Obesity, inflammation and COVID-19
DOI: https://doi.org/10.4414/smw.2020.20349
Solongevity Research, Scientific Director, R&D,
Obesity, inflammation and COVID-19
The most recent statistics from the United States and France highlight an important risk factor for the development of severe forms of COVID-19: obesity. We know the reason for this: obesity generates a chronic asymptomatic inflammatory state that favours an exaggerated inflammatory response of the immune system to the virus, which is the basis of the severe forms of COVID-19. Bad news? Not necessarily: it is enough to lose weight to reduce the impact of the virus on our organism.
It is summer and many of us worry that if we manage to get to a beach, we may not be able to fit into our bathing suits. After months of sedentary working life our body has accumulated excess calories and transformed them into adipose tissue. If the problem were only the appearance of the waist we could easily console ourselves and try to reduce it with some nice swims and, if possible, eating a little less.
But autumn, with the possible return of the virus, could bring us bad surprises. Two recent studies, one French [1] and one American [2], have shown that obesity is an important risk factor for the development of severe forms of COVID-19. And this is regardless of the disease most frequently associated with obesity: diabetes. In other words, even a “healthy” obese person is at risk of severe COVID-19. In the case of the French research, the results show that the frequency of obesity in hospitalised patients with severe forms of COVID-19 is 25%, whereas in the normal adult population it is 12%. The American data are even more significant and the reason is very simple: in the United States 40% of the population is obese. In Italy we can try to reassure ourselves with a comparatively “modest” 20%. The high percentage of obese people in the United States is probably a reason for their significantly lower average age of patients with COVID-19.
Before we go any further, let’s clarify how to figure out if we’re obese. A somewhat rough way is to measure body mass index. You can find it on Google: you will see a calculation window where you can enter the weight and height: from 20 to 25 kg/m2 we are normal weight, from 26 to 29 kg/m2we are overweight and from 30 kg/m2 and above we are obese. If the result indicates a problem, it is better to ask a doctor for a more thorough clinical evaluation. It is important to know how fat is distributed in our body; in particular, it is important to assess how much “visceral” fat we have, that is, what accumulates in the abdomen. To calculate this, all you need to do is measure the waist and perform a bioelectrical impedance (BIA) test. We will soon see why visceral fat is so important.
First let’s come to the reason for this association between obesity and COVID-19. The reasons are numerous. The first and most obvious is that obesity reduces diaphragm excursion and has a strong impact on the ability to ventilate. When the virus hits the lungs, you need to be very prepared to breathe strongly, because viral pneumonia reduces the ability of the lung to perform gaseous exchanges. A fundamental rule in the prevention of COVID-19 is to do breathing exercises to increase the strength of your diaphragm and chest muscles and increase your ventilatory capacity.
As I had the opportunity to share in my article of July 9 [3], the research of Andrea Cossarizza’s group in Modena has clearly shown that when the disease progresses towards its most severe forms, a real storm in the immune system is triggered, in which the molecules that regulate its functioning, cytokines, create a friendly fire between the cells of the system that damages the lung and all the other tissues that are attacked by the virus. We still don’t know exactly what triggers this storm. Surely the virus is putting its own spin on it. When it enters the cells, it manages with a couple of moves to block the defences of innate immunity (especially a class of very important molecules called interferons) and to activate all the cytokines that have a normal function: to activate the inflammatory response.
Mind you, inflammation in itself is a good thing because it can limit, at least initially, the spread of the virus. The problem with COVID-19 is the massive inflammation that results because the cells exaggerate their response.
