensive care. These measures included the reinforcement of hygiene (e.g., correctly washing one’s hands; using disinfectant; not touching one’s eyes, nose or mouth; and maintaining respiratory etiquette, such as covering one’s mouth and nose with one’s elbow or a tissue when sneezing or coughing) and a policy of physical (also called “social”) distancing [5, 6].
The WHO recommended that everyone maintain a distance of at least one meter between themselves and the person nearest to them when outside their home, while the Swiss Federal Office of Public Health (FOPH) recommended a distance of at least two meters between individuals [7]. Austria closed its borders on 13 March 2020, and thus travel and crossing borders were restricted according to the Schengen Agreement [8]. Gatherings of more than five people were prohibited in Switzerland on 20 March 2020 [7]. The WHO and the FOPH also recommended staying away from crowded places, working from home if possible and stopping all travel [9–11]. Individuals were instructed to stay at home in self-isolation for at least 10 (FOPH) to 14 days (WHO) if they or a close contact showed COVID-19-related symptoms such as a temperature over 38.0°C or coughing [12].
The principality of Liechtenstein is a double-landlocked country between Austria and Switzerland. The country has a surface area of 160 km2, and at the end of 2019 it was home to 38,749 residents, resulting in a population density of 242 residents per km2. The median age of the residents is 42 years [13, 14]. The health system is characterised by mandatory health insurance. There is one national hospital in Liechtenstein. However, residents also have access to outpatient and/or hospital care in Switzerland and Austria. The country forms a customs union with the Swiss Confederation in accordance with their customs treaty and is subject to the Swiss Epidemics Act of 2012 [15]. One of the measures by its neighbouring countries that affected Liechtenstein was that Austria closed its borders to Liechtenstein, such that only people with proof of employment in Liechtenstein were allowed to cross the border [16]. Liechtenstein and Switzerland have close diplomatic and economic relations with each other and therefore have open borders. During the pandemic, there was no change in the border control between these two countries [17].
The course of the COVID-19 pandemic in Liechtenstein was characterised by the early implementation of epidemiologic measures, as well as a lack of major events promoting the spread of the pandemic (such as carnivals or soccer games). The epidemiological measures were adopted from Switzerland and were relatively mild compared to those of other European countries: the population was never put under lockdown, it maintained the right to move freely, and gatherings of up to five persons were allowed. Most importantly, the population adhered well to the measures recommended by the government. Liechtenstein’s last documented COVID-19 case during the first wave of the pandemic was on 23 April 2020. Hence, it was one of the first countries to flatten the COVID-19 infection curve completely during the first wave of the pandemic. On the day of the submission of this manuscript for publication, after nearly 10 weeks without a confirmed case, another case of COVID-19 was reported on 3 July 2020.
The aim of this study was to characterise the development of the COVID-19 pandemic in Liechtenstein and to highlight the containment strategies used in its initial phase. Since it is suspected that many COVID-19 cases go unnoticed due to a lack of symptoms or the presence of only mild symptoms, and are therefore not included in the disease statistics of public health agencies, it can be expected that the actual number of cases among the general population is higher [18]. We therefore investigated whether additional cases could be detected. To do so, we included not only the diagnosed COVID-19 patients but also their close household and workplace contacts.
This is an observational study describing all the patients who had a real-time polymerase chain reaction (RT-PCR)-confirmed diagnosis of COVID-19 infection (RT-PCR-confirmed patients = RCP) in the Principality of Liechtenstein during March and April 2020. Until 29 March 2020, the country’s health system centralised all suspected COVID-19 cases for diagnosis and treatment at the national hospital (Landesspital Liechtenstein) [19]. Starting on 30 March 2020, suspected COVID-19 cases were referred to either a drive-through testing facility or the national hospital, depending on the severity of their symptoms [20]. Cases were meticulously monitored for their health status. After the pandemic revealed no new cases in the country for one week (i.e., from 30 April 2020), we invited the country’s surviving COVID-19 patients for a follow-up visit that included taking their medical history and blood samples. These patients were questioned about their household contacts (individuals living in the same household or relatives/friends they spent a substantial amount of time in close proximity to around the time of symptom onset) and close workplace contacts (individuals who spent at least 15 minutes in the same office as them in the two days prior to symptom onset), and these contacts were asked to participate (antibody testing and history taking) in the study. When their blood samples were taken, these contacts were also asked about COVID-19 symptoms using a standardised questionnaire, and their vitals (blood pressure, SO2, temperature) were recorded. The study protocol was verified by the Kantonale Ethikkommission Zürich (BASEC-Number 2020-00676). The study participants (both patients and close contacts) gave written informed consent for their participation in the study. The study is in accordance with the Declaration of Helsinki, as revised in 2013, and was funded with a grant from the Liechtenstein Ministry of Health.
To identify COVID-19 patients with severe symptoms at an early stage, the national hospital established a so-called monitoring and early warning system, through which confirmed COVID-19 patients were called periodically by medical doctors. Patients were asked to come in for a thorough clinical examination, as well as laboratory and imaging investigations, if their condition worsened. Using a standardised questionnaire, the patients’ baseline data (date of birth, sex, country of residence), symptoms, risk factors (pre-existing medical conditions, smoking status), conventional contact-tracing information (i.e., asking patients about their contacts) and suspected mode of transmission were recorded in a database. By contacting the patients on average every 48 hours over the course of at least 10 days and until 2 days after the complete resolution of their symptoms, an extensive follow-up database was built. From 2 March to 23 April 2020, 95 patients were included in this database. Even though Liechtenstein instructed its inhabitants to visit the national hospital in the case of a suspected COVID-19 infection, individuals were also allowed to attend hospitals in the neighbouring countries of Switzerland and Austria. If such a hospital visit occurred, then by law, institutions from both countries had to report the cases of COVID-19 in patients residing in Liechtenstein to the Liechtenstein Office of Public Health. To ensure that the national hospital’s database was representative of the country’s COVID-19 cases, the database was crosschecked with the official national record of reported COVID-19 cases. COVID-19 infection was confirmed by RT-PCR testing with a COBAS 6800 analyser (Roche Diagnostics, Rotkreuz, Switzerland). This method targets the E-Gene and the Orf1ab gene and has a lower limit of detection of 25 copies/ml. At the time of follow-up (at least three weeks after symptom onset or 23 April 2020 in asymptomatic individuals), the patients and their household contacts underwent serological testing from venous blood samples using an electrochemiluminescence immunoassay (ECLIA) run on a COBAS 6000 analyser (Roche Diagnostics, Rotkreuz, Switzerland). Positive results were subsequently confirmed through CE-marked, enzyme-linked immunoassays (ELISA; Euroimmune SARS-CoV-2 IgG and IgA; Lucerne, Switzerland) run on a DSX analyser (Dynex Technologies, Denkendorf, Germany). In the case of capillary blood sampling (n = 5), a validated, CE-marked, gold nanoparticle-based immunochromatographic test kit for the qualitative determination of COVID-19 IgM and IgG antibodies, which displays a high specificity for IgG, was used (Sugentech SGTi-flex COVID-19 IgM/IgG, Disposan, Schlieren, Switzerland). Furthermore, the patients and their household contacts were characterised with a metabolic and haematological panel (alkaline phosphatase, total bilirubin, alanine aminotransferase, aspartate aminotransferase, gamma-glutamyltransferase, lactate dehydrogenase, creatine kinase, lipase, creatinine, estimated glomerular filtration rate, uric acid, albumin, protein, calcium, sodium, potassium, phosphate, lipid panel, HbA1c, glucose, complete blood count, C-reactive protein, thyroid stimulating hormone, vitamin B12, folate and D-dimer) utilising standard, routine methods. All laboratory measurements were performed in an ISO 17025-accredited medical laboratory authorised by the Swiss Federal Office of Public Health. We also screened the media releases of the Liechtenstein government during February to June 2020 to systematically summarise the implemented COVID-19-related public health measures.
