
Figure 1 Setup for the supraclavicular block.
DOI: https://doi.org/10.4414/smw.2020.20288
Distal radius fractures are among the most common fractures in humans [1, 2]. In Switzerland, the annual incidence among adults ≥50 years old is 63.2/10,000 in women and 18.9/10,000 in men [1]. Ultrasound is gaining importance in the treatment of distal radius fractures. They can be diagnosed with a sensitivity of 95–97% and a specificity of 95–96% using ultrasound [3]. There is also evidence that ultrasound can be used to guide the repositioning of distal radius fractures and reduce reduction attempts [4, 5]. Furthermore, there is some evidence that surgery was negatively associated with the use of ultrasound for reduction [4].
To improve patient satisfaction in the emergency department, pain management is one of the most important factors [6]. Currently, most patients with distal radius fractures receive procedural sedation, even though procedural sedation is associated with rare but serious adverse events and needs constant monitoring [7]. In the operative setting, brachial plexus block has shown benefits for pain management, muscle relaxation and hospital discharge [8]. Several studies have shown that all the advantages of the brachial plexus block can be extended to the emergency department [9–11]. Ultrasound-guided regional anaesthesia (UGRA) is a reliable method to achieve an efficient and effective brachial plexus block with fewer side effects than when the procedure is performed without sonographic visualisation [11, 12].
So far, most studies have used radiological endpoints to measure the quality of distal radius fractures treatment [4, 13]. However, there is growing evidence that radiological indices do not correlate with the functional outcome, particularly in older patients [2, 14, 15]. One case series showed that 89% of all elderly patients with distal radius fractures and conservative therapy have good to excellent outcomes [2]. Furthermore, surgery is associated with longer hospital stays, higher risks and higher costs [2, 15]. Therefore, the goal should be to optimise conservative repositioning so that no further surgery is required.
The use of ultrasound in the emergency department is increasing, but there is a lack of studies on the use of ultrasound on multiple occasions during the treatment of a single injury. Therefore, the aim of our investigation was to perform an ultrasound-guided reduction (UGR) under UGRA after receiving the x-ray of the fracture and to compare this new procedure with usual treatment, in order to test safety, feasibility and effectiveness.
This retrospective cohort study was carried out in the emergency department of the University Hospital Basel (Switzerland) between February 2014 and October 2017. The local ethics committee approved the study protocol. The goal of the study was to compare UGR with usual care, in order to test safety, feasibility and effectiveness.
The primary goal (endpoint) was to anaesthetise and perform the fracture reduction by means of ultrasound in the emergency department (feasibility). The next endpoint was the minimisation of operative interventions in these patients (effectiveness). Procedure-related complications such as nerve injuries, bleeding, infections and pneumothoraces were listed (safety).
Patients over 18 years old with a distal radius fracture were eligible for inclusion. Only isolated distal forearm fractures were included, so the pain management was not influenced by other injuries. Oral informed consent was given by all patients after information on the procedure and the side effects of both treatments.
After standard clinical assessment and initial x-ray, the emergency physician in charge decided on the necessity of a reduction. UGR was offered if a UGRA-trained emergency physician was on duty. In the absence of a trained interventionalist, usual care was initiated as described in the protocols of our hospital (www.medstandards.org).
Patients in the intervention group received UGRA in the form of a supraclavicular or an axillar block (figs 1–3 ). A HITACH Hi Vision AVIUS with a 50-mm linear-array probe (5.0–13.0 MHz) or a MINDRAY TE7 with 16 MHz linear transducer was used. The regional anaesthesia was 13 to 40 ml bupivacaine 0.5% or prilocaine 2% and was applied with a PAJUNK SonoPlex Stim cannula 22G x 50 mm. It was single-dose regional anaesthesia without additional stimulation. To perform the UGRA, emergency physicians had to attend a 2-day course in ultrasound-guided regional anaesthesia. The same ultrasound set-up was used to guide the reposition. A long-axis view generated the necessary information for this procedure (fig. 4).

Figure 1 Setup for the supraclavicular block.

Figure 2 Anatomical schema and Doppler ultrasound image of the brachial plexus.
