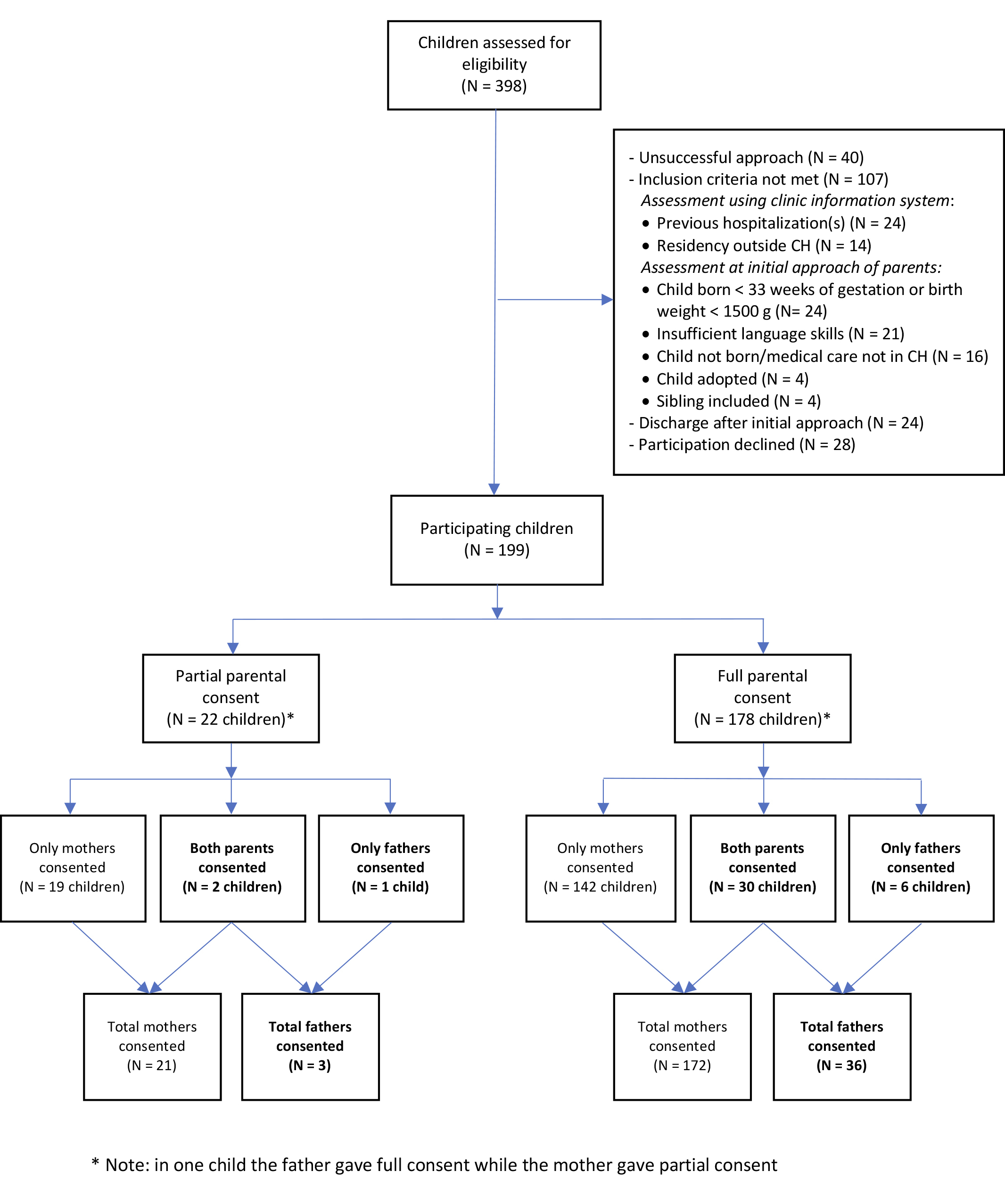
Figure 1 Study flow chart (modified from figure 1 in [3]).
