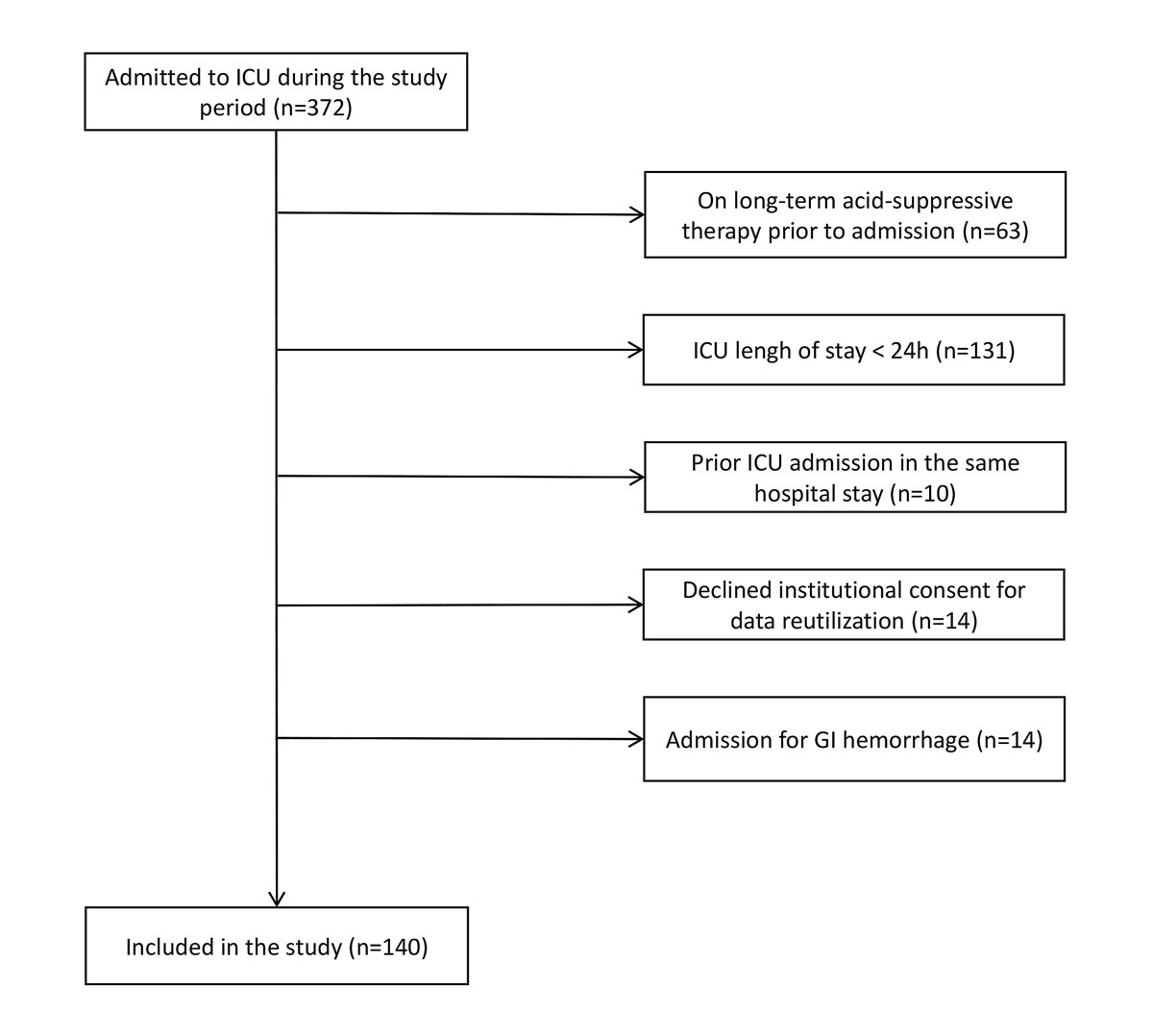
Figure 1 Patients’ inclusion. GI = gastrointestinal; ICU = intensive care unit
DOI: https://doi.org/10.4414/smw.2020.20322
activated partial thromboplastin time
Clostridioides difficile infection
H2 receptor antagonists
intensive care unit
international normalised ratio
proton pump inhibitor
Stress ulcers have long been a feared complication of critical illnesses. They are thought to be related to a reduction in mucosal blood flow and/or a decrease of mucosal defence mechanisms against acid and pepsin. Usually located in the gastro-duodenal area, severe stress ulcers can lead to catastrophic bleeding [1, 2].
The incidence of stress ulcers is low nowadays (less than 5% of critically ill patients), probably thanks to the implementation of prophylactic measures collectively referred to as stress ulcer prophylaxis [3, 4]. Stress ulcer prophylaxis includes non-pharmacological measures that should probably be universally applied to patients admitted to the intensive care unit (ICU): early enteral nutrition, avoidance of gastrotoxic drugs and early shock reversal [5]. Pharmacological measures include proton pump inhibitors (PPIs) and H2 receptor antagonists (H2RA). Such therapy is generally viewed by clinicians as cheap and well tolerated. It is therefore prescribed to a very large proportion of patients in the ICU [6]. However, the indications and duration of this widespread prescription are being increasingly debated. Indeed, given the number of patients treated, inadequate stress ulcer prophylaxis prescription will have cost implications. In addition, recent data have challenged its safety and suggested that it could be associated with an increased incidence of complications such as pneumonia, Clostridioides difficile colitis [7] or cardiovascular events [8, 9]. These complications might lead to increased mortality, length of stay and costs. Hence, the adequacy of stress ulcer prophylaxis administration represents an important health issue.
