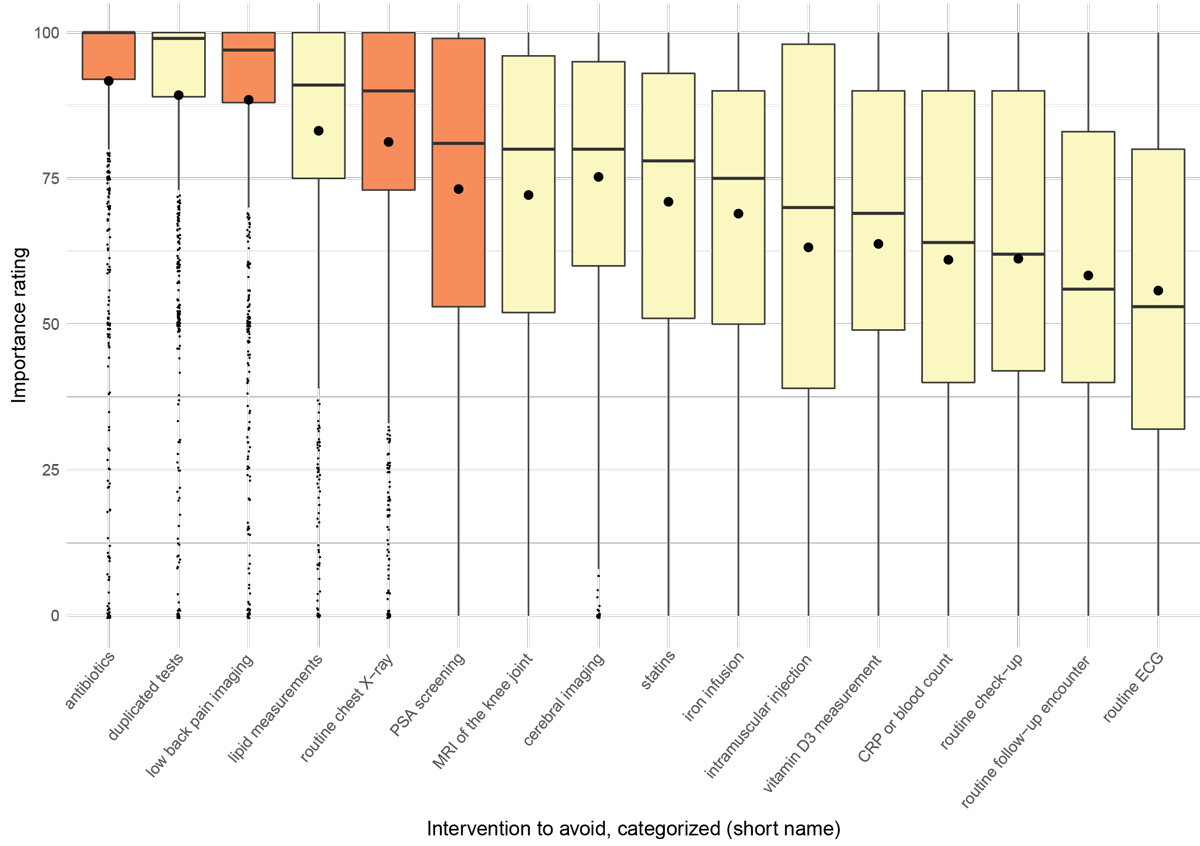
Figure 1 Boxplots of importance ratings on a numeric scale 0–100 from survey round two (highlighted: RIAs that correspond to the 2014 SGAIM top 5 recommendations for ambulatory internal medicine [3]; large dots: means; small dots: outliers).