DOI: https://doi.org/10.4414/smw.2020.20289
Vaccine hesitancy is listed by the World Health Organization (WHO) as one of the 10 current global health threats [1]. This is of great concern as vaccination has been shown to be immensely successful, cost-effective and prevents millions of deaths every year. In most societies, mothers are the primary caregivers of young children and thus involved in well-baby visits and other health-related issues of their children. However, especially in industrialised countries, fathers are increasingly involved in these activities, making vaccination a true “family affair” today. Although immunisations are generally well implemented in infants and young children, substantial gaps are often found in older children, adolescents and, especially, in adults [2].
We recently conducted a large survey amongst parents of young children, exploring the implementation of immunisations in pregnancy and the general immunisation status of the children and their parents in Switzerland. Here we report data on the immunisation status and attitudes concerning immunisation of fathers of young children. Our findings in mothers and children have been reported elsewhere [3].
Furthermore, to put our findings in the context of previous publications, we performed a literature review to identify previous studies focusing on the completeness of the immunisation status of fathers to compare them with our findings.
The Ethics Committee of North-Western and Central Switzerland, EKNZ, approved the study in November 2016 (Project-ID 2016-01894).
The Swiss National Immunisation Technical Advisory Group (Eidgenössische Kommission für Impffragen, EKIF or Commission fédérale pour les vaccinations, CFV) currently recommends, among others, the following immunisations of potential relevance for fathers of young children:
This was a survey among parents of children who were hospitalised at the University of Basel Children’s Hospital, Basel, Switzerland, details of which have been published before [3]. Briefly, for parents to be eligible, their child had to be born on or after 1 January 2013 and be at least 6 months old at the time of hospitalisation. Further inclusion criteria are shown in figure 1 below.
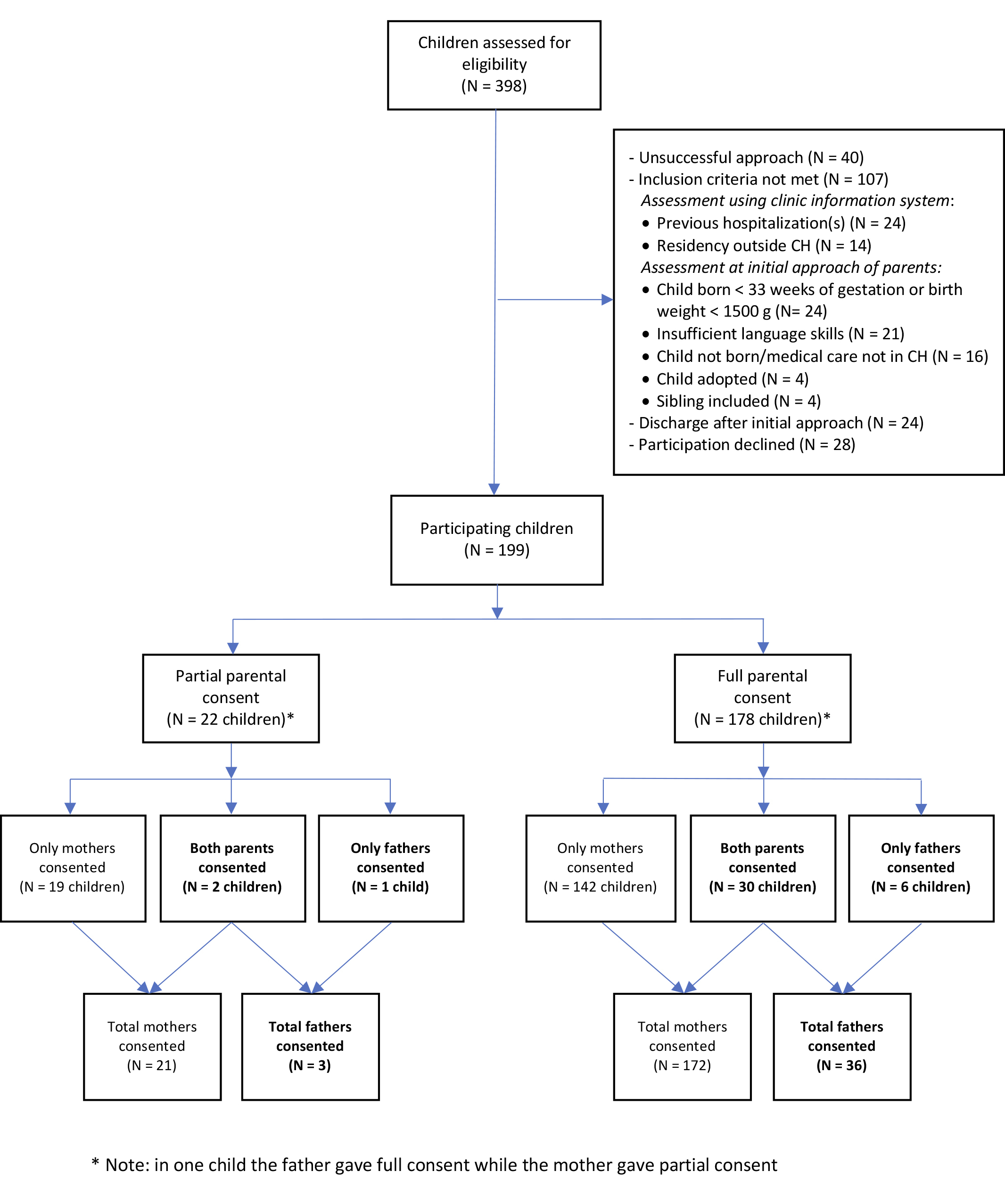
Figure 1 Study flow chart (modified from figure 1 in [3]).
