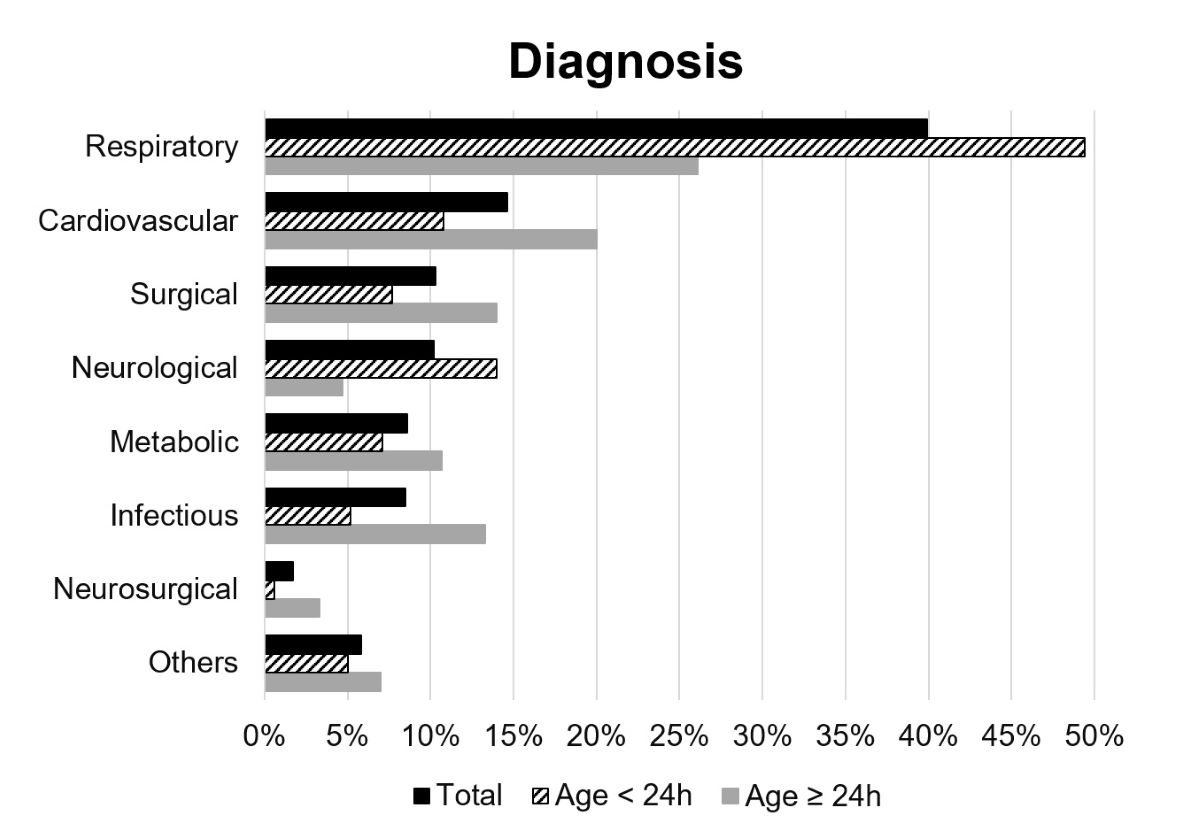
Figure 1 Medical problems requiring transport according to diagnosis. Only the main reason for transport was considered.
DOI: https://doi.org/10.4414/smw.2020.20308
Neonatal interfacility transport is an important part of regionalised perinatal care. It enables ill or preterm neonates to receive the best possible care from medical staff with an appropriate level of expertise. Although antenatal transfer to a perinatal centre is the preferred option when specialised neonatal care is anticipated, postnatal transports are inevitable [1, 2]. Therefore, a neonatal transport service is required to ensure transports for preterm and term neonates needing a higher level of care, as well as to transfer convalescent neonates to hospitals with lower levels of care. Transfers are therefore mainly performed by specialised neonatal transport teams [3].
Due to differences in demography and geography, models for organising neonatal care and transport vary between countries and regions [4–6]. In Canada neonatal transports are predominantly performed by dedicated hospital-based neonatal transport teams [5], while in the UK neonatal transport is mainly organised by unit-based neonatal transport teams and centralised transport services [4]. In Switzerland, three levels of neonatal care are defined by the Swiss Society of Neonatology: level I, a postnatal ward providing care for healthy neonates, level II, a neonatal care unit providing care to moderately ill neonates and equipped without (IIA) or with (IIB) noninvasive ventilation, and level III, a neonatal intensive care unit (NICU) [7]. Perinatal care and transfer are organised by nine networks representing different geographic regions and without a centralised transport service [8]. Therefore, neonatal transport is performed by individual neonatal units which provide hospital-based neonatal transport teams. Some of these perform only a few urgent transport runs, while others complete up to 300 transports per year [9]. The neonatal transport teams of the University Children’s Hospital Zurich are unit-based teams covering neonatal transfers in the region of Zurich and its surroundings. This represents the largest Swiss perinatal network, with around 17,000 births per year [10], covering an area of about 2000 km2 and including two level III NICUs/paediatric intensive care units (PICU), five level IIB neonatal care units and 13 level I centres [11, 12]. The University Children’s Hospital Zurich provides level III neonatal care on a PICU and level IIB neonatal care on a NICU due to logistical reasons. Therefore, its paediatric subspecialties include neonatal, surgical, cardiac, metabolic and neurological care, as well as treatment of critically ill neonates with multi-organ failure on the PICU and NICU.