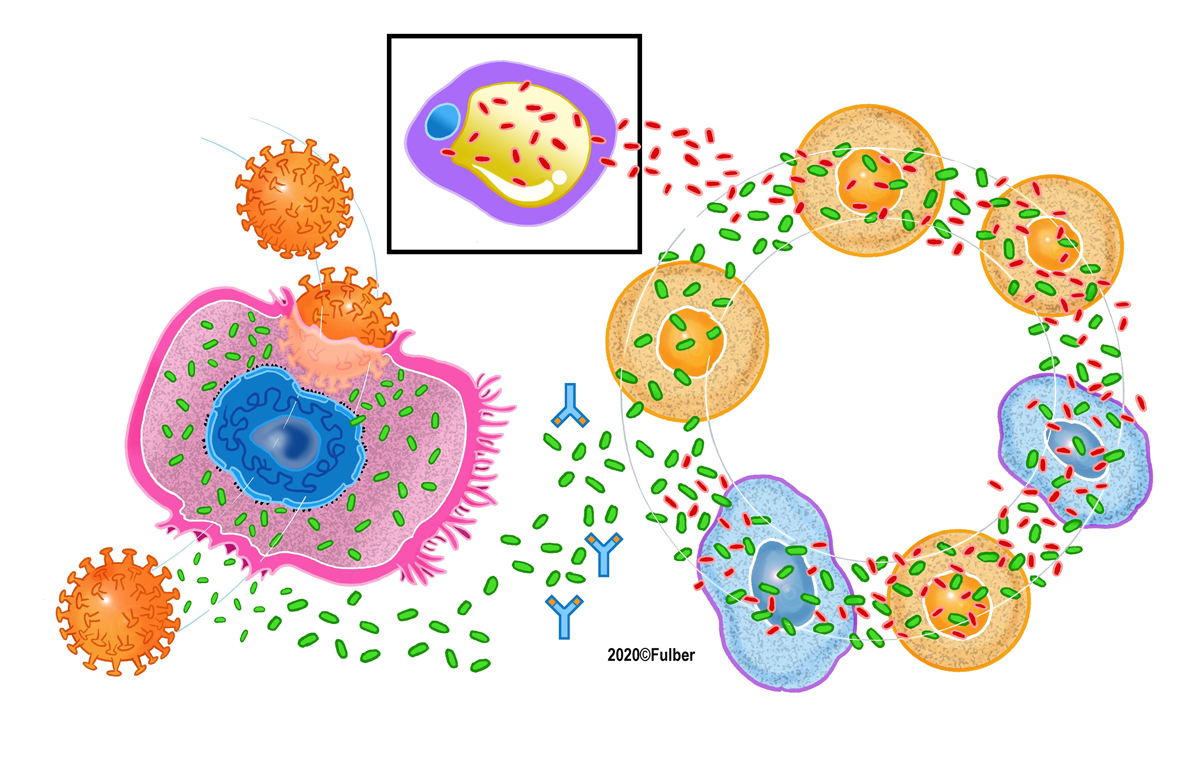
Figure 1 highlights what happens: when the virus enters the cell, the cell reacts by producing a large amount of inflammatory cytokines that trigger a vortex of reactions between the various cells of the system: the cytokine storm.
At this point you might ask me: what does obesity have to do with it? It’s very simple. Adipose tissue, and in particular its cells called adipocytes, is a strong producer of inflammatory cytokines, the leading player of the immune system. Particularly effective in this is the adipose tissue that accumulates in the abdomen, the visceral fat (hence the importance of its evaluation).
For years now we have known that adipocytes produce molecules called “adipokines”, which are nothing but cytokines specialised in doing damage to our body because they create a state of chronic inflammation that over time and whilst we are unaware, damages all tissues and, last but not least, creates the conditions for the onset of diabetes [4].
Now let’s imagine the three components of the perverse game that is unleashed in COVID-19: the cells of the lung (lung alveolar cells) that are attacked by the virus, the lymphocytes of the immune system and adipocytes. The lung alveolar cells, once infected, produce inflammatory cytokines that trigger the reaction of the lymphocytes; in the meantime the adipocytes add their adipokines that aggravate the situation. You can find them at the top of figure 1. Result: what could be a normal inflammatory response turns into a cytokine storm because there are too many cytokines and adipokines.
In a past article, I described how research has allowed the identification of drugs that can block this phenomenon [3]. That’s great news. But please do not count on those drugs as the solution to the problem, as they will only give them to you once you reach the serious stage of the disease. Vaccines and other developments remain promising but still uncertain. Thankfully, there are aspects over which we have some control and can play it smart: lose weight and increase your ventilatory capacity with specific exercises.
I anticipate an objection that you have already made to me in the past: what about the cases of athletes who ended up in the hospital with serious COVID-19? The answer lies in the fact that the clinical outcome of the coronavirus infection depends largely on the amount of virus that infects the body, what virologists call “viral load”. Healthy, sporty young people who are attacked by an exaggerated viral load, as can happen, may find themselves fighting in the same conditions as an elderly or obese person who is attacked by a modest viral load. Given that we have no way of knowing what type of viral load we may be exposed to, let us do our best to prepare ourselves to face the worst. Always of course hoping for the best.
References
1
Caussy
C
,
Pattou
F
,
Wallet
F
,
Simon
C
,
Chalopin
S
,
Telliam
C
, et al.; COVID Outcomes HCL Consortium and Lille COVID–Obesity Study Group. Prevalence of obesity among adult inpatients with COVID-19 in France. Lancet Diabetes Endocrinol. 2020;8(7):562–4. doi:.https://doi.org/10.1016/S2213-8587(20)30160-1
2
Kass
DA
,
Duggal
P
,
Cingolani
O
. Obesity could shift severe COVID-19 disease to younger ages. Lancet. 2020;395(10236):1544–5. doi:.https://doi.org/10.1016/S0140-6736(20)31024-2
3
Beretta
A
. Unexpected liaisons between old cytokines and new deadly virus. Swiss Med Wkly. 2020;150:w20315. doi:.https://doi.org/10.4414/smw.2020.20315
4
Ouchi
N
,
Parker
JL
,
Lugus
JJ
,
Walsh
K
. Adipokines in inflammation and metabolic disease. Nat Rev Immunol. 2011;11(2):85–97. doi:.https://doi.org/10.1038/nri2921