Study enrolment occurred on a weekly basis according to the availability of the investigator (MLE) between January and June 2017. Basic screening for eligibility used the hospital’s clinic information system. The remaining inclusion criteria were assessed during a personal approach to the parents. The study was then briefly explained by the investigator and detailed information and a consent form were distributed in written form to all eligible parents in either German, English or French. If communication in one of these three languages was not possible, the child was excluded from the study. In a second approach, the mother and/or the father were interviewed, and the vaccination records of the child and participating parent(s) were obtained, if available. If study participants did not provide the vaccination records while in hospital, we sent a reminder by mail several days after discharge.
Parents were asked to give consent for the complete interview. Parents who declined were asked if they were willing to participate in a short interview consisting of four questions, regarding their age, education level, attitudes towards vaccinations in general and availability of vaccination records. All parents who gave consent for the complete interview were offered free vaccination counselling on the basis of their documented vaccinations.
Vaccination status was categorised as “up to date” if the following were documented:
The standardised study interview was divided into three parts. The first part contained questions to the mother, the second part contained questions to the father (appendix 1) and the third part contained questions concerning the child, which were posed to the first participating parent if both parents took part. We classified parental education according to the International Standard Classification of Education (ISCE) [4]. Data from the interviews were electronically recorded via secuTrial, a web-based database application.
We developed an immunisation score specifically for fathers of young children, with the goal of quantifying completeness of their immunisation status and correlating it with that of their children (appendix 2).
Sample size was calculated on the basis of the primary endpoint of the original study, which was recommendations and immunisations received by the children’s mothers during pregnancy [3]. For all other calculated frequencies, no inference was made. All analyses of secondary research questions are exclusively exploratory. Data was analysed using R language and environment.
We searched in PubMed for studies published between 1 April 2009 and 1 December 2019 with the combination of MeSH terms, title or abstract (fathers OR paternal OR parental OR parents) AND (vaccination status OR immunisation status OR immunization status OR vaccination coverage OR immunisation coverage OR immunization coverage OR vaccination record OR immunisation record OR immunization record) in December 2019.
