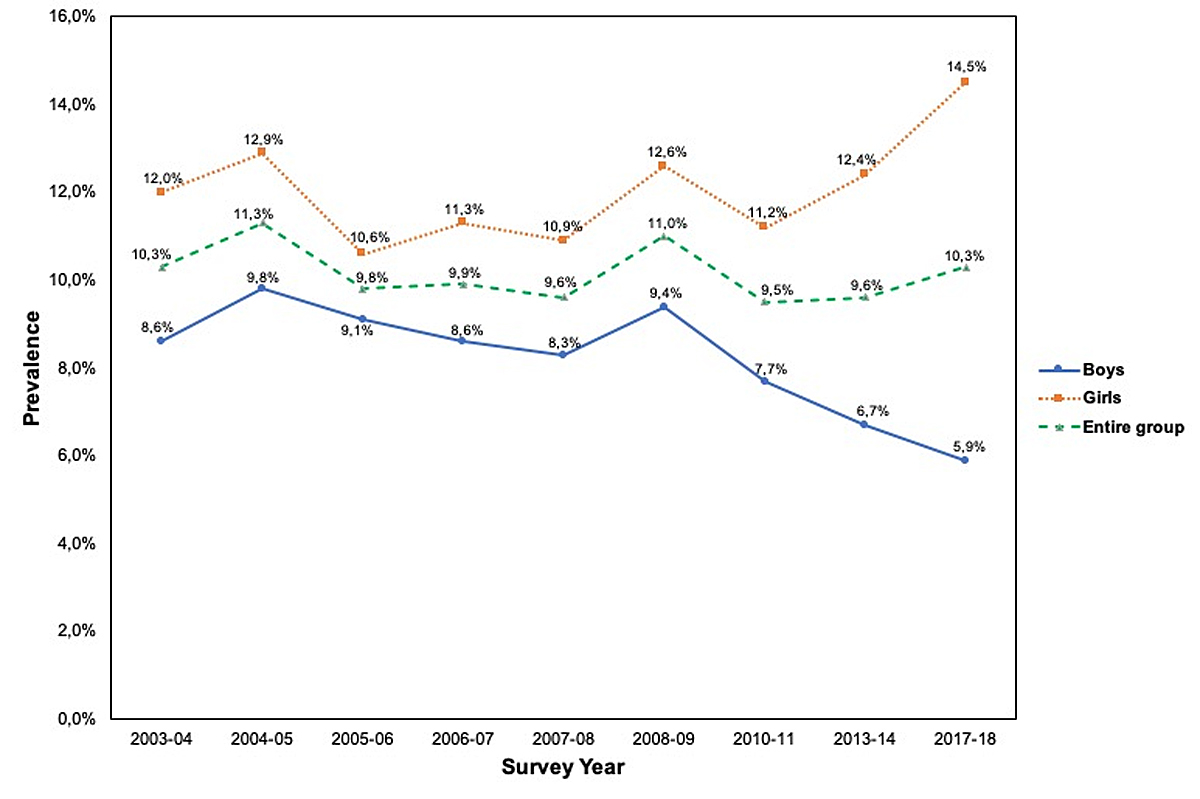
Figure 1 Trends in the prevalence of overweight among Geneva children aged 5–6 years between 2003–04 and 2017–18 by gender.
DOI: https://doi.org/10.4414/smw.2020.20309
Childhood malnutrition problems have become a serious global public health issue [1]. The increasing prevalence of overweight and obesity in childhood has become an epidemic and a major health challenge of the 21st century [1–3]. An estimation published in 2016 showed that the proportion of children and adolescents suffering from obesity had increased from 11 million to 124 million in 40 years, in both high-, middle- and low-income countries [2, 4].
Excessive fat accumulation has been attributed to an imbalance between energy intake and expenditure [5–7], which has a multifactorial origin. Hereditary, environmental and socioeconomic factors play a role in the predisposition to and development of overweight and obesity. Studies suggest that heritable factors are responsible for 40 to 85% of the variation in adiposity [8]. Exposure to an obesogenic environment – such as parental overweight, unhealthy eating habits, shortened sleep duration, sedentary lifestyle, environmental and nutritional influences during a critical period in development (particularly during gestation), parental education, lower average household income, globalisation and urbanisation – have also been shown to play a role in the increased prevalence [3, 7, 9, 10].
Overweight and obesity in childhood affect children’s health in many ways, with negative consequences for their physical, mental and social well-being throughout life [11, 12]. Physical comorbidities affect various body systems, and the resulting medical conditions can include type 2 diabetes mellitus, metabolic syndrome, hyperandrogenism, hypertension, dyslipidaemia, adult coronary heart disease, nonalcoholic fatty liver disease, cholelithiasis, obstructive sleep apnoea, hypoventilation syndrome, fractures, slipped capital femoral epiphysis, tibia vara, musculoskeletal pain, idiopathic intracranial hypertension, intertrigo, furunculosis and hidradenitis suppurativa. Although most of these physical health conditions have an impact throughout adulthood, adult coronary heart disease can also act in the short term, leading to premature death [3, 13].
Other negative effects include stigma, discrimination and social marginalisation, which can affect academic performance and lead to the onset of mental disorders such as anxiety, depression, distorted body image and poor self-esteem [5, 12, 13]. Furthermore, the presence of parental obesity, BMI trajectory during childhood, age and severity of childhood obesity are all strong predictors of adult obesity, which increases the risk of non-communicable diseases [3, 5]. Lastly, obesity also contributes significantly to healthcare costs incurred during adulthood [14, 15].
