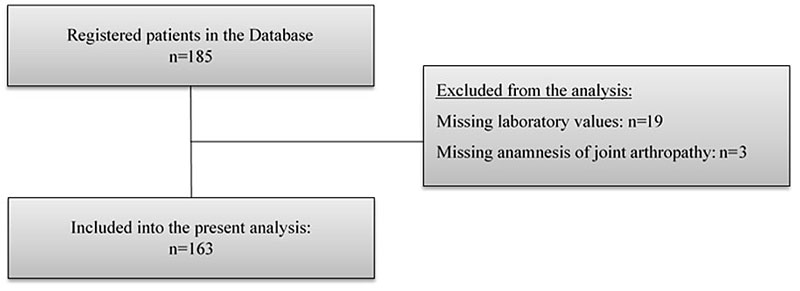
Figure 1 Flow diagram of the Swiss Haemochromatosis Cohort.
DOI: https://doi.org/10.4414/smw.2020.20294
Classic hereditary haemochromatosis is an autosomal recessive iron overload disorder associated with mutation of the HFE gene, located on chromosome 6. In the most cases, the mutation is a change of a single base resulting in the substitution of tyrosine for cysteine at position 282 of the HFE protein (human homeostatic iron regulator protein, high Fe2+ protein). All persons who are homozygous for the C282Y mutation are genetically predisposed to a chain of events that may culminate in severe damage to multiple organs. In the Caucasian population, the prevalence of homozygosity for the C282Y mutation is approximately 0.5% and the prevalence of heterozygosity about 10% [1–6].
The classic findings on presentation – diabetes, bronze skin and cirrhosis – were first described in the 19th century [7–9] and have become much rarer today thanks to increasingly early diagnosis [10]. Nowadays, the onset of symptoms occurs in middle-aged adults and symptoms are unspecific, such as fatigue and arthralgia, sometimes associated with slightly increased liver enzyme levels. In accordance with the diagnostic algorithm, patients suffering from hereditary haemochromatosis commonly present with increased serum ferritin levels and increased transferrin saturation values, suggesting iron accumulation in the tissues. In hereditary haemochromatosis, serum ferritin levels above 1000 ng/ml may indicate substantial liver disease in persons homozygous for the C282Y mutation, regardless of their age or serum liver enzyme levels [11, 12]. However, despite the wide range of end‐organ toxicities in haemochromatosis, patients are often diagnosed as a result of incidentally noted hyperferritinaemia without obvious organ damage [13]. Late complications such as liver cirrhosis, heart disease, hypogonadism, destructive arthritis, insulin-dependent diabetes and hepatocellular carcinoma cannot be reversed, although their progression can be slowed. Therefore, early diagnosis is important for prognosis of the patients.
In general, a screening for hereditary haemochromatosis is theoretically attractive: in Caucasians, the disease is highly prevalent and potentially fatal if untreated. Also, a safe, effective and cheap symptomatic treatment is available in form of phlebotomy. By simply measuring serum ferritin levels or transferrin saturation, indications of the disorder can be found, but unfortunately routine testing is uncommon in the preclinical setting [10, 14].
Thus, we aimed to identify iron overload-associated symptoms and typical findings in patients with hereditary haemochromatosis which might help to facilitate detection and diagnosis in daily clinical routine.
This study reports data from the Swiss Haemochromatosis Cohort (SHC). The detailed methods of the longitudinal observational study of the SHC have already been published [6]. The study was conducted in accordance with the principles of the Declaration of Helsinki; approval was obtained from the Ethics Committee of the Canton of Zurich, Switzerland, (KEK 2010-0364).
The main methods are summarised here.