Several reports have suggested that stress ulcer prophylaxis prescription during ICU stay might be inadequate [6, 10, 11]. In the absence of a strong consensus on initiation criteria, this inadequacy seems mostly related to stress ulcer prophylaxis maintenance after the critical phase. Stress ulcer prophylaxis prescription appears to be insufficiently challenged throughout ICU stay, and on many occasions is maintained on ICU, or even on hospital, discharge. The Swiss Society of Intensive Medicine, as part of its "Choosing wisely" campaign, has recently recommended assessing the adequacy of stress ulcer prophylaxis, as well as of other common practices in intensive medicine [12].
This study aims to evaluate the frequency and adequacy of stress ulcer prophylaxis prescription in a tertiary ICU of a Swiss university hospital. In addition, it aims to evaluate stress ulcer prophylaxis duration and its continuation on ICU and hospital discharge, as well as its potential health economics consequences.
This was a monocentric, observational study conducted in the adult intensive care unit (ICU) of the Centre Hospitalier Universitaire Vaudois (CHUV), a tertiary, university-affiliated hospital. This is a 35-bed ICU with approximately 2000 admissions per year. All consecutive patients admitted between 1 October and 5 December 2017 were considered for inclusion in the study. Exclusion criteria were: ICU length of stay less than 24 hours, pre-existing acid-suppressive therapy prior to admission, admission for a gastrointestinal haemorrhage, prior ICU admission in the same hospital stay, and declined consent for data reutilisation.
The study protocol was approved by the Ethics Committee of Vaud (CER-VD 2018-00568). The need for specific individual informed patient consent was waived due to the observational nature of the study. Patients who declined our institution’s general consent for data reutilisation were excluded from the study.
All data were obtained using electronic chart records (Metavision®, IMD Soft, Tel Aviv, Israel and SOARIAN®, Cerner, North Kansas City, USA). We collected the following data: sex, age, history of gastrointestinal bleeding, PPI or H2RA receipt on ICU admission, diagnosis, corticosteroid treatment, mechanical ventilation duration, enteral nutrition, and laboratory tests results. For patients with multiple ICU stays, only the first was considered for baseline data, and only the last for outcome data.
For each patient and each study day, the presence of an indication for stress ulcer prophylaxis was assessed. During the ICU stay, based on our local policy, stress ulcer prophylaxis was considered as indicated in the following situations: platelet count <50 G/l, international normalised ratio (INR) >1.5, aPTT (activated partial thromboplastin time) >2 times baseline, prolonged (>48 hrs) mechanical ventilation, history of gastrointestinal bleeding, traumatic brain injury, spinal trauma, severe (>20% body surface area) burn and shock. In addition, in other situations (prolonged [>7 days] ICU admission and need for high-dose [>250 mg equivalent hydrocortisone] corticosteroids), our local policy recommends “considering stress ulcer prophylaxis”. These last two criteria were considered as minor criteria.
Outside of the ICU, our institutional guidelines recommend against stress ulcer prophylaxis.
For each patient and each study day, the actual prescription of stress ulcer prophylaxis was assessed. The assessment was performed by two investigators (JP for ICU stays and MF for ward stays). For each study day, patients’ medical charts were screened for an indication for stress ulcer prophylaxis and for its prescription. The prescription was considered adequate if: (1) the drug was prescribed in the presence of a recognised indication (above), (2) the drug was not prescribed in the absence of a recognised indication (above) or (3) if our local guidelines recommended “considering stress ulcer prophylaxis”, irrespective of the actual drug prescription. All other situations were considered as inadequate. Unclear situations were discussed with the senior investigators (PV and AS).
After ICU discharge, including on hospital discharge, stress ulcer prophylaxis continuation was considered adequate if a new indication for PPI or H2RA was present, as defined by the US Food and Drug Administration (FDA) and the UK National Institute for Health and Care Excellence (NICE) guidelines (supplementary table S1 in appendix 1) [13–17].
In order to evaluate the societal impact of inadequate stress ulcer prophylaxis prescription, we estimated the direct costs associated with inadequate stress ulcer prophylaxis prescription. This evaluation was performed for the entire ICU stay based on the number of patients-days during which the therapy was prescribed while not indicated, the type of stress ulcer prophylaxis and its specific daily cost. This cost was then extrapolated to an entire year, assuming a similar inadequate to adequate therapy ratio.
In a second step, we estimated the potential costs associated with inadequate stress ulcer prophylaxis maintenance on hospital discharge. We based our estimation on the number of patients discharged with a stress ulcer prophylaxis prescription in the absence of an indication for acid-suppressive therapy and the daily cost of such therapy. We report the additional costs associated with mean therapy durations of 3 and 12 months after ICU discharge.