The aim of the present study is to estimate the prevalences of overweight and obesity and their time trends among 5-to 6-year-old schoolchildren in Geneva over a 15-year period starting in 2003–2004, and to compare these with results from other areas of Switzerland. We hypothesised that the trends observed in Geneva would be similar to those observed in other large cities in the country.
Following our previous publication, we have continued to implement preventive measures affecting all age groups through schools and in day-care centres.
From a nutritional perspective, the efforts have been focused on healthy, balanced eating (Fourchette Verte) in all age groups, nutritional education in class (Senso5 for primary schools and nutritional education for the adolescents), the promotion of our nutritional pyramid, and school regulations on which snacks are authorised for school breaks (Collation Saine project).
As for physical activity, we have implemented two projects for the day care centres, BB aime bouger and Youpla bouge, with the aim of encouraging movement in toddlers. For older children, the rules for medical excuses have been changed and we have introduced adapted physical education for children with injuries or chronic diseases.
Data were obtained from nine methodologically similar cross-sectional surveys carried out by the School Health Service of Geneva (Service de santé de l'enfance et de la jeunesse) and conducted between 2003–04 and 2017–18. The data were recorded using the same questions in all surveys and the sampling methods were the same in all the surveys, except for the 2017–18 school year when a representative group was used. For the 2017–18 school year, it was not possible to collect data on the totality of the age group for logistical reasons and because of a change in the organisation of health visits. We therefore decided to use a representative sample of students instead.
In the canton of Geneva (Switzerland), all newly enrolled schoolchildren attending their first year of school – a period in which children present major changes in relation to their eating and physical activity habits [16, 17] – undergo a mandatory health visit in the company of their parents – hence the age group chosen for this study. During this systematic health check at school, the school nurses ask the parents and the child questions about health-related topics such as vaccination, nutrition, exercise, well-being and integration. A full description of the methodology for the anthropometric data collection has been published in another article [18].
A total of 26,313 schoolchildren (13,395 boys and 12,918 girls) aged 5–6 years and enrolled in the public school system of the canton of Geneva were screened during this period. Children attending private schools in Geneva were not included in the study. In the 2017–18 school year, the data provided was not exhaustive, in contrast to some of the previous years, but was from a representative sample (21.1%) randomly selected from among schoolchildren of the same age and representing one class from each primary school in the canton of Geneva.
For the purpose of the study, the measuring methodologies and equipment used in all schools were identical across the nine surveys. As previously agreed with the parents, the children’s weight and height measurements were taken by the school nurses using standard anthropometric techniques [19] and then plotted on a weight-to-height and BMI curve [20]. A negligible number of parents (<0.3%) refused the weight and height measurements.
Body weight (kg) was measured while the children were in underclothes, without their shoes, using a regularly calibrated SECA™ digital scale (SECA™ Alpha, Model 770, Hamburg, Germany). Height (cm) was measured during inspiration using a wall-mounted or balance-mounted height scale. The data were then discussed with the child and his or her parents. If necessary, the school nurse scheduled another meeting for further explanations [18].
The data collected by the nurses was anonymously transferred to a database where the body mass index (BMI) could be calculated and compared to international standards [18], thus enabling an estimate of the prevalence of overweight and obesity for each school year.
The body mass index (BMI) or Quetelet Index, described in 1832 [21], is a measure of human body shape based on an individual’s mass and height. BMI was calculated for each child using their weight in kilograms divided by the square of their height in metres (kg/m2).
In children, BMI varies substantially with gender and age. The International Obesity Task Force (IOTF) provided BMI cut-off points for overweight and obesity by gender and age range from 2-18 years, defined according to Cole et al.’s criterion [20] and based on the percentile value corresponding to overweight (BMI ≥25 kg/m2) or obesity (BMI ≥30 kg/m2) at age 18 years, obtained by averaging data from six countries or areas: Brazil, Hong Kong, the Netherlands, Singapore, the United Kingdom and the United States [20].
Depending on their weight status, each child was allocated to one of three groups: normal (including underweight) ISO-BMI <25, overweight ISO-BMI 25–30, and obese ISO–BMI > 30 [20].
All data were reviewed exhaustively to detect data entry errors. Prevalences of obesity, overweight and normal weight were analysed separately for boys and girls.
Categorical variables were expressed in terms of number of cases and percentages. The normality of the distribution of the variables (height and weight) was determined with the Kolmogorov-Smirnov test. Comparisons between the prevalences of overweight and obesity were made using trend chi-square tests. Changes in prevalence rates were also determined with these tests. Tests of trends used the p <0.05 significance level.
Statistical analysis was performed using STATA™ (STATACorp, Texas, USA) version 13.0 for Windows.
Table 1 shows the prevalence of overweight and obesity in children aged 5–6 years in the canton of Geneva over the 15-year study period.