For the initial search no language restrictions were applied; no studies had to be excluded because the full text was in a language other than English, German or French. Identified articles were categorised by MLE as eligible by their title, followed by abstract content and full text reading. UH independently reviewed all abstracts and the full text of those articles remaining after categorisation by the first reviewer (MLE) and a 10% subset of all titles excluded by the first reviewer (MLE). Disagreements between the two reviewers were solved by discussion.
To be included in the review the paper had to focus on general vaccination status of fathers or both parents. Papers that focused on solely one vaccination such as pertussis or influenza were excluded.
A total of 398 children met the age criterion and were screened for eligibility; 199 (50%) of children and 39 (10%) of their fathers participated (fig. 1). In 36 instances the father gave consent for the complete interview and 3 fathers consented to the short interview.
General characteristics of the 39 participating fathers are shown in table 1. The great majority had a positive or mostly positive attitude towards vaccinations, irrespective of their educational level. The following detailed analyses are based on interviews with the 36 fathers who gave full consent for study participation.
Table 1 General characteristics of participating fathers.
| Fathers | Partial and full consent | Full consent | |
|---|---|---|---|
| Age (in years) | |||
| Total n | 39 | 36 | |
| Mean | 35.3 | 35.1 | |
| SD | 5.8 | 5.7 | |
| Median | 34 | 34 | |
| IQR | 31.5–39 | 31.75–38.25 | |
| Range | 26–52 | 26–52 | |
| Educational level* | |||
| Total n | 39 | 36 | |
| Compulsory School (0–3), n (%; 95% CI) | 3 (7.7; 2–22) | 3 (8.3; 2.2–23.6) | |
| Apprenticeship (4), n (%; 95% CI) | 18 (46.2; 30.4–62.6) | 16 (44.4; 28.3–61.7) | |
| Higher Education (5–8), n (%; 95% CI) | 18 (46.2; 30.4–62.6) | 17 (47.2; 30.8–64.3) | |
| Attitude towards vaccination | |||
| Total n | 39 | 36 | |
| Negative, n (%; 95% CI) | 0 (0; 0–11.2) | 0 (0; 0–12) | |
| Mostly negative, n (%; 95% CI) | 2 (5.1; 0.9–18.6) | 2 (5.6; 1–20) | |
| Mostly positive, n (%; 95% CI) | 28 (71.8; 54.9–84.5) | 25 (69.4; 51.7–83.1) | |
| Positive, n (%; 95% CI) | 9 (23.1; 11.7–39.7) | 9 (25; 12.7–42.5) | |
| Vaccination records† | |||
| Total n | 39 | 36 | |
| Record existent, n (%; 95% CI) | 23 (59; 42.2–74) | 21 (58.3; 40.9–74) | |
| Record available, n (%; 95% CI) | Unknown | 15 (41.7; 26–59.1) | |
CI= confidence interval; IQR= interquartile range; SD= standard deviation * According to International Standard Classification of Education Levels † Existent: according to history; available: provided to study investigator for assessment
Only 15 (42%) of 36 fathers were able to provide their immunisation records; 6 (17%) stated that they possess records (but did not provide them for consultation) and the remaining 15 (42%) fathers stated that they had no records.
All fathers had one or more physician contacts in the 5 years before study participation, mainly with general practitioners. However, only 9 (25%) of 36 stated that their immunisation records were assessed during their last medical consultation and 15 (48%) of 31 with specific knowledge on the timing reported that the last assessment of their immunisation status by a physician was <5 years ago.