Continuous variables were given as medians and interquartile ranges (IQRs), whereas proportions were given as percentages with 95% confidence intervals (CIs). Associations between variables were calculated with Spearman’s rank correlation. Medians were compared with the Mann-Whitney U-test or the Kruskal-Wallis test, followed by Conover’s post hoc test. Proportions were compared using a chi-square test. A p-value <0.05 was considered statistically significant. Medcalc version 18.11.3 (Mariakerke, Belgium) was used for statistical computations. Graphs were drawn with Excel (Microsoft, Seattle, USA) and Adobe Illustrator (Adobe Inc., Delaware, USA).
The first case of COVID-19 confirmed by RT-PCR in Liechtenstein was diagnosed on 2 March 2020. To stop the spread of the pandemic, the government of Liechtenstein implemented the following political measures in a stepwise manner: the establishment of a national task force involving all stakeholders on 2 February 2020; the establishment of a separate testing unit at the national hospital on 3 March 2020; the prohibition of visits to patients in the hospital or people in care facilities on 11 March 2020; the prohibition of social gatherings of more than five people and the closing of schools and universities on 16 March 2020; and the closing of some public places (such as public playgrounds and sports facilities), nonessential shops (all shops except pharmacies and food stores) and restaurants on 19 March 2020 [17, 21, 22]. Public transport was reduced, with low occupancy of transport vehicles [23]. There was never an official recommendation or requirement to wear masks in public, and people could move freely at all times, even though it was recommended that they stay at home, follow hygienic measures such as hand washing and hand disinfection, and practice social distancing whenever possible. Universal mask wearing was mandatory in all healthcare institutions, whether or not there was any patient contact. Healthcare workers were required to wear personal protective equipment (e.g., gloves, gowns, eye-protection, FFP3 masks) when caring for suspected or confirmed COVID-19 cases. Samples from suspected COVID-19 cases for testing were primarily taken at the Landesspital Liechtenstein (LLS). On 30 March 2020, an additional drive-through testing facility in Vaduz was established outside the hospital grounds [20]. Testing was available to the residents of Liechtenstein and to anyone working in Liechtenstein, regardless of their place of residence. The test criteria varied over time and were adapted according to the official recommendations of the FOPH. Initially, only people who had recently travelled to a high-risk region or had been in contact with a confirmed COVID-19 case and who showed specific symptoms (temperature ≥38°C and/or signs of an upper airway infection) were tested [12]. After the disease had spread across several European countries, the test criteria were changed to include people showing specific symptoms and meeting at least one additional criterion, such as the need for hospitalisation, bilateral pneumonia of unknown origin in hospitalised patients, belonging to a high-risk group (e.g., those aged >65 years or with pre-existing conditions such as cancer, heart or lung disease) or being a healthcare worker [24]. On 13 March 2020 it was decided to extend the threshold for testing to anyone showing symptoms compatible with COVID-19 infection. The cost of the RT-PCR test was covered by mandatory insurance. However, depending on individual insurance plans, some patients had to pay a deductible. RCP were instructed to stay at home in self-isolation for at least 10 days after symptom onset and until 2 days after the complete resolution of their symptoms [25]. Self-isolation measures recommended by the Liechtenstein Office of Public Health included staying alone in a designated room in the home, even when consuming meals, and, if possible, using a separate bathroom from the rest of the household. Cutlery, towels and toiletries were not to be shared and regular washing of clothes, towels and bedding was recommended. A distance of at least two metres from others had to be kept, and if the patients had to leave their home for a doctor’s visit, wearing a mask was mandatory. Patients who lived alone were asked to have food and medications delivered to their doorstep by relatives, acquaintances or delivery services. Patients were instructed to inform their close contacts and these individuals also had to quarantine for 10 days.
After exponential growth during the first 10 days after the diagnosis of the second case on 10 March 2020, the number of new RT-PCR-confirmed infections steadily decreased (fig. 1). The last recorded case occurred on 23 April 2020. A detailed overview of the public health measures is provided in figure 1. After several days with no new infections, the government decided to relax the prevention measures, starting on 27 April 2020 [26].
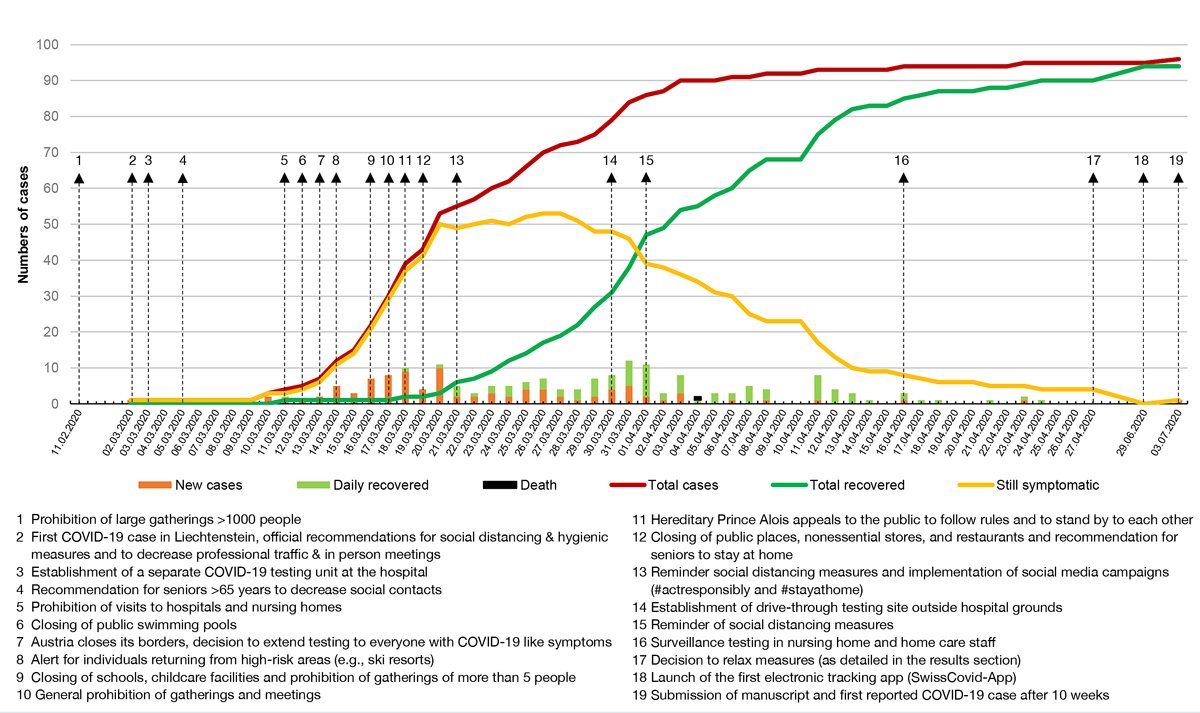
Figure 1 Timeline of PCR-confirmed COVID-19 cases in Liechtenstein with reference to public health measures taken during the first wave.