Except for the Regional Perinatal Network of Lausanne [8], neonatal transport activities in Switzerland have not yet been quantitatively described. Therefore, a national database, as well as national guidelines on neonatal transport standards and quality metrics that allow benchmarking and improvements in transport quality are missing compared to other countries [13, 14]. The aims of this study were to explore transport activities by the neonatal transport teams of the University Children’s Hospital Zurich with a focus on time intervals during transport, to describe the characteristics of the transported neonates and to quantify the medical procedures performed during transport runs in order to identify opportunities for improvements in the organisation of the transports.
This study is a retrospective analysis of prospectively collected data on neonatal transports by the neonatal transport teams of the University Children’s Hospital Zurich between 1 January 2014 and 31 December 2018. Transfers performed within the perinatal network of Zurich, as well as transports throughout Switzerland and to neighbouring countries, were included. The transport runs were grouped into three categories: (1) urgent transfers, including transports of neonates that were hemodynamically unstable or in need of an immediate medical procedure performed by the neonatal transport teams, such as respiratory support or care with a higher level of expertise than provided at the referral hospital, (2) non-urgent transfers, including transports of haemodynamically stable neonates who were referred to other hospitals for further diagnostics or treatment without needing an immediate medical procedure performed by the neonatal transport teams, and (3) retransfers, including transports of convalescent neonates to hospitals closer to their parents’ home and referrals to other medical facilities due to a lack of capacity. The classification was determined at the time of transport demand according to vital parameters, diagnosis, need for medical procedures and level of neonatal care of the referral hospital. As there was no defined checklist, the classification also depended on the initial assessment of the doctor responding to the transport demand. For urgent and non-urgent transfers, referral hospitals activated the transport service whenever neonates needed a higher level of neonatal care than they provided.
Only transport runs concerning neonates with a corrected gestational age of up to 44 weeks and a weight less than 5 kg were included in this study. The medical problems causing transport demand were grouped according to the following categories: respiratory, cardiovascular, surgical, neurosurgical, neurological, metabolic, infectious, and other diseases. Only the main cause for transport was considered.
The neonatal transport teams of the University Children’s Hospital Zurich are available 24 hours a day all year round and are staffed by specially trained consultants (neonatologists and/or paediatric intensivists), fellows (paediatricians, neonatologists or paediatric intensivists in training) or assistant doctors (paediatricians in training) of the neonatology/paediatric intensive care team, and neonatology or paediatric intensive care nurses. The composition of the neonatal transport teams is determined by a specific protocol that defines three different patient groups. Group 1 includes haemodynamically unstable neonates who are or need to be intubated. These transports are performed by a consultant and an experienced neonatology or paediatric intensive care nurse. Group 2 includes haemodynamically stable neonates with respiratory support. These transports are performed by an experienced fellow or assistant doctor and a neonatology or paediatric intensive care nurse. Group 3 includes all other neonates and transports. These transfers are performed by a fellow or assistant doctor and a neonatology or paediatric intensive care nurse, or by a nurse only. At the University Children’s Hospital Zurich, a two-day training course is mandatory for all medical staff undertaking neonatal transports, and regular refresher courses are routine. As unit-based neonatal transport teams, transport staff are in-house around the clock but not dedicated, and therefore are responsible for bedside patient care as well as for attending to transport demands. During the study period, a specially equipped ambulance (neonatal transports with incubator only) and a driver were based at the University Children’s Hospital Zurich around the clock to accomplish ground transport. For air transport, a rescue helicopter (Rega, Dübendorf, Switzerland) had to be called.
To identify the medical procedures performed during transports, interventions were assessed separately for the neonatal transport teams and the referral care team.
The transport runs were subdivided into four time intervals to assess transport times: (1) preparation time, defined as the interval between the emergency call and the departure of the neonatal transport teams, (2) traffic duration time I, defined as the interval between the departure of the neonatal transport teams from the University Children’s Hospital Zurich and their arrival at the referral hospital, (3) stabilisation time, defined as the interval between arrival at the referral hospital and departure from the referral hospital, (4) traffic duration time II, defined as the interval between departure from the referral hospital and arrival at the admission hospital.
Ethical approval for this study was waived by the ethics committee of the canton of Zurich (KEK ZH Nr. 2019-00996).
Information was collected from written transport forms entered into the electronic database that systematically documented administrative data, the times of different phases of transport, data about transported neonates and the medical procedures performed during transport runs. To complete the data, computerised transport reports written by a member of the neonatal transport team were studied. For most transports, a written registration form including details of the transport demands was available. This form was analysed to gain information about the referral hospital as well as the reason for transport. Diagnoses were extracted from the registration form, thus giving the medical problem which led the referral hospital to make the transport demand. If no registration form was available, diagnoses were extracted from the neonate’s medical chart. Furthermore, information regarding pregnancy and delivery, length of stay and place of discharge was acquired from the neonate’s medical chart and the electronic medical database. Numbers of and reasons for refusals of transports were extracted from an Excel file generated by the members of the neonatal transport teams.
Data analysis of the study items was performed by applying descriptive and explorative statistics using frequencies with percentages and measures of central tendency and dispersion. Transport data were assessed separately for urgent, non-urgent and retransfers. All analyses were performed using IBM® SPSS® Statistics 25 for Microsoft®.
