Healthcare professionals’ opinions on psychological screening in follow-up care for childhood cancer survivors
DOI: https://doi.org/10.4414/smw.2020.20356
Erika
Harjua, Manya Jerina
Hendriksab, Katharina
Rosera, Gisela
Michela
aDepartment of Health Sciences and Medicine,
bDepartment of Neonatology,
Healthcare professionals’ opinions on psychological screening in follow-up care for childhood cancer survivors
Summary
INTRODUCTION
Implementation of screening for psychological distress in populations at risk, as recommended in existing guidelines, can be challenging on different levels: structural, organisational and personal (provider and patient). A specific group at risk for psychological distress, including anxiety and depression, is the growing population of childhood cancer survivors (CCS). In many countries, including Switzerland, the standardised assessment of psychological late effects during follow-up care is not yet established. The emotion thermometer, a short and validated assessment tool to screen for psychological distress, might facilitate implementation of psychological screening in Swiss CCS follow-up care.
AIMS OF THE STUDY
To inform implementation strategy and assess readiness of centres to integrate standardised psychological screening, we conducted a cross-sectional survey. We describe healthcare professionals’ opinions on (i) the current standard of psychological screening in follow-up care, (ii) their experience using the emotion thermometer, and (iii) perceived barriers and facilitators of possible implementation of psychological screening, including the emotion thermometer.
METHODS
We contacted 49 healthcare professionals involved in CCS follow-up care in all nine paediatric oncology clinics in Switzerland. The electronic survey included closed and open questions.
RESULTS
A majority of the healthcare professionals (17/24, 71%) stated that assessment of psychological distress is currently not standard in follow-up care. On the contrary, about half of them (11/24, 46%) think that psychological distress is adequately assessed in follow-up care. None of the participants had any previous experience with the emotion thermometer. After being informed about the emotion thermometer, nearly 80% (19/24) agree that it appears to be a good screening instrument and support the idea of regular application during follow-up care. Facilitators of implementation included the instrument’s brevity, its ability to visualise psychological topics and raising awareness of the need to think about the psychological side of follow-up care. Barriers included lack of time, the additional effort and the perception that instead an informal assessment would be sufficient. Concerns about using an artificial assessment, rather than a natural conversation, were also expressed.
CONCLUSIONS
There is overall agreement that screening for psychological late effects is not yet standard in follow-up care in Switzerland. It is important to mitigate perceived barriers and concerns of healthcare professionals to enable a successful implementation of psychological distress screening according to the established standards of care.
Introduction
Continuous medical advances in diagnosis and treatment of childhood malignancies have resulted in international survival rates exceeding 80% [1]. This growing population of childhood cancer survivors (CCS) is at risk for psychological late effects, including distress [2, 3], depression [4, 5] and post-traumatic stress [6, 7]. Even long into survivorship, risk for distress [8, 9] and persistent emotional problems remain high [10]. Heightened distress has been associated with poor adherence to treatment recommendations [11], unmet needs in health care [12] and worse quality of life [13, 14]. Studies among long-term CCS suggest that psychological distress may be underdiagnosed and undertreated [8, 9, 15]. Left untreated, debilitating consequences may occur [16]. Consequently, there is need for psychological screening and support along the survivorship trajectory.
CCS are advised to attend life-long follow-up care [17] where their physical status is systematically monitored for cancer recurrence, second malignancies and late complications [18]. In Switzerland, around 180 CCS transition from treatment to follow-up care yearly [19, 20]. Regular follow-up care has been available for survivors up to 10 years after end of treatment in the nine paediatric oncology centres. Recently, follow-up care for long-term survivors (including adult survivors of childhood cancer) has been established in various centres, four of which have already set up an interdisciplinary follow-up clinic. Additionally, a separate specialised outpatient clinic offers long-term follow-up care to adult CCS. Standards and guidelines for optimal psychosocial care of cancer patients and survivors [21–25] highlight the significance of psychosocial surveillance and recommend implementing standardised screening for psychological distress [23, 25].
To help identify distress, psychological screening instruments have been developed, including in paediatric age groups [26, 27]. One example is the emotion thermometer, a validated and reliable instrument for distress screening in time-constrained clinical settings that seems promising for implementation in CCS follow-up care as a result of all reported positive qualities [28–31].
Unfortunately, in most countries, including Switzerland, implementation of these recommendations in CCS follow-up care is lacking and standardised assessment of psychological late effects, irrespective of the instrument, is not yet established [32, 33]. To date, few studies have explored the reasons behind this implementation paucity from the perspective of the healthcare professionals involved [33–36]. Perceived barriers can be attributed to challenges in healthcare delivery, specifically, the structure of healthcare systems and organisational characteristics of work places, including limited human resources, time constraints and restricted financing possibilities [32, 34, 36, 37]. Additional barriers to implementation can be ascribed to the personal characteristics and perspectives of the healthcare professionals involved. With respect to provider-level attributes, studies have described low confidence of healthcare professionals, low acceptability of psychological screening and/or instruments, and lack of training and support for an in-depth psychological evaluation [34–37].
The combination of established standards, available instruments and the risk for psychological late effects, makes the absence of systematic screening in these survivors concerning. The main aim of the study was therefore to investigate the perspectives of healthcare professionals directly involved in CCS follow-up care and identify possible barriers and facilitators towards implementation. . We describe (i) healthcare professionals’ opinions on the current standard of psychological screening in follow-up care, (ii) their experience using the emotion thermometer, and (iii) perceived barriers to and facilitators of possible implementation. This study contributes to the assessment of readiness of healthcare professionals for the integration of psychological screening in CCS follow-up care and inform implementation.
Materials and methods
We conducted a cross-sectional electronic survey among healthcare professionals involved in follow-up care of CCS in the nine paediatric oncology clinics in Switzerland. We included both closed questions and one open question to assess information about and experiences with screening practices, and perceived barriers to and facilitators of possible implementation. This manuscript adheres to the ‘Strengthening the Reporting of Observational Studies in Epidemiology’ (STROBE) reporting guidelines [38].