Special measures and risk-reduction plans had to be universally installed and implemented. In a first step, non-essential shops such as hairdressers, massage and cosmetic studios, and small markets were allowed to open. Businesses had to comply with regulations concerning hygienic measures (e.g., masks were mandatory for employees at hair salons). The hospital and medical practices were allowed to perform elective procedures which had been postponed during the past months due to the pandemic [27]. On 11 May 2020, schools were opened for an in-person orientation week. From 15 May 2020, religious services were allowed to take place and restaurants and bars could open. The maximum number of people at a table was restricted to four and conventional tracking (taking of patrons’ contact information) was established in most places. Businesses from the leisure sector (e.g., museums, libraries, sports centres and outdoor swimming pools) were also allowed to open. Starting on 18 May 2020, all schools and day-care centres were opened [28]. From 6 June 2020, public or private gatherings of up to 300 people were allowed [29].
In-person lectures at the university were allowed from 8 June 2020 [28]. On 26 June 2020 the government decided to revoke all previously implemented measures [30]. On 29 June 2020 the SwissCovid app, the first contact tracing app available in Switzerland and Liechtenstein, was launched, and the Liechtenstein government highly recommended its use [31].
On the day of the submission of this manuscript, 3 July 2020, the first de novo COVID-19 case was reported following a period of 10 weeks without any new cases. During the first wave of the pandemic, the whole population diligently adhered to public health measures, with only a small number of minor breaches reported by the national police [32].
A total of 95 RCP were seen at our institution, of which 82 resided in Liechtenstein. An additional 13 patients residing outside of Liechtenstein were also diagnosed. A flowchart for the inclusion of patients is shown in figure 2. The median age of these cases was 39 years, and gender was equally distributed. Seniors were rarely affected (14%, 95% CI 8–22%); only four patients were in each of the age ranges 65 to 69 years of age, 70 to 79 years of age and 80 to 89 years of age. One 94-year-old patient died 14 days after symptom onset. Of the 95 patients, the deceased and four other patients were not available for follow-up laboratory investigations.
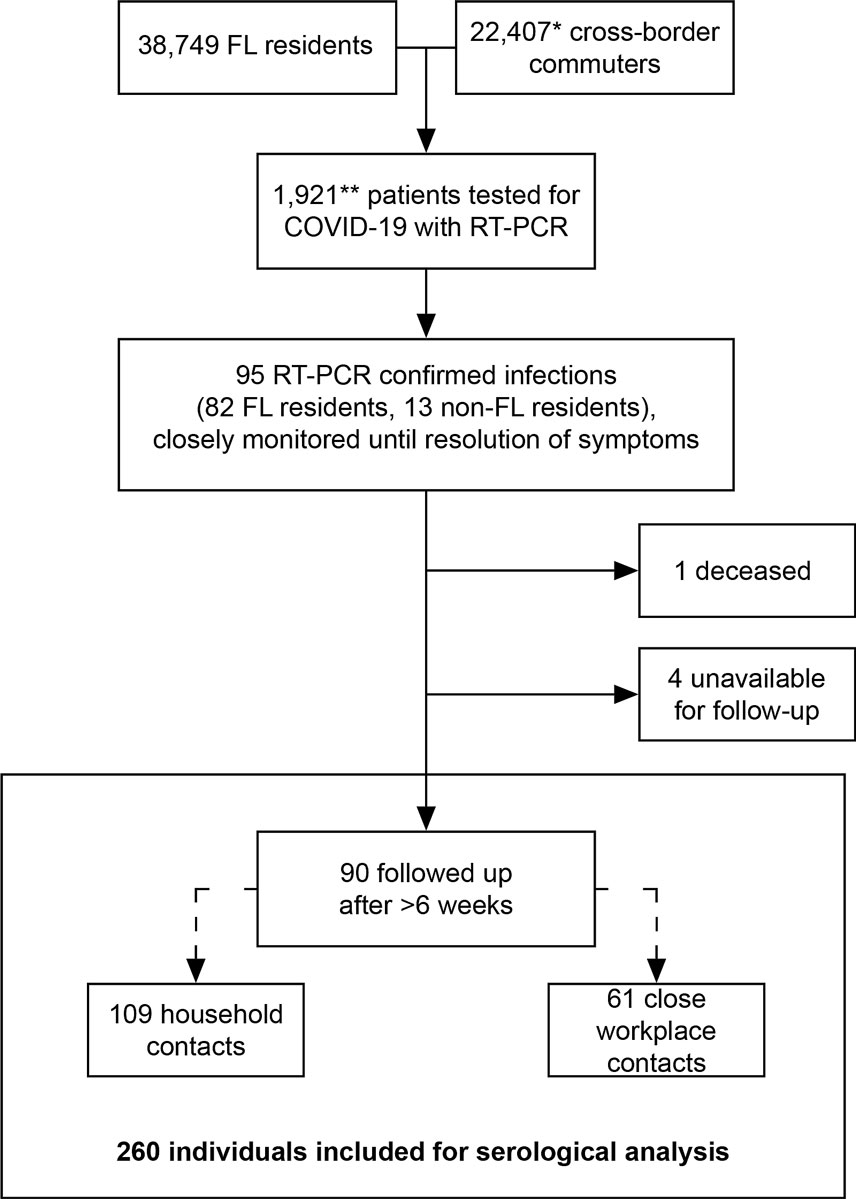
Figure 2 Flowchart of participant inclusion.
* Estimated from the headcount of the workforce residing outside Liechtenstein as per 31 December 2018, corrected for overall workforce growth of 2.6% as per 31 December 2019. Data from the National Office of Statistics Liechtenstein, Vaduz [13, 14].
** As per 23 April 2020 [33]
FL = Fürstentum Liechtenstein, RT-PCR = real-time polymerase chain reaction
Fourteen patients lived alone. The remaining 81 patients lived with 127 individuals, of which 109 (86%, 95% CI 79–91%) consented to participate in the follow-up investigation. Determining the exact number of eligible close workplace contacts was not possible, but 61 people consented to participate in the follow-up investigation. Interestingly, this follow-up investigation identified an additional 35 out of the 109 (32%, 95% CI 24–41%) household contacts and 8 out of the 61 (13%, 95% CI 7–24%) close workplace contacts as having been infected, as confirmed by antibody testing.