During the study period, 1110 transport runs, including 883 (79.5%) urgent, 105 (9.5%) non-urgent and 122 (11.0%) retransfers, were performed by the neonatal transport teams of the University Children’s Hospital Zurich, resulting in an average of 0.6 transfers per day. A total of 1110 transport runs for approximately 85,000 deliveries in the district served over a period of five years shows that neonatal transport by our neonatal transport teams was required in 1.3% of deliveries. A total of 47 hospitals were served, with a median distance of 21 km (range 1.8–727), and 89.7% of the transfers were completed within the perinatal network of Zurich. The transport runs involved 1050 neonates; 58 (5.5%) were transported twice and 1 (0.1%) was transported three times. Over the study period, 194 transport runs were refused due to a lack of cots or unavailability of the neonatal transport teams, and these were excluded from further analysis. Overall, 55.7% of the declined transports concerned neonates on their first day of life, and the most common reason for transport demand was respiratory distress (45.4%), followed by metabolic (15.5%) and neurological diseases (7.2%). Of the declined transport demands, 123 (63.4%) were from level I centres, 47 (24.2%) were from level IIB centres and 18 (9.3%) were from level III centres. For six cases (3.1%) data was missing. In the case of a lack of cots or unavailability of our neonatal transport teams, transfers were performed by out of region teams, who admitted the neonates to their corresponding sites.
Ground transport accounted for 90.7% and air transport for 9.1% of the cases. On two occasions (0.2%) both ground and air transport were used.
In 67.0% of the urgent cases, transport demand was made within 24 hours after birth and on seven occasions (0.8%) transport demand was made before birth. For non-urgent (61.0%) and retransfers (87.7%), transport demand was predominantly made more than 24 hours postnatally. During the study period there were 667 (60.1%) transports from level I, 4 (0.4%) transports from level IIA, 396 (35.7%) transports from level IIB and 39 (3.5%) transports from level III centres. Most neonates were handed over to the neonatal transport teams in the delivery room (42.8%) for urgent transfers, in the postnatal ward (58.1%) for non-urgent transfers and in the PICU (53.3%) for retransfers. Overall, transport runs led to 877 (79.0%) admissions to the University Children’s Hospital Zurich. Additionally, 222 (20.0%) transports led to admissions to other hospitals: 10 (0.9%) admissions to level I centres, 1 (0.1%) admission to a level IIA centre, 99 (8.9%) admissions to level IIB centres, 107 (9.6%) admissions to level III centres and 5 (0.5%) admissions to foreign hospitals. Neonates were not transferred on 11 (1.0%) occasions: due to death at the delivery room in eight cases, refusal of parents in two cases and total recovery in one case. The admission ward was mainly a PICU or an NICU (60.1%) for urgent transfers, while most neonates from non-urgent (82.9%) and retransfers (77.0%) were admitted to a neonatal care unit.
Overall, 59.1% of the neonates were transported within the first 24 hours after birth, and these had a median age of 4 hours (range 0–23). The remaining 40.9% were aged older than 1 day and had a median age of 3 days (range 1–138) at the time of transfer. Table 1 shows a complete description of the sample.
Table 1 Sample characteristics.
| Characteristics |
Total
N = 1050 (100%) |
Age <24h
n = 621 (59.1%) |
Age ≥24h
n = 429 (40.9%) |
|---|---|---|---|
| Sex, n (%) | |||
| Female | 443 (42.2) | 266 (42.8) | 177 (41.3) |
| Male | 607 (57.8) | 355 (57.2) | 252 (58.7) |
| Corrected gestational age, n (%) | |||
| ≥37 0/7 weeks | 816 (77.7) | 465 (74.9) | 351 (81.8) |
| Between 32 0/7 and 36 6/7 weeks | 203 (19.3) | 138 (22.2) | 65 (15.2) |
| <32 0/7 weeks | 8 (0.8) | 3 (0.5) | 5 (1.2) |
| Not known | 23 (2.2) | 15 (2.4) | 8 (1.9) |
| Weight at admission, n (%) | |||
| ≥2500 g | 855 (81.4) | 502 (80.8) | 353 (82.3) |
| <2500 g | 167 (15.9) | 100 (16.1) | 67 (15.6) |
| Median (range) | 3168g (500–4950) | 3135g (500–4950) | 3200g (900–4900) |
| Not known | 28 (2.7) | 19 (3.1) | 9 (2.1) |
| Pregnancy, n (%) | |||
| Single | 962 (91.6) | 578 (93.1) | 384 (89.5) |
| Twins | 67 (6.4) | 35 (5.6) | 32 (7.5) |
| Not known | 21 (2.0) | 8 (1.3) | 13 (3.0) |
| Mode of delivery, n (%) | |||
| Vaginal | 408 (38.9) | 231 (37.2) | 177 (41.3) |
| Caesarean section | 481 (45.8) | 290 (46.7) | 191 (44.5) |
| Vacuum/forceps extraction | 138 (13.1) | 92 (14.8) | 46 (10.7) |
| Not known | 23 (2.2) | 8 (1.3) | 15 (3.5) |
| APGAR 5′, n (%) | |||
| <5 | 84 (13.5) | ||
| Not known | 31 (5.0) | ||
| Cord pH, n (%) | |||
| <7.15 | 193 (36.1) | ||
| Not known | 86 (13.8) |
At the time of transport demand, 34 (3.2%) neonates were undergoing cardiopulmonary resuscitation (CPR) and 103 (9.8%) were stabilised, having been resuscitated. The most common reason for transport demand was respiratory distress (39.9%). All medical reasons for transport are listed according to diagnosis groups in figure 1.
