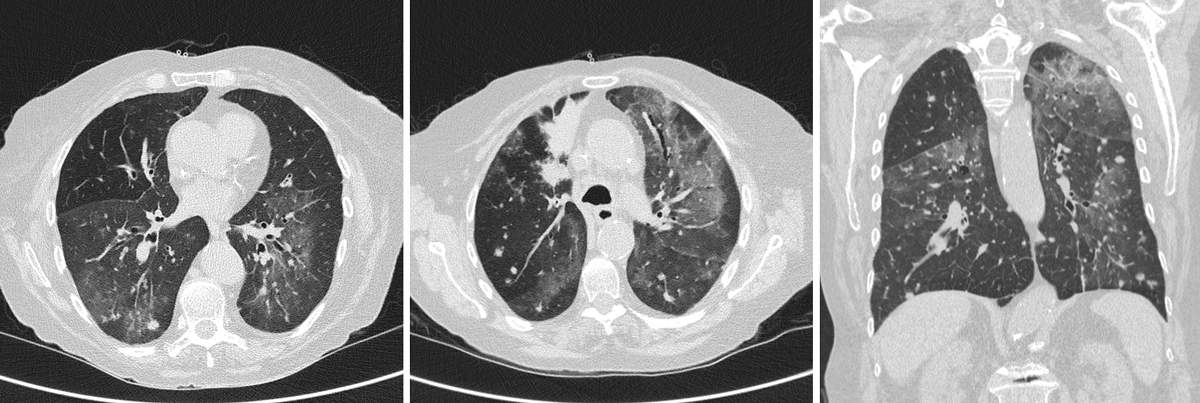
Figure 1 Coronary and sagittal ultralow-dose chest CT scan showing diffuse bilateral ground-glass opacities and multiple bilateral nodules.
DOI: https://doi.org/10.4414/smw.2020.20312
The SARS-CoV2 infection has rapidly spread through Southern Switzerland, with 3327 reported cases, 350 fatalities and a cumulative prevalence of 94.2/10,000 cases reported as of 26 June 2020 [1]. We present the case of a patient admitted to hospital with interstitial pneumonia who had the clinical and radiological features of COVID-19 infection, but after further investigation a different pathogen was identified, highlighting the importance of a thorough diagnostic work-up. With this case report we would like to present the diagnostic challenges faced during a pandemic when patients present with symptoms similar to those of the pandemic infection.
We aimed to highlight the importance of a thorough differential diagnosis even during a pandemic.
The patient was a 77-year-old female patient with progressive stage IV lung adenocarcinoma (biopsy on 5 September 2019 showed: non-small cell lung cancer with bilateral lung nodules; G12A mutation of KRAS 2; EGFR, BRAF and HER2 without mutation; no membrane expression of programmed cell death ligand [PD-L]), advanced chronic obstructive pulmonary disease (COPD), KDIGO stage IIIB chronic renal disease and recent bilateral pulmonary embolism. She started an immuno-chemotherapy regime with carboplatin/pemetrexed and pembrolizumab. Her drug therapy included inhaled bronchodilators, moderate-dose prednisone for frequent COPD exacerbations and oral anticoagulation.
The patient was admitted to our hospital on 31 March 2020 with fever, cough and severe dyspnoea after 7 days of antibiotic treatment with levofloxacin for a suspected community-acquired pneumonia. On arrival, she was dyspnoeic with an oxygen saturation of 85% on room air. On clinical examination there was diffuse wheezing with bilateral crackles at the lung bases. Blood tests identified lymphopenia (0.5 × 109/l), elevated C-reactive protein of 62 mg/l and negative procalcitonin. We tested swabs for influenza A and B and respiratory syncytial virus, and urine for pneumococcus and Legionella pneumophila antigens, which were negative. Ultralow-dose chest computed tomography (CT) identified diffuse bilateral ground-glass opacities and multiple bilateral nodules (fig. 1). As the clinical and the radiological findings were strongly suggestive of COVID-19, we tested multiple nasopharyngeal swabs for SARS-CoV-2, which were negative. We completed the diagnostic work-up with serological and polymerase chain reaction (PCR) testing of stool and induced sputum samples, which were all negative.