All costs were estimated based on the ex-factory prices for stress ulcer prophylaxis medications. Since a large number of preparations are available, we report the range (minimum and maximum) of prices for each situation. The prices and elements taken into account for the calculations are presented in the appendix 1 (supplementary figs S1–S3 ).
Continuous data with normal distributions are reported as mean (standard deviation). Non-normally distributed data are reported as median (inter-quartile range). Ordinal data are reported as number (percentage). SPSS version 25 was used for statistical analysis.
During the study period (fig. 1), 372 patients were admitted to our ICU. Of these, 63 (16.9%) were on long-term acid-suppressive therapy, 131 (35.2%) stayed less than 24h in the ICU, 10 (2.7%) had already been admitted to the ICU, 14 (3.7%) had acid-suppressive therapy initiated for gastrointestinal bleeding and 14 (3.7%) denied their institutional consent to participate in research. Hence, 140 patients (855 patient-days) were included in this study’s analysis. Their characteristics on ICU admission are presented in table 1. In summary, around two thirds were men (96 men, 44 women), median age was 65 years (17–92) and median length of stay in the ICU was 3.8 days (1–47).
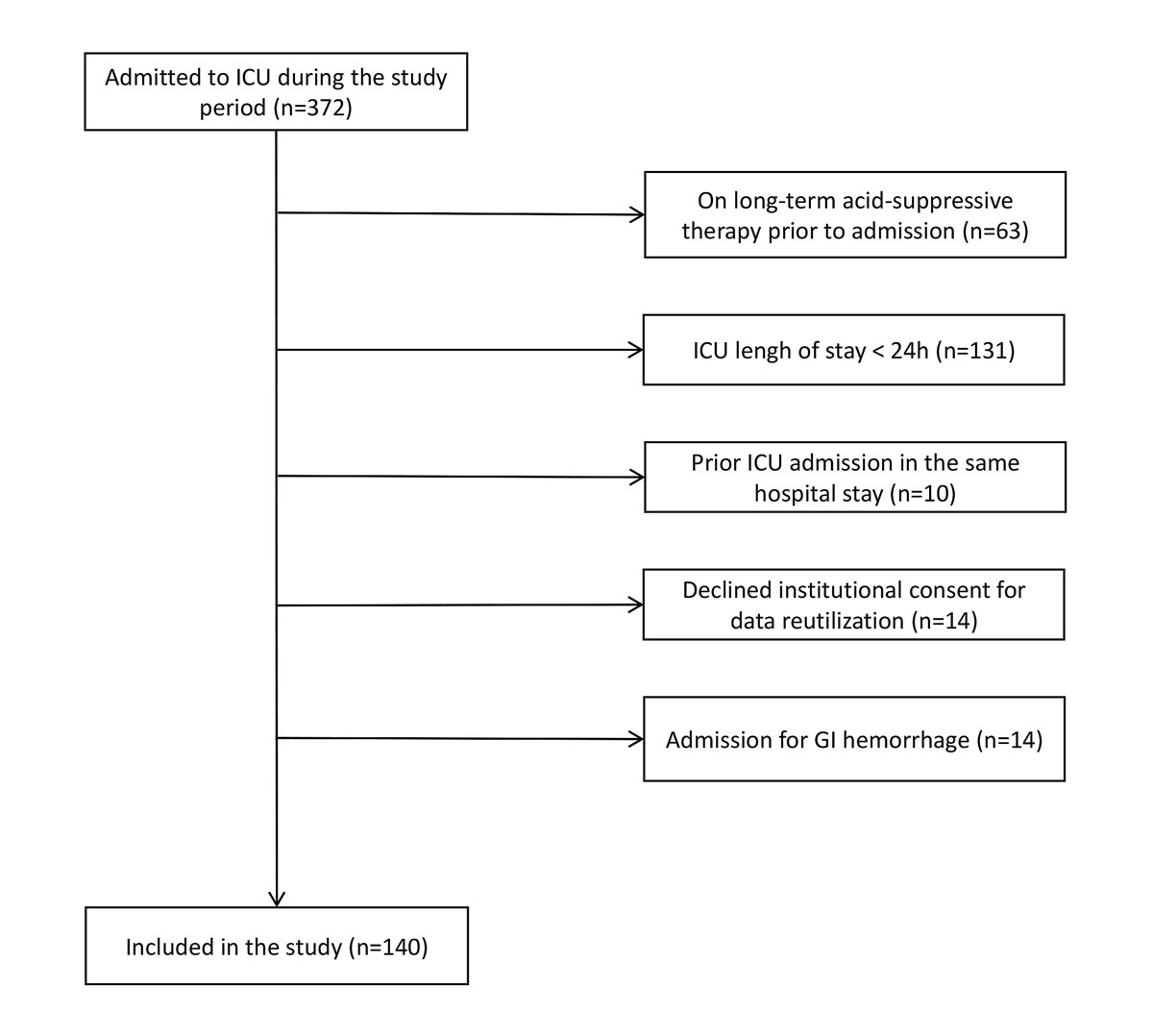
Figure 1 Patients’ inclusion. GI = gastrointestinal; ICU = intensive care unit
Table 1 Patients’ characteristics (n = 140).
| Median age, (IQR) years | 65 (19–92) |
| Male sex, n (%) | 96 (68.6%) |
| Median length of stay, (IQR) days | 3.8 (2.4–7.9) |
| Median SAPS II score, (IQR) | 44.5 (33.0–60.0) |
| Patients’ category (on ICU admission), n (%) | |
| – Medical | 42 (29%) |
| – Cardiac medical | 29 (20%) |
| – Cardiothoracic surgery | 29 (20%) |
| – Neurosurgery | 18 (12%) |
| – Surgery (others) | 22 (13.9%) |
| ICU mortality, n (%) | 24 (17.1%) |
| Hospital mortality, n (%) | 27 (20.7%) |
Over the study period, 130 (92.9%) patients received stress ulcer prophylaxis at some stage during their ICU stay. This corresponded to 796 (79.7%) patient-days.