The patient characteristics are given in table 1. Notably, the median age of the RCP was relatively young. The investigation of the patients’ household contacts and close workplace contacts with antibody testing identified, on average, one additional COVID-19 case that had not been detected through the official testing guidelines that were in place at the time for every two RCP (43 close contacts of 90 RCP [0.48, 95% Cl 0.38–0.58]). Whereas all the RCP except one, a healthcare professional whose partner had tested positive for COVID-19, showed clinical symptoms of COVID-19 disease, 10 out of the 35 COVID-19 cases discovered among the household contacts (29%, 95% CI 16–45) and 1 out of the 8 COVID-19 cases discovered within the close workplace contacts (13%, 95% CI 3–48%) were asymptomatic. In total, approximately one-fourth (11/43) of the household and close workplace contacts with COVID-19 were asymptomatic.
Table 1 Patient characteristics. Columns depicting the patient characteristics for all RT-PCR confirmed patients (PCR+), all household contacts (Household), all work contacts (Work), contacts with positive serology (Serology+ contacts), and all confirmed COVID-19 patients (PCR+ or serology+ contacts)
| PCR+ | Household | Work | Serology+ contacts | PCR+ or serology+ contacts | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n total = 95 |
Median with (IQR) n
or percentage with 95% CI |
n total = 109 |
Median with (IQR) n
or percentage with 95% CI |
n Total = 61 |
Median with (IQR) n
or percentage with 95% CI |
n total = 43 |
Median with (IQR) n
or percentage with 95% CI |
n total = 138 |
Median with (IQR) n
or percentage with 95% CI |
|
| Sex (female) | 46 | 48% (39–59) | 55 | 50% (41–60) | 26 | 43% (34–55) | 18 | 42% (28–57) | 64 | 46% (38–55) |
| Age (years) | 39 (28; 56) | 38 (23; 52) | 42 (30; 54) | 36 (20; 52) | 41 (25; 55) | |||||
| Country of residence | ||||||||||
| – FL | 82 | 86% (7–;92) | 99 | 91% (84–95) | 28 | 46% (34–58) | 31 | 72% (57–83) | 113 | 82% (74–87) |
| – CH | 12 | 13% (7–21) | 10 | 9% (5–17) | 28 | 46% (34–58) | 11 | 26% (15–40) | 23 | 17% (11–24) |
| – A | 1 | 1% (0.3–6) | 0 | 0% (0–3) | 5 | 8% (4–18) | 1 | 2% (1–12) | 2 | 1% (0.4–5) |
| Smoker | 11 | 11% (7–20) | 14 | 13% (8;21) | 15 | 25% (16–37) | 2 | 5% (1–15) | 13 | 9% (6–15) |
| Preexisting conditions | 23* | 24% (17–34) | 22† | 20% (14–29) | 9‡ | 15% (8–25) | 3§ | 7% (3–19) | 26¶ | 19% (13–26) |
| Exposure | ||||||||||
| – Contact | 38 | 40% (31–50) | – | – | – | – | 40 | 93% (81–97) | 78 | 57% (48–65) |
| – High risk area | 21 | 22% (15–32) | – | – | – | – | 3 | 7% (3–19) | 24 | 17% (12–25) |
| – Unknown | 36 | 38% (29–48) | – | – | – | – | 0 | 0% (0–8) | 36 | 26% (19–34) |
| Development | ||||||||||
| – Symptomatic (anamnestic) | 93 | 99% (94–99) | 49 | 46% (37–56) | 28 | 46% (34–58) | 32 | 74% (60–85) | 125 | 91% (85–94) |
| – Length of symptoms (days) | 14 (9; 17) n = 91 |
8 (2; 8) n = 28 |
10 (3; 14) n = 23 |
8 (0; 11) n = 22 |
13 (8; 17) n = 113 |
|||||
| – In contact with general practitioner | 27 | 28% (21–38) | 0 | 0% (0–3) | 1 | 2% (0.4–9) | 1 | 2% (1–12) | 28 | 20% (14–28) |
| – Emergency room consultation | 15 | 16% (10–25) | 0 | 0% (0–3) | 0 | 0% (0–6) | 0 | 0% (0–8) | 15 | 11% (7–17) |
| – Hospitalisation | 13 | 14% (8–22) | 0 | 0% (0–3) | 1 | 2% (0.4–9) | 1 | 2% (1–12) | 15 | 11% (7–17) |
| – IMC or mechanical ventilation | 0 | 0% (0–4) | 0 | 0% (0–3) | 0 | 0% (0–6) | 1 | 2% (1–12) | 1 | 1% (0.2–4) |
| – Death | 1 | 1% (0.3–6) | 0 | 0% (0–3) | 0 | 0% (0–6) | 0 | 0% (0–8) | 1 | 1% (0.2–4) |
RT-PCR = real-time polymerase chain reaction; IQR = interquartile range; CI= confidence interval; FL= Fürstentum (Principality of) Liechtenstein; CH= Confederatio Helvetica (Switzerland); A= Austria; IMC= intermediate care unit * Diabetes (n = 2), hypertension (n = 8), cardiovascular disease (n = 8), cerebrovascular disease (n = 2), airway disease or pneumonia (n = 8), intestinal disease (n = 1), cancer (n = 3); 7 individuals had more than one preexisting condition. † Diabetes (n = 2), hypertension (n = 7), cardiovascular disease (n = 7), cerebrovascular disease (n = 2), airway disease or pneumonia (n = 3), intestinal disease (n = 0), cancer (n = 1); 4 individuals had more than one preexisting condition. ‡ Diabetes (n = 1), hypertension (n = 2), cardiovascular disease (n = 1), cerebrovascular disease (n = 0), airway disease or pneumonia (n = 3), intestinal disease (n = 0), cancer (n = 1); 1 individual had more than one preexisting condition. § Diabetes (n = 1), hypertension (n = 2), cardiovascular disease (n = 0), cerebrovascular disease (n = 0), airway disease or pneumonia (n = 0), intestinal disease (n = 0), cancer (n = 0); no individual had more than one preexisting condition. ¶ Diabetes (n = 3), hypertension (n = 10), cardiovascular disease (n = 8), cerebrovascular disease (n = 2), airway disease or pneumonia (n = 8), intestinal disease (n = 1), cancer (n = 3); 7 individuals had more than one preexisting condition
We compared the testing rates in the four German-speaking countries connected by the Alps in table 2 [34–37]. It can be seen that Liechtenstein’s testing rate was about 91% to 125% higher than those of the three other German-speaking countries. The test positivity rate per population was second to Switzerland, which had the highest incidences in its non-German-speaking cantons.