We contacted the patients during routine clinical visits at the University Hospital Zurich, Hospital Linth or via the Swiss haemochromatosis patient’s organisation, and suggested that they participate in this study. The patients included in this analysis were diagnosed between 1971 and 2019. The patients had been initially diagnosed as having hereditary haemochromatosis on the basis of clinical, biochemical or histological signs of iron overload, or through family screening. Iron overload was defined as elevated serum ferritin (>300 mg/l for men, >200 mg/l for women) and/or elevated transferrin saturation (>50% for men, >45% for women). The diagnosis of hereditary haemochromatosis was genetically confirmed in all patients. Patients were registered in the Swiss haemochromatosis database, included in the prospective cohort and offered routine examinations including a clinical assessment, laboratory blood analyses and, if required, annual liver imaging using ultrasound. The following features were considered clinical manifestations of hereditary haemochromatosis: metacarpophalangeal arthropathy, upper ankle joint arthropathy, diabetes mellitus and hepatopathy, hypogonadism and cardiomyopathy. The presence of arthropathy was assessed by history and clinical examination. Hepatopathy was defined as either elevated liver enzymes (aspartate and/or alanine transaminase [AST/ALT] above the upper limit of 50 U/l) or positive liver histology. Positive liver histology was defined as portal-portal bridging fibrosis or cirrhosis, corresponding to grade 3 and 4 on a scoring system from 0 to 4 [6, 15, 16]. Cardiomyopathy was specified as either dilated or restrictive cardiomyopathy with documented cardiac iron overload. The diagnosis of hypogonadism was based on typical clinical characteristics in combination with low testosterone levels.
The following data were collected at the time of diagnosis of hereditary haemochromatosis and included into the present analysis: type of HFE gene mutation, age, sex, serum ferritin level, transferrin saturation, elevation of transaminases, histological result of liver biopsy (if available), serological testing for hepatitis B and C, and clinical manifestations. The following variables were recorded during the progress of the disease and extracted from the medical records for the present analysis: body mass index (BMI) and the self-reported amount of alcohol consumption. Considerable alcohol consumption was defined as intake of >20 g (men) or >10g (women) of ethanol per day. If patients were followed up by primary care physicians, their medical records were obtained for this study.
All patients received treatment with intensive phlebotomies from the time of diagnosis until depletion of iron stores, followed by maintenance phlebotomies where necessary.
Continuous variables are expressed as medians with the corresponding interquartile ranges (IQRs). If a normal distribution was found through Kolmogorov-Smirnov testing, variables were compared using Levene and t-tests; if a non-normal distribution was found, the unpaired Mann-Whitney U-test was used. Dichotomous variables are expressed as absolute numbers and percentages and were compared using the Fisher´s exact test or chi-square test, as appropriate, and categorical variables were compared using the Kruskal-Wallis test. Correlations between continuous variables were tested using Spearman’s rho, and results are presented as Spearman's coefficient r. The prognostic relevance of serum ferritin levels regarding the primary study endpoint of serum ferritin levels ≥1000 µg/ml was tested using univariable logistic regression analysis and results presented as odds ratios (ORs) with the corresponding 95% confidence intervals (95% CIs). Multiple logistic regression was used to assess for the independent effects of relevant variables on the outcome. A two-sided significance level of α <0.05 was defined to indicate statistical significance. All statistical analyses were performed using Statistics Package for Social Sciences (IBM SPSS Statistics, Version 26, IBM Corp. Armonk, NY).
From 185 patients included in the SHC database, 19 had to be excluded because of a missing serum ferritin value at diagnosis and 3 because of incomplete clinical data. Overall, 163 patients with genetically and clinically confirmed hereditary haemochromatosis were included in the present study (fig. 1). The baseline characteristics, clinical symptoms, laboratory values and initial findings are shown in table 1. The median age at the time of diagnosis was 48.0 years (IQR 37.0–57.0) and the cohort consisted of 54 (33.1%) female patients. The mutations were known in all patients, 148 (90.8%) were C282Y homozygous and 15 (9.2%) C282Y/H63D compound heterozygous. Median serum ferritin levels on admission were of 1218.0 µg/ml (IQR 624.0–2128.0). Liver disease was present in 84 (51.5%) patients at diagnosis and arthropathy complaints in 88 (54.0%). Cardiomyopathy (n = 3; 1.8%), diabetes mellitus (n = 13; 8.0%) and hypogonadism (n = 11; 6.8%) were infrequent in the cohort.
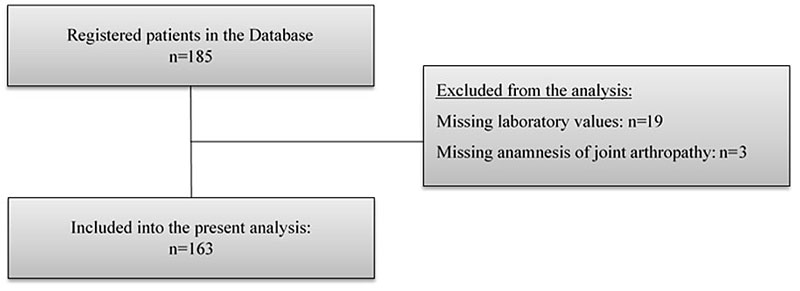
Figure 1 Flow diagram of the Swiss Haemochromatosis Cohort.