DOI: https://doi.org/10.4414/smw.2020.20283
confidence interval
C-reactive protein
electrocardiography
general practitioner
interquartile range
odds ratio
recommendation to avoid
standard deviation
Swiss Society of General Internal Medicine
The “Smarter Medicine” top-five list for ambulatory general internal medicine published in 2014
There is increasing concern about low-value healthcare, leading to harm and unwarranted costs [1]. As a reaction, campaigns such as “Choosing Wisely” were launched and disseminated worldwide [2]. In Switzerland, the Swiss Society of General Internal Medicine (SGAIM) started the campaign in 2014 under the label “Smarter Medicine” [3, 4]. Meanwhile, 11 Swiss medical societies have contributed to the campaign by developing their own recommendations of interventions to avoid (RIAs) [3]. However, the impact of these campaigns has been questioned for several reasons [5–8].
Usually the development of “Choosing Wisely” RIAs starts with an expert panel defining a first set of RIAs. In a second step, this set is then validated by members of the society that intends to publish a “Choosing Wisely” list, by focus groups or by peers [9–11]. As the priorities of general practitioners (GPs) concerning RIAs may differ substantially from experts’ priorities [12], the credibility and acceptance of RIAs may benefit from early involvement of GPs in the development process [9–11].
Therefore the aim of our study was to develop RIAs for ambulatory general medicine with substantial involvement of Swiss GPs right from the beginning.
This was a cross-sectional explorative study using qualitative and quantitative research methods, with a two-round Delphi procedure [13]: a first round to generate RIAs directly from GPs’ personal experiences and perceptions, and a second round to rate the most frequent suggestions from round one by importance.
We contacted all SGAIM members by newsletter e-mail combined with postal mailing (first round November 2018; second round June 2019). Before the first mailing, members were encouraged to participate by an announcement of the survey in the official SGAIM journal Primary and Hospital Care. We provided all mailings, as well as the instructions and items for the survey, in the language of the practice location (“language region”), in order to avoid selection bias due to language reluctance.
In the first round, we asked participants to suggest two prioritised RIAs in ambulatory care that they think are either not beneficial or even harmful for the patient. The answers were captured in an online survey form using the SurveyMonkey online tool [14], with two free-text boxes for the prioritised suggestions, a third free-text box for notes/comments and fill-in boxes for physician characteristics (see table 1 below). Additionally, participants were asked through which medium (newsletter e-mail, postal mailing, medical journal) the survey had come to their attention, and whether they knew the “Smarter Medicine” top-five list for ambulatory general internal medicine published in 2014 (T5L) [3].
Table 1 Participants’ characteristics of survey rounds one and two.
| Characteristic |
1st round
(N1 = 538) |
2nd round
(N2 = 1357) |
Reference population*
(NR = 8308) |
|---|---|---|---|
| Used in regression analyses: | |||
| Knowledge about “Smarter Medicine” top 5 list (published in 2014) (%N) | 433 (80.5%) | n/a | n/a |
| Gender, female (%N) | n/a | 455 (33.5%) | 41.3% |
| Age, years, mean (SD) | 52.7 (11.3) | 53.2 (11.9) | 51.6 (11.6) |
| Practice language region | |||
| German speaking part of Switzerland (%N) | 452 (84.0%) | 1128 (83.1%) | 72.3% |
| Non-German speaking part† of Switzerland (%N) | 86 (16.0%) | 229 (16.9%) | 27.7% |
| Practice location | |||
| Urban (%N) | 247 (45.9%) | 629 (46.4%) | 76.1% |
| Periurban (%N) | 147 (27.3%) | 369 (27.2%) | 15.7% |
| Rural (%N) | 142 (26.4%) | 352 (25.9%) | 8.2% |
| Practice type‡ | |||
| Single practice (%N) | 148 (27.5%) | 349 (25.7%) | 27.8% |
| Group practice (%N) | 308 (57.2%) | 647 (47.7%) | 34.8% |
| Hospital (%N) | 76 (14.1%) | 252 (18.6%) | 27.8% |
| Not used in regression analyses: | |||
| Workload, patients per week (SD) | 80.8 (45.4) | n/a | n/a |
| Medium by which the survey came to their attention | |||
| Newsletter e-mail (%N) | 310 (57.6%) | n/a | n/a |
| Postal mailing (%N) | 143 (26.6%) | n/a | n/a |
| Medical journal article (%N) | 9 (1.7%) | n/a | n/a |
| Several of the above, or other (%N) | 57 (10.6%) | n/a | n/a |
* The reference population consists of the (general) internist members of the Swiss Medical Association [15]. Numbers not summing up to the total N (or 100%) are explained by missing values. † Including French and Italian speaking participants. ‡ Participants of the 1st and the 2nd round significantly differed only for practice type (p = 0.008).