Table 2 Testing rates in four German-speaking countries as of 26 April 2020 [34–37].
| Country | Population | Tests | Positive tests | Tests per 1,000 inhabitants | Positive test rate in the population | Positive tests per total tests |
|---|---|---|---|---|---|---|
| Liechtenstein | 38,749 | 2172 | 95 | 56.1 | 0.245% | 4.4% |
| Switzerland | 8,060,600 | 256,075 | 34,026 | 31.7 | 0.422% | 13.4% |
| Germany | 83,166,700 | 2,446,644 | 174,549 | 29.4 | 0.209% | 7.1% |
| Austria | 8,901,064 | 221,544 | 15,175 | 24.9 | 0.171% | 6.9% |
With a total population of 38,749, the incidence of COVID-19 as observed until 23 April 2020 in the residential population of Liechtenstein (n = 82) was 211 cases per 100,000 population (0.211%). During this time, 2021 RT-PCR tests were performed in 1921 patients. The one case of death with COVID-19 gives a mortality rate of 2.58 per 100,000 population in the study period. Adjusting for the additional 31 cases identified by antibody testing and resident in Liechtenstein leads to an incidence of 292 cases per 100,000 population (0.292%).
Thirteen of the 95 RCP required hospitalisation (14%, 95% CI 8–22%). These 13 all needed supplemental oxygen, but none required mechanical ventilation or intensive care treatment. One patient, a multimorbid nursing home resident, died at age 94 fourteen days after her diagnosis with COVID-19. This corresponds to a national mortality rate of 1.1% (95% CI 0.3–5.7%) among the RCP and 0.7% (95% CI 0.2–3.9%) among all cases. The other RCP all completely recovered, and the average duration of symptoms was 14 days (IQR 9–17), with the 95th percentile having symptoms lasting 28 days.
The RCP showed significantly higher frequencies of clinical symptoms than the COVID-19 cases detected among the household and close workplace contacts (all symptoms are detailed in table 3; all had p<0.05 except throat pain, p = 0.08; vomiting, p = 0.29; and malaise, p = 0.45). In summary, the clinical presentation of the RCP was mild to moderate, but more severe than that of the household and close workplace contacts.
Table 3 Symptoms reported by RT-PCR- or antibody-positive cases. This table summarises the symptoms patients experienced during the course of their COVID-19 infections as well as the initial presenting symptoms (symptoms experienced on the first day of symptomatic disease).
| All reported symptoms | Presenting symptoms | |||
|---|---|---|---|---|
| n total = 138 | n | Percentage with 95% CI | n | Percentage with 95% Cl |
| Cough | 87 | 63% (55–70%) | 53 | 38% (31–47%) |
| Fever | 69 | 50% (42–58%) | 49 | 36% (28–44%) |
| Dysgeusia | 64 | 46% (38–55%) | 10 | 7% (4–13%) |
| Headache | 63 | 46% (38–54%) | 39 | 28% (21–36%) |
| Fatigue | 63 | 46% (38–54%) | 25 | 18% (13–25%) |
| Anosmia | 51 | 37% (29–45%) | 9 | 7% (4–12%) |
| Rheumatic pains | 46 | 33% (26–42%) | 26 | 19% (13–26%) |
| Rhinitis | 42 | 30% (23–39%) | 16 | 12% (7–18%) |
| Sore throat | 38 | 28% (21–36%) | 25 | 18% (13–25%) |
| Chest pain | 36 | 26% (19–34%) | 3 | 2% (1–6%) |
| Weight loss | 35 | 25% (19–33%) | – | – |
| Shivering | 31 | 22% (16–30%) | 18 | 13% (8–20%) |
| Dyspnoea | 29 | 21% (15–29%) | 4 | 3% (1–7%) |
| Diarrhoea | 29 | 21% (15–29%) | 14 | 10% (6–16%) |
| Generally feeling ill | 29 | 21% (15–29%) | 17 | 12% (8–19%) |
| Nausea | 15 | 11% (7–17%) | 3 | 2% (1–6%) |
| Vomiting | 5 | 4% (2–8%) | – | – |
| Other symptoms | 22* | 16% (11–23%) | 8† | 6% (3–11%) |
| Asymptomatic | 12 | 9% (5–15%) | – | – |
CI = confidence interval; RT-PCR = real-time polymerase chain reaction * Burning eye sensation (n = 6), sensitive skin (n = 4), vertigo (n = 4), back pain (n = 2), depression (n = 1), otalgia (n = 1), head pressure (n = 1), nosebleed (n = 1), sinusitis (n = 1), skin rash (n = 1) † Burning eye sensation (n = 4), sensitive skin (n = 1), vertigo (n = 1), back pain (n = 1), otalgia (n = 1)
Routine clinical chemistry and haematological parameters did not differ significantly between all COVID-19 cases (RCP, household and workplace contact cases [n = 129; four individuals had no values due to low sample volume obtained in capillary blood sampling; five individuals had no values due to non-availability for blood drawing for non-serological laboratory testing]) and non-diseased close contacts (n = 126, one individual without values due to low sample volume obtained in capillary blood sampling).
The frequencies of pre-existing chronic disease (3/43, 7%, 95% CI 3–19 vs 28/127, 22%, 95% CI 16–30%; p = 0.02) and nicotine consumption (2/43, 5%, 95% CI 1–15% vs 27/127, 22%, 95% CI 15-30%; p = 0.01) differed significantly between those close contacts with (n = 43) and without COVID-19 (n = 127). There were no significant differences in age (36, IQR 20–52 vs 41, IQR 26–53 years; p = 0.25) or gender (18/43, 42% female, 95% CI 28–57% vs 63/127, 50% female, 95% CI 41–58; p = 0.37) between the two groups. In summary, except for lower nicotine consumption and fewer pre-existing chronic conditions, neither demographic (age, gender) nor laboratory variables were associated with the occurrence of COVID-19 in close contacts of COVID-19 patients.
Of the 95 RCP, 38 (40%, 95% CI 31–50%) knew they had had contact with another confirmed COVID-19 case and a further 21 (22%, 95% CI 15–32%) contracted the disease in a high-risk region (e.g., ski resorts in Tyrolia, Northern Italy). Notably, in 36 cases (38%, 95% CI 29–48%) no source of infection could be identified. In the case of the 94-year-old nursing home resident, three staff members who had been in contact with this patient tested positive for COVID-19, but no other nursing home residents or institutionalised individuals were affected.
Household contacts were significantly more affected by infection than close workplace contacts (35/106, 32%, 95% CI 24–41% vs 8/61, 13%, 95% CI 7–24; p = 0.006). Only seven out of the 35 infected household contacts (20%, 95% CI 10–36%) had implemented isolation measures (e.g., physical distancing, hygienic measures) in response to the affected COVID-19 index cases. This frequency was significantly higher (55/74, 74%, 95% CI 63–83; p <0.001) in household contacts who did not contract COVID-19. In summary, no likely source for having contracted COVID-19 could be identified for a substantial proportion of the RCP. Furthermore, isolation measures in households had a protective effect against the transfer of COVID-19 to other household members.