Table 1 Baseline characteristics, symptoms and laboratory measurements for patients with hereditary haemochromatosis included in the present analysis.
|
All
(n = 163) |
|
|---|---|
| Age (years), median (IQR) | 48.0 (37.0–57.0) |
| Sex (female), n (%) | 54 (33.1) |
| Body mass index (kg/m2), median (IQR) | 23.9 (21.7 - 26.5) n = 159 |
| Alcohol intake*, n (%) | 36 (22.1) |
| HFE mutations | |
| – C282Y homozygote, n (%) | 148 (90.8) |
| – C282Y/H63D compound heterozygote, n (%) | 15 (9.2) |
| Serum ferritin (µg/ml), median (IQR) | 1218.0 (624.0–2128.0) |
| Transferrin saturation (%), median (IQR) | 85.0 (67.0–94.1) n = 113 |
| Liver disease†, n (%) | 84 (51.5) |
| – Elevated liver enzymes‡, n (%) | 78 (49.7) n = 157 |
| – Liver fibrosis on biopsy§, n (%) | 34 (53.1) n = 64 |
| Arthropathy (total), n (%) | 88 (54.0) |
| Cardiomyopathy, n (%) | 3 (1.8) |
| Diabetes mellitus, n (%) | 13 (8.0) |
| Hypogonadism, n (%) | 11 (6.8) |
* Defined as consumption of more than 1 standard drink (10g ethanol) per day for women and >2 standard drinks for men † Cirrhosis or severe, portal-portal bridging fibrosis in biopsy and/or elevated liver enzymes ‡ aspartate and/or alanine aminotransferase >50 U/l § Either cirrhosis or severe, portal-portal bridging fibrosis
To determine the risk factors for higher serum ferritin levels in the cohort, we divided the study population in two groups according to serum ferritin levels ≥1000 µg/ml on admission, based on previous studies [17]. Baseline characteristics, symptoms and clinical findings are shown and compared in table 2. Of 163 patients included in the study, 89 (54.6%) presented with serum ferritin levels ≥1000 µg/ml.
Table 2 Baseline characteristics, symptoms and laboratory measurements of patients with hereditary haemochromatosis included in the present analysis stratified according to substantial iron overload.
|
Serum ferritin <1000 µg/ml
(n = 74) |
Serum ferritin ≥1000 µg/ml
(n = 89) |
p-value | |
|---|---|---|---|
| Age (years), median (IQR) | 46.5 (32.8–57.3) | 50.0 (43.0–57.0) | 0.054 |
| Sex (female), n (%) | 37 (50.0) | 17 (19.1) | <0.001 |
| Body mass index (kg/m2), median (IQR) | 23.3 (21.4–26.3) n = 72 |
24.4 (22.2–26.9) n = 87 |
0.215 |
| Alcohol intake*, n (%) | 17 (23.0) | 19 (21.4) | 0.803 |
| HFE mutations | |||
| – C282Y homozygote, n (%) | 61 (82.4) | 87 (97.8) | 0.001 |
| – C282Y/H63D compound heterozygote, n (%) | 13 (17.6) | 2 (2.2) | 0.001 |
| Serum ferritin (µg/ml), median (IQR) | 590.0 (377.0–806.0) | 2000.0 (1529.0–3659.0) | <0.001 |
| Transferrin saturation (%), median (IQR) | 78.0 (57.5–91.9) n = 53 |
89.2 (79.9 – 94.5) n = 60 |
0.014 |
| Liver disease†, n (%) | 15 (20.3) | 69 (77.5) | <0.001 |
| – AST >50 U/l, n (%) | 4 (6.4) n = 63 |
33 (40.2) n = 82 |
<0.001 |
| – ALT >50 U/l, n (%) | 15 (20.8) n = 72 |
61 (72.6) n = 84 |
<0.001 |
| – Liver fibrosis in biopsy‡, n (%) | 15 (53.6) n = 28 |
19 (52.8) n = 36 |
0.950 |
| Arthropathy (total), n (%) | 30 (40.5) | 58 (65.2) | 0.002 |
| – MCP joint, n (%) | 17 (23.0) | 46 (51.7) | <0.001 |