Table 1 Prevalence (95% confidence intervals) of overweight and obesity in Geneva children aged 5-6 years over nine school years between 2003–04 and 2017–18 using Cole’s reference.
| Survey year | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 2003–04 | 2004–05 | 2005–06 | 2006–07 | 2007–08 | 2008–09 | 2010–11 | 2013–14 | 2017–18 | |
| Entire group | |||||||||
| n | 3728 | 3908 | 3718 | 3109 | 3533 | 2609 | 2600 | 2184 | 924 |
| Normal* | 86.1 (84.9–87.1) |
85.5 (84.3–86.5) |
87.3 (86.1–88.3) |
87.4 (86.1–88.5) |
87.3 (86.1–88.3) |
85.7 (84.3–86.9) |
88.0 (86.6–89.1) |
87.2 (85.7–88.5) |
85.4 (82.9–87.5) |
| Overweight | 10.3 (9.3–11.3) |
11.3 (10.3–12.3) |
9.8 (8.8–10.8) |
9.9 (8.8–11.0) |
9.6 (8.6–10.6) |
11.0 (9.8–12.2) |
9.5 (8.4–10.6) |
9.6 (8.4–10.9) |
10.3 (8.5–12.4) |
| Obese | 3.6 (3.0–4.2) |
3.1 (2.6–3.6) |
2.8 (2.3–3.3) |
2.7 (2.1–3.3) |
3.1 (2.5–3.7) |
3.3 (2.6–4.0) |
2.5 (1.9–3.0) |
3.2 (2.5–4.0) |
4.3 (3.1–5.8) |
| Overweight and obese | 13.95 (12.8–15.0) |
14.4 (13.3–15.5) |
12.6 (11.5–13.7) |
12.6 (11.4–13.8) |
12.7 (11.6–13.8) |
14.3 (13.0–15.7) |
12.0 (10.8–13.3) |
12.8 (11.4–14.2) |
14.6 (12.4–17.0) |
| Girls | |||||||||
| n | 1802 | 1927 | 1834 | 1175 | 1764 | 1423 | 1365 | 1158 | 470 |
| Normal* | 84.2 (82.4–85.8) |
83.8 (82.0–85.3) |
86.5 (84.8–87.9) |
85.6 (83.4–87.4) |
85.8 (84.0–87.3) |
83.8 (81.8–85.6) |
86.3 (84.3–88.0) |
84.4 (82.2–86.3) |
81.0 (77.2–84.2) |
| Overweight | 12.0 (10.5–13.5) |
12.9 (11.4–14.4) |
10.6 (9.2–12.0) |
11.3 (9.6–13.2) |
10.9 (9.5–12.4) |
12.6 (10.9–14.4) |
11.2 (9.6–12.9) |
12.4 (10.6–14.4) |
14.5 (11.6–17.9) |
| Obese | 3.8 (3.0–4.7) |
3.3 (2.5–4.1) |
2.9 (2.2–3.7) |
3.1 (2.2–4.2) |
3.3 (2.5–4.2) |
3.6 (2.7–4.6) |
2.5 (1.7–3.4) |
3.2 (2.3–4.3) |
4.5 (2.9–6.7) |
| Overweight and obese | 15.8 (14.1–17.5) |
16.2 (14.6–17.9) |
13.5 (12.0–15.1) |
14.4 (12.5–16.5) |
14.2 (12.6–15.9) |
16.2 (14.3–18.2) |
13.7 (11.9–15.6) |
15.6 (13.6–17.8) |
19.0 (15.7–22.7) |
| Boys | |||||||||
| n | 1926 | 1981 | 1884 | 1934 | 1769 | 1186 | 1235 | 1026 | 454 |
| Normal* | 87.9 (86.3–89.2) |
87.2 (85.6–88.5) |
88.1 (86.5–89.4) |
89.1 (87.6–90.4) |
88.8 (87.2–90.1) |
87.7 (85.7–89.4) |
89.7 (87.8–91.2) |
90.1 (88.1–91.7) |
89.9 (86.7–92.3) |
| Overweight | 8.6 (7.4–9.9) |
9.8 (8.5–11.1) |
9.1 (7.8–10.4) |
8.6 (7.4–9.9) |
8.3 (7.1–9.6) |
9.4 (7.8–11.1) |
7.7 (6.3–9.3) |
6.7 (5.3–8.3) |
5.9 (4.0–8.4) |
| Obese | 3.5 (2.7–4.4) |
3.0 (2.3–3.8) |
2.8 (2.1–3.6) |
2.3 (1.7–3.0) |
2.9 (2.2–3.7) |
2.9 (2.0–4.0) |
2.6 (1.8–3.6) |
3.2 (2.2–4.4) |
4.2 (2.7–6.4) |
| Overweight and obese | 12.1 (10.7–13.6) |
12.8 (11.4–14.3) |
11.9 (10.5–13.4) |
10.9 (9.5–12.3) |
11.2 (9.8–12.7) |
12.3 (10.5–14.2) |
10.3 (8.7–12.1) |
9.9 (8.2–11.8) |
10.1 (7.6–13.2) |
* Including underweight
Taking the entire group into consideration and using Cole’s references [20], we observe that the prevalence of overweight children has stayed stable at around 10.3% since 2003–04; it has increased slightly (0.7 points) since 2013–14, but this increase is not significant (fig. 1). With regard to obesity, the prevalence has increased by 0.7 points since 2003–04, but this increase is not statistically significant. However, since 2010–11, the year when the lowest obesity prevalence was reported, there has been a relatively marked and statistically significant increase of 1.9 points (p = 0.0130) (fig. 2).