In the group of fathers with a positive attitude towards immunisation, total immunisation scores were highest, with a mean of 4.4 out of a maximum possible score of 11, as compared with 3.1 and 3.0 in those with mostly positive and mostly negative attitudes, respectively. Although nonparametric regression models showed no significant correlation as a result of the small numbers, a trend correlation of an up-to-date immunisation status of children with a positive paternal attitude to vaccinations was noted. All children of fathers with positive or mostly positive attitudes towards immunisation had maximum mean immunisation scores: 3 of a maximum of 3 in children age 6 to <12 months, 6 of 6 in children ≥12 to <24 months, and 10 of 10 in children ≥24 months of age.
We offered immunisation counselling to all participating fathers. Fourteen (39%) of 36 were interested and 13 (36%) provided immunisation records as the basis for the individual counselling. Of these, 2 (15%) were up to date with all generally recommended immunisations for adults. The remaining 11 (85%) fathers had one or more gaps and received individual recommendations for catch-up or booster immunisations accordingly. Follow-up on the outcome of counselling 4–6 weeks later was successful in eight (73%) of them. Of these, one (13%) had received the recommended vaccination(s) in the meantime. Two mentioned that they had forgotten about it or had not had time yet to consult a physician for administration of the recommended immunisations. One father stated that he did not deem the recommended immunisations useful, another that the family doctor had not had an appointment available yet, and two stated that they intended to receive the immunisations at their next regular physician’s appointment. One father gave no reason for noncompliance with our recommendation.
Overall, 20 (56%) fathers had received a recommendation for immunisation against pertussis after birth of their child by a healthcare professional and 13 (65%) of them said they were then immunised. Pertussis immunisation was predominantly recommended by paediatricians (n = 7) and the vaccine had been administered by paediatricians (n = 5), general practitioners (n = 5) and other physicians (n = 3). The main reason for noncompliance was the notion of fathers that pertussis immunisation was not considered useful (n = 4 of 7).
The PubMed search yielded 1376 results (appendix 3). Of these, 1203 were excluded for not being relevant to the study question on the basis of the study title. All abstracts of the remaining 173 publications were read and 154 deemed irrelevant to our study question. The remaining 19 papers were read in full; this resulted in exclusion of 16 due to lack of relevance leaving 3 studies (summarised in table 2) that matched our inclusion criteria.
Table 2 Studies included in the review.
| Study | Cheffins et al. 2011 [ 5 ] | Rossmann et al. 2014 [ 6 ] | Spaan et al. 2017 [ 7 ] |
|---|---|---|---|
| Country/region | Australia, Queensland | USA, Texas | Netherlands |
| Study type, setting, and year of performance | Prospective cohort study in 8 general practices, year unknown | Survey on acceptability of recommended vaccinations among a convenience sample at a county hospital, year unknown | Cross-sectional observational study using online questionnaires in orthodox protestants, 2013 |
| Study population | 177 parents of children <4 years of age | 258 predominantly Hispanic, underinsured and medically underserved adult contacts (other than mothers) of newborn infants, 18–73 years of age | 981 adults 18–40 years of age with (n = 357) or without children (n = 624) |
| Number of fathers | 48 | 166 | 260 male participants, number of fathers not reported |
| Immunisations assessed | MMR, pertussis, tetanus, varicella (self-reported) | Receipt of recommended routine childhood immunisations (self-reported) | Vaccination status categories: fully vaccinated, partly vaccinated, not vaccinated, unknown (self-reported) |
| Intervention | Recommendation for catch-up immunisations based on parent’s history and national guidelines; follow-up 2 months later | Tdap, influenza, PCV, MCV were offered on site free of charge to those with immunisation gaps and/or fulfilled indications after education about pertussis and other recommended adult immunisations | None |
| Major findings | Vaccination status was incomplete for >1 vaccine in 66% of parents Most frequently recommended vaccines: pertussis (46%) and tetanus (26%) 53% of parents with immunisation gaps complied with recommended vaccinations Most common reason for non-compliance: “haven’t got around to it” (36%) |
Willingness to receive vaccines if indicated: Tdap 76.1%, influenza 73.3%, PCV 53.3%, MCV 50.5% Attitudes towards cocooning: “good or great idea” in 97.2% of participants |
Vaccination coverage of respondents reported to be 55.3% Vaccination coverage decreased with increasing level of religious conservatism from 80.0% (low) to 57.0% (medium) to 10.8% (high) |
| Shortcomings | No specific results for fathers reported | No specific results for fathers reported No specific results on previous actual vaccinations or those administered during intervention reported |
No specific results for fathers reported No vaccine specific results reported Level of completeness of vaccinations not reported |
MCV = meningococcal conjugate vaccine; MMR = measles, mumps, rubella vaccine; PCV = pneumococcal conjugate vaccine; Tdap = tetanus-diphtheria-acellular pertussis combination vaccine
Cheffins et al. [5] examined the self-reported parental immunisation status for MMR, pertussis, tetanus and varicella. Data were collected from 177 parents including 48 fathers during the child’s vaccination appointment in general practices in Queensland, Australia, and 66% had at least one vaccine missing.