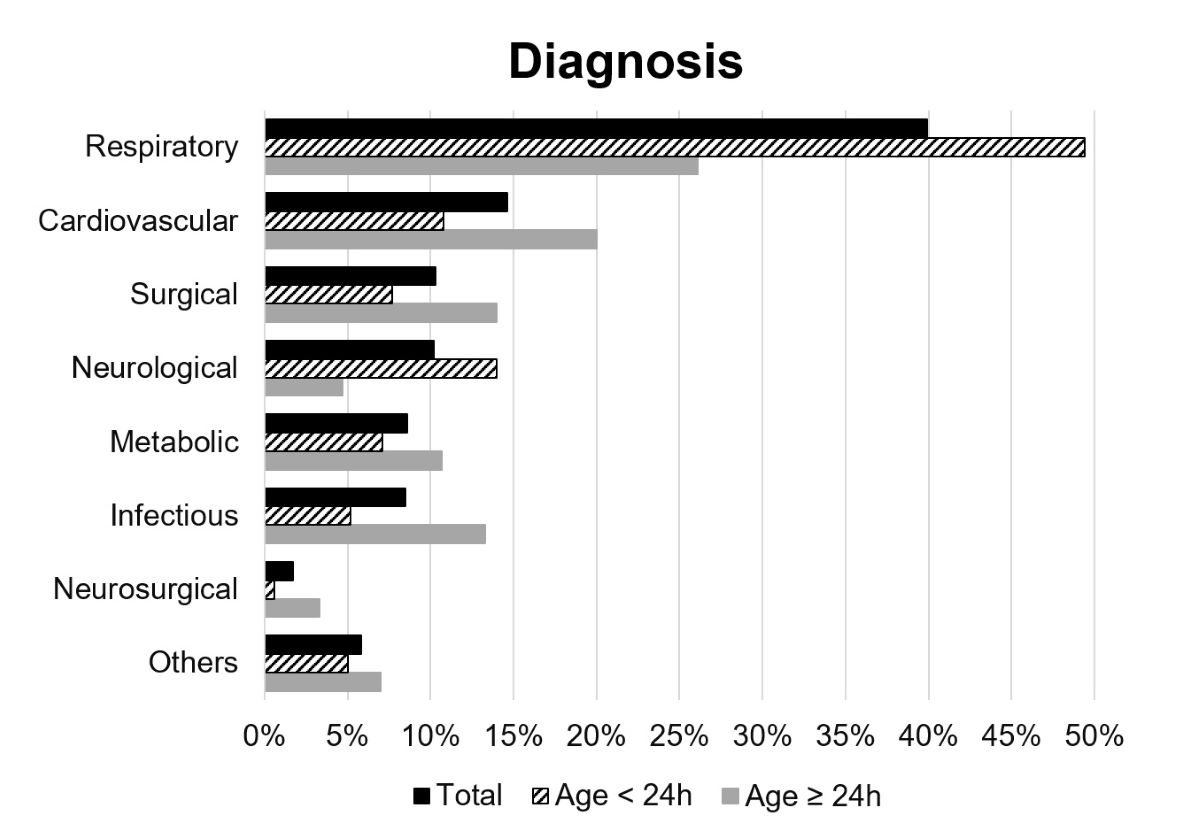
Figure 1 Medical problems requiring transport according to diagnosis. Only the main reason for transport was considered.
Of the 1050 patients, 870 (82.9%) were primarily admitted to the University Children’s Hospital Zurich and stayed there for a median of 7 days (range 0–376). They were mainly discharged home (61.8%), while 16.0% were referred to neonatal or paediatric wards of other hospitals, 10.8% to postnatal wards and 7.8% to paediatric wards of the University Children’s Hospital Zurich for further treatment. Another 3.4% died during hospitalisation, among them 4.3% of the neonates transported on their first day of life and 2.1% of the neonates transported after their first day of life.
All transport team members were bedside staff and not dedicated transport team members. Overall, 44.4% of the transport runs were performed by assistant doctors, 36.2% by consultants, 10.6% by nurses only and 8.8% by fellows.
All medical procedures performed during transport are listed in figure 2. Most of the interventions performed by the neonatal transport teams during transport runs addressed peripheral intravenous line placement (41.8%) and feeding tube placement (41.8%). Endotracheal intubation with mechanical ventilation was needed in 15.0% (performed by the neonatal transport teams in 8.0%) and continuous positive airway pressure (CPAP) with nasal cannula in 20.0% (performed by the neonatal transport teams in 9.5%) of all cases. During one (0.1%) urgent transport run, the drainage of a pneumothorax was necessary. Other medical procedures performed by the referral care team included peripheral intravenous line placement in 35.8%, umbilical intravenous line placement in 8.9%, feeding tube placement in 23.9%, administration of antibiotics in 10.4%, administration of surfactant in 0.8%, continuous infusion of prostaglandins in 3.2% and of catecholamines in 4.2% of cases.