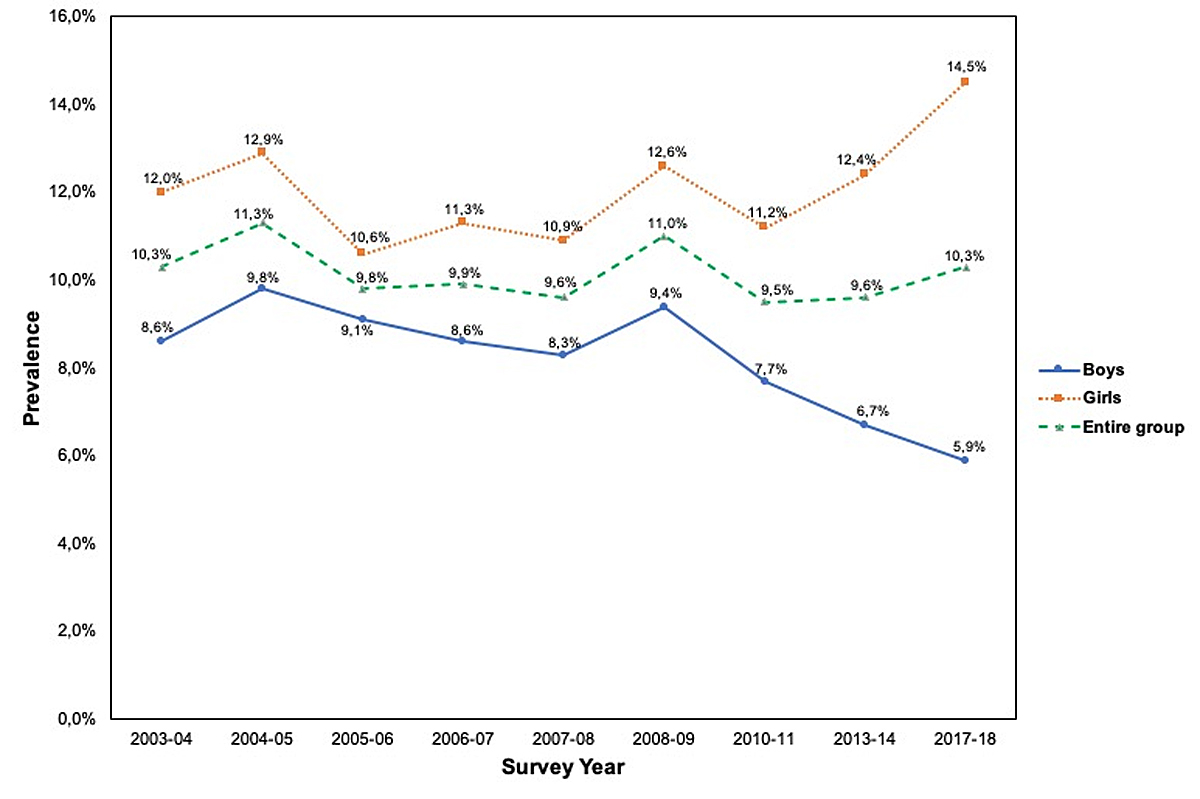
Figure 1 Trends in the prevalence of overweight among Geneva children aged 5–6 years between 2003–04 and 2017–18 by gender.

Figure 2 Trends in the prevalence of obesity among Geneva children aged 5–6 years between 2003–04 and 2017–18 by gender.
Analysing each variable by gender, the assessment shows an increase of 2.5 points (p = 0.14) in the prevalence of overweight among girls since the 2003–04 school year (prevalence of overweight among girls was 12.0% in 2003–04 and 14.5% in 2017–18). The increase has not been steady, but the increase since 2010–11 is statistically significant (prevalence of overweight among girls was 11.2% in 2010–11 and 14.5% in 2017–18, an increase of 3.3 points) (fig. 1). The prevalence of obesity has shown a similar non-significant increase (0.7 points) since 2003–04, but this rise has become more important since 2010–11, with an increase of 2.0 points (fig. 2).
Among boys after an initial decline followed by an increase, overweight has now decreased by 2.7 points (p = 0.06) since 2003–04. However, only the decrease since 2008–09 is significant (3.5 points, p = 0.0287) (fig. 1). The prevalence of obesity among boys has increased by 0.7 points since 2003–04 (prevalence was 3.5% in 2003–04 and 4.2% in 2017–18). However, the prevalence changed from 2.6% in 2010–11 to 4.2% in 2017–18, an increase of 1.6 points (fig. 2). Moreover, we observed that the prevalence curves of obesity and overweight are beginning to converge, which corresponds to a relative increase in the number of obese boys compared to the number of overweight boys.
The prevalence of overweight among children aged 5–6 years is still lower for boys than for girls, with an 8.6-point difference (fig. 1). Overweight in girls has tended to increase since 2013. The trend seems to have started around 2010–11, contrary to overweight in boys, which has been decreasing at a steady rate since 2008–09 (fig. 1). On the other hand, the prevalence of obesity is roughly the same among boys and girls in this age group, and has also shown an important increase since 2010–11 (fig. 2).
The present study investigated trends in the prevalence of overweight and obesity in children aged 5–6 years in the canton of Geneva from the 2003–04 school year to the 2017–18 one. It builds on the results of a previously published study which reported a stabilisation and a non-significant decrease in the prevalence of overweight and obesity for the same age group from 2003–04 to 2007–08 [22].
The new data obtained in the present study reveal a general stabilisation in overweight rates between 2003–04 and 2017–18. However, we identified an important difference between girls and boys due to a statistically significant increase in the prevalence of overweight in girls from 2010–11 onwards and a continuous decline in the prevalence of overweight in boys from the same age group. In addition, this study also shows a non-significant increase in the general prevalence of obesity during the same period. At the same time, there has been a relatively marked and significant increase in obesity for both boys and girls since 2010–11. We also observed a relative increase in the percentage of obese children compared to all overweight children, which is a more recent phenomenon.