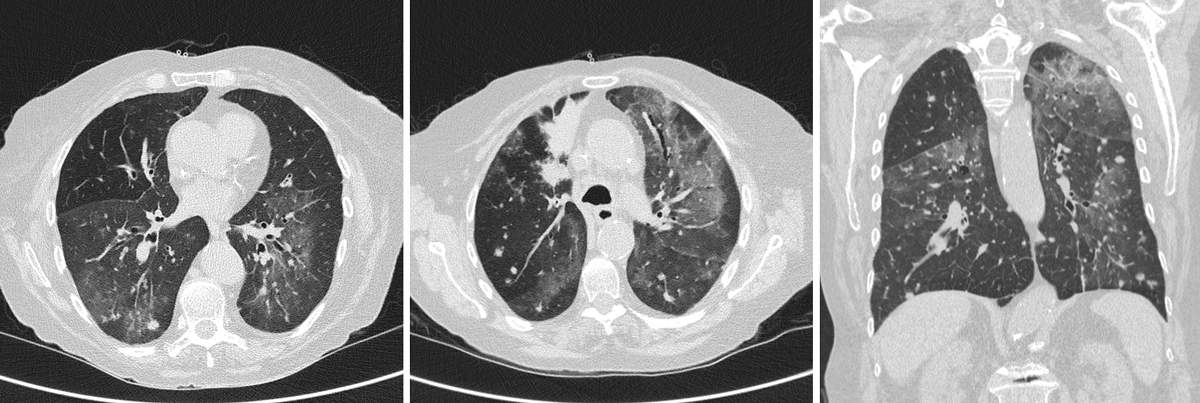
Figure 1 Coronary and sagittal ultralow-dose chest CT scan showing diffuse bilateral ground-glass opacities and multiple bilateral nodules.
Because of the prolonged immunosuppressive drug therapy (pemetrexed, pembrolizumab and moderate-dose prednisone), we included in the differential diagnosis other causes of interstitial pneumonia such as opportunistic infections. Human immunodeficiency virus (HIV) serology was negative. We evaluated the possibility of bronchoalveolar lavage, but because of an unfavourable risk-benefit ratio we opted for the less invasive induced sputum collection, in which semi-quantitative PCR detected a concentration higher than 105 copies of DNA per capillary of Pneumocystis jirovecii, above the established cut-off for significance [2]. Specific treatment was promptly initiated. Immunotherapy-induced pneumonia was also a possibility owing to the recent treatment with pembrolizumab, which was therefore stopped, although this differential diagnosis was unlikely.
The initial response to the treatment was encouraging, but after 1 week we witnessed a rapid deterioration due to progression of the lung adenocarcinoma, and after a multidisciplinary and family meeting, a best supportive care approach was chosen. The patient passed away on day 11 of the hospital stay. In this case we decided not to proceed with an autopsy even if the diagnosis was challenging as in the end we had a clear cause of death.
The clinical course during hospital admission is summarised in figure 2.