Rossmann et al. [6] investigated the acceptability of recommended vaccinations for adult contacts (other than the mothers) of new-born infants during well-baby visits at a county hospital in Texas, USA. Self-reported receipt of recommended routine childhood immunisations was assessed without further classification and no specific details were reported.
Finally, Spaan et al. [7] examined vaccination coverage in orthodox Protestants in the Netherlands. Most (55.3%) respondents reported being “vaccinated”, but the level of completeness according to national recommendations was not addressed.
Unfortunately, no specific data that would have allowed us to distinguish the immunisation status of fathers from other men and/or mothers was reported in any of these three studies.
We assessed the attitude of fathers concerning immunisations and compliance with recently implemented recommendations for immunisation against pertussis after the child’s birth in Switzerland. The great majority of fathers stated that they had a positive or mostly positive attitude towards vaccinations. However, their willingness to participate in vaccination counselling was disappointingly low at 38%. Further, the fact that only 15% of fathers who participated in immunisation counselling were up to date with all generally recommended immunisations for adults is worrisome and so is the lack of motivation to close immunisation gaps.
Apparently, reviewing the immunisation status of their patients during consultations is a low priority for many primary care physicians in Switzerland, as indicated by the high proportion of missed opportunities for vaccinations during physician visits: the majority of fathers stated that their immunisation status was not reviewed during their last physician visit within the previous 5 years. This is worrying, as we found substantial immunisation gaps: only 15% of fathers who participated in immunisation counselling and provided their immunisation records were up to date with all their immunisations and the mean immunisation score was 4.4 of a maximum of 11 points. Of specific concern is the fact that up-to-date immunisations are especially important for persons who are in close contact with young children, as they are a frequent source of transmission of infectious diseases such as pertussis [8]. Unfortunately, our survey did not address the specific reason for the last physician visit. Admittedly, during consultations for acute diseases assessing the general immunisation status is challenging. However, a standing order in the physician’s office could delegate this important task to office assistants. We propose that access to immunisations should be simplified and any physician visit by men should be used to check their immunisation status, including those with gynaecologists when accompanying their pregnant partners and paediatricians when accompanying their child. As we have shown, several fathers had received their pertussis immunisation from a paediatrician. The option of receiving vaccinations on site during a consultation with the child without the need to arrange a separate consultation with another doctor should be attractive for fathers. As shown in the study by Rossmann et al. [6], the willingness to receive immunisations on the same day and on site during a well-baby visit is high.
Our review of the literature resulted in only three studies and parental immunisation status was assessed in sufficient detail in one of them [5]. Of note, only 34% of participating parents had a complete immunisation status. However, data were not stratified by mothers and fathers, and immunisations were self-reported but not verified by vaccination documentation, which could have resulted in over-reporting. In our study, 30% of mothers [3] and 15% of fathers were up-to-date with their immunisations. Significant immunisation gaps were also found in adults in a Swiss study conducted by Valeri et al. in 2014, where free evaluation of immunisation status was offered in pharmacies. Proportions of up-to-date tetanus immunisation were 56% and 44% and those for diphtheria were 45% and 34% for >5 and >6 doses, respectively [2].