The relative difference in the trends for boys and girls, especially since 2011, is of interest but is difficult to interpret because of the eminently multifactorial origin of overweight and obesity and the unclear ways in which these factors depend on sex. Some of these numerous factors have probably not changed much over the 10-year period (genetics, urbanisation, educational profile of the population), whilst others might have changed more (trends, immigration, eating habits, sleep duration, sedentary lifestyle).
At this young age group, the family is probably the main influence on behaviour, with a child’s environment having a smaller effect. It might be easier to encourage boys to be active than girls, since boys tend to be more spontaneously active than girls. This was highlighted in Epstein's paper [23], which studied slightly older children (~10 years of age) and compared the effects of family-based obesity treatment on boys and girls.
A Chinese paper by Wang et al. [24] analysed the factors contributing to sex differences in a large group of 6- to 17-year-old Chinese children. Interestingly, in this study boys were about twice as likely to be overweight or obese (16.8%) as girls (8.4%), highlighting the cultural, environmental and genetic differences between countries that make comparisons complicated. This being said, boys were more likely to exceeded energy intake recommendations, underestimate their body weight and be satisfied with their levels of physical activity than girls. They also showed that mothers were better at estimating their daughters’ weight and tended to underestimate the weight of their sons. Again, it is difficult to extrapolate these findings to a group of younger and culturally different children. It could, however, suggest that we should analyse similar variables in our population.
Data from Switzerland collected in previous investigations – as part of a study that analysed six national, cross-sectional representative school-based health surveys (1999, 2002, 2004, 2007, 2009 and 2012) [25–28] of Swiss children aged 6–12 years located in five geographic regions and also divided according to language (French, German and Italian) [28] – showed a stabilisation or decrease in the prevalence of overweight and obesity in childhood over this period, but with significant fluctuations [25, 26, 29]. Similar observations were made in other studies conducted between 1995 and 2008 of 467,294 children aged 2–19 years from nine countries (Australia, China, England, France, the Netherlands, New Zealand, Sweden, the United States and Switzerland) [30].
Nevertheless, data from 2017 – published by Health Promotion Switzerland (Promotion Santé Suisse or PSCH) in the third edition of its project “Comparative monitoring of the BMI of children and adolescents in Switzerland”, which analysed the prevalence of obesity and overweight in children and teenagers from 11 cantons and cities (cantons of Bern, Grisons, Jura, Lucerne, Obwalden, St Gallen and Uri, and the cities of Fribourg, Bern, Zurich and Basel) – showed a reduction in the proportion of overweight and obese students across all school levels of nearly 3%, from 19% in 2010 to 16% in 2017 [29]. These results are similar to those of an analysis conducted during the 2017–18 school year – also by Health Promotion Switzerland – in the cities of Basel, Bern and Zurich, which showed a downward trend and found that the lowest prevalence (19.3%) of overweight and obesity in children and adolescents was among children of primary school age. Only Cycle III (older students) showed an increase, which has stabilised in recent years. It also showed that nationality, social origin and place of schooling invariably play important roles in explaining the prevalence of overweight and obesity [31].
Furthermore, it is important to note that since 2010, there has been a marked difference between the results of the PSCH study and the results obtained in the canton of Geneva, with the latter having shown an increase in the prevalence of obesity and overweight among Geneva children. The reason for this is unclear, but it might be related to the growth in Geneva’s population recorded in 2010, which was one of the highest recorded increases since the beginning of the 1970s. This growth was essentially due to a large influx of foreign migrants: 75% of the new population of the canton of Geneva at that time was of non-Swiss nationality [32]. In addition, it is important to keep in mind that Geneva is a small and multicultural canton whose total resident population in 2018 was 501,748 inhabitants, of which 40.1% were foreigners. The most common nationalities are French (18%), Italian (6%), Spanish (5%), Portuguese (4%), English (3%) and American (3%) [33].
In addition, the link to migration is underpinned by the fact that migration is a risk factor for obesity and overweight, as reported in the literature [9]. Analyses have revealed that children with low economic status and from certain countries are more likely to be overweight or obese than Swiss children [18]. The common elements linking these risk factors are mostly economic, since immigrants tend to be of lower socioeconomic status and live in the more affordable areas of the canton. Guessous et al. [34] reported that overweight and obesity are associated with socioeconomic and sociodemographic factors. They also showed that the spatial dependence of children’s BMI was associated with the areas’ income levels [34].
It is difficult to find studies that use the same age range as ours. A similar study on the evolution of the prevalence of overweight among 5- to 6-year-old children according to socioeconomic status in Bordeaux showed a decrease in the prevalence of overweight between 2004 and 2010 in middle to high socioeconomic status areas, while the prevalence was stable in low socioeconomic status areas [35]. Thus, these results do not appear to be isolated. On the other hand, the prevalence of overweight and obesity among Chinese preschool children increased from 2006 to 2010 and then stayed stable until 2014 among children aged 5–6 years [36].
Moreover, another cross-sectional survey, conducted in 2010 in seven European countries (Italy, Germany, the Netherlands, Romania, Bulgaria, Lithuania and Turkey), analysed 5206 school children aged 6-11 years and revealed relatively high prevalences of overweight (15.6%) and obesity (4.9%). This was mostly due to the Eastern European regions, where certain socio-demographic factors and lifestyles are associated with being overweight. This region also shows lower rates of overweight and obesity with better macro-economic indicators. There is a notable difference between Eastern and Western Europe: the proportion of overweight and obesity was 24.5% in Eastern Europe and 11.9% in Western Europe, with Romanian children having the highest prevalence of overweight (31.4%) and Italians the lowest (10.4%) [37].