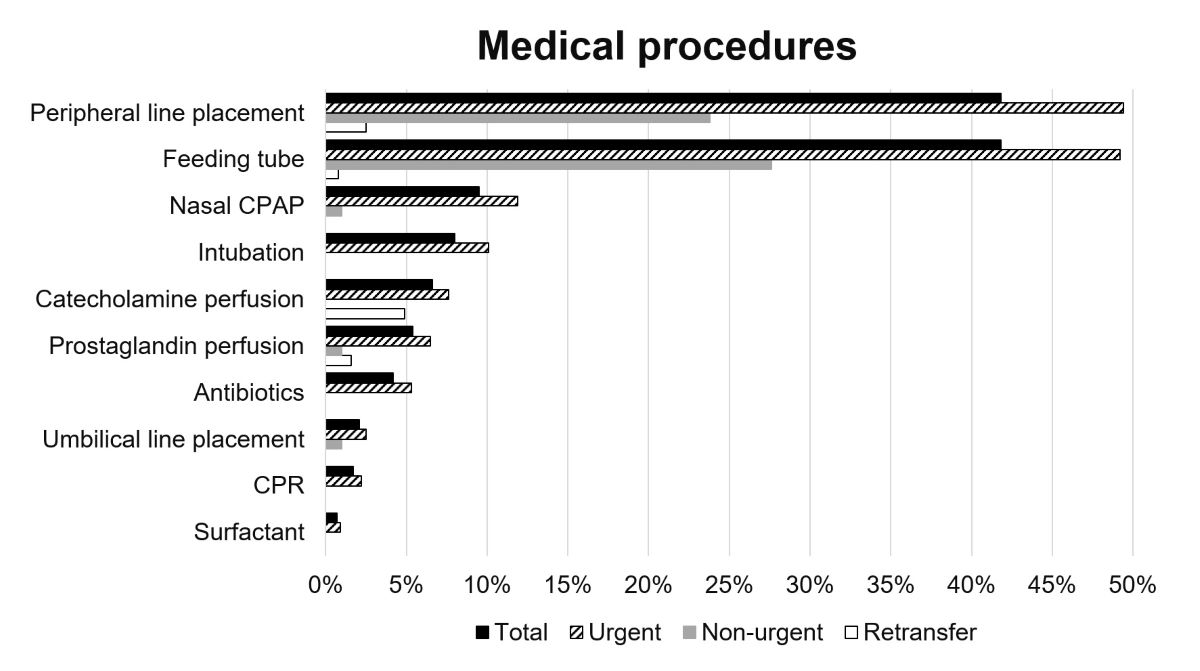
Figure 2 Medical procedures performed by neonatal transport teams during transport runs. CPAP = continuous positive airway pressure; CPR = cardiopulmonary resuscitation
A full dataset on timing was available for 773 (87.5%) out of 883 urgent transport runs (including air and ground transport). The median times and ranges of the four time intervals are shown in figure 3. The median preparation interval was shorter for ground transport (median 35 min, range 8–225) than for air transport (median 50 min, range 20–260). For transfers of neonates undergoing CPR at the time of transport demand, preparation time was 18 min (range 10–45). The median distance of all urgent transfers to the referral hospital was 20.4 km (range 1.8–225.9) and the median distance to the admission hospital was 19.5 km (range 1.3–225.9). For non-urgent transfers, the preparation interval was longer (median 60 min, range 15–447), while the stabilisation interval was shorter (median 35 min, range 5–78).
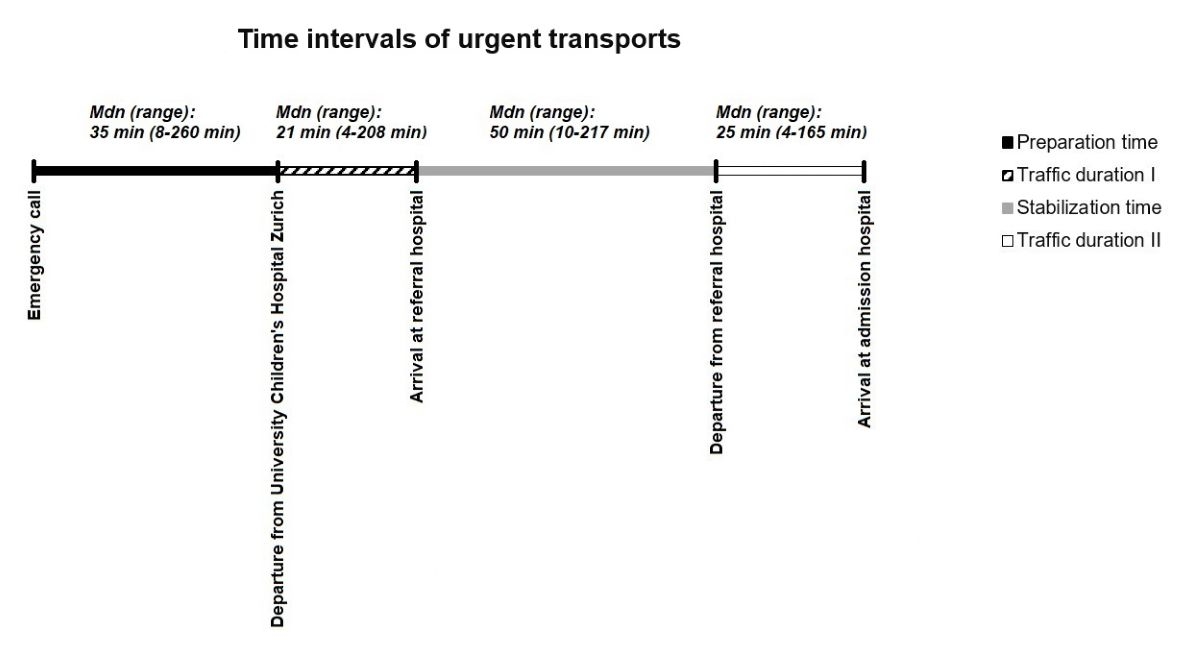
Figure 3 Time for intervals of urgent transfers.