| – Elbow joint, n (%) | 2 (2.7) | 8 (9.0) | 0.113 |
| – Upper ankle joint, n (%) | 8 (10.8) | 27 (30.4) | 0.003 |
| – Hip joint, n (%) | 12 (16.2) | 19 (21.3) | 0.406 |
| – Knee joint, n (%) | 10 (13.5) | 15 (16.9) | 0.556 |
| Cardiomyopathy, n (%) | 2 (2.7) | 1 (1.1) | 0.591 |
| Diabetes mellitus, n (%) | 2 (2.7) | 11 (12.3) | 0.039 |
| Hypogonadism, n (%) | 3 (4.1) | 8 (9.0) | 0.348 |
AST = aspartate aminotransferase; ALT = alanine aminotransferase; MCP = metacarpophalangeal * Defined as consumption of more than 1 standard drink (10g ethanol) per day for women and >2 standard drinks for men † Cirrhosis or severe, portal-portal bridging fibrosis in biopsy and/or elevated liver enzymes ‡ Either cirrhosis or severe, portal-portal bridging fibrosis
Patients with higher serum ferritin levels were significantly more frequently male (37 [59.0%] vs 72 [80.1%]; p <0.001), less frequently had the C28Y/H63D compound heterozygous mutation (13 [17.6%] vs 2 [2.2%]; p <0.001), had higher liver enzymes (AST >50 U/l: 4 [6.4%] vs 33 [40.2%]; p <0.001 and ALT >50 U/l: 15 [20.8%] vs 61 [72.6%]; p <0.001) and more often joint arthropathy (30 [40.5%] vs 58 [65.2%]; p = 0.002), especially metacarpophalangeal arthropathy (17 [23.0%] vs 46 [51.7%]; p <0.001) and upper ankle joint arthropathy (8 [10.8%] vs 27 [30.4%]; p = 0.003), whereas there was no significant difference for elbow, hip and knee arthropathy.
Several predictors for the primary endpoint of serum ferritin levels ≥1000 µg/ml could be identified in regression analysis: elevated liver enzymes and arthropathy, respectively, were associated with a 9.4-fold (95% CI 4.5- to 19.6-fold; p <0.001) and 2.7-fold (95% CI 1.5- to 5.2-fold; p = 0.002) increased risk for serum ferritin levels ≥1000 µg/ml. ALT levels >50 U/l (10.1, 95% CI 4.8–21.2; p <0.001) and AST levels >50 U/l (9.9, 95% CI 3.2–30.0; p < 0.001), as well as metacarpophalangeal joint arthropathy (3.6, 95% CI 1.8–7.1; p <0.001), upper ankle joint arthropathy (3.6, 95% CI 1.5–8.5; p = 0.004) and diabetes mellitus (5.1, 95% CI 1.1–23.7; p <0.039) were significant predictors for the primary endpoint of serum ferritin levels ≥1000 µg/ml. Cardiomyopathy (0.3, 95% CI 0.0–3.8, p = 0.356) and hypogonadism (2.6, 95% CI 0.6–10.8; p = 0.181) were not associated with hereditary haemochromatosis.
To assess for the independent effects of the most relevant variables associated with serum ferritin levels ≥1000 µg/ml, we performed multiple logistic regression analyses. Through stepwise testing, we identified ALT levels >50 U/l and metacarpophalangeal joint arthropathy as the most common findings associated with iron overload. Both remained the only parameters highly significant throughout multiple logistic regression and multiple logistic regression adjusted for age, sex and BMI. The results are shown in table 3. Interestingly, elevated ALT levels >50 U/l were also found in 15 (20.8%) patients and metacarpophalangeal joint arthropathy in 17 (23.0%) patients with serum ferritin levels <1000 µg/ml; see also table 2 .