Another study estimating worldwide trends in body mass index from 1957 to 2016 used 1,099 sources to provide data on 24.1 million participants aged 5–17 years from 200 countries and cities to show that the global age-standardised prevalence of obesity increased from 0.7% (95% CI 0.4–1.2) in 1975 to 5.6% (95% CI 4.8–6.5) in 2016 in girls, and from 0.9% (95% CI 0.5–1.3) in 1975 to 7.8% (95% CI 6.7–9.1) in 2016 in boys. In 2016, 50 (95% credible interval 24–89) million girls and 74 (95% credible interval 39–125) million boys worldwide were estimated to be obese [16].
Our study has some limitations. First of all, children attending private schools in the canton of Geneva were not included in the study because the School Health Service of Geneva does not have the mandate to carry out health controls in private schools. Secondly, our study only focuses on one particular age group and is thus not representative of all children in the canton of Geneva. There is also a paucity of studies on overweight and obesity in 5- to 6-year-old schoolchildren around the world, and particularly in Switzerland, which limits our ability to compare our results. Thirdly, we used BMI as a measure of adiposity. This measure has been criticised in children because it is less sensitive than skinfold thickness or other methods to estimate body fat and lacks internationally accepted definitions of overweight and obesity in children. However, it does help to provide internationally comparable prevalence rates of overweight and obesity in children. Fourthly, we used the IOTF reference values which, according to the studies carried out by Zimmerman et al. [38], who validated the accuracy of the BMI reference values of the Centers for Disease Control and Prevention (CDC) [39] and the criteria of the International Obesity Task Force (IOTF) in classifying adiposity in children in Switzerland, give an underestimation of the values for obesity in these children. They showed that both the IOTF and the CDC criteria have high sensitivity and specificity for predicting overweight. For obesity, however, it is preferable to take into account the CDC criteria, which have a higher sensitivity and specificity for predicting obesity than the IOTF criteria. Finally, it is obviously difficult to identify the causality of fat accumulation and the imbalance between energy intake and expenditure with this kind of study. To do that would require an epidemiologic, analytical design.
These results are on the whole encouraging and tend to show that the trend is stabilising or even decreasing. Despite this promising observation, it still remains difficult to determine which factors have the greatest influence on this trend.
Environmental factors such as the food industry, social trends and the built environment have an important influence, but changes in these factors can be slow and are often strongly influenced by commercial interests and marketing.
From a behavioural standpoint, educational efforts must continue, whether in day care centres, in schools, in the population or for all the professionals involved with these issues.
If we hope to further decrease the proportion of young people affected by this issue, it could be time for them to stand up and manifest their disagreement with the heavily commercialised, profit-driven environment in which children's health does not seem to be a priority.
A "Greta Thunberg" kind of action by young people might create change, considering the difficulties national and international agencies have inducing changes in profit-driven environments. Boycotting products or companies has been shown to be effective in the past, and maybe we can use this approach to induce a change before it is too late.
A stabilisation and, to some extent, a decrease in overweight and obesity rates seem to be continuing, which is consistent with results from other Swiss cities, as well as other countries worldwide. Nevertheless, the best way to further reduce the problem is to continue monitoring BMI and to implement proven prevention strategies that influence energy intake and expenditure. If a further decrease in overweight and obesity becomes an objective, more aggressive approaches might be necessary.
Evidence-based approaches consisting of multi-component interventions – such as structured physical activity programmes, physical education lessons, the integration of physical activity into the school curriculum, promoting active transport to school, after-school sport programmes, sport in activity breaks, healthy lifestyle education, improving healthy eating, modifying school meals to increase the intake of fruit and vegetables, discouraging sugar-sweetened drinks, and behavioural and cognitive psychological interventions – seem to be more successful than single-component interventions for weight management [40–42]. A systematic Cochrane review indicated a small effect, but estimated that a large number of children and adolescents could benefit from these interventions [41]. In addition, a meta-analysis by Mahmood et al. [43] showed a statistically significant beneficial effect of school-based intervention programmes on the prevalence of obesity. They found that the interventions had a relative risk of 0.58 (RR 0.43 to 0.78), suggesting that a 42% reduction in the prevalence of obesity among schoolchildren through school-based intervention programmes is possible [43]. The success or failure of interventions depends on multiple factors such as the duration of the interventions, the quality of the education or diet programmes and, more importantly, the adherence rates of schoolchildren to the interventions. To promote physical activity in a school, it is important to have a structured physical activity programme which is implemented by specialised and trained staff, as well as an increase in the number and quality of physical education lessons [40].
New approaches could prove useful and must be considered, since overweight and obesity levels seem to be stabilising despite current preventive measures. These could include a “Greta Thunberg” type of approach and the boycotting of products or companies by children and families.
Finally, it is important to help children develop healthy eating habits and to continue reducing sedentary lifestyles and increasing daily physical activity, as recommended by the World Health Organization (WHO), through a multimodal approach including parents, schools, the built environment, addressing income inequalities and the industry [5, 40].
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Wang Y , Lim H . The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int Rev Psychiatry. 2012;24(3):176–88. doi:.https://doi.org/10.3109/09540261.2012.688195
2WHO Taking action on childhood obesity report [Internet]. WHO. [cited 2019 Feb 26]. Available from: http://www.who.int/nutrition/publications/obesity/taking-action-childhood-obesity-report/en/
3Organisation européenne de coopération économique. Health at a glance 2017: OECD indicators. Paris: OECD; 2017.