This analysis characterises the first wave of the COVID-19 pandemic and its successful containment within 52 days after the occurrence of the first case in the Principality of Liechtenstein. Relevant public health measures were already in place or about to be implemented when the second case was diagnosed. Initially, these measures comprised mainly low-threshold access to testing and the close monitoring of confirmed cases. Further measures were implemented as the pandemic developed. The public health measures were mostly those of the Swiss Federal Office of Public Health, with some modifications. These measures can be considered relatively moderate, especially as there were no restrictions regarding residents’ freedom of movement outside of the home. This approach was in contrast to the lockdowns seen in Italy, Spain and France, who had much more restrictive regulations. The adherence of the population to the public health measures was high, with large civil movements and the Princely House of Liechtenstein supporting the work of the government and health professionals, especially by raising awareness and caring for high-risk groups. Masks were only required within healthcare and care home settings, which was less restrictive than the mask requirements in, e.g., Austria. Visits to healthcare facilities were prohibited, nonessential shops and restaurants were closed, and gatherings and meetings of more than five people were not allowed. We hypothesise that the key factor behind the containment of the pandemic in Liechtenstein was the high adherence of the population to the recommended measures.
The incidence in Liechtenstein on 23 April 2020 was 0.211%, higher than that of the canton of Zurich and 14 other Swiss cantons [38]. Approximately 14% of Liechtenstein’s COVID-19 patients had to be hospitalised, which is comparable to the respective number in Switzerland (12%). With no patients needing intensive care and a mortality rate of only 1% (compared to 4.4% in Switzerland), the course and outcomes of COVID-19 in Liechtenstein were very favourable. The major determinants of this favourable outcome were probably that the median age of the patients was 39 years and that seniors aged 65 and older accounted for only 13 patients, just 5 of whom were aged 80 years or older. On 23 April 2020, the median age of the COVID-19 patients in Switzerland was 52, substantially higher than that in Liechtenstein [38]. When looking at the 2018 national census numbers for Switzerland and for Liechtenstein, the median age of the general population for both countries is 42 years. Another possible determinant of the favourable outcome could be that the testing frequency in Liechtenstein was considerably higher than in Switzerland (0.81 vs 0.53 tests per 1000 inhabitants per day). Furthermore, although there was one COVID-19 case discovered in a nursing home, an epidemic spreading through nursing homes was effectively prevented, as no other nursing home residents were affected. Effective and early measures taken in nursing homes (i.e., masks, increased hygiene measures, prohibition of visits to nursing home residents, targeted testing of staff members in contact with the index patient) contributed to containing the pandemic and preventing further serious outcomes in high-risk individuals.
When investigating sources of COVID-19 infections, only approximately 60% of the patients could retrospectively provide a potential source. These investigations were performed conventionally by asking the patients and/or their relatives. The fact that 40% of the patients did not know by which route they had contracted the disease illustrates the insufficiency of the conventional tracking of infections. The first tracking app to replace conventional case tracking became available in Switzerland and Liechtenstein on 29 June 2020, much later than the end of the first wave [39]. It can be expected that electronic aids will be much more accurate than conventional case tracking, and the present data would support the widespread use of, e.g., tracking apps on smartphones [40, 41].
Serological antibody testing of household and close workplace contacts increased the number of identified COVID-19 cases by almost 50%. These cases were overlooked because the patients often did not fully develop clinical symptoms and therefore did not present themselves at testing sites. A quarter of the affected close contacts remained asymptomatic, a rate almost identical to that reported by Buitrago-Garcia et al. [42] During the course of the pandemic, the criteria for patients to undergo RT-PCR testing changed. Our data indicate that testing close contacts by RT-PCR in the appropriate time window and additional serology tests could be important procedures for the identification of COVID-19 cases, regardless of the presence of clinical symptoms [43–45]. Looking at the biochemical and haematological laboratory parameters, our study unfortunately did not provide any insights into what would protect individuals from contracting COVID-19 [46].
Thirty-two percent of the examined household contacts were infected with SARS-CoV-2, as opposed to 13% of the close workplace contacts. These numbers are comparable to those in a study done in Switzerland [47]. We believe that there are three reasons for this difference. First, individuals spend more time at home than at work, especially during times of widespread home office use, which was frequently the case during the COVID-19 pandemic. Second, individuals probably spend more time with and have more intimate relationships with their household members than with their workplace colleagues. Finally, employers had to implement safety measures guaranteeing social distancing and hygiene at work. Even though such measures were also proposed for private households, adherence in households is expected to be lower than in workplaces.
The household contacts without COVID-19 had a significantly higher frequency of implementing isolation measures in response to the RCP than those with COVID-19. This finding suggests that the isolation of COVID-19 patients from other household members within their homes is an effective preventive measure. When informed about the positive result of their RT-PCR test, patients were instructed to isolate themselves within their homes [32, 46]. However, it is the personal perception of the authors that the importance of these measures could be emphasised more in future information campaigns for the general public. Individual factors like the availability of separate rooms in an apartment for diseased cases should be assessed and taken into account when planning the implementation of effective isolation measures in homes. Since household contacts are an important source of new COVID-19 infections, the public health agenda should focus on explaining to both COVID-19 patients and the general population how to effectively implement preventive measures at home. Helping COVID-19 patients and their relatives to implement such measures is expected to decrease the transmission of the disease in households.
The present study has strengths and limitations. The population-based nature of the study is unique and represents a strength. As all cases in the country could be included at the patient level, no sampling bias was introduced by the selection of affected individuals. Another strength is that the patients could be completely followed up with clinical examinations, and 95% were available for follow-up laboratory exams. The study has a relatively low absolute case number, however, which results in large confidence intervals for the different estimates of frequencies. Furthermore, Liechtenstein’s population is predominantly of Caucasian origin. The extrapolation of our findings to other settings might therefore be limited. Furthermore, although the country made the largest possible efforts to identify all cases through contact tracing and antibody testing, it is probable that not all COVID-19 cases of the first wave were detected. The described incidence can therefore be considered an underestimate. Another population-based study, performed in June 2020 using randomly selected residents and periodic surveillance testing in healthcare workers, however, showed a very low incidence in both the general population and in the healthcare workers, a population at risk of contracting COVID-19 (data not shown). The underestimation thus cannot be considered large. Nevertheless, we provide evidence for current or potential improvements to public health measures (i.e., antibody testing of household contacts, contact tracing, quarantining of household contacts and installation of preventive measures at work and at home). We therefore think that these limitations do not invalidate our findings.
In conclusion, we can report that a close, rapid and dedicated collaboration of all relevant stakeholders in a small country allowed for the complete workup of all the COVID-19 patients nationwide. A multitude of factors (e.g., the young age of the affected patients, low-threshold access to testing, the close monitoring of cases, high alertness and the adherence of the population to public health measures) led to the early containment of the pandemic, with a very low rate of serious outcomes. Finally, our work suggests that several measures can or potentially could improve the containment of COVID-19. These measures include the laboratory testing of household contacts to identify additional cases not presenting to healthcare services, extensive contact tracing to improve the early recognition of potentially high-risk situations for contracting COVID-19, the isolation of COVID-19 patients within their household and the installation of preventive measures to reduce the spread of infection in both home and workplace settings.