Compliance with ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethics approval has been granted by the Ethics Commission Nordwest- und Zentralschweiz (EKNZ 2017-01740).
Sample and procedure
All healthcare professionals who were employed in one of the nine paediatric oncology clinics and directly involved in follow-up care (oncologists, nurses, psychologists, medical assistants or other) were eligible and invited to participate. First, members of the Swiss Paediatric Oncology Group (SPOG) were informed about the study during their annual meeting and indicated their willingness to participate. Then contact information of the eligible healthcare professionals was provided by the SPOG coordination centre. Eligible individuals received an e-mail including study information and an open link to the electronic survey in German. A version translated into either of the other Swiss languages (French and Italian) or a paper version of the survey was available upon request. A reminder to participate was sent after 2 weeks. Data collection took place from January to March 2018.
Measurements
We developed an electronic survey using SoSciSurvey (Data Management and Survey Tool, www.SoSciSurvey.de) [39], a free, secure, web-based application designed to support data collection for research studies. The survey was designed and questions developed by EH. The final version was agreed upon and tested within GM’s research team by four other researchers. With this 15-item survey we collected both quantitative (closed questions and Likert scales) and qualitative (one open question assessing personal opinions and experiences) information.
We assessed sociodemographic information on the participants (sex, age at time of the study, profession, work place and involvement in follow-up care).
Information on involvement in follow-up care was assessed by duration of involvement in CCS follow-up care (“little experience”, “<1 year” or “≥1year”). We briefly presented information on the emotion thermometer in the survey. The emotion thermometer was designed in 2007 to expand on its predecessor, the distress thermometer (National Comprehensive Cancer Network [NCCN]) [23, 30, 40]. The emotion thermometer is a short self-report tool that consists of five domains: four emotion domains (distress, DT; anxiety, AnxT; depression, DepT; and anger, AngT) and one outcome domain (need for help, HelpT) in visual-analogue format (thermometers) ranging from 0 to 10 [30, 40]. The cut-off threshold for distress is ≥4 [30]. Higher scores should be addressed by the clinician and if necessary followed by a careful clinical assessment [41]. The tool is easy to understand for most patients, including older people and children [41].
To assess the perception of current standard of psychological screening practice in follow-up care, participants answered to the statements “Psychological late effects of CCS are sufficiently assessed in follow-up care, even without the emotion thermometer” and “Assessment of psychological late effects of CCS in follow-up care is already standard”, using a four-point Likert scale (1 “strongly disagree”, 2 “disagree“, 3 “agree”, 4 “strongly agree”). Participants were asked about their experience of using the emotion thermometer in follow-up care, using the same four-point Likert scale, in four statements, “I was surprised about the scores the CCS reported through the emotion thermometer”, “The CCS’ reports on the emotion thermometer had an influence on the follow-up appointment”, “The emotion thermometer made it easier for me to ask the relevant questions during the follow-up appointment”, and “The emotion thermometer helped me in finding points that needed intervention, that I would otherwise not have found.”
Finally, to assess opinions on the potential implementation of the emotion thermometer, participants answered to the statements “The emotion thermometer seems to be a good instrument to assess psychological late effects”, “It is a good idea to fill in the emotion thermometer regularly before follow-up care” and “The emotion thermometer is able to quickly detect possible difficulties of CCS” using the same four-point Likert scale. Participants were additionally asked one open question to assess positive or negative aspects of the emotion thermometer.
Data analyses
Statistical analyses were performed with STATA version 15.1 (StataCorp, College Station, TX, USA). To describe the study population, we used descriptive statistics. Additionally, we used non-parametric Fisher’s exact tests for small samples. All responses were either: 2 “disagree” or 3 “agree”, apart from two responses, such that we dichotomised answers into disagreement (1 and 2) / agreement (3 and 4). Fisher’s exact tests were used to test for associations between healthcare professionals’ sociodemographic characteristics and their opinions about the current standard of psychological screening practice in follow-up care.
An inductive thematic analysis guided by Braun and Clarke’s approach [42] was used for the answers to the open question on perceived positive and negative aspects of the emotion thermometer using ATLAS.ti 8. Two researchers (EH and MJH) with experience in qualitative health research analysed the qualitative data. First, initial codes were generated through systematic coding by the first author (EH). After the first coding (EH), a second reviewer (MJH) confirmed its reliability independently. Second, identified codes were reviewed and collated into overarching themes. Finally, themes were reviewed by both coders (EH and MJH) until consensus was reached. Several strategies were used to ensure accuracy in the data analysis. Credibility was complemented by peer debriefing among the coders. All coding was cross-checked and completed by the second coder. Discrepancies were resolved through repeated discussion. Representative quotes were selected and presented in text. To ensure accuracy and quality of participants’ quotes, back-to-back translation was performed [43].
Results
Participants
In total, we contacted 49 (100%) eligible healthcare professionals involved in follow-up care in the paediatric oncology clinics. Of those contacted, we received one active refusal. The survey was accessed by 41 healthcare professionals, of whom 34 partially filled out the survey. Incomplete surveys, such as those where outcome-relevant questions were not completed, were excluded. Finally, 24 healthcare professionals from seven of the nine paediatric oncology clinics were included in the analyses (49% response rate; 17 [71%] female; table 1). Mean age at the time of the study was 41 years (standard deviation 8.6, range 24–55). In total, the 24 participating healthcare professionals self-reported their professional status as 11 paediatric oncologists, 11 nurses, including one expert nurse in paediatric oncology, (each 46%), and two physician researchers (referred to as scientists) involved in paediatric oncology (8%). Most participants had more than 1 year of experience in follow-up care (17/24, 71%). The majority was employed in the German-speaking part of Switzerland (18/24, 75%). There were no significant differences in the distribution of professions with regard to sex and geographical location of workplace. Paediatric oncologists were older (p <0.001), and involvement in follow-up care differed between the professions with all paediatric oncologists having more than 1 year of experience (p = 0.017).