The weekly distribution shows that the number of transports was similar for every day (fig. 4). The most common time for transports was between 14:00 and 16:00 for urgent transfers (13.9%) and retransfers (28.7%), while the most common time for non-urgent transfers was between 10:00 and 12:00 (23.8%) (fig. 4).

Figure 4 Weekly and daily distribution of three categories of transport runs.
This study showed that transport runs by the neonatal transport teams of the University Children’s Hospital Zurich were predominantly urgent transfers, whereas in other settings elective or retransfers were more frequent [8, 15]. Nevertheless, the severity of the illness of the transported neonates was rather low according to the medical procedures performed by the neonatal transport teams, the admission rate to the PICU or NICU and the death rate. As most transports were from level I centres with limited expertise in neonatal care and usually a lack of in-house neonatologists or paediatricians, the neonatal transport teams of the University Children’s Hospital Zurich were the first responders for moderately as well as seriously ill neonates. Therefore, even neonates with mild diseases often required an urgent transfer because they needed either a higher level of expertise or intensive care medical procedures. The number of urgent transfers performed per year is among the highest in Switzerland, comparable to the number found for the Regional Perinatal Network of Lausanne [8, 9]. Therefore, a dedicated, highly efficient neonatal transport system staffed by members with training in neonatal transport and expertise in handling neonatal emergencies, including advanced neonatal resuscitation, is required to guarantee the best possible care for ill neonates. Additionally, clear pathways and protocols for activating the transport service should be established for the referral hospitals to increase its efficacy. Furthermore, the referral care team should receive regular simulation training on caring for the neonates before transport, including the performance of simple medical procedures. The weekly and daily distribution of transports emphasises its unpredictability and the need for a transport system that is available 24 hours a day all year round, as shown elsewhere [8]. For unit-based neonatal transport teams, this might be especially challenging on weekends and during the night, as the number of staff on the neonatal/intensive care unit is reduced.
Overall, 1.3% of the neonates born in our service area required neonatal transport by the neonatal transport teams of the University Children’s Hospital Zurich. This overall incidence of the need for postnatal transport is in agreement with previous studies. However, the transported neonates in this study included fewer preterm neonates and more neonates aged older than one day at the time of transfer compared to other studies [8, 15]. Due to the local infrastructure and patient allocation, the University Children’s Hospital Zurich does not normally provide care for preterm neonates less than 32 weeks of gestational age except for in special situations, for example if surgery is needed. Whereas in other transport settings the reasons for transport were mainly respiratory distress [8, 16], only 39.9% were referred due to respiratory distress in this study, indicating a more heterogeneous cohort. A possible explanation is the lower number of preterm neonates compared to the other publications. Additionally, the paediatric subspecialties of the University Children’s Hospital Zurich include neonatal, surgical, cardiac, metabolic, neurological and intensive care, which might have led to a more heterogeneous cohort. The heterogeneity of the transported neonates regarding their diagnoses requires profound knowledge and should be considered in the training of neonatal transport team staff.
The interventions performed during transport mostly addressed simple medical procedures such as peripheral intravenous line placement and feeding tube placement. Nevertheless, the neonatal transport team staff regularly needed to perform intensive care interventions such as endotracheal intubation and pleural drainage. Because generally more intensive care interventions are required in transfers of neonates compared to other populations, members of the neonatal transport teams need to be able to perform these interventions at any time [17]. For this reason, specific simulation training using validated assessment tools and frequent refresher courses are recommended to ensure the maintenance of these competencies [17]. Additionally, appropriate administration of drugs such as antibiotics, catecholamines, surfactant and prostaglandin is crucial to providing optimal care [18–20]. In order to guarantee a high quality of care during transports, quality improvement strategies including national guidelines on safe, effective, efficient and patient-centred neonatal transports should be implemented. Additionally, the performance of the neonatal transport teams should be assessed using a reliable and objective score based on changes in the neonatal condition during transport. In California, a score to estimate the quality of neonatal transport has been developed using changes in the Transport Risk Index of Physiologic Stability (TRIPS) score to identify benchmark teams with the least deterioration [21, 22]. Furthermore, complications that occur on transport runs should be reported and discussed in training [13].