The drug administered as stress ulcer prophylaxis was esomeprazole in 686 patient-days (86.2%), ranitidine in 108 patient-days (13.6%) and both in 2 patient-days (0.2%, intra-day prescription modification).
As presented in figure 2, mechanical ventilation was the most common indication for stress ulcer prophylaxis (461 patient-days, 54.0%), followed by shock (66 patient-days, 7.7%) and traumatic brain injury (66 patient-days, 7.7%). Prolonged ICU stay was also very common (350 patient-days, 40.9%), and a major criterion was present for 315 patient-days.
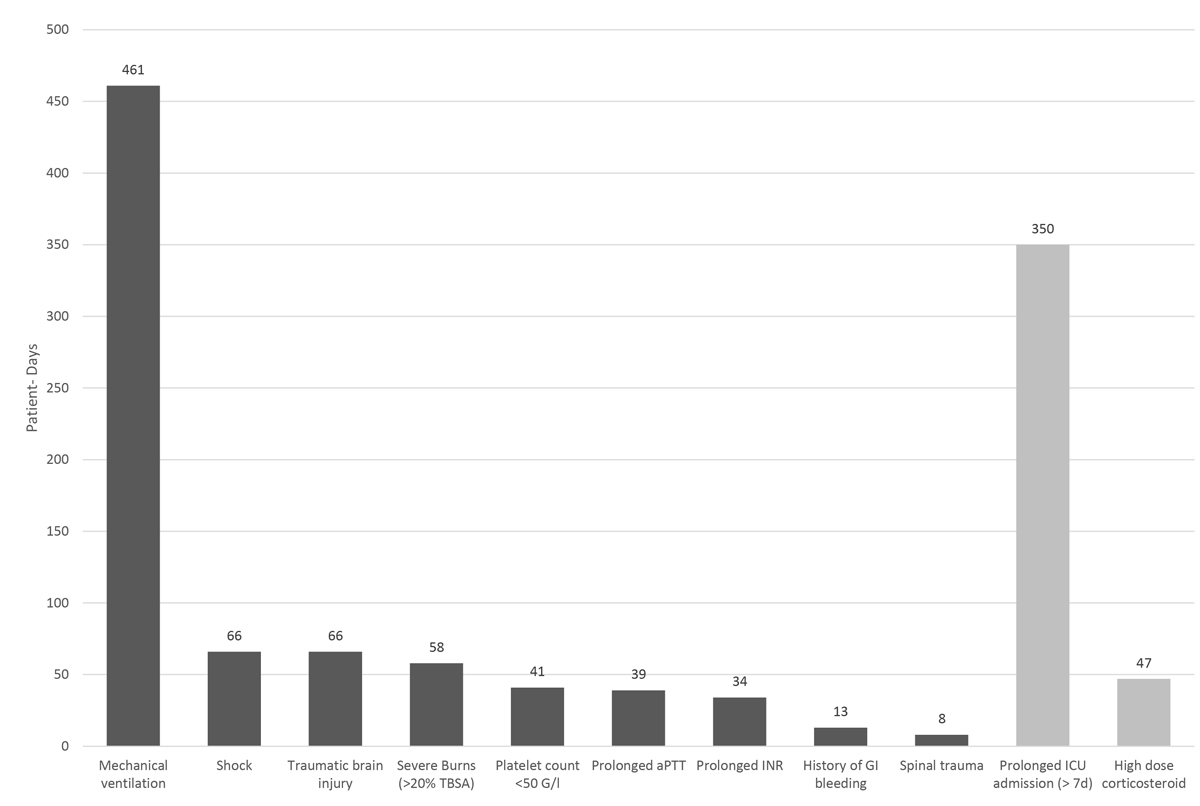
Figure 2 Criteria for stress ulcer prophylaxis (SUP) prescription in the intensive care unit. Number of patients-days during which criteria for SUP prescription were fulfilled according to our local guidelines (more than one criterion might be fulfilled in a single patient-day). aPTT = activated partial thromboplastin time; GI = gastrointestinal; ICU = intensive care unit; INR = international normalised ratio; TBSA = total body surface area
As depicted in figure 3, stress ulcer prophylaxis prescription was adequate in 297 patient-days (34.7%): it was prescribed with a recognised indication in 253 patient-days (29.6%) and not prescribed in the absence of an indication in 44 patient-days (5.1%). On the other hand, stress ulcer prophylaxis prescription was inadequate in 558 patient-days (65.3%): stress ulcer prophylaxis was prescribed in the absence of a recognised indication in 543 patient-days (63.5%) and not prescribed in the presence of a recognised indication in 15 patient-days (1.8%).