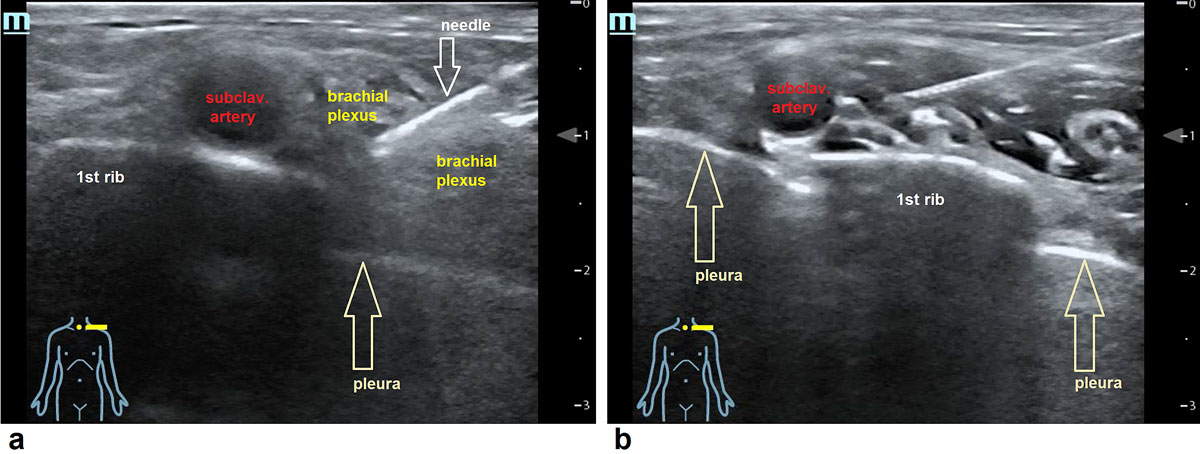
Figure 3 Ultrasound image of the brachial plexus. (a) Needle is placed between the nerves of the brachial plexus in the supraclavicular region above the first rib. (b) After injection of 15 ml local anaesthetic the nerves are surrounded with the fluid.

Figure 4 Ultrasound guided reposition of the distal radius fracture.
The control group was double the size of the intervention group. Controls were chosen from the database of the University Hospital Basel and had to have the same diagnosis, the same sex and the same age as the patients; additionally, they had to be treated in the same time period as the intervention group. The first patients identified by the computer as fulfilling all criteria were added to the control group. Control patients all received the current standard therapy, which is procedural sedation with midazolam 1–2 mg intravenously and morphine titrated in 2-mg steps as clinically needed. The reduction was performed with extension and clinical palpation, followed by check radiography.
Patients in the intervention group also had a second x-ray after the repositioning. The orthopaedic surgeon on call decided whether surgery was needed after reduction in all patients. Orthopaedic surgeons were not informed about the study’s content and aim. If no surgery was indicated, the patients were discharged with a cast and ambulatory standard care.
All participants completed their entire treatment at the University Hospital Basel.
If at any point in the 3-month follow-up a decision to operate was made, the case was marked as an operation, regardless of the time-point of the decision.
Data collection and statistical analysis by logistic regression were performed with JASP (Vs 0.9.1, 2018 University of Amsterdam). Logistic regression was used for associations between the groups and the interventions. All analyses were controlled for group, age and sex. Because of the wide variation in age in our cohort, we did a subgroup analysis for elderly patients (over 60 years).
Safety was defined as a complication rate under 2%. Feasibility was defined as the consecutive inclusion of over 50 patients solely by trained emergency physicians. Effectiveness was defined as a comparable rate of operations in the intervention and control groups.
Throughout the study period, 71 consecutive patients were enrolled. The control group consisted of 142 patients, selected as described in the methods section. In total, there were 213 distal radius fractures and 211 were isolated distal radius fractures. Two had additional distal ulna fractures (one in each group). There were no significant differences in the baseline characteristics of both groups (table 1). Twenty-five patients (35%) of the intervention group and 67 patients (47%) of the control group underwent surgery (table 2).
Table 1 Baseline characteristics for all patients and patients aged ≥60 years.
| All patients | Patients ≥60 | |||
|---|---|---|---|---|
| Intervention group | Control group | Intervention group | Control group | |
| Total cases, n | 71 | 142 | 54 | 106 |
| Female, n (%) | 59 (83.1) | 115 (81.0) | 50 (92.6) | 95 (89.6) |
| Age | ||||
| Median | 78.00 | 73.50 | 80.50 | 79.50 |
| Minimum | 25 | 21 | 61 | 60 |
| Maximum | 92 | 98 | 92 | 98 |
Table 2 Operation rates for all patients and patients aged ≥60 years.
| All patients | Patients ≥60 | |||
|---|---|---|---|---|
| Intervention group | Control group | Intervention group | Control group | |
| Total cases, n | 71 | 142 | 54 | 106 |
| Op yes, n (%) | 25 (35.2) | 67 (47.2) | 12 (22.2) | 43 (40.6) |
Op yes: Patients who underwent surgery after primarily being treated conservatively
In the multivariate regression model testing the association between group and surgery, adjusted for age and sex, no significant difference could be shown (p = 0.08). The patients’ age was inversely associated (p <0.001) with surgery (table 3, figure 5).