To provide safe and efficient care to transported neonates, time intervals during transport, and especially the time between the emergency call and arrival at the neonate’s bedside, should be as short as possible, as there is an association between transport duration and increased neonatal mortality [23]. According to the time goals of most Canadian neonatal transport teams and the standards set in the United States of America, neonatal transport teams should ideally be able to depart within 30 min after the emergency call was made [5, 24]. This is especially important in Switzerland due to the high number of level I centres with limited expertise in neonatal intensive care. In the UK, on the other hand, a preparation interval of 60 min was set as a benchmark for critical transports [25], as most local units provide neonatal intensive care [15]. For the neonatal transport teams of the University Children’s Hospital Zurich, the preparation interval was longer than 30 min for ground and air transport, even though an ambulance and a driver were based at the hospital. A possible explanation is that the staff of the neonatal transport teams are not dedicated to transport activities, but had to hand over their patients to other members of the neonatal/intensive care unit after transport demand. Additionally, the absence of a centralised transfer number at the University Children’s Hospital Zurich sometimes caused delays, as multiple phones calls were necessary to check on staffing, as well as bed availability. For air transport, preparation time was longer because the helicopters were not hospital-based, had to be remodelled to accommodate an incubator, and staff had to wait for the helicopter’s arrival at the University Children’s Hospital Zurich. In the UK, the introduction of a centralised neonatal transfer service has led to a significant improvement in reaction time [26]. However, centralised neonatal transport teams have not yet been introduced in Switzerland due to economic reasons; it is assumed that 1000 neonatal transports per year are necessary to guarantee bearable costs [9]. Nevertheless, processes should be defined to shorten preparation times. The big range of preparation times reflects a non-standardised approach prior to departure. A first step could be a centralised transfer number which allocates the teams for transports. Neonatal transport teams in California reported that having a transfer centre with a centralised number at the receiving hospital helped them to have adequate transfer information and to reduce preparation time [14]. In addition, neonatal transport simulations in SimLab will be started in order to improve processes affecting the reaction times, the teamwork and the training of the staff. Finally, the introduction of dedicated neonatal transport teams should be considered to decrease preparation times consistently, as unit-based neonatal transport teams take staff away from in-house patient care, delay departure and lack flexibility [14]. Further research is needed to quantify the costs of dedicated neonatal transport teams or centralised neonatal transfer services, and the number of transports needed to justify these costs in Switzerland. A study in Italy concluded that between 200 and 350 transports per year are required for financial viability and to acquire and maintain appropriate skill levels among neonatal transport team staff [27].
The stabilisation time of urgent transfers was similar to that found in other studies [8, 16]. A Canadian study showed that stabilisation time is mainly increased when neonatal transport team staff need to perform intensive care interventions [28]. Therefore, the stabilisation time might be decreased if intensive care interventions such as endotracheal intubation are performed by the referral care team before the arrival of the neonatal transport teams [28]. However, in our setting, with short distances, it is more important that the referral care teams are able to perform basic neonatal resuscitation of good quality.
This study quantitatively describes the transport activities of the neonatal transport teams of the University Children’s Hospital Zurich over a five-year period which included 1110 transport runs. As data on neonatal transport in Switzerland is sparse, the study adds substantial knowledge to that domain, helping the establishment of benchmarks to control the quality and efficacy of neonatal transports. Nevertheless, this study has several limitations. Data was incomplete for various transport runs, especially when the transfer did not include the University Children’s Hospital Zurich as the referral or admission hospital. Furthermore, registration and transport forms were filled in less accurately by some members of the neonatal transport teams than by others. Finally, as the study only explored the transport runs of a single centre in a defined setting, its findings’ generalisability to other neonatal transport teams is limited. As this is one of only two surveys describing neonatal transport activities in Switzerland, further studies are needed to assess its quality and efficacy.
The high proportion of urgent transfers emphasises the need for an efficient neonatal transport system available 24 hours a day all year round, and for dedicated neonatal transport teams staffed by members with training in neonatal transport and expertise in handling neonatal emergencies. To provide the best possible care to the vulnerable neonates, the heterogeneous nature of the cohort of transported neonates regarding the diagnoses transport demand was made for and the medical procedures performed during transport should be considered in simulation training of neonatal transport team staff. Furthermore, processes to improve preparation time should be defined and implemented in order to reduce it to less than 30 min so as to guarantee efficient care. National guidelines on the standard of neonatal transport and quality metrics also need to be established in Switzerland in order to set benchmarks and to improve the quality of the transports.
The authors would like to acknowledge Maja Hug, who helped to establish the transport courses together with Vera Bernet. We also thank the team at the University Children’s Hospital Zurich, which organises the neonatal transport courses, and all members of the neonatology/paediatric intensive care team for conducting the transports.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Messner H . Neonatal transport: a review of the current evidence. Early Hum Dev. 2011;87(Suppl 1):S77. doi:.https://doi.org/10.1016/j.earlhumdev.2011.01.018
2 Hohlagschwandtner M , Husslein P , Klebermass K , Weninger M , Nardi A , Langer M . Perinatal mortality and morbidity. Comparison between maternal transport, neonatal transport and inpatient antenatal treatment. Arch Gynecol Obstet. 2001;265(3):113–8. doi:.https://doi.org/10.1007/s004040100197
3 Fenton AC , Leslie A . Who should staff neonatal transport teams? Early Hum Dev. 2009;85(8):487–90. doi:.https://doi.org/10.1016/j.earlhumdev.2009.05.006
4 Fenton AC , Leslie A . The state of neonatal transport services in the UK. Arch Dis Child Fetal Neonatal Ed. 2012;97(6):F477–81. doi:.https://doi.org/10.1136/archdischild-2011-300573
5 Soliman Y , Paul R , Pearson K , Alshaikh B , Thomas S , Yusuf K . Neonatal transport services, a cross-sectional study. J Matern Fetal Neonatal Med. 2019;1–6. doi:.https://doi.org/10.1080/14767058.2019.1618823
6 Gente M , Aufieri R , Agostino R , Fedeli T , Calevo MG , Massirio P , et al.; Neonatal Transport Study Group of the Italian Society of Neonatology (SIN). Nationwide survey of neonatal transportation practices in Italy. Ital J Pediatr. 2019;45(1):51. doi:.https://doi.org/10.1186/s13052-019-0640-z
7Swiss Society of Neonatology. Standards for Levels of Neonatal Care in Switzerland. https://www.neonet.ch/application/files/7715/6880/5956/Level_Standards_2019-03-14.pdf. Published 14 March 2019.