Table 1 Characteristics of participants working in follow-up care of childhood cancer survivors: by profession.
| |
Total
(n = 24)
|
Oncologists
(n = 11)
|
Nurses
(n = 11)
|
Scientists
(n = 2)
|
p-value*
|
|
Mean
|
Range
|
Mean
|
Range
|
Mean
|
Range
|
Mean
|
Range
|
| Age at study (years) |
41.00 |
24–55 |
47.00 |
40–55 |
34.00 |
24–41 |
48.00 |
40–55 |
<0.001
|
| |
n
|
%
|
n
|
%
|
n
|
%
|
n
|
%
|
|
| – <40 years |
9 |
37 |
0 |
0 |
9 |
82 |
0 |
0 |
|
| – ≥40 years |
15 |
63 |
11 |
100 |
2 |
18 |
2 |
100 |
| Sex |
|
|
|
|
|
|
|
|
0.171 |
| – Male |
7 |
29 |
5 |
45 |
1 |
9 |
1 |
50 |
| – Female |
17 |
71 |
6 |
55 |
10 |
91 |
1 |
50 |
| Language part of Switzerland |
|
|
|
|
|
|
|
|
0.306 |
| – German |
18 |
75 |
6 |
55 |
10 |
91 |
2 |
100 |
| – French and Italian |
3 |
12.5 |
3 |
27 |
0 |
0 |
0 |
0 |
| – Unknown |
3 |
12.5 |
2 |
18 |
1 |
9 |
0 |
0 |
| Involvement in follow-up care |
|
|
|
|
|
|
|
|
0.017
|
| – Little experience |
6 |
25 |
0 |
0 |
5 |
45 |
1 |
50 |
| – <1 year |
1 |
4 |
0 |
0 |
1 |
10 |
0 |
0 |
| – ≥1 year |
17 |
71 |
11 |
100 |
5 |
45 |
1 |
50 |
Current standard of psychological screening practice in follow-up care
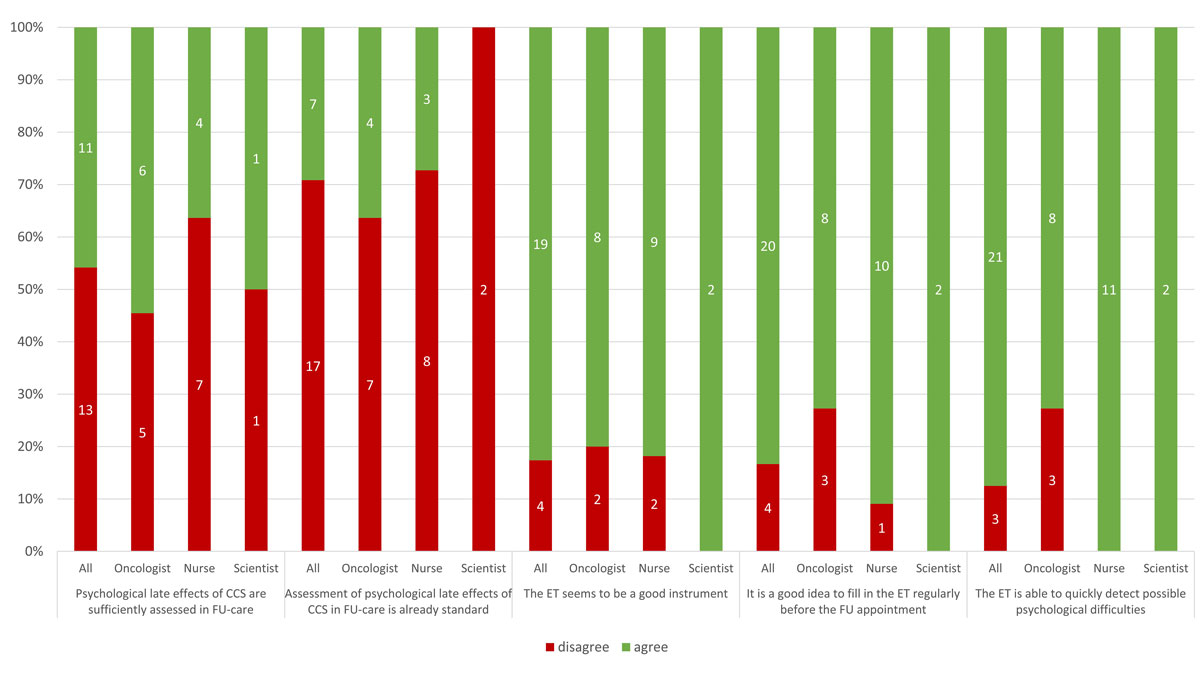
About half of the healthcare professionals (13/24, 54%) disagreed that psychological late effects are adequately assessed in follow-up care, with slightly more nurses than oncologists disagreeing (7/11, 64% vs 5/11, 45%) (fig. 1).
With regard to the statement whether screening for psychological late effects was standard in CCS follow-up care, more than two thirds disagreed (71%). Half (n = 3) of the paediatric oncologists who had agreed (n = 6) with the statement that psychological late effects are adequately assessed, disagreed that screening for psychological late effects was standard. None of the sociodemographic characteristics including sex, age at the time of the study, profession, work place or involvement in follow-up care was associated with the two outcomes on the current standard of psychological screening practice in follow-up care (table 2).