4 Lobstein T , Jackson-Leach R , Moodie ML , Hall KD , Gortmaker SL , Swinburn BA , et al. Child and adolescent obesity: part of a bigger picture. Lancet. 2015;385(9986):2510–20. doi:.https://doi.org/10.1016/S0140-6736(14)61746-3
5 Nishtar S , Gluckman P , Armstrong T . Ending childhood obesity: a time for action. Lancet. 2016;387(10021):825–7. doi:.https://doi.org/10.1016/S0140-6736(16)00140-9
6WHO Obesity [Internet]. WHO. [cited 2019 May 26]. Available from: https://www.who.int/topics/obesity/en/
7 Eagle TF , Sheetz A , Gurm R , Woodward AC , Kline-Rogers E , Leibowitz R , et al. Understanding childhood obesity in America: linkages between household income, community resources, and children’s behaviors. Am Heart J. 2012;163(5):836–43. doi:.https://doi.org/10.1016/j.ahj.2012.02.025
8 Schrempft S , van Jaarsveld CHM , Fisher A , Herle M , Smith AD , Fildes A , et al. Variation in the Heritability of Child Body Mass Index by Obesogenic Home Environment. JAMA Pediatr. 2018;172(12):1153–60. doi:.https://doi.org/10.1001/jamapediatrics.2018.1508
9World Health Organization Commission on Ending Childhood Obesity. Report of the Commission on Ending Childhood Obesity. Geneva: World Health Organization; 2016.
10 Townshend T , Lake A . Obesogenic environments: current evidence of the built and food environments. Perspect Public Health. 2017;137(1):38–44. doi:.https://doi.org/10.1177/1757913916679860
11 Hoare E , Crooks N , Hayward J , Allender S , Strugnell C . Associations between combined overweight and obesity, lifestyle behavioural risk and quality of life among Australian regional school children: baseline findings of the Goulburn Valley health behaviours monitoring study. Health Qual Life Outcomes. 2019;17(1):16. doi:.https://doi.org/10.1186/s12955-019-1086-0
12 Sahoo K , Sahoo B , Choudhury AK , Sofi NY , Kumar R , Bhadoria AS . Childhood obesity: causes and consequences. J Family Med Prim Care. 2015;4(2):187–92. doi:.https://doi.org/10.4103/2249-4863.154628
13Comorbidities and complications of obesity in children and adolescents - UpToDate [Internet]. [cited 2019 May 25]. Available from: https://www.uptodate.com/contents/comorbidities-and-complications-of-obesity-in-children-and-adolescents/print?search=childhood%20obesityy&topicRef=5874&source=see_link
14 Black N , Hughes R , Jones AM . The health care costs of childhood obesity in Australia: An instrumental variables approach. Econ Hum Biol. 2018;31:1–13. doi:.https://doi.org/10.1016/j.ehb.2018.07.003
15 Sonntag D , Ali S , Lehnert T , Konnopka A , Riedel-Heller S , König H-H . Estimating the lifetime cost of childhood obesity in Germany: Results of a Markov Model. Pediatr Obes. 2015;10(6):416–22. doi:.https://doi.org/10.1111/ijpo.278
16 Abarca-Gómez L , Abdeen ZA , Hamid ZA , Abu-Rmeileh NM , Acosta-Cazares B , Acuin C , et al.; NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–42. doi:.https://doi.org/10.1016/S0140-6736(17)32129-3
17 Pérez-Rodrigo C , Aranceta J . School-based nutrition education: lessons learned and new perspectives. Public Health Nutr. 2001;4(1A):131–9. doi:.https://doi.org/10.1079/PHN2000108
18 Jeannot E , Mahler P , Elia N , Cerruti B , Chastonnay P . Sociodemographic and Economic Determinants of Overweight and Obesity for Public-school Children in Geneva State, Switzerland: A Cross-sectional Study. Int J Prev Med. 2015;6(1):39. doi:.https://doi.org/10.4103/2008-7802.156836
19World Health Organization. | Physical status: the use and interpretation of anthropometry [Internet]. [Cited 2019 Mar 25]. Available from: https://www.who.int/childgrowth/publications/physical_status/en/
20 Cole TJ , Bellizzi MC , Flegal KM , Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–3. doi:.https://doi.org/10.1136/bmj.320.7244.1240
21 Eknoyan G . Adolphe Quetelet (1796-1874)--the average man and indices of obesity. Nephrol Dial Transplant. 2008;23(1):47–51. doi:.https://doi.org/10.1093/ndt/gfm517
22 Jeannot E , Mahler P , Duperrex O , Chastonay P . Evolution of overweight and obesity among elementary school children in Geneva. Swiss Med Wkly. 2010;140:w13040. doi:.https://doi.org/10.4414/smw.2010.13040
23 Epstein LH , Paluch RA , Raynor HA . Sex differences in obese children and siblings in family-based obesity treatment. Obes Res. 2001;9(12):746–53. doi:.https://doi.org/10.1038/oby.2001.103
24 Wang VH , Min J , Xue H , Du S , Xu F , Wang H , et al. What factors may contribute to sex differences in childhood obesity prevalence in China? Public Health Nutr. 2018;21(11):2056–64. doi:.https://doi.org/10.1017/S1368980018000290
25 Murer SB , Saarsalu S , Zimmermann MB , Aeberli I . Pediatric adiposity stabilized in Switzerland between 1999 and 2012. Eur J Nutr. 2014;53(3):865–75. doi:.https://doi.org/10.1007/s00394-013-0590-y
26 Aeberli I , Henschen I , Molinari L , Zimmermann MB . Stabilization of the prevalence of childhood obesity in Switzerland. Swiss Med Wkly. 2010;140:w13046. doi:.https://doi.org/10.4414/smw.2010.13046
27 Aeberli I , Ammann RS , Knabenhans M , Molinari L , Zimmermann MB . Decrease in the prevalence of paediatric adiposity in Switzerland from 2002 to 2007. Public Health Nutr. 2010;13(6):806–11. doi:.https://doi.org/10.1017/S1368980009991558
28 Zimmermann MB , Gübeli C , Püntener C , Molinari L . Overweight and obesity in 6-12 year old children in Switzerland. Swiss Med Wkly. 2004;134(35-36):523–8.