In our study, the great majority of fathers stated that they had a positive or mostly positive attitude towards vaccinations, which is an ideal prerequisite for successful individual counselling and public information campaigns. Surprisingly, however, only approximately 40% of all fathers showed interest in immunisation counselling. We are concerned that this may indicate a lack of interest and competence in health issues in general.
Healthcare providers have a strong influence on vaccine acceptance [9]. Therefore, it will be crucial to improve their confidence in vaccination and additional efforts must be made to engage them in activities aimed at tackling vaccine hesitancy amongst their patients in the future.
Immunisation records in Switzerland are currently primarily paper based. In routine and emergency consultations, where patients rarely have their vaccination records available, this often poses a problem. This made data collection of documented immunisations cumbersome for the participants and investigators in this study. Specifically, only 58% of fathers in our study stated that they possessed vaccination records and only 41% could provide them. This may indicate that in fact they were missing in many cases. Electronic immunisation records, which can be accessed and updated whenever necessary either by a physician or the patients themselves, are a possible solution to this problem. In fact, electronic documentation of vaccination records has been available in Switzerland since 2012 via the website http://www.meineimpfungen.ch on a voluntary basis. Unfortunately, however, its use still is far from optimal with only 150,000 registrations (<2% of the population in Switzerland) since its launch. Encouragingly, a 20% increase in new registrations was observed in 2017. Currently, campaigns supported by the Swiss Federal Office of Public Health are being performed to increase awareness among medical personnel and to promote the use of electronic vaccination records [10].
A comparison of our results with other studies regarding pertussis immunisation in parents of young children shows that no progress regarding implementation of the so-called “cocooning strategy” has been made during the past several years [11, 12]. Parental knowledge about pertussis has been shown to be insufficient in multiple studies [11–13]. Therefore additional information for parents is evidently needed, even more so because doubt about its usefulness is the most important reason for refusal of pertussis immunisation after birth of the child. Ideally, pertussis immunisation should be offered to fathers and mothers (if not immunised during pregnancy) after delivery of the new-born on the maternity ward or on the occasion of the first well-baby visit with the paediatrician, at the latest.
Our study has strengths and limitations. A major strength is the personal interview that was conducted by the same investigator with every participant, as well as the consultation of vaccination records where available. However, since the results originate from these interviews, recall bias cannot be excluded. The hospital as a setting for this type of intervention can arguably be challenging as parents may be preoccupied with their sick child. As children in intensive care were not included in our study, none of the children was in a critical state of health. More suitable access to parents, for example during routine paediatrician or family doctor visits, should be explored in the future.
Many of our analyses of secondary endpoints did not reveal significant findings because of the limited sample size and low participation rate of fathers (20%), which is a limitation of our study. Therefore, our findings should be interpreted carefully and not be generalised. However, whereas many such investigations have been performed in mothers, as the literature search has shown, this is the first study to investigate immunisation attitudes and status in fathers of young children and report specific results for fathers. Only one other study has investigated immunisation status in parents of young children, without providing separate data for fathers [5]. We encourage other study groups to enlarge the knowledge in the future.
Finally, as we limited the literature search to studies that assessed the general vaccination status of fathers or both parents we may have missed relevant papers on adherence to some of the specific vaccines such as MMR, pertussis or influenza.
In conclusion, more efforts are needed by health care providers to inform and vaccinate fathers of young children as this is a group with often incomplete immunisation status and, until now, potentially missed opportunities for catch-up vaccinations. Easier access to vaccinations should be provided and supported by child health policy makers.
The appendices are available as PDF files at https://smw.ch/article/doi/smw.2020.20289.