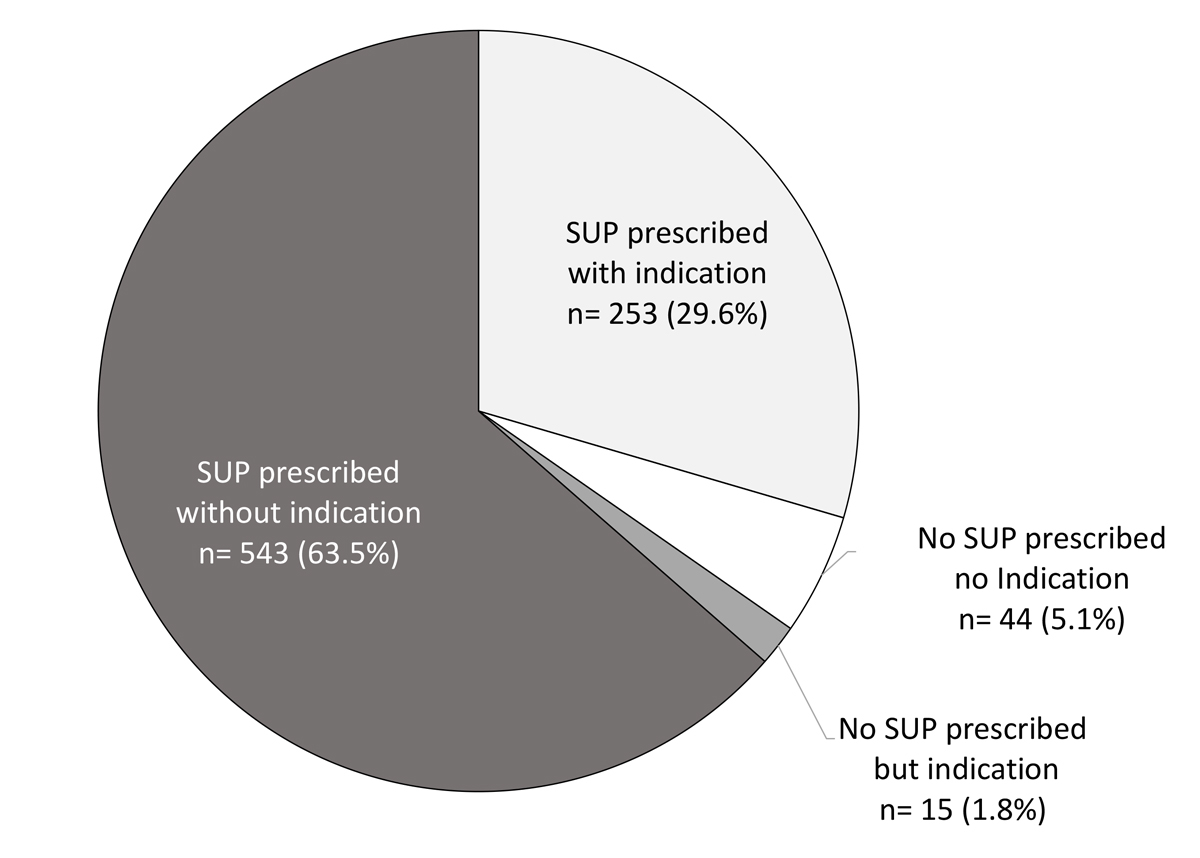
Figure 3 Adequacy of stress ulcer prophylaxis (SUP) prescription during intensive care unit stay. Indication: presence of a recognised indication according to our local guidelines.
Of the 130 patients who received stress ulcer prophylaxis at any time during their ICU stay, 106 (81.5%) survived to ICU discharge. Of these, eight (7.5%) developed an indication for acid-suppressive therapy during their stay and were prescribed the therapy on ICU discharge. Twelve (11.3%) were transferred to another acute hospital with an ongoing stress ulcer prophylaxis prescription (nine with stress ulcer prophylaxis, including six without an indication). Finally, 55 (51.9% of survivors) were transferred to the ward while still receiving stress ulcer prophylaxis without a recognised indication (fig. 4).