29Monitoring comparative des données relatives au poids des enfants et des adolescent-e-s en Suisse [Internet]. Gesundheitsfoerderung.ch. [Cited 2019 Mar 20]. Available from: https://promotionsante.ch/assets/public/documents/fr/5-grundlagen/publikationen/ernaehrungbewegung/arbeitspapiere/Document_de_travail_041_PSCH_2017-09_- _Monitoring_IMC_comparatif.pdf
30 Olds T , Maher C , Zumin S , Péneau S , Lioret S , Castetbon K , et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int J Pediatr Obes. 2011;6(5-6):342–60. doi:.https://doi.org/10.3109/17477166.2011.605895
31Monitoring de l’IMC chez les enfants et les adolescent-e-s: des chiffres réjouissants [Internet]. Gesundheitsfoerderung.ch. [Cited 2019 May 26]. Available from: https://promotionsante.ch/qui-sommes-nous/medias/communiques-de-presse/article/monitoring-de-limc-chez-les-enfants-et-les-adolescent-e-s-des-chiffres-rejouissants.html
32Statistiques cantonales - République et canton de Genève [Internet]. [Cited 2019 Apr 7]. Available from: https://www.ge.ch/statistique/publications/welcome.asp?collec=date&mm1=01%2F01&aaaa1=2011&mm2=01%2F31&aaaa2=2011&collection=Donn%E9es+g%E9n%E9rales&serie=Bulletin+statistique&Rechercher=Rechercher
33Statistiques cantonales - République et canton de Genève, Bilan et état de la population du canton de Genève en 2018. [Internet]. [Cited 2019 Apr 12]. Available from:https://www.ge.ch/statistique/publications/welcome.asp?collec=date&mm1=03%2F01&aaaa1=2019&mm2=03%2F31&aaaa2=2019&collection=Informations+statistiques&serie=Toutes&Rechercher=Rechercher
34 Guessous I , Joost S , Jeannot E , Theler J-M , Mahler P , Gaspoz J-M ; GIRAPH Group. A comparison of the spatial dependence of body mass index among adults and children in a Swiss general population. Nutr Diabetes. 2014;4(3):e111. doi:.https://doi.org/10.1038/nutd.2014.8
35 Thibault H , Carriere C , Langevin C , Barberger-Gateau P , Maurice S . Evolution of overweight prevalence among 5-6-year-old children according to socio-economic status. Acta Paediatr. 2013;102(3):273–7. doi:.https://doi.org/10.1111/apa.12093
36 Xiao Y , Qiao Y , Pan L , Liu J , Zhang T , Li N , et al. Trends in the Prevalence of Overweight and Obesity among Chinese Preschool Children from 2006 to 2014. PLoS One. 2015;10(8):e0134466. doi:.https://doi.org/10.1371/journal.pone.0134466
37 Olaya B , Moneta MV , Pez O , Bitfoi A , Carta MG , Eke C , et al. Country-level and individual correlates of overweight and obesity among primary school children: a cross-sectional study in seven European countries. BMC Public Health. 2015;15(1):475. doi:.https://doi.org/10.1186/s12889-015-1809-z
38 Zimmermann MB , Gübeli C , Püntener C , Molinari L . Detection of overweight and obesity in a national sample of 6-12-y-old Swiss children: accuracy and validity of reference values for body mass index from the US Centers for Disease Control and Prevention and the International Obesity Task Force. Am J Clin Nutr. 2004;79(5):838–43. doi:.https://doi.org/10.1093/ajcn/79.5.838
39 Kuczmarski RJ , Ogden CL , Grummer-Strawn LM , Flegal KM , Guo SS , Wei R , et al. CDC growth charts: United States. Adv Data. 2000;(314):1–27.
40 Messing S , Rütten A , Abu-Omar K , Ungerer-Röhrich U , Goodwin L , Burlacu I , et al. How Can Physical Activity Be Promoted Among Children and Adolescents? A Systematic Review of Reviews Across Settings. Front Public Health. 2019;7:55. doi:.https://doi.org/10.3389/fpubh.2019.00055
41 Martin A , Saunders DH , Shenkin SD , Sproule J . Lifestyle intervention for improving school achievement in overweight or obese children and adolescents. Cochrane Database Syst Rev. 2014;(3):CD009728. doi:.https://doi.org/10.1002/14651858.CD009728.pub2
42 Shaw K , O’Rourke P , Del Mar C , Kenardy J . Psychological interventions for overweight or obesity. Cochrane Database Syst Rev. 2005;(2):CD003818. doi:.https://doi.org/10.1002/14651858.CD003818.pub2
43 Mahmood S , Perveen T , Dino A , Ibrahim F , Mehraj J . Effectiveness of school-based intervention programs in reducing prevalence of overweight. Indian J Community Med. 2014;39(2):87–93. doi:.https://doi.org/10.4103/0970-0218.132724
No financial support and no other potential conflict of interest relevant to this article was reported.