Table 3 Coefficients for all patients.
| Odds ratio | p-value | 95% confidence interval (odds ratio scale) | ||
|---|---|---|---|---|
| Lower bound | Upper bound | |||
| Age | 0.943 | <0.001 | 0.922 | 0.964 |
| Group (intervention) | 0.563 | 0.083 | 0.294 | 1.078 |
| Gender (f) | 1.807 | 0.187 | 0.751 | 4.350 |

Figure 5 Correlation between age and operation likelihood.
Op: Operation, Yes(1): Patients who underwent surgery after primarily being treated conservatively, No(0): completely conservatively treated patients, P: likelihood, grey dots: every dot represents one patient. Grey banner: 95% confidence interval, black line: operation likelihood according to patient’s age.
A predefined subgroup analysis in patients ≥60 years of age was conducted. In this subgroup, 54 patients were in the intervention group, and 106 in the control group. Age and gender were not significantly different (see table 1). Twelve patients (22%) underwent surgery in the intervention group and 43 (41%) in the control group. The multivariate logistic regression, adjusted for age and sex showed a significant (p = 0.035) negative correlation between intervention and operation (odds ratio 0.426, 95% confidence interval 0.193–0.942) (table 4, figure 6). Age was also negatively correlated with surgery in this intervention subgroup (p <0.001).
Table 4 Coefficients for patients aged ≥60 years.
| Odds ratio | p-value | 95% confidence interval (odds ratio scale) | ||
|---|---|---|---|---|
| Lower bound | Upper bound | |||
| Age | 0.917 | <0.001 | 0.879 | 0.956 |
| Group (intervention) | 0.426 | 0.035 | 0.193 | 0.942 |
| Gender (f) | 2.169 | 0.232 | 0.609 | 7.723 |

Figure 6 Correlation between treatment group and operation likelihood in patients ≥60 years old.
Op: Operation, Yes(1): Patients who underwent surgery after primarily being treated conservatively, No(0): completely conservatively treated patients, P: likelihood, grey dots: every dot represents one patient, black dot: represent the mean likelihood to get an operation, plot: shows the 95% confidence interval of the operation likelihood.
There was one (1.4%) complication related to UGRA or UGR in the 71 patients in the intervention group: an 89-year-old cachectic patient who had UGRA by an emergency physician with the minimum training required (2 day course and fewer than 10 interventions). The patient fully recovered within 1 week of hospitalisation without sequelae. No other side effects from UGRA were detected within the 3-month follow-up.
The main results of the study related to the feasibility, the relative safety and the effectiveness of UGR.
We were therefore particularly interested in the results in patients aged 60 and over and had predefined an analysis in this subgroup, in which UGR could well have the most impact. According to the literature, older patients have the highest incidence of distal radius fractures and the lowest incidence of surgery [1]. In our subgroup analysis of elderly patients, only 22% underwent surgery in the intervention group, as compared with 41% in the control group. A comparable study claimed to achieve a lower operation rate by using ultrasound-guided reduction [4]. However, this can only be proven by strict randomisation, as retrospective cohort studies are prone to selection bias.
Still, UGR is a promising method, as reduction may be achieved by improved muscle relaxation, lower levels of pain and direct visual feedback during reduction. To regard the effect of UGRA compared to reduction under procedural sedation on pain score during and after the reduction, further studies are necessary. Additional benefits of the use of ultrasound include the lack of radiation, the economic advantage over fluoroscopy [13], the cooling effect of ultrasound gel [3], its availability in most emergency departments, the possibility of detecting additional soft tissue injuries [13] and the steep learning curve inherent to the method [3]. UGRA and UGR should therefore be used more widely in emergency medicine [11].
The main limitation is that of a single centre study. External validity is therefore limited. The second limitation is that it was a retrospective cohort study, a method that is prone to inclusion bias. It cannot be guaranteed that the controls are similar to the patients, as they were only matched for age, sex and time of inclusion. Third, the study was not powered to show superiority because it was not clear which effect size the intervention would have due to lack of data in the literature. However, the pilot study character allows hypothesis generation, such as the usefulness in a population over 60 years of age.
Our study suggests, that in distal radius fractures of elder patients, ultrasound guided regional anaesthesia of the brachial plexus in combination with ultrasound guided reduction of the fracture is a feasible method to lower the number of operations in this group of patients. Further research is required to support this preliminary statement.