Table 3 Univariate and multiple logistic regression analysis comparing patients with substantial iron overload (serum ferritin levels >1000 ng/ml).
|
Exp B (95% CI)
p-value |
|||
|---|---|---|---|
| Univariate logistic regression | Multivariate logistic regression | Multivariate logistic regression adjusted for age, sex and BMI* | |
| Elevated ALT >50 U/l | 10.08 (4.79–21.21) <0.001 |
10.22 (6.67–22.38) <0.001 |
12.43 (5.01–30.83) <0.001 |
| MCP joint arthropathy | 3.59 (1.81–7.10) <0.001 |
3.94 (1.75–8.90) 0.001 |
3.63 (1.42–9.29) 0.007 |
ALT = alanine aminotransferase; BMI = body mass index; CI = confidence interval; MCP = metacarpophalangeal * Values for age, sex and BMI not shown
In this study analysing the prospective Swiss haemochromatosis cohort including 163 genetically confirmed hereditary haemochromatosis patients with a complete clinical and laboratory assessment at the time of the diagnosis, including measured serum ferritin levels, only elevated ALT and metacarpophalangeal arthropathy remained independently associated with elevated ferritin levels in haemochromatosis and should therefore be considered by clinicians as important signs indicating substantial iron overload. Elevated ALT and metacarpophalangeal arthropathy were already found in patients without substantial iron overload, so they might be helpful in the timely diagnosis of hereditary haemochromatosis. Importantly, both elevated ALT and metacarpophalangeal arthropathy can also be late findings in a patient with hereditary haemochromatosis. This fact has potential implications for the likelihood of advanced complications of the disease. Thus, serum ferritin levels should be evaluated in order to estimate the degree of iron overload and to stratify the individual risk for the hereditary haemochromatosis patient.
Early diagnosis, monitoring and initiation of phlebotomy treatment benefits the course of the disease, preventing or at least slowing organ damage such as liver cirrhosis and hepatocellular carcinoma, as already reported [6, 18]. In a previous study of our hereditary haemochromatosis cohort, we found that 9% of the patients developed hepatocellular carcinoma during the mean follow-up time of 14 years. We found that higher age at diagnosis showed the strongest association with the occurrence of hepatocellular carcinoma in Swiss haemochromatosis patients [6]. However, early diagnosis can be challenging because disease manifestations can vary from asymptomatic patients, in whom the disease is discovered randomly in connection with routine blood sampling, to unspecific symptoms, such as fatigue, arthralgia, abdominal pain and potency problems in early disease stages [19]. Early studies emphasised focusing on clinical signs of advanced iron overload with liver cirrhosis, restrictive cardiomyopathy, diabetes mellitus and progressive skin pigmentation, also called bronze diabetes [20]. Since then these manifestations have become rarer as the time to diagnosis has shortened owing to increased disease awareness by medical doctors and, partly, to screening programmes [17]. Also, in our large real-life time cohort, we found a low prevalence of cardiomyopathy, diabetes mellitus and hypogonadism.
A late diagnosis based on presentation of overt iron overload leads to a delayed therapy initiation, which results in irreversible organ damage [6, 18]. Thus, clinicians need to be aware of signs and symptoms that raise suspicion of hereditary haemochromatosis, which then can be further elucidated by the measurement of iron indices and genetic testing for the HFE mutations. Ideally, these signs and symptoms should be routine, easy-to-assess and cheap to measure. We found that metacarpophalangeal joint arthropathy and elevated ALT, both broadly assessed in a routine medical examination, have the potential to point to the correct diagnosis. Importantly, joints are frequently affected by hereditary haemochromatosis, and this significantly decreases quality of life and increases the risk for need of joint replacement [21]. A clinically characteristic arthropathy develops in two thirds of patients with hereditary haemochromatosis and presents as arthritis of the second and third metacarpophalangeal joints, which appears similar to osteoarthritis or, more rarely, rheumatoid arthritis [22, 23]. The mechanisms behind a pronounced involvement of the metacarpophalangeal joints, which usually starts in the second and third joints with subsequent bony enlargement, is still not completely understood. On one hand, iron deposition in joints may lead to intra-articular production of reactive oxygen species, particularly the superoxide anion, which causes cartilage inflammation and degeneration [24, 25]. Additionally, the crystal ferric salt deposition stimulates intra-articular calcium pyrophosphate production, which further accelerates the inflammatory and degenerative processes [23, 26]. On the other hand, because humans intensively use their hands, the metacarpophalangeal joints are particularly frequently strained. This can lead to cumulative attrition and increasing inflammation of these joints during the lifetime in patients with this inherited disease.
These studies are limited by the fact that not all hereditary haemochromatosis patients develop arthropathy, which somewhat limits the sensitivity of the clinical joint examination for diagnosis [22]. On the other hand, metacarpophalangeal arthropathy appeared in our cohort to be a finding highly specific for hereditary haemochromatosis.