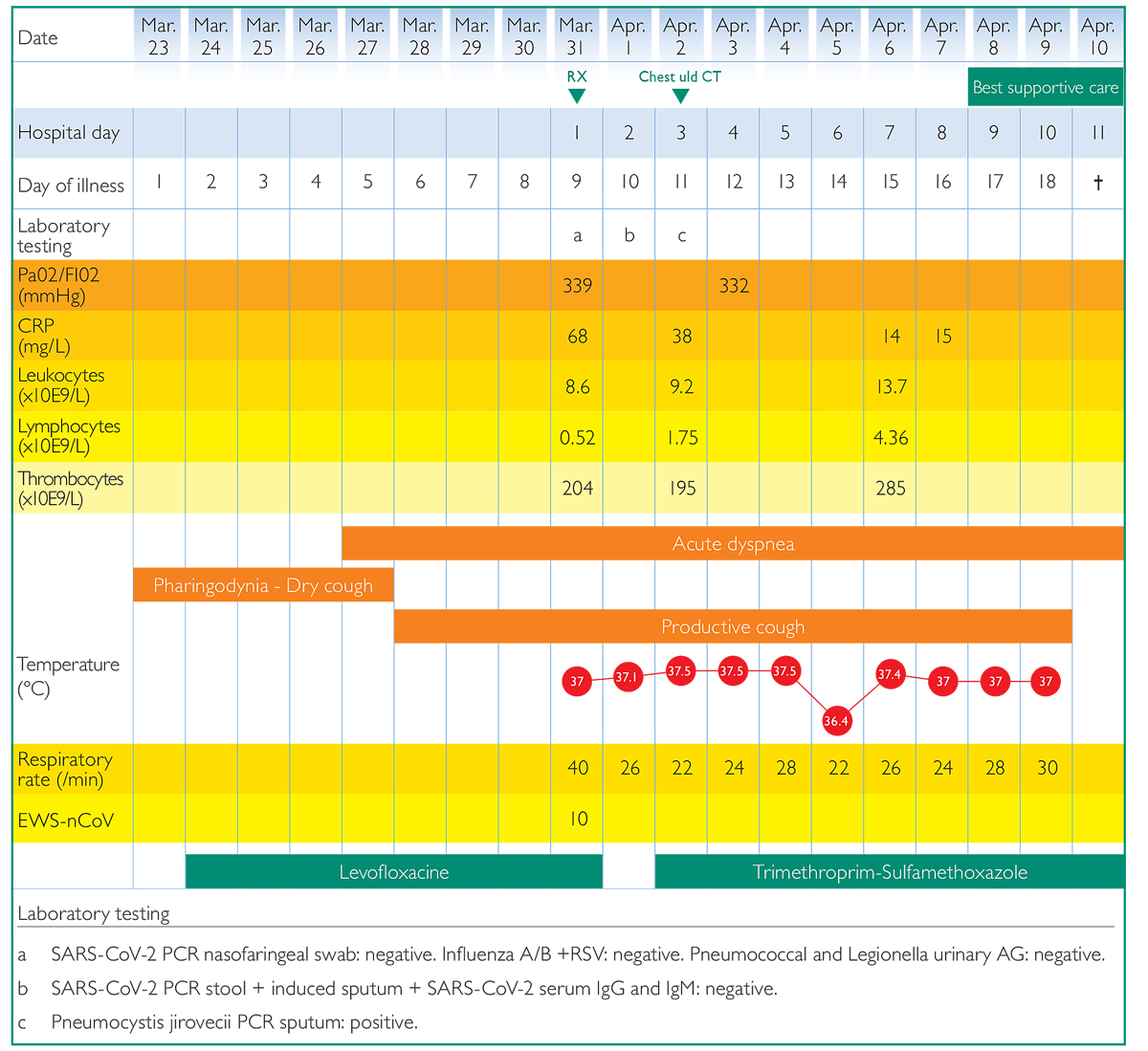
Figure 2 Clinical course during hospital admission, with details of signs and symptoms, laboratory findings, imaging and therapy received.
During the present pandemic many patients with clinical presentations similar to COVID-19 are seeking medical attention and there is a tendency to attribute one particular diagnosis to all patients. Since a pandemic is a challenging time for every doctor in the field, some guidelines for clinical practice have been created [3–5], although we still have so much to learn about this virus. Because of the peculiar situation in which we are living, sometimes patients are suspected of having SARS-CoV-2 infection even when their tests are negative. Our patient had a presentation of an interstitial pneumonia compatible with SARS-CoV-2 infection. The multiple negative tests for COVID-19 and the immunocompromised status pointed towards a different aetiology.