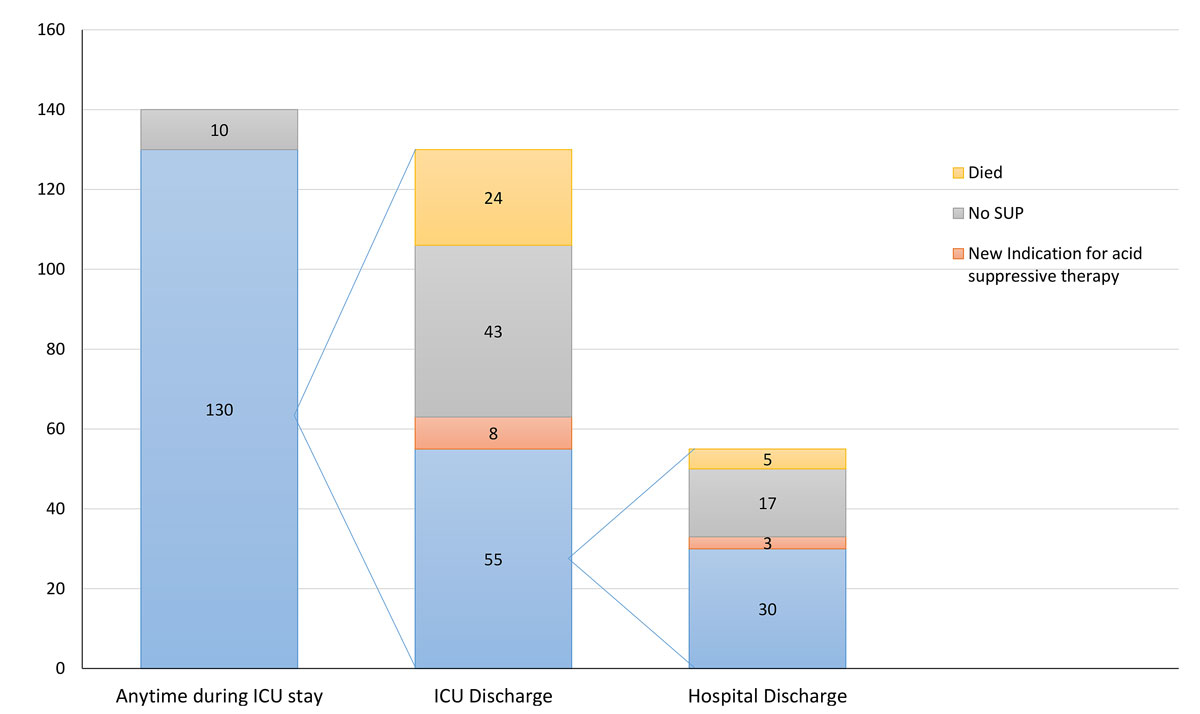
Figure 4 Adequacy of acid-suppressive therapy on ward stay and hospital discharge.
Of the 55 patients discharged to the ward with an ongoing stress ulcer prophylaxis prescription, five (9.1%) died while on the ward. Of those who survived to hospital discharge, three (6.0%) developed a new indication for acid-suppressive therapy during their post-ICU hospital stay. One had incomplete data, so discharge treatment could not be verified. However, 30 patients (60%, 30.3% of all survivors) were discharged from the hospital on acid-suppressive therapy without a recognised indication.
Based on ex-factory prices, the excess costs associated with inadequate therapy during the study period correspond to CHF 1220 (approx. EUR 1100). Extrapolated to our entire ICU population, this would correspond to an excess cost of CHF 6743 (approx. EUR 6000) per year.
Depending on the type and brand of stress ulcer prophylaxis used, the excess costs associated with inadequate stress ulcer prophylaxis prescription on hospital discharge would range from CHF 8361 to 22,855 (EUR 7500 to 20,500) if maintained for three months, or from CHF 33,912 to 92,692 (EUR 31,832 to 87,012) if maintained for 12 months.
We performed a retrospective observational study on 855 ICU patient-days to assess the frequency and adequacy of stress ulcer prophylaxis prescription in a tertiary ICU of a Swiss university hospital. We found that stress ulcer prophylaxis was prescribed in 92.8% of patients (796 patient-days), that it mainly consisted of esomeprazole and that the main indications were mechanical ventilation, prolonged ICU stay and shock. We found that stress ulcer prophylaxis prescription was inadequate in 65.2% of cases, mostly because it was prescribed in the absence of a recognised indication. More surprisingly, we found that even in the absence of a new indication for acid-suppressive therapy, stress ulcer prophylaxis was maintained on ICU discharge in almost 50% of patients and on hospital discharge in more than 25% of patients. Despite the relatively low cost of the medication, our health economics analysis demonstrates that this inadequate prescription is associated with only minor in-hospital additional costs, but with potentially significant costs when continued after discharge.
As summarised in supplementary table S2 (appendix 1), our results are largely consistent with data obtained in other settings and health care systems. In a Swiss general surgery department [18], stress ulcer prophylaxis was administered without indication in 79% of the 67 evaluated patients and continued on hospital discharge in 33% of those with a de novo anti-acid prescription. In Australia, two studies reported very similar rates of inadequate continuation of acid-suppressive medication on ICUs (63%) and on hospital discharge (39 and 48.9%) [6, 10]. Similar observations were made in the United States, where 20–30% of ICU survivors appeared to have been discharged from hospital with an ongoing stress ulcer prophylaxis without indication [11, 13]. Finally, an international survey of 97 ICU in 11 countries suggested that in almost 20% of the participating sites, stress ulcer prophylaxis was not stopped upon discharge to the ward. Similarly, 31–39% of patients treated with stress ulcer prophylaxis during ICU stays were reported to be discharged from hospital with ongoing treatment [3].
The health economics aspects were also considered in other healthcare systems. Indeed, in a retrospective study involving five ICUs in Western Australia, it was estimated that during the study period, 1482 patients were inadequately prescribed PPI on hospital discharge [10]. The additional cost associated with these inadequate prescriptions was estimated to be 250,811 Australian dollars (AUD). Extrapolated across the entire country, translates into excess costs of AUD 22.4 million per year. In another study, Thomas et al. reviewed the pharmacy costs of more than 20,000 patients receiving PPI inappropriately after hospital admission over a four-year period and found that the inadequate global expense was approximately USD 3 million [14].