The strength of these studies is that we analysed a large, prospective, nation-wide, well-defined cohort of hereditary haemochromatosis patients, all with a genetically proven diagnosis, and included patients not only from a tertiary care centre, but also from primary care. Thus, we consider the cohort to reflect adequately the clinical picture of hereditary haemochromatosis encountered in daily practice. Furthermore, we assessed patients regularly, and collected complete clinical, biochemical, genetic and phenotypic information. However, the present study is a simple association study without a control group and does not give an answer to which patients are “truly” suffering from hereditary haemochromatosis at initial presentation. The diagnosis of hereditary haemochromatosis was based on the known algorithm for the diagnosis of hereditary haemochromatosis. Our analyses included patients with iron overload disease due to hereditary haemochromatosis and an HFE mutation. We did not test or compare data from other primary types of hereditary haemochromatosis or other secondary iron overload diseases such as thalassaemia. Other studies are needed to determine whether elevated ALT levels and metacarpophalangeal arthropathy are also associated with iron overload in those patients.
In conclusion, the results of the present observational study found elevated liver enzymes and small joint arthropathy to be associated with iron overload. Especially elevated ALT levels and metacarpophalangeal joint arthropathy are parameters easy to determine at low cost to identify patients with significant iron overload and therefore at risk for hereditary haemochromatosis.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Edwards CQ , Griffen LM , Goldgar D , Drummond C , Skolnick MH , Kushner JP . Prevalence of hemochromatosis among 11,065 presumably healthy blood donors. N Engl J Med. 1988;318(21):1355–62. doi:.https://doi.org/10.1056/NEJM198805263182103
2 Feder JN , Gnirke A , Thomas W , Tsuchihashi Z , Ruddy DA , Basava A , et al. A novel MHC class I-like gene is mutated in patients with hereditary haemochromatosis. Nat Genet. 1996;13(4):399–408. doi:.https://doi.org/10.1038/ng0896-399
3 Merryweather-Clarke AT , Pointon JJ , Jouanolle AM , Rochette J , Robson KJ . Geography of HFE C282Y and H63D mutations. Genet Test. 2000;4(2):183–98. doi:.https://doi.org/10.1089/10906570050114902
4 Asberg A , Hveem K , Thorstensen K , Ellekjter E , Kannelønning K , Fjøsne U , et al.; A. Åsberg, K. Hveem, K. Thorstensen. Screening for hemochromatosis: high prevalence and low morbidity in an unselected population of 65,238 persons. Scand J Gastroenterol. 2001;36(10):1108–15. doi:.https://doi.org/10.1080/003655201750422747
5 Beutler E , Felitti VJ , Koziol JA , Ho NJ , Gelbart T . Penetrance of 845G--> A (C282Y) HFE hereditary haemochromatosis mutation in the USA. Lancet. 2002;359(9302):211–8. doi:.https://doi.org/10.1016/S0140-6736(02)07447-0
6 Nowak A , Giger RS , Krayenbuehl PA . Higher age at diagnosis of hemochromatosis is the strongest predictor of the occurrence of hepatocellular carcinoma in the Swiss hemochromatosis cohort: A prospective longitudinal observational study. Medicine (Baltimore). 2018;97(42):e12886. doi:.https://doi.org/10.1097/MD.0000000000012886
7Trousseau A. Glycosurie, diabete sucré. Clinique Médical de l'Hôtel-Dieu de Paris, 2nd edn, vol 2. Paris: Baillière; 1865. p 663–98.
8 Troisier M . Diabète sucré. Bull Soc Anat Paris. 1871;44:231–5.
9 von Recklinghausen F . Uber hāmochromatose. Tageblatt der (62). Versammlung Deutsch Naturforscher und Arzte in Heidelberg. 1889;62:324–5.