Table 2 Characteristics associated with opinions on the current standard of psychological screening practice in follow-up care.
| |
Total (%)
|
Psychological late effects are sufficiently assessed in follow-up care
|
Assessment of psychological late-effects in follow-up care is already standard
|
|
Agreement
|
Disagreement
|
p-value*
|
Agreement
|
Disagreement
|
p-value*
|
|
n (%)
|
n (%)
|
n (%)
|
n (%)
|
n (%)
|
| Sex |
|
|
|
0.386 |
|
|
0.374 |
| – Male |
7 (29) |
2 (18) |
5 (38) |
3 (43) |
4 (24) |
| – Female |
17 (71) |
9 (82) |
8 (62) |
4 (57) |
13 (76) |
| Age at study |
|
|
|
1.000 |
|
|
1.000 |
| – <40 years |
9 (38) |
4 (36) |
5 (38) |
3 (43) |
6 (35) |
| – ≥40 years |
15 (62) |
7 (64) |
8 (62) |
4 (57) |
11 (65) |
| Profession |
|
|
|
0.829 |
|
|
1.000 |
| – Oncologists |
11 (46) |
6 (55) |
5 (38) |
4 (57) |
7 (41) |
| – Nurses |
11 (46) |
4 (36) |
7 (54) |
3 (43) |
8 (47) |
| – Scientists |
2 (8) |
1 (9) |
1 (8) |
|
0 (0) |
2 (12) |
| Language part of Switzerland |
|
|
|
0.825 |
|
|
1.000 |
| – German |
18 (74) |
8 (73) |
10 (77) |
5 (72) |
13 (76) |
| – French and Italian |
3 (13) |
1 (9) |
2 (15) |
1 (14) |
2 (12) |
| – Unknown |
3 (13) |
2 (18) |
1 (8) |
|
1 (14) |
2 (12) |
| Involvement in follow-up care |
|
|
|
1.000 |
|
|
1.000 |
| – Little experience |
6 (25) |
3 (27) |
3 (23) |
2 (29) |
4 (24) |
| – <1 year |
1 (4) |
0 (0) |
1 (8) |
0 (0) |
1 (6) |
| – ≥1 year |
17 (71) |
8 (73) |
9 (70) |
5 (71) |
12 (71) |
Healthcare professionals experiences with the emotion thermometer
None of the healthcare professionals reported having experience with the emotion thermometer. However, most agreed that it seemed to be a good instrument to assess psychological late effects (19/24, 79%) and able to quickly detect possible psychological difficulties in CCS (21/24, 88%). A majority of healthcare professionals also approved of the idea of survivors filling in the emotion thermometer regularly before follow-up appointments (20/24, 83%) (fig. 1).
Perceived positive or negative perspectives of using the emotion thermometer
Overall, positive or negative aspects of emotion thermometer could be ascribed to the level of either organisational characteristics of work places, personal characteristics of involved individuals, or instrument-specific attributes. In addition, our analysis of the open question identified both barriers and facilitators to the implementation of emotion thermometer (example quotes are presented below).
Positive perspectives
Organisational facilitators: At the organisational level the emotion thermometer can function as a facilitator for “raising awareness to think about the psychological side of follow-up care” and some healthcare professionals considered the emotion thermometer could be “helpful to deliberately ask” about psychological topics. Efficiency, due to the emotion thermometer’s brevity, was also mentioned as a facilitator at the organisational level.
Instrument-specific strengths: Healthcare professionals consistently mentioned positive instrument-specific attributes. Many pointed out that the emotion thermometer helps “visualise psychological topics and express feelings.” They described the instrument as “easy to use, quick and efficient.” Participants stated that the emotion thermometer can “serve as a door opener” and “starting point for conversations” in the follow-up appointment because it “records the emotional side.” This results in information that the “doctor can later pick up on” and “those affected can take a position.” Healthcare professionals furthermore perceived that using the emotion thermometer “helps to address CCS’ emotions” and gives “a quick overview of possible problems.”
Negative perspectives
Organisational barriers: A majority of healthcare professionals stated the issue that “plenty of assessment instruments already exist” and the emotion thermometer would be “an additional scale.” This was then also perceived as an “additional expenditure.” With regard to the everyday life in the clinic, “lack of time” was experienced as a barrier “to thoroughly address needs and psychological topics.” Participants also mentioned that using the emotion thermometer could “raise expectations in patients” that could “not be fulfilled in the time constrained clinical setting.”
Personal characteristics: Healthcare professionals expressed personal concerns about using the emotion thermometer because it seemed “a bit artificial” and they would “prefer a more natural conversation when asking about psychosocial aspects.” In fact, they counter-argued that they were “already asking specific questions on psychological topics in follow-up care.” A related issue was that it would “not replace the further clinical assessment” as it was perceived as “too superficial.” Inconsistent with the statement that the emotion thermometer was too superficial, healthcare professionals also perceived that the emotion thermometer contains “too personal questions.”
Instrument-specific limitations: Although healthcare professionals agreed on the many instrument-specific strengths, they also found that the emotion thermometer was “not suitable for all age groups”, specifically “not for small children” since those would “not be able to assess their emotions with the emotion thermometer.” Furthermore, they perceived the emotion thermometer as “not able to capture the complexity of psychological problems” and “too superficial if used as an exclusive instrument.”
Discussion
This study describes the opinions of healthcare professionals involved in CCS follow-up care on the current standard of psychological screening practice and their experience and perception of using the emotion thermometer. The majority of healthcare professionals agreed that assessment of psychological distress is currently not standard in follow-up care. Contrarily, around half of healthcare professionals agreed with the statement that psychological distress is sufficiently assessed in follow-up care. This discrepancy in opinions indicates existing inconsistencies in the delivery of follow-up care in Switzerland [32]. Inconsistencies in the use of guidelines across the Swiss paediatric oncology clinics have recently been addressed in another study, highlighting that a standardised concept of adequate follow-up care in Switzerland is required [32]. Although consensus on optimal psychosocial cancer care across the survivorship trajectory has resulted in published guidelines [21, 22, 25], implementation of recommended psychological screening in follow-up care is still rare [33, 44]. Thus far, only a few studies have explored influential factors related to the missing implementation of psychological screening with standardised instruments in healthcare professionals [33, 34, 36, 37].