The authors would like to express their gratitude to the many motivated persons involved in making this study possible. Thanks to the staff of the Landesspital Liechtenstein for their great work during the pandemic and especially for their support and flexibility during the follow-up phase of this study. Thanks to the Liechtensteinische Ärztekammer for running the central drive-through testing facility in Vaduz with their dedicated team. Thanks to the team at the labormedizinisches zentrum Dr Risch for making the test procedures available from the very early phase of the pandemic. Thanks to Dr Silvia Dehler, MD MPH for critically proofreading our manuscript and for her very helpful discussion with us. Last but not least, we were overwhelmed by the great willingness of the COVID-19 patients and their close contacts to contribute to science. Their support and cooperation ultimately allowed us to combat the pandemic with greater effectiveness. Thank you.
This study was funded by the Liechtenstein Ministry of Health.
The authors declare that there are no conflicts of interest regarding the publication of this paper.
1 Wu F , Zhao S , Yu B , Chen Y-M , Wang W , Song Z-G , et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–9. doi:.https://doi.org/10.1038/s41586-020-2008-3
2 Huang C , Wang Y , Li X , Ren L , Zhao J , Hu Y , et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:.https://doi.org/10.1016/S0140-6736(20)30183-5
3 Gautier J-F , Ravussin Y . A New Symptom of COVID-19: Loss of Taste and Smell. Obesity (Silver Spring). 2020;28(5):848. doi:.https://doi.org/10.1002/oby.22809
4 Lechien JR , Chiesa-Estomba CM , De Siati DR , Horoi M , Le Bon SD , Rodriguez A , et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. 2020;277(8):2251–61. doi:.https://doi.org/10.1007/s00405-020-05965-1
5Der Bundesrat. Neue Hygiene- und Verhaltensregeln zum Schutz gegen das neue Coronavirus. [accessed 2020 Jun 30]. Available from: https://www.admin.ch/gov/de/start/dokumentation/medienmitteilungen.msg-id-78304.html
6 Lemaitre JC , Perez-Saez J , Azman AS , Rinaldo A , Fellay J . Assessing the impact of non-pharmaceutical interventions on SARS-CoV-2 transmission in Switzerland. Swiss Med Wkly. 2020;150:w20295.
7Der Bundesrat. Coronavirus: Bundesrat verbietet Ansammlungen von mehr als fünf Personen. [accessed 2020 Jun 30]. Available from: https://www.admin.ch/gov/de/start/dokumentation/medienmitteilungen.msg-id-78513.html
8Der Bundesrat. Verordnung 2 über Massnahmen zur Bekämpfung des Coronavirus. (COVID-19). [accessed 2020 Jun 30]. Available from: https://www.admin.ch/opc/de/classified-compilation/20200744/index.html
9 Chinazzi M , Davis JT , Ajelli M , Gioannini C , Litvinova M , Merler S , et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. doi:.https://doi.org/10.1126/science.aba9757
10 Rodríguez-Morales AJ , MacGregor K , Kanagarajah S , Patel D , Schlagenhauf P . Going global - Travel and the 2019 novel coronavirus. Travel Med Infect Dis. 2020;33:101578. doi:.https://doi.org/10.1016/j.tmaid.2020.101578
11 Wells CR , Sah P , Moghadas SM , Pandey A , Shoukat A , Wang Y , et al. Impact of international travel and border control measures on the global spread of the novel 2019 coronavirus outbreak. Proc Natl Acad Sci USA. 2020;117(13):7504–9. doi:.https://doi.org/10.1073/pnas.2002616117
12Bundesamt für Gesundheit. Neuartiges Coronavirus (COVID-19) Verdachts-, Beprobungs- und Meldekriterien 26.2.2020. [accessed 2020 Jun 30]. Available from: https://www.bag.admin.ch/bag/de/home/krankheiten/infektionskrankheiten-bekaempfen/meldesysteme-infektionskrankheiten/meldepflichtige-ik/meldeformulare.html
13Amt für Statistik Fürstentum Liechtenstein. Bevölkerungsstatistik vorläufige Ergebnisse 31. Dezember 2019. [accessed 2020 Jun 30] Available from: https://www.llv.li/files/as/bevolkerungsstatistik-vorlaufige-ergebnisse-31-dezember-2019.pdf
14Amt für Statistik Fürstentum Liechtenstein. Beschäftigungsstatistik 2018. [accessed 2020 Jun 30] Available from: https://www.llv.li/files/as/beschaftigungsstatistik-2018.pdf
15Schiess P. Der Zollvertrag und die Massnahmen zur Bekämpfung des Coronavirus. Wie Schweizer Recht via Zollanschlussvertrag und Epidemiengesetz in Liechtenstein Anwendung findet. Bendern (Arbeitspapiere Liechtenstein-Institut, 65). [accessed 2020 Jun 26]. Available from: https://www.liechtenstein-institut.li/publikationen/schiess-ruetimann-patricia-m-2020-der-zollvertrag-und-die-massnahmen-zur-bekaempfung-des-coronavirus
16Regierung des Fürstentum Liechtenstein. Medienmitteilung 16.3.2020: Regierung verschärft Massnahmen zur Verlangsamung der Ausbreitung des Corona-Virus. [accessed 2020 Jun 26]. Available from: https://www.regierung.li/coronavirus/2020-3
17Regierung des Fürstentum Liechtenstein. Medienmitteilung 17.3.2020: Generelles Veranstaltungsverbot und weitere Schliessungen. [accessed 2020 Jun 26]. Available from: https://www.regierung.li/coronavirus/2020-3
18 Mizumoto K , Kagaya K , Zarebski A , Chowell G . Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25(10):2000180. doi:.https://doi.org/10.2807/1560-7917.ES.2020.25.10.2000180
19Regierung des Fürstentum Liechtenstein. Medienmitteilung 26.2.2020: Liechtenstein ist auf Coronavirus vorbereitet. [accessed 2020 Jun 26]. Available from: https://www.regierung.li/media/attachments/80-coronavirus.pdf?t=637293305811334665
20Regierung des Fürstentum Liechtenstein. Medienmitteilung 30.03.2020: - Drive-Through Anlage in Betrieb genommen. Regierung Liechtenstein. [accessed 2020 Jun 26]. Available from: https://www.regierung.li/coronavirus/2020-3
21Regierung des Fürstentum Liechtenstein. Medienmitteilung 11.03.2020: Besuchsverbot in Pflegeheimen. [accessed 2020 Jun 26]. Available from: https://www.regierung.li/coronavirus/2020-3
22Regierung des Fürstentum Liechtenstein. Medienmitteilung 11.02.2020: Regierung setzt Stab „neues Coronavirus 2019‐nCoV“ ein. [accessed 2020 Jun 26]. Available from: https://www.regierung.li/media/attachments/57-stab-coronavirus.pdf?t=637275754464486760