Our data confirm that stress ulcer prophylaxis is prescribed to almost all patients while in ICU. However, the rationale for this practice is increasingly challenged by recent literature. A recent network meta-analysis of randomised clinical trials concluded that compared with no prophylaxis, PPIs were associated with a 1.6% absolute risk reduction in gastrointestinal bleeding, but also with a 3% increase in pneumonia [15]. This observation largely relies on observational data, as discussed by Barletta et al. in a systematic review [16]. In addition, several studies have suggested an association between stress ulcer prophylaxis, C. difficile infections and PPIs [16, 17, 19, 20]. Finally, a recent multicentre, blinded and randomised study in ICU patients at risk of gastrointestinal bleeding failed to demonstrate a benefit of pantoprazole in terms of 90-day mortality. There was also no difference in terms of a composite outcome of new-onset pneumonia, CDI or acute myocardial infarction [21].
Hence, the indication for stress ulcer prophylaxis initiation should be weighed against its potential risks. In addition, it is of paramount importance to regularly review and challenge stress ulcer prophylaxis prescription throughout the ICU stay [22]. Our data suggest that in a modern tertiary ICU with protocoled indications, this is still not the case, and the therapy is inadequately maintained in a large number of patients all the way to hospital discharge. Some data have suggested that a pharmacist-driven medication review could significantly decrease this rate [11] and perhaps should be implemented in clinical practice. Indeed, such a medication review would probably improve protocol adherence and drug interaction identification and avoid common prescription errors.
This study has several strengths. First, it includes all consecutive patients admitted to our ICU during the study period. Second, a thorough evaluation of medical prescription on a day-to-day basis was conducted and detailed results are provided on a patient-day basis. Third, our intensive care unit is a large and multidisciplinary one with established guidelines for therapy initiation.
However, it also has several limitations worth discussing. First, it is a retrospective study and our findings might have been influenced by documentation bias. In addition, only a limited number of patients were included. However, given the magnitude of the effect observed, a chance finding appears unlikely and efforts were made to perform an exhaustive data collection. In addition, the characteristics of the patients included in the study are very similar to those observed in our general ICU population in terms of age, severity, admission diagnoses and length of stay. Hence, sample bias appears unlikely. Second, this is a single centre study and its external validity cannot be ascertained. However, our data is largely consistent with previously published data from other health care systems. Third, the indications for prescriptions, including an ICU stay longer than seven days, might be debatable and might have influenced the number of inadequate prescriptions. Nevertheless, this is highly unlikely to modify our conclusions. Finally, our evaluation of the financial impact of inadequate stress ulcer prophylaxis prescription after hospital discharge is largely hypothetical, and we can only provide a reasonable range of potential costs. A prospective study would be required to assess the real costs associated with inadequate post-discharge anti-acid therapy maintenance.
Stress ulcer prophylaxis was prescribed to the vast majority of patients admitted to the ICU. This prescription was inappropriate (not indicated or not prescribed while indicated) in almost two thirds of ICU patient-days. Moreover, this prescription was erroneously maintained in a very large number of patients both on the ICU and after hospital discharge. Prescribers should be reminded of the stress ulcer prophylaxis guidelines and the need for a daily re-evaluation, especially on ICU discharge.
Table S1: Indications for acid suppressant therapy.
Table S2: Summary of studies reporting data on stress ulcer prophylaxis adequacy and its prescription on ICU / hospital discharge.
Figure S1: Cost estimations.
Figure S2: Simulated costs for inpatients.
Figure S3: Simulated costs for outpatients.
The appendix is available as a separate file at https://smw.ch/article/doi/smw.2020.20322.
The study was supported by the research fund of the intensive care unit.
The authors declare that they have no conflicts of interest.
1 Cook DJ , Griffith LE , Walter SD , Guyatt GH , Meade MO , Heyland DK , et al.; Canadian Critical Care Trials Group. The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients. Crit Care. 2001;5(6):368–75. doi:.https://doi.org/10.1186/cc1071
2 Marik PE , Vasu T , Hirani A , Pachinburavan M . Stress ulcer prophylaxis in the new millennium: a systematic review and meta-analysis. Crit Care Med. 2010;38(11):2222–8. doi:.https://doi.org/10.1097/CCM.0b013e3181f17adf
3 Krag M , Perner A , Wetterslev J , Wise MP , Borthwick M , Bendel S , et al.; SUP-ICU co-authors. Prevalence and outcome of gastrointestinal bleeding and use of acid suppressants in acutely ill adult intensive care patients. Intensive Care Med. 2015;41(5):833–45. doi:.https://doi.org/10.1007/s00134-015-3725-1
4 Cook DJ , Witt LG , Cook RJ , Guyatt GH . Stress ulcer prophylaxis in the critically ill: a meta-analysis. Am J Med. 1991;91(5):519–27. doi:.https://doi.org/10.1016/0002-9343(91)90189-5
5 Rhodes A , Evans LE , Alhazzani W , Levy MM , Antonelli M , Ferrer R , et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43(3):304–77. doi:.https://doi.org/10.1007/s00134-017-4683-6
6 Farley KJ , Barned KL , Crozier TM . Inappropriate continuation of stress ulcer prophylaxis beyond the intensive care setting. Crit Care Resusc. 2013;15(2):147–51.