In our study, none of the study participants had any previous experience with, or knowledge of, the emotion thermometer. Previous findings have shown that a knowledge gap on available instruments for psychological screening exists [34, 36]. One study reported that healthcare professionals from a large Canadian paediatric cancer centre wish to be informed about existing standardised instruments available for use in psychosocial care and wish to receive information on how to use them correctly [34]. In another study from Belgium, healthcare professionals additionally described having insufficient knowledge or education to effectively meet psychosocial needs [36]. A lack of knowledge-translation of existing instruments may result in a lack of use of evidence-based tools. Our recent systematic review showed that the emotion thermometer is valid and reliable, but rarely used [29]. A lack of use and experience may negatively impact knowledge dissemination and appreciation of psychological screening instruments and their benefits for follow-up care. A national survey in the US showed that across 44 states, less than 50% of paediatric oncology institutions use an evidence-based psychosocial screening approach [33]. Psychosocial screening standards were primarily met by informal discussion and an evidence-based approach was found in less than half of the centres [33].
Our results show that insufficient knowledge of available validated instruments was only one of the many barriers to standardised psychological screening. In fact, when learning about the emotion thermometer, the vast majority of our study participants agreed that it seemed to be a good instrument for assessing psychological late effects. Instrument-specific strengths were mentioned by all healthcare professionals, pointing toward the advantage of regularly using the emotion thermometer in follow-up care.
As one of the advantages of using the emotion thermometer, participants further reported that it increased awareness of the need to think of the psychological side of follow-up care. Looking at the emotion thermometer reminded them to consciously ask about psychological topics. The overall agreement on the importance of psychological screening suggests that psychological topics are addressed in some form. This was also confirmed by approximately half of healthcare professionals who agreed with the statement that psychological late effects are sufficiently assessed in follow-up care. In Belgium, healthcare professionals reported using the general question “How are you?” in over one third of the consultations to discuss psychosocial concerns in patients. The rest spontaneously addressed psychosocial aspects [36]. Similarly, the nationwide study in the US showed that psychosocial standards were met by informal discussion [33]. However, in a time-constrained setting the informal assessment of psychological problems may also vary in depth and result in inconsistent delivery of care. A study investigating healthcare professionals’ responses to emotional cues of cancer patients showed that 38% of emotional cues in conversations were ignored [45]. Furthermore, healthcare professionals responded more to informational than to emotional cues [45]. Systematic use of short screening instruments, such as the emotion thermometer, might therefore be beneficial as it prompts clinicians to actively ask about psychological late effects and provides concise documentation.
In our study, participants were concerned that when confronting survivors with psychological screening, survivors would in turn have higher expectations for the follow-up appointment, such as expecting to have their problems solved at once. Like our participants, other healthcare professionals have expressed experiencing fear that they could not fulfil expectations related to psychosocial concerns [36]. However, future research investigating patient-provider dynamics could provide insight into these propositions. The use of a standardised assessment could improve patient-provider conversations [33, 46]. Furthermore, communicating clear expectations for screening to facilitate the consistent use of psychosocial screening tools has been suggested [34].
Linked to this particular concern, lack of consultation time and lack of resources, as well as the infrastructure to follow-up on problems discovered, have been mentioned among the many barriers to psychosocial communication [37] and routine assessment of patient reported outcomes [47]. These findings are consistent with our study where healthcare professionals also said that they lacked time for a thorough psychological assessment. Some organisational barriers may be difficult to address, whereas others, such as perceived lack of time, may be alleviated by the brevity of the emotion thermometer. In fact, screening with the emotion thermometer takes less than 2 minutes [30, 40] and does not impact clinic visit time [31].
Opinions on emotion thermometer-specific attributes were discordant. For some, the emotion thermometer seemed too superficial, for others too personal. This indicates that individual preferences in communication and variations in personal attitudes exist amongst Swiss healthcare professionals. With regard to psychosocial screening, personal attitudes and values have been listed as a limiting factor to psychosocial risk screening [34]. Personal attitudes and values may reinforce perceived barriers to change in personal performance: from an informal conversation to actively using standardised psychological screening measures.
Among the instrument-specific strengths, the emotion thermometer’s ability to visualise psychological topics and help express feelings was highlighted by many healthcare professionals. A minority of healthcare professionals, however, experienced this particular instrument-specific property as a limitation of the tool, stating that it may not be suitable for all ages, especially small children. Even though the emotion thermometer is described as suitable for children [41], to date, there are no publications on the emotion thermometer being used in younger populations (aged ≤18 years). The emotion thermometer was designed to expand the existing distress thermometer (NCCN) [23]. A recent study examined another adapted distress thermometer (NCCN), similar to the emotion thermometer, in a paediatric outpatient setting including children diagnosed with cancer aged 7–21 years [27, 48]. This adapted distress thermometer proved to be reliable, valid and acceptable [27]. Testing and validating the emotion thermometer in younger populations, especially survivors in follow-up care, should further inform its clinical utility.
Not using the existing evidence-based approaches recommended by guidelines and thus not meeting the standards is of concern [33, 36]. Particularly, centres with low staff numbers and limited resources may prefer informal assessment of psychological distress rather than using an additional psychosocial tool. Informal assessment may lead to inconsistent and delayed delivery of specific psychological care [36]. This disregards the preventive approach of the recommended standards of care [33, 36]. In the long term, a standardised approach to psychological screening is beneficial for patients, their families and healthcare professionals [33].