The authors would like to acknowledge all study participants and the staff of the UKBB for their cooperation in conducting this study.
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
UH is a member of The Global Pertussis Initiative (GPI) which is supported by Sanofi, USA and has received speaker fees for product independent vaccination related scientific presentations from Pfizer, Germany, and Sanofi Pasteur, France. All other authors declared no competing interest.
1 https://www.who.int/emergencies/ten-threats-to-global-health-in-2019. [Accessed 2020 May 6]
2 Valeri F , Hatz C , Jordan D , Leuthold C , Czock A , Lang P . Immunisation coverage of adults: a vaccination counselling campaign in the pharmacies in Switzerland. Swiss Med Wkly. 2014;144:w13955. doi:.https://doi.org/10.4414/smw.2014.13955
3 Erb ML , Erlanger TE , Heininger U . Child-parent immunization survey: How well are national immunization recommendations accepted by the target groups? Vaccine X. 2019;1:100013. doi:.https://doi.org/10.1016/j.jvacx.2019.100013
4ISCE. 2011. 2018. pp. 1–88. Http://uis.Unesco.org/en/topic/international-Standard-Classification-Education-Isced. Last accessed May 6, 2020
5 Cheffins T , Spillman M , Larkins S , Heal C . Recommending vaccination - general practice intervention with new parents. Aust Fam Physician. 2011;40(6):437–9.
6 Rossmann Beel E , Rench MA , Montesinos DP , Healy CM . Acceptability of immunization in adult contacts of infants: possibility of expanding platforms to increase adult vaccine uptake. Vaccine. 2014;32(22):2540–5. doi:.https://doi.org/10.1016/j.vaccine.2014.03.056
7 Spaan DH , Ruijs WLM , Hautvast JLA , Tostmann A . Increase in vaccination coverage between subsequent generations of orthodox Protestants in The Netherlands. Eur J Public Health. 2017;27(3):524–30. doi:.https://doi.org/10.1093/eurpub/ckx017
8 Wiley KE , Zuo Y , Macartney KK , McIntyre PB . Sources of pertussis infection in young infants: a review of key evidence informing targeting of the cocoon strategy. Vaccine. 2013;31(4):618–25. doi:.https://doi.org/10.1016/j.vaccine.2012.11.052
9 Paterson P , Meurice F , Stanberry LR , Glismann S , Rosenthal SL , Larson HJ . Vaccine hesitancy and healthcare providers. Vaccine. 2016;34(52):6700–6. doi:.https://doi.org/10.1016/j.vaccine.2016.10.042
10Bundesamt für Gesundheit. Europäische Impfwoche 23.-29. April 2018: der schweizerische elektronische Impfausweis. Bull BAG 17/2018 Apr 23: p 11.
11 Urwyler P , Heininger U . Protecting newborns from pertussis - the challenge of complete cocooning. BMC Infect Dis. 2014;14(1):397. doi:.https://doi.org/10.1186/1471-2334-14-397
12 Donnan EJ , Fielding JE , Rowe SL , Franklin LJ , Vally H . A cross sectional survey of attitudes, awareness and uptake of the parental pertussis booster vaccine as part of a cocooning strategy, Victoria, Australia. BMC Public Health. 2013;13(1):676. doi:.https://doi.org/10.1186/1471-2458-13-676
13 Suryadevara M , Bonville CA , Cibula DA , Valente M , Handel A , Domachowse JR , et al. Pertussis vaccine for adults: Knowledge, attitudes, and vaccine receipt among adults with children in the household. Vaccine. 2014;32(51):7000–4. doi:.https://doi.org/10.1016/j.vaccine.2014.10.018
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
UH is a member of The Global Pertussis Initiative (GPI) which is supported by Sanofi, USA and has received speaker fees for product independent vaccination related scientific presentations from Pfizer, Germany, and Sanofi Pasteur, France. All other authors declared no competing interest.