7 MacLaren R , Reynolds PM , Allen RR . Histamine-2 receptor antagonists vs proton pump inhibitors on gastrointestinal tract hemorrhage and infectious complications in the intensive care unit. JAMA Intern Med. 2014;174(4):564–74. doi:.https://doi.org/10.1001/jamainternmed.2013.14673
8 Charlot M , Grove EL , Hansen PR , Olesen JB , Ahlehoff O , Selmer C , et al. Proton pump inhibitor use and risk of adverse cardiovascular events in aspirin treated patients with first time myocardial infarction: nationwide propensity score matched study. BMJ. 2011;342(may11 1):d2690. doi:.https://doi.org/10.1136/bmj.d2690
9 Sehested TSG , Gerds TA , Fosbøl EL , Hansen PW , Charlot MG , Carlson N , et al. Long-term use of proton pump inhibitors, dose-response relationship and associated risk of ischemic stroke and myocardial infarction. J Intern Med. 2018;283(3):268–81. doi:.https://doi.org/10.1111/joim.12698
10 Tan B , Norman R , Litton E , Heath C , Hawkins DJ , Krishnamurthy R , et al. Incidence and cost of stress ulcer prophylaxis after discharge from the intensive care unit: a retrospective study. Crit Care Resusc. 2016;18(4):270–4.
11 Pavlov A , Muravyev R , Amoateng-Adjepong Y , Manthous CA . Inappropriate discharge on bronchodilators and acid-blocking medications after ICU admission: importance of medication reconciliation. Respir Care. 2014;59(10):1524–9. doi:.https://doi.org/10.4187/respcare.02913
12 Fumeaux T , Luca L . Top-9-liste de la SSMI: faire plus avec moins. Bull Med Suisses. 2017;40:1293–4.
13 Farrell CP , Mercogliano G , Kuntz CL . Overuse of stress ulcer prophylaxis in the critical care setting and beyond. J Crit Care. 2010;25(2):214–20. doi:.https://doi.org/10.1016/j.jcrc.2009.05.014
14 Thomas L , Culley EJ , Gladowski P , Goff V , Fong J , Marche SM . Longitudinal analysis of the costs associated with inpatient initiation and subsequent outpatient continuation of proton pump inhibitor therapy for stress ulcer prophylaxis in a large managed care organization. J Manag Care Pharm. 2010;16(2):122–9. doi:.https://doi.org/10.18553/jmcp.2010.16.2.122
15 Alhazzani W , Alshamsi F , Belley-Cote E , Heels-Ansdell D , Brignardello-Petersen R , Alquraini M , et al. Efficacy and safety of stress ulcer prophylaxis in critically ill patients: a network meta-analysis of randomized trials. Intensive Care Med. 2018;44(1):1–11. doi:.https://doi.org/10.1007/s00134-017-5005-8
16 Barletta JF , Bruno JJ , Buckley MS , Cook DJ . Stress Ulcer Prophylaxis. Crit Care Med. 2016;44(7):1395–405. doi:.https://doi.org/10.1097/CCM.0000000000001872
17 Marker S , Krag M , Møller MH . What’s new with stress ulcer prophylaxis in the ICU? Intensive Care Med. 2017;43(8):1132–4. doi:.https://doi.org/10.1007/s00134-017-4733-0
18 Bez C , Perrottet N , Zingg T , Leung Ki EL , Demartines N , Pannatier A . Stress ulcer prophylaxis in non-critically ill patients: a prospective evaluation of current practice in a general surgery department. J Eval Clin Pract. 2013;19(2):374–8. doi:.https://doi.org/10.1111/j.1365-2753.2012.01838.x
19 Huang HB , Jiang W , Wang CY , Qin HY , Du B . Stress ulcer prophylaxis in intensive care unit patients receiving enteral nutrition: a systematic review and meta-analysis. Crit Care. 2018;22(1):20. doi:.https://doi.org/10.1186/s13054-017-1937-1
20 Sridharan K , Sivaramakrishnan G , Gnanaraj J . Pharmacological interventions for stress ulcer prophylaxis in critically ill patients: a mixed treatment comparison network meta-analysis and a recursive cumulative meta-analysis. Expert Opin Pharmacother. 2018;19(2):151–8. doi:.https://doi.org/10.1080/14656566.2017.1419187
21 Krag M , Marker S , Perner A , Wetterslev J , Wise MP , Schefold JC , et al.; SUP-ICU trial group. Pantoprazole in Patients at Risk for Gastrointestinal Bleeding in the ICU. N Engl J Med. 2018;379(23):2199–208. doi:.https://doi.org/10.1056/NEJMoa1714919
22 Esteves M , Rollason V , Grosgurin O . [Proton pump inhibitors overprescription]. Rev Med Suisse. 2017;13(579):1782–6.
Contributed equally to the work
All authors read and approved the final manuscript and agree to be personally accountable for their contributions.
The study was supported by the research fund of the intensive care unit.
The authors declare that they have no conflicts of interest.