Study limitations and strengths
Our study presents subjective opinions of healthcare professionals, which might differ within one institution, despite the provision of same care. Due to the number of paediatric oncology clinics in Switzerland our sample size is small. In turn there was a limited number of healthcare professionals who could provide resourceful primary data. However, we invited all healthcare professionals directly involved in CCS follow-up care, from all SPOG centres, to participate, in order to maximise generalisability of our findings. We specifically inquired about the emotion thermometer. However, despite showing the emotion thermometer in the questionnaire and providing information briefly, participants might not have had enough experience to provide an informed opinion. Additionally, social desirability bias might have influenced responses.
Strengths of our study include the recruitment of participants for whom our study topic was highly relevant, including various professions involved in CCS follow-up care. Another strength is the electronic survey including closed questions and one open question, which allowed not only a quantitative, but also a qualitative analysis of healthcare professionals’ opinions on the current standard of psychological follow-up care. The qualitative approach categorising perceived barriers and facilitators resulted in a deeper understanding of perceived positive and negative aspects of the emotion thermometer. Furthermore, we found great consistency between our findings and those of previous studies worldwide, as for instance shown by Schepers et al. in their study in over 50 countries [33, 34, 37, 47]. Therefore, we expect that our results are generalisable to other institutions in many other countries. This makes it possible to provide suggestions for future implementation also in other countries. Furthermore, for accuracy and high-quality of citations we used back-to-back translation, which is relevant when collecting data in one language and presenting results in another.
Clinical implications
Psychological topics are discussed in follow-up care in Switzerland; however, the assessment is not standardised. Use of the emotion thermometer to screen for psychological distress and assist in identifying survivors in need seems promising. With regard to psychological screening, research shows varying opinions; some state psychological screening should be performed by psychosocial staff only [34], whereas other healthcare professionals consider that addressing psychosocial issues is not part of the physician’s role, explaining that they do not feel qualified to do so [34, 36, 37]. Indisputably, discussing about who is responsible for the psychological part of care in the cancer trajectory needs to come first, since it might have an effect on the implementation process for standardised psychological screening [34, 36, 37].
We recommend providing essential information on potential instruments and their specific benefit for implementation to increase acceptability and facilitate a successful implementation. Additionally, specifically for the emotion thermometer, personal concerns about replacing the clinical assessment could be alleviated by pointing out that the instrument facilitates the detection of emotional areas in need without lengthening clinic visit time. Finally, including all involved individuals in the implementation of standardised psychological screening is necessary for provision of evidence-based care. Future studies should implement a short screening tool, such as the emotion thermometer, into follow-up care to address opinions of both healthcare professionals and CCS when they have experienced screening. Additionally, it will be crucial to evaluate the effectiveness to detect psychological distress in follow-up care.
Conclusion
Despite healthcare professionals confirming the good attributes of the emotion thermometer and agreeing on its regular use before follow-up appointment, our results reveal that healthcare professionals’ hesitance may hamper the implementation of evidence-based instruments for psychological screening.
It is important to mitigate perceived barriers and concerns of healthcare professionals to enable a successful implementation of psychological distress screening according to the established standards of care.
Acknowledgements
We thank all healthcare professionals for participating in our survey and the SPOG coordination centre for their support in the recruitment of participants.
References
1
Gatta
G
,
Botta
L
,
Rossi
S
,
Aareleid
T
,
Bielska-Lasota
M
,
Clavel
J
, et al.; EUROCARE Working Group. Childhood cancer survival in Europe 1999-2007: results of EUROCARE-5--a population-based study. Lancet Oncol. 2014;15(1):35–47. doi:.https://doi.org/10.1016/S1470-2045(13)70548-5
2
Gianinazzi
ME
,
Rueegg
CS
,
Wengenroth
L
,
Bergstraesser
E
,
Rischewski
J
,
Ammann
RA
, et al.; for Swiss Pediatric Oncology Group (SPOG). Adolescent survivors of childhood cancer: are they vulnerable for psychological distress?
Psychooncology. 2013;22(9):2051–8. doi:.https://doi.org/10.1002/pon.3249
3
Michel
G
,
Rebholz
CE
,
von der Weid
NX
,
Bergstraesser
E
,
Kuehni
CE
. Psychological distress in adult survivors of childhood cancer: the Swiss Childhood Cancer Survivor study. J Clin Oncol. 2010;28(10):1740–8. doi:.https://doi.org/10.1200/JCO.2009.23.4534
4
Kaye
EC
,
Brinkman
TM
,
Baker
JN
. Development of depression in survivors of childhood and adolescent cancer: a multi-level life course conceptual framework. Support Care Cancer. 2017;25(6):2009–17. doi:.https://doi.org/10.1007/s00520-017-3659-y
5
Zeltzer
LK
,
Recklitis
C
,
Buchbinder
D
,
Zebrack
B
,
Casillas
J
,
Tsao
JC
, et al.
Psychological status in childhood cancer survivors: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2009;27(14):2396–404. doi:.https://doi.org/10.1200/JCO.2008.21.1433
6
Bruce
M
. A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clin Psychol Rev. 2006;26(3):233–56. doi:.https://doi.org/10.1016/j.cpr.2005.10.002
7
Rourke
MT
,
Hobbie
WL
,
Schwartz
L
,
Kazak
AE
. Posttraumatic stress disorder (PTSD) in young adult survivors of childhood cancer. Pediatr Blood Cancer. 2007;49(2):177–82. doi:.https://doi.org/10.1002/pbc.20942
8
D’Agostino
NM
,
Edelstein
K
,
Zhang
N
,
Recklitis
CJ
,
Brinkman
TM
,
Srivastava
D
, et al.
Comorbid symptoms of emotional distress in adult survivors of childhood cancer. Cancer. 2016;122(20):3215–24. doi:.https://doi.org/10.1002/cncr.30171
9
Wiener
L
,
Battles
H
,
Bernstein
D
,
Long
L
,
Derdak
J
,
Mackall
CL
, et al.