It is therefore of the outmost importance to remember the clinical reality of immunocompromised patients during the SARS-CoV-2 pandemic. P. jirovecii is a fungus causing pneumonia in humans and risk factors associated with this kind of infection are solid organ transplantation, HIV infection and administration of immune-modulatory drugs [6], whereas SARS-CoV-2 seems to affect patients regardless of their immune status [7]. Signs and symptoms present in both entities are fever, dry cough and dyspnoea. CT findings associated with P. jirovecii include diffuse bilateral ground-glass opacities, usually present in the mid to late stages of the disease, and giving a radiological appearance similar to SARS-CoV-2 [6, 8]. Both infections are associated with increased lactate dehydrogenase levels and lymphopenia [6, 8].
The radiological diagnosis of P. jirovecii can be problematic, since patterns of presentation are variable. It is important to stress that a differential diagnosis is key, not only because of the pandemic, but because we are still understanding the many faces of SARS-CoV-2 infection. Unfortunately the symptoms of SARS-CoV-2 are far from specific, as they are shared with many other frequent respiratory infections. Furthermore, this patient had already a difficult clinical picture involving the lungs (lung adenocarcinoma and COPD exacerbations), making it difficult to put things in the right perspective. The chest CT scan identified diffuse bilateral ground-glass opacities and multiple bilateral nodules. The clinical and radiological presentation of SARS-CoV-2 is common to different pathogens, so a better understanding of the CT scan and pathology findings will be key in developing more precise and reliable guidelines.
The importance of differential diagnostics in clinical practice should be a given, especially during times of pandemic. The novel coronavirus infection introduced new guidelines for and approaches to the investigation of immunocompromised patients, so it is especially important not to forget the basis of differential diagnosis, and adopt wise approach to these complex patients. This case report illustrates the importance of a thorough differential diagnosis even in the times of COVID-19 pandemic, since timely diagnosis and appropriate management may affect the outcome.
We wish to thank Dr Martina Baronio and Dr Adriana Tamburello for their technical support.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 COVID-19 information on Switzerland. https://www.corona-data.ch/. Cited on 2020 June 26.
2 Flori P , Bellete B , Durand F , Raberin H , Cazorla C , Hafid J , et al. Comparison between real-time PCR, conventional PCR and different staining techniques for diagnosing Pneumocystis jiroveci pneumonia from bronchoalveolar lavage specimens. J Med Microbiol. 2004;53(Pt 7):603–7. doi:.https://doi.org/10.1099/jmm.0.45528-0
3 Alhazzani W , Møller MH , Arabi YM , Loeb M , Gong MN , Fan E , et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020;46(5):854–87. doi:.https://doi.org/10.1007/s00134-020-06022-5
4 Cook TM , El-Boghdadly K , McGuire B , McNarry AF , Patel A , Higgs A . Consensus guidelines for managing the airway in patients with COVID ‐19. Anaesthesia. 2020;75(6):785–99. doi:.https://doi.org/10.1111/anae.15054
5 Bhimraj A , Morgan RL , Shumaker AH , Lavergne V , Baden L , Cheng VC-C , et al. Infectious Diseases Society of America Guidelines on the Treatment and Management of Patients with COVID-19. Clin Infect Dis. 2020;ciaa478. doi:.https://doi.org/10.1093/cid/ciaa478
6 White PL , Backx M , Barnes RA . Diagnosis and management of Pneumocystis jirovecii infection. Expert Rev Anti Infect Ther. 2017;15(5):435–47. doi:.https://doi.org/10.1080/14787210.2017.1305887
7 Chua F , Armstrong-James D , Desai SR , Barnett J , Kouranos V , Kon OM , et al. The role of CT in case ascertainment and management of COVID-19 pneumonia in the UK: insights from high-incidence regions. Lancet Respir Med. 2020;8(5):438–40. doi:.https://doi.org/10.1016/S2213-2600(20)30132-6
8 Zhou F , Yu T , Du R , Fan G , Liu Y , Liu Z , et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62. doi:.https://doi.org/10.1016/S0140-6736(20)30566-3
No financial support and no other potential conflict of interest relevant to this article was reported.