8 McEvoy CG , Descloux E , Schuler Barazzoni M , Stadelmann Diaw C , Tolsa J-F , Roth-Kleiner M . Evaluation of Neonatal Transport in Western Switzerland: A Model of Perinatal Regionalization. Clin Med Insights Pediatr. 2017;11:1179556517709021. doi:.https://doi.org/10.1177/1179556517709021
9 Roth-Kleiner M , Berger TM , Arlettaz Mieth R . Neue Herausforderungen für die regionale Zusammenarbeit. Swiss Med Forum. 2019;19(2526):408–10. doi:.https://doi.org/10.4414/smf.2019.08267
10Swiss Federal Statistical Office. Lebendgeburten nach Kanton und Staatsangehörigkeitskategorie der Mutter, 1970-2018. Neuchâtel: Federal Statistical Office. 2019.
11Swiss Society of Neonatology. Accredited neonatology units. https://www.neonet.ch/unit-accreditation/accredited-neonatology-units. (Accessed 2019 December 18)
12Kanton Zürich Regierungsrat. Zürcher Spitalliste 2012 Akutsomatik (Version 2018.1; ab 1. Januar 2018). Zürich. 2018.
13 Lee KS . Neonatal transport metrics and quality improvement in a regional transport service. Transl Pediatr. 2019;8(3):233–45. doi:.https://doi.org/10.21037/tp.2019.07.04
14 Akula VP , Hedli LC , Van Meurs K , Gould JB , Peiyi K , Lee HC . Neonatal transport in California: findings from a qualitative investigation. J Perinatol. 2020;40(3):394–403. doi:.https://doi.org/10.1038/s41372-019-0409-7
15 Kempley ST , Sinha AK ; Thames Regional Perinatal Group. Census of neonatal transfers in London and the South East of England. Arch Dis Child Fetal Neonatal Ed. 2004;89(6):F521–6. doi:.https://doi.org/10.1136/adc.2003.029017
16 Sampaio TZAL , Wilson M , Aubertin C , Redpath S . Diagnosis Discordance and Neonatal Transport: A Single-Center Retrospective Chart Review. Am J Perinatol. 2019;36(5):522–5. doi:.https://doi.org/10.1055/s-0038-1669906
17 Whyte HE , Jefferies AL ; Canadian Paediatric Society, Fetus and Newborn Committee. The interfacility transport of critically ill newborns. Paediatr Child Health. 2015;20(5):265–9. doi:.https://doi.org/10.1093/pch/20.5.265
18 Shivananda S , Kirsh J , Whyte HE , Muthalally K , McNamara PJ . Accuracy of clinical diagnosis and decision to commence intravenous prostaglandin E1 in neonates presenting with hypoxemia in a transport setting. J Crit Care. 2010;25(1):174.e1–9. doi:.https://doi.org/10.1016/j.jcrc.2009.04.005
19 Sumpton JE , Kronick JB . Medication use during neonatal and pediatric critical care transport. Can J Hosp Pharm. 1991;44(3):153–6, 166.
20 McNamara PJ , Mak W , Whyte HE . Dedicated neonatal retrieval teams improve delivery room resuscitation of outborn premature infants. J Perinatol. 2005;25(5):309–14. doi:.https://doi.org/10.1038/sj.jp.7211263
21 Gould JB , Danielsen BH , Bollman L , Hackel A , Murphy B . Estimating the quality of neonatal transport in California. J Perinatol. 2013;33(12):964–70. doi:.https://doi.org/10.1038/jp.2013.57
22 Lee SK , Zupancic JA , Pendray M , Thiessen P , Schmidt B , Whyte R , et al.; Canadian Neonatal Network. Transport risk index of physiologic stability: a practical system for assessing infant transport care. J Pediatr. 2001;139(2):220–6. doi:.https://doi.org/10.1067/mpd.2001.115576
23 Mori R , Fujimura M , Shiraishi J , Evans B , Corkett M , Negishi H , et al. Duration of inter-facility neonatal transport and neonatal mortality: systematic review and cohort study. Pediatr Int. 2007;49(4):452–8. doi:.https://doi.org/10.1111/j.1442-200X.2007.02393.x
24Taskforce on interhospital transport, American Academy of Pediatrics. Guidelines for air and ground transport on neonatal and pediatric patients, 2nd ed. Elk Grove Village: American Academy of Pediatrics; 1999.
25Devon C, Jackson A. NTG Annual Transport Data.2019. http://ukntg.net/wp-content/uploads/2020/01/2019-NTG-data-report.pdf. Published January 2020.
26 Kempley ST , Baki Y , Hayter G , Ratnavel N , Cavazzoni E , Reyes T ; Thames Regional Perinatal Group; Neonatal Transfer Service for London, Kent, Surrey and Sussex. Effect of a centralised transfer service on characteristics of inter-hospital neonatal transfers. Arch Dis Child Fetal Neonatal Ed. 2007;92(3):F185–8. doi:.https://doi.org/10.1136/adc.2006.106047
27 Bellini C , Pasquarella M , Ramenghi LA , Ambrosino D , Sciomachen AF . Evaluation of neonatal transport in a European country shows that regional provision is not cost-effective or sustainable and needs to be re-organised. Acta Paediatr. 2018;107(1):57–62. doi:.https://doi.org/10.1111/apa.14084
28 Chen P , Macnab AJ , Sun C . Effect of transport team interventions on stabilization time in neonatal and pediatric interfacility transports. Air Med J. 2005;24(6):244–7. doi:.https://doi.org/10.1016/j.amj.2005.08.003
Contributed equally
No financial support and no other potential conflict of interest relevant to this article was reported.