Persistent psychological distress in long-term survivors of pediatric sarcoma: the experience at a single institution. Psychooncology. 2006;15(10):898–910. doi:.https://doi.org/10.1002/pon.1024
10
Secinti
E
,
Thompson
EJ
,
Richards
M
,
Gaysina
D
. Research Review: Childhood chronic physical illness and adult emotional health - a systematic review and meta-analysis. J Child Psychol Psychiatry. 2017;58(7):753–69. doi:.https://doi.org/10.1111/jcpp.12727
11
Jacobsen
PB
. Screening for psychological distress in cancer patients: challenges and opportunities. J Clin Oncol. 2007;25(29):4526–7. doi:.https://doi.org/10.1200/JCO.2007.13.1367
12
Foster
C
,
Wright
D
,
Hill
H
,
Hopkinson
J
,
Roffe
L
. Psychosocial implications of living 5 years or more following a cancer diagnosis: a systematic review of the research evidence. Eur J Cancer Care (Engl). 2009;18(3):223–47. doi:.https://doi.org/10.1111/j.1365-2354.2008.01001.x
13
Calaminus
G
,
Weinspach
S
,
Teske
C
,
Göbel
U
. Quality of life in children and adolescents with cancer. First results of an evaluation of 49 patients with the PEDQOL questionnaire. Klin Padiatr. 2000;212(4):211–5. doi:.https://doi.org/10.1055/s-2000-9679
14
Wengenroth
L
,
Gianinazzi
ME
,
Rueegg
CS
,
Lüer
S
,
Bergstraesser
E
,
Kuehni
CE
, et al.
Health-related quality of life in young survivors of childhood cancer. Qual Life Res. 2015;24(9):2151–61. doi:.https://doi.org/10.1007/s11136-015-0961-3
15
Gianinazzi
ME
,
Rueegg
CS
,
von der Weid
NX
,
Niggli
FK
,
Kuehni
CE
,
Michel
G
; Swiss Paediatric Oncology Group (SPOG). Mental health-care utilization in survivors of childhood cancer and siblings: the Swiss childhood cancer survivor study. Support Care Cancer. 2014;22(2):339–49. doi:.https://doi.org/10.1007/s00520-013-1976-3
16
Zebrack
BJ
,
Gurney
JG
,
Oeffinger
K
,
Whitton
J
,
Packer
RJ
,
Mertens
A
, et al.
Psychological outcomes in long-term survivors of childhood brain cancer: a report from the childhood cancer survivor study. J Clin Oncol. 2004;22(6):999–1006. doi:.https://doi.org/10.1200/JCO.2004.06.148
17
Jankovic
M
,
Haupt
R
,
Spinetta
JJ
,
Beck
JD
,
Byrne
J
,
Calaminus
G
, et al.
Long-term survivors of childhood cancer: cure and care—the Erice Statement (2006) revised after 10 years (2016). J Cancer Surviv. 2018;12(5):647–50. doi:.https://doi.org/10.1007/s11764-018-0701-0
18
Michel
G
,
Mulder
RL
,
van der Pal
HJH
,
Skinner
R
,
Bárdi
E
,
Brown
MC
, et al.
Evidence-based recommendations for the organization of long-term follow-up care for childhood and adolescent cancer survivors: a report from the PanCareSurFup Guidelines Working Group. J Cancer Surviv. 2019;13(5):759–72. doi:.https://doi.org/10.1007/s11764-019-00795-5
19Pfeiffer V, Redmond S, Kuonen R, Sommer G, Spycher B, Singh P, et al. Swiss Childhood Cancer Registry Annual Report 2015/2016. Bern, Switzerland: Swiss Childhood Cancer Registry; 2017
20
Schindler
M
,
Belle
FN
,
Grotzer
MA
,
von der Weid
NX
,
Kuehni
CE
; Swiss Paediatric Oncology Group (SPOG). Childhood cancer survival in Switzerland (1976-2013): Time-trends and predictors. Int J Cancer. 2017;140(1):62–74. doi:.https://doi.org/10.1002/ijc.30434
21(SIGN) SIGN. Long-term follow up of survivors of childhood cancer. Edinburgh, 2013
22CsOG. Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent and Young Adult Cancers. Monrovia, CA: Children's Oncology Group; 2013
23NCCN. NCCN Clinical Practice Guidelines in Oncology, Distress Management. National Comprehensive Cancer Network; 2007
24
Sieswerda
E
,
Postma
A
,
van Dalen
EC
,
van der Pal
HJH
,
Tissing
WJE
,
Rammeloo
LAJ
, et al.; Late Effects of Childhood Cancer task force of the Dutch Childhood Oncology Group (DCOG LATER). The Dutch Childhood Oncology Group guideline for follow-up of asymptomatic cardiac dysfunction in childhood cancer survivors. Ann Oncol. 2012;23(8):2191–8. doi:.https://doi.org/10.1093/annonc/mdr595
25
Wiener
L
,
Kazak
AE
,
Noll
RB
,
Patenaude
AF
,
Kupst
MJ
. Standards for the Psychosocial Care of Children With Cancer and Their Families: An Introduction to the Special Issue. Pediatr Blood Cancer. 2015;62(S5, Suppl 5):S419–24. doi:.https://doi.org/10.1002/pbc.25675
26
Mitchell
AJ
. Pooled results from 38 analyses of the accuracy of distress thermometer and other ultra-short methods of detecting cancer-related mood disorders. J Clin Oncol. 2007;25(29):4670–81. doi:.https://doi.org/10.1200/JCO.2006.10.0438
27
Wiener
L
,
Battles
H
,
Zadeh
S
,
Widemann
BC
,
Pao
M
. Validity, specificity, feasibility and acceptability of a brief pediatric distress thermometer in outpatient clinics. Psychooncology. 2017;26(4):461–8. doi:.https://doi.org/10.1002/pon.4038
28
Beck
KR
,
Tan
SM
,
Lum
SS
,
Lim
LE
,
Krishna
LK
. Validation of the emotion thermometers and hospital anxiety and depression scales in Singapore: Screening cancer patients for distress, anxiety and depression. Asia Pac J Clin Oncol. 2016;12(2):e241–9. doi:.https://doi.org/10.1111/ajco.12180
29
Harju
E
,
Michel
G
,
Roser
K.