10 Pietrangelo A . Hereditary hemochromatosis--a new look at an old disease. N Engl J Med. 2004;350(23):2383–97. doi:.https://doi.org/10.1056/NEJMra031573
11 Guyader D , Jacquelinet C , Moirand R , Turlin B , Mendler MH , Chaperon J , et al. Noninvasive prediction of fibrosis in C282Y homozygous hemochromatosis. Gastroenterology. 1998;115(4):929–36. doi:.https://doi.org/10.1016/S0016-5085(98)70265-3
12 Morrison ED , Brandhagen DJ , Phatak PD , Barton JC , Krawitt EL , El-Serag HB , et al. Serum ferritin level predicts advanced hepatic fibrosis among U.S. patients with phenotypic hemochromatosis. Ann Intern Med. 2003;138(8):627–33. doi:.https://doi.org/10.7326/0003-4819-138-8-200304150-00008
13 Senjo H , Higuchi T , Okada S , Takahashi O . Hyperferritinemia: causes and significance in a general hospital. Hematology. 2018;23(10):817–22. doi:.https://doi.org/10.1080/10245332.2018.1488569
14 Adams P , Brissot P , Powell LW . EASL International Consensus Conference on Haemochromatosis. J Hepatol. 2000;33(3):487–504. doi:.https://doi.org/10.1016/S0168-8278(01)80874-6
15 Bedossa P , Bioulac-Sage P , Callard P ; The French METAVIR Cooperative Study Group. Intraobserver and interobserver variations in liver biopsy interpretation in patients with chronic hepatitis C. Hepatology. 1994;20(1 Pt 1):15–20.
16 Batts KP , Ludwig J . Chronic hepatitis. An update on terminology and reporting. Am J Surg Pathol. 1995;19(12):1409–17. doi:.https://doi.org/10.1097/00000478-199512000-00007
17 Allen KJ , Gurrin LC , Constantine CC , Osborne NJ , Delatycki MB , Nicoll AJ , et al. Iron-overload-related disease in HFE hereditary hemochromatosis. N Engl J Med. 2008;358(3):221–30. doi:.https://doi.org/10.1056/NEJMoa073286
18 Niederau C , Fischer R , Sonnenberg A , Stremmel W , Trampisch HJ , Strohmeyer G . Survival and causes of death in cirrhotic and in noncirrhotic patients with primary hemochromatosis. N Engl J Med. 1985;313(20):1256–62. doi:.https://doi.org/10.1056/NEJM198511143132004
19 Milman NT , Schioedt FV , Junker AE , Magnussen K . Diagnosis and Treatment of Genetic HFE-Hemochromatosis: The Danish Aspect. Gastroenterol Res. 2019;12(5):221–32. doi:.https://doi.org/10.14740/gr1206
20 Yang Q , McDonnell SM , Khoury MJ , Cono J , Parrish RG . Hemochromatosis-associated mortality in the United States from 1979 to 1992: an analysis of Multiple-Cause Mortality Data. Ann Intern Med. 1998;129(11):946–53. doi:.https://doi.org/10.7326/0003-4819-129-11_Part_2-199812011-00005
21 Wijarnpreecha K , Aby ES , Panjawatanan P , Kroner PT , Harnois DM , Palmer WC , et al. Hereditary hemochromatosis and risk of joint replacement surgery: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2020. Epub ahead of print. doi:.https://doi.org/10.1097/MEG.0000000000001704
22 Sahinbegovic E , Dallos T , Aigner E , Axmann R , Manger B , Englbrecht M , et al. Musculoskeletal disease burden of hereditary hemochromatosis. Arthritis Rheum. 2010;62(12):3792–8. doi:.https://doi.org/10.1002/art.27712
23 Adamson TC, 3rd , Resnik CS , Guerra J, Jr , Vint VC , Weisman MH , Resnick D . Hand and wrist arthropathies of hemochromatosis and calcium pyrophosphate deposition disease: distinct radiographic features. Radiology. 1983;147(2):377–81. doi:.https://doi.org/10.1148/radiology.147.2.6300958
24 Afonso V , Champy R , Mitrovic D , Collin P , Lomri A . Reactive oxygen species and superoxide dismutases: role in joint diseases. Joint Bone Spine. 2007;74(4):324–9. doi:.https://doi.org/10.1016/j.jbspin.2007.02.002
25 Henrotin Y , Kurz B , Aigner T . Oxygen and reactive oxygen species in cartilage degradation: friends or foes? Osteoarthritis Cartilage. 2005;13(8):643–54. doi:.https://doi.org/10.1016/j.joca.2005.04.002
26 Hearn PR , Russell RG . Formation of calcium pyrophosphate crystals in vitro: implications for calcium pyrophosphate crystal deposition disease (pseudogout). Ann Rheum Dis. 1980;39(3):222–7. doi:.https://doi.org/10.1136/ard.39.3.222
Contributed equally
No financial support and no other potential conflict of interest relevant to this article was reported.