This work was supported by scientific funds of the Emergency Department of the University Hospital Basel.
No potential conflict of interest relevant to this article was reported.
1 MacIntyre NJ , Dewan N . Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther. 2016;29(2):136–45. doi:.https://doi.org/10.1016/j.jht.2016.03.003
2 Gehrmann SV , Windolf J , Kaufmann RA . Distal radius fracture management in elderly patients: a literature review. J Hand Surg Am. 2008;33(3):421–9. doi:.https://doi.org/10.1016/j.jhsa.2007.12.016
3 Schmid GL , Lippmann S , Unverzagt S , Hofmann C , Deutsch T , Frese T . The investigation of suspected fracture-a comparison of ultrasound with conventional imaging. Dtsch Arztebl Int. 2017;114(45):757–64. doi:.https://doi.org/10.3238/arztebl.2017.0757
4 Sabzghabaei A , Shojaee M , Arhami Dolatabadi A , Manouchehrifar M , Asadi M . Ultrasound-Guided Reduction of Distal Radius Fractures. Emergency (Tehran). 2016;4(3):132–5.
5 Ang S-H , Lee S-W , Lam K-Y . Ultrasound-guided reduction of distal radius fractures. Am J Emerg Med. 2010;28(9):1002–8. doi:.https://doi.org/10.1016/j.ajem.2009.05.022
6 Bhakta HC , Marco CA . Pain management: association with patient satisfaction among emergency department patients. J Emerg Med. 2014;46(4):456–64. doi:.https://doi.org/10.1016/j.jemermed.2013.04.018
7 Stone MB , Wang R , Price DD . Ultrasound-guided supraclavicular brachial plexus nerve block vs procedural sedation for the treatment of upper extremity emergencies. Am J Emerg Med. 2008;26(6):706–10. doi:.https://doi.org/10.1016/j.ajem.2007.09.011
8 Galos DK , Taormina DP , Crespo A , Ding DY , Sapienza A , Jain S , et al. Does Brachial Plexus Blockade Result in Improved Pain Scores After Distal Radius Fracture Fixation? A Randomized Trial. Clin Orthop Relat Res. 2016;474(5):1247–54. doi:.https://doi.org/10.1007/s11999-016-4735-1
9 Schoell E , Feissli S , Bingisser R , Ammann S , Mueller AM , Haeni DL . Comparison of ultrasound-guided interscalene block versus procedural sedation for closed shoulder reduction in a Swiss university emergency department. Emergency Medicine and Healthcare. 2017;5(1):1–5. doi:.https://doi.org/10.7243/2052-6229-5-1
10 Alimohammadi H , Shojaee M , Samiei M , Abyari S , Vafaee A , Mirkheshti A . Nerve Stimulator Guided Axillary Block in Painless Reduction of Distal Radius Fractures; a Randomized Clinical Trial. Emergency (Tehran). 2013;1(1):11–4.
11 Herring AA . Bringing Ultrasound-guided Regional Anesthesia to Emergency Medicine. AEM Educ Train. 2017;1(2):165–8. doi:.https://doi.org/10.1002/aet2.10027
12 Gauss A , Tugtekin I , Georgieff M , Dinse-Lambracht A , Keipke D , Gorsewski G . Incidence of clinically symptomatic pneumothorax in ultrasound-guided infraclavicular and supraclavicular brachial plexus block. Anaesthesia. 2014;69(4):327–36. doi:.https://doi.org/10.1111/anae.12586
13 Kodama N , Takemura Y , Ueba H , Imai S , Matsusue Y . Ultrasound-assisted closed reduction of distal radius fractures. J Hand Surg Am. 2014;39(7):1287–94. doi:.https://doi.org/10.1016/j.jhsa.2014.02.031
14 Anzarut A , Johnson JA , Rowe BH , Lambert RGW , Blitz S , Majumdar SR . Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated distal radius fractures. J Hand Surg Am. 2004;29(6):1121–7. doi:.https://doi.org/10.1016/j.jhsa.2004.07.002
15 Jaremko JL , Lambert RGW , Rowe BH , Johnson JA , Majumdar SR . Do radiographic indices of distal radius fracture reduction predict outcomes in older adults receiving conservative treatment? Clin Radiol. 2007;62(1):65–72. doi:.https://doi.org/10.1016/j.crad.2006.08.013
This work was supported by scientific funds of the Emergency Department of the University Hospital Basel.
No potential conflict of interest relevant to this article was reported.