A systematic review on the use of the emotion thermometer in individuals diagnosed with cancer. Manuscript submitted for publication. 2018
30
Mitchell
AJ
,
Baker-Glenn
EA
,
Granger
L
,
Symonds
P
. Can the Distress Thermometer be improved by additional mood domains? Part I. Initial validation of the Emotion Thermometers tool. Psychooncology. 2010;19(2):125–33. doi:.https://doi.org/10.1002/pon.1523
31
Schubart
JR
,
Emerich
M
,
Farnan
M
,
Stanley Smith
J
,
Kauffman
GL
,
Kass
RB
. Screening for psychological distress in surgical breast cancer patients. Ann Surg Oncol. 2014;21(10):3348–53. doi:.https://doi.org/10.1245/s10434-014-3919-8
32
Meier
JH
,
Ansari
M
,
Popovic
MB
,
Bergstraesser
E
,
Brazzola
P
,
Eisenreich
B
, et al.
Aftercare in Pediatric Oncology in Switzerland - Current State, Challenges and Future Directions. Schweizer Krebsbulletin. 2018:273–9
33
Scialla
MA
,
Canter
KS
,
Chen
FF
,
Kolb
EA
,
Sandler
E
,
Wiener
L
, et al.
Delivery of care consistent with the psychosocial standards in pediatric cancer: Current practices in the United States. Pediatr Blood Cancer. 2018;65(3):e26869. doi:.https://doi.org/10.1002/pbc.26869
34
Barrera
M
,
Alexander
S
,
Shama
W
,
Mills
D
,
Desjardins
L
,
Hancock
K
. Perceived benefits of and barriers to psychosocial risk screening in pediatric oncology by health care providers. Pediatr Blood Cancer. 2018;65(12):e27429. doi:.https://doi.org/10.1002/pbc.27429
35
Mitchell
A
,
Waller
A
,
Carlson
LE
. Implementing a screening programme for distress in cancer settings Science and practice. Psychooncology. 2012;9:259–75.
36
Schouten
B
,
Bergs
J
,
Vankrunkelsven
P
,
Hellings
J
. Healthcare professionals’ perspectives on the prevalence, barriers and management of psychosocial issues in cancer care: A mixed methods study. Eur J Cancer Care (Engl). 2019;28(1):e12936. doi:.https://doi.org/10.1111/ecc.12936
37
Fagerlind
H
,
Kettis
Å
,
Glimelius
B
,
Ring
L
. Barriers against psychosocial communication: oncologists’ perceptions. J Clin Oncol. 2013;31(30):3815–22. doi:.https://doi.org/10.1200/JCO.2012.45.1609
38
von Elm
E
,
Altman
DG
,
Egger
M
,
Pocock
SJ
,
Gøtzsche
PC
,
Vandenbroucke
JP
; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9. doi:.https://doi.org/10.1016/j.ijsu.2014.07.013
39Leiner DJ. SoSci Survey (Version 2.5.00-i)) 2014. Available from: https://www.soscisurvey.de/index.php?page=privacy&l=eng.
40
Mitchell
AJ
,
Baker-Glenn
EA
,
Park
B
,
Granger
L
,
Symonds
P
. Can the Distress Thermometer be improved by additional mood domains? Part II. What is the optimal combination of Emotion Thermometers?
Psychooncology. 2010;19(2):134–40. doi:.https://doi.org/10.1002/pon.1557
41Mitchell A. Emotion Thermometers Tool [Internet]. 2016 [cited 2018 January 7]. Available from: http://www.psycho-oncology.info/ET.htm.
42Clarke V, Braun V. Successful Qualitative Research: A Practical Guide for Beginners. London, UK: SAGE Publishing; 2013
43
van Nes
F
,
Abma
T
,
Jonsson
H
,
Deeg
D
. Language differences in qualitative research: is meaning lost in translation?
Eur J Ageing. 2010;7(4):313–6. doi:.https://doi.org/10.1007/s10433-010-0168-y
44
Michel
G
,
Vetsch
J
. Screening for psychological late effects in childhood, adolescent and young adult cancer survivors: a systematic review. Curr Opin Oncol. 2015;27(4):297–305. doi:.https://doi.org/10.1097/CCO.0000000000000196
45
Butow
PN
,
Brown
RF
,
Cogar
S
,
Tattersall
MH
,
Dunn
SM
. Oncologists’ reactions to cancer patients’ verbal cues. Psychooncology. 2002;11(1):47–58. doi:.https://doi.org/10.1002/pon.556
46
Velikova
G
,
Booth
L
,
Smith
AB
,
Brown
PM
,
Lynch
P
,
Brown
JM
, et al.
Measuring quality of life in routine oncology practice improves communication and patient well-being: a randomized controlled trial. J Clin Oncol. 2004;22(4):714–24. doi:.https://doi.org/10.1200/JCO.2004.06.078
47
Schepers
SA
,
Haverman
L
,
Zadeh
S
,
Grootenhuis
MA
,
Wiener
L
. Healthcare Professionals’ Preferences and Perceived Barriers for Routine Assessment of Patient-Reported Outcomes in Pediatric Oncology Practice: Moving Toward International Processes of Change. Pediatr Blood Cancer. 2016;63(12):2181–8. doi:.https://doi.org/10.1002/pbc.26135
48
Patel
SK
,
Mullins
W
,
Turk
A
,
Dekel
N
,
Kinjo
C
,
Sato
JK
. Distress screening, rater agreement, and services in pediatric oncology. Psychooncology. 2011;20(12):1324–33. doi:.https://doi.org/10.1002/pon.1859