23Liechtensteinisches Vaterland. Liemobil reduziert Fahrplan-Angebot. [accessed 2020 March 18]. Available from: https://www.vaterland.li/liechtenstein/vermischtes/liemobil-reduziert-angebot;art171,414347
24Bundesamt für Gesundheit. Neuartiges Coronavirus (COVID-19) Verdachts-, Beprobungs- und Meldekriterien 20.03.2020. [accessed 2020 Jun 26]. Available from: https://www.bag.admin.ch/bag/de/home/krankheiten/infektionskrankheiten-bekaempfen/meldesysteme-infektionskrankheiten/meldepflichtige-ik/meldeformulare.html
25Amt für Gesundheit Fürstentum Liechtenstein. Anweisung zu Selbstisolation. [accessed 2020 June 26]. Available from: https://www.llv.li/files/ag/anweisung-selbst-isol-_200401.pdf
26Regierung des Fürstentum Liechtenstein. Medienmitteilung 17.04.2020: Regierung orientiert über das weitere Vorgehen in Zusammenhang mit dem Coronavirus. [accessed 2020 Jun 26]. Available from: https://www.regierung.li/coronavirus/2020-4
27Regierung Liechtenstein. Medienmitteilung 27.04.2020 - erste Massnahmen Lockerung [Internet]. Regierung Liechtenstein. 2020. [cited 2020 Sep 6] Available from: https://www.regierung.li/media/attachments/212-corona-massnahmen-und-wirtschaft.pdf?t=637350190453776117
28Regierung Liechtenstein. Medienmitteilung 30.04.2020 - weitere Lockerung [Internet]. Regierung Liechtenstein. 2020. Available from: https://www.regierung.li/media/attachments/229-corona-massnahmen-0430.pdf?t=637350190453776117
29Regierung Liechtenstein. Medienmitteilung 29.05.2020 - Start in eine neue Normalität [Internet]. Regierung Liechtenstein. 2020. [cited 2020 Sep 6] Available from: https://www.regierung.li/media/attachments/293-corona-neue-normalitaet-0529.pdf?t=637350196817652922
30Regierung Liechtenstein. Medienmitteilung 24.06.2020 - Weitgehende Rückkehr zur Normalität [Internet]. Regierung Liechtenstein. 2020 [cited 2020 Sep 6]. Available from: https://www.regierung.li/media/attachments/351-corona-rueckkehr-normalitaet-0624.pdf?t=637350195227330034
31Regierung Liechtenstein. Medienmitteilung 29.06.2020 - Contact tracing [Internet]. Regierung Liechtenstein. 2020. [cited 2020 Sep 6] Available from: https://www.regierung.li/media/attachments/362-swiss-covid-app.pdf?t=637350198384900256
32Liechtensteiner Vaterland. «Es ist noch zu früh für eine Entwarnung». [accessed 2020 April 15]. Available from: https://www.vaterland.li/liechtenstein/vermischtes/es-ist-noch-zu-frueh-fuer-eine-entwarnung;art171,416324
33 Baron RC , Risch L , Weber M , Thiel S , Grossmann K , Wohlwend N , et al. Frequency of serological non-responders and false-negative RT-PCR results in SARS-CoV-2 testing: a population-based study. Clin Chem Lab Med. 2020: Epub ahead of print. doi:.https://doi.org/10.1515/cclm-2020-0978
34Eidgenössisches Bundesamt für Gesundheit. COVID-19 in der Schweiz, Anzahl Tests. [accessed 2020 September 3]. Available from: https://covid-19-schweiz.bagapps.ch/de-3.html
35 Robert Koch Institut. Erfassung der SARS-CoV-2-Testzahlen in Deutschland (Stand 19.8.2020). Epidemiologisches Bulletin. 2020;34:1–2.
36Österreichisches Bundesministerium Soziales, Gesundheit, Pflege und Konsumentenschutz. Coronavirus, Aktuelle Informationen. [accessed 2020 September 3]. Available from: https://www.sozialministerium.at/Informationen-zum-Coronavirus/Neuartiges-Coronavirus-(2019-nCov).html
37Der Standard. Aktuelle Zahlen zum Coronavirus. [accessed 2020 September 3]. Available from: https://www.derstandard.at/story/2000115810293/aktuelle-zahlen-zum-coronavirus
38Bundesamt für Gesundheit (BAG). Coronavirus Krankheit 2019 (COVID-19) Situationsbericht zur epidemiologischen Lage in der Schweiz und im Fürstentum Liechtenstein.
39Regierung des Fürstentum Liechtenstein. MEDIENMITTEILUNG Nr 362. [accessed 2020 June 29]. Available from: https://www.regierung.li/media/attachments/362-swiss-covid-app.pdf?t=637332946010225297
40 Salathé M , Althaus CL , Neher R , Stringhini S , Hodcroft E , Fellay J , et al. COVID-19 epidemic in Switzerland: on the importance of testing, contact tracing and isolation. Swiss Med Wkly. 2020;150:w20225. doi:.https://doi.org/10.4414/smw.2020.20225
41 Bicher MR , Rippinger C , Urach C , Brunmeir D , Siebert U , Popper N . Agent-Based Simulation for Evaluation of Contact-Tracing Policies Against the Spread of SARS-CoV-2. medRxiv. 2020:2020.2005.2012.20098970.
42 Buitrago-Garcia DC , Egli-Gany D , Counotte MJ , et al. The role of asymptomatic SARS-CoV-2 infections: rapid living systematic review and meta-analysis. medRxiv 2020:2020.2004.2025.20079103.
43 Ellinghaus D , Degenhardt F , Bujanda L , Buti M , Albillos A , Invernizzi P , et al.; Severe Covid-19 GWAS Group. Genomewide Association Study of Severe Covid-19 with Respiratory Failure. N Engl J Med. 2020;NEJMoa2020283. doi:.https://doi.org/10.1056/NEJMoa2020283
44 Long Q-X , Liu B-Z , Deng H-J , Wu G-C , Deng K , Chen Y-K , et al. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat Med. 2020;26(6):845–8. doi:.https://doi.org/10.1038/s41591-020-0897-1
45 Kucirka LM , Lauer SA , Laeyendecker O , Boon D , Lessler J . Variation in False-Negative Rate of Reverse Transcriptase Polymerase Chain Reaction-Based SARS-CoV-2 Tests by Time Since Exposure. Ann Intern Med. 2020;173(4):262–7. doi:.https://doi.org/10.7326/M20-1495
46 Hella J , Cercamondi CI , Mhimbira F , Sasamalo M , Stoffel N , Zwahlen M , et al. Anemia in tuberculosis cases and household controls from Tanzania: Contribution of disease, coinfections, and the role of hepcidin. PLoS One. 2018;13(4):e0195985. doi:.https://doi.org/10.1371/journal.pone.0195985
47 Stringhini S , Wisniak A , Piumatti G , Azman AS , Lauer SA , Baysson H , et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study. Lancet. 2020;396(10247):313–9. doi:.https://doi.org/10.1016/S0140-6736(20)31304-0
Contributed equally
This study was funded by the Liechtenstein Ministry of Health.
The authors declare that there are no conflicts of interest regarding the publication of this paper.