In the second round, we coded, grouped and re-phrased RIAs to create comprehensive items. Subsequently, we sent out a set of the 16 most frequently named RIAs to the same target population (for definitions of coding, grouping, re-phrasing and frequencies, see the “Analysis” section). Again we used newsletter e-mail and postal mailing. Participants of round two were asked to rate each of the 16 interventions by importance (relevance) on a 0 to 100 numerical scale, using the SurveyMonkey tool [14] again. For details of the survey features, see appendix 1.
Ethics approval was not deemed to be necessary, as no intervention among GPs or patients took place. The informed consent from participants was obtained in the online survey form, with the information that data will be used anonymously and without transfer to any third party, and that consent is given by proceeding in the survey form.
The RIA suggestions collected in the first round were analysed using thematic analysis methodology [16]. First, the researchers coded the suggestions independently (MM coded the whole dataset, SNJ, SM and OS each coded a third of the dataset). In a next step, we grouped codes with different wording but the same meaning by consensus within the study group. We then counted frequencies of all code groups and selected the 16 most frequently named groups. The number of 16 was chosen to give a manageable size for the second survey round, in order to avoid an excessive workload for the participants. All 16 most frequently named groups were re-phrased by consensus within the research group, in order to provide unambiguous RIA statements for the round two rating procedure, by interactive discussion in the research group, and decisions were taken in consensus.
For both rounds we calculated counts and proportions of the categorical variables, and means, medians, standard deviations (SDs), and interquartile ranges (IQRs) of the numerical variables. We compared the GP characteristics from round one with those from round two using chi-square and t-tests as appropriate, and with the reference population of Swiss general internal medicine physicians [15]. We explored associations of GP characteristics with suggesting each of the 16 most frequently named code groups from round one using (univariate and fully adjusted) logistic regression models, and associations of GP characteristics with importance ratings from round two by (univariate and fully adjusted) linear regression. Knowledge about the T5L, GPs age and gender, language region, practice location and type were included as covariates. In addition we carried out a sensitivity analysis excluding GPs working in a hospital setting. For all analyses we used the statistical software R, Version 3.5.0 [17].
We compared the RIAs selected for round two with published recommendations of low-value healthcare activities to be avoided from “Choosing Wisely” lists of USA, Canada, UK, Australia, Switzerland and Germany, as available from the corresponding websites [2, 3, 18–21].
In the first round, 538 out of 7318 members approached suggested 1074 interventions (response rate 7.4%). In the second round 1357 out of 7468 members approached provided ratings for the 16 RIAs (response rate 18.2%). Overall, 33.5% of participants were female, mean age was 53.2 years (SD 11.9) and 80.5% of all participants (81.2% from the German speaking part, 76.7% from the non-German speaking part of Switzerland) knew the T5L (table 1). The 16 most frequently named RIAs (coded, grouped and re-phrased) from round one covered 43.9% of all 1074 suggestions.
Out of the 16 most frequently mentioned RIAs, 13 were concordant with at least one “Choosing Wisely” RIA from an international list [2, 3, 18–21], whereas the RIAs duplicated tests (e.g., laboratory tests, electrocardiography [ECG], x-rays) due to unavailable test results or medical records, C-reactive protein (CRP) measurement or white blood cell counts without consequences, such as in viral infections, and intramuscular injection in acute lower back pain have not been published on any of these lists up to now. Four of the six highest rated RIAs were concordant with the T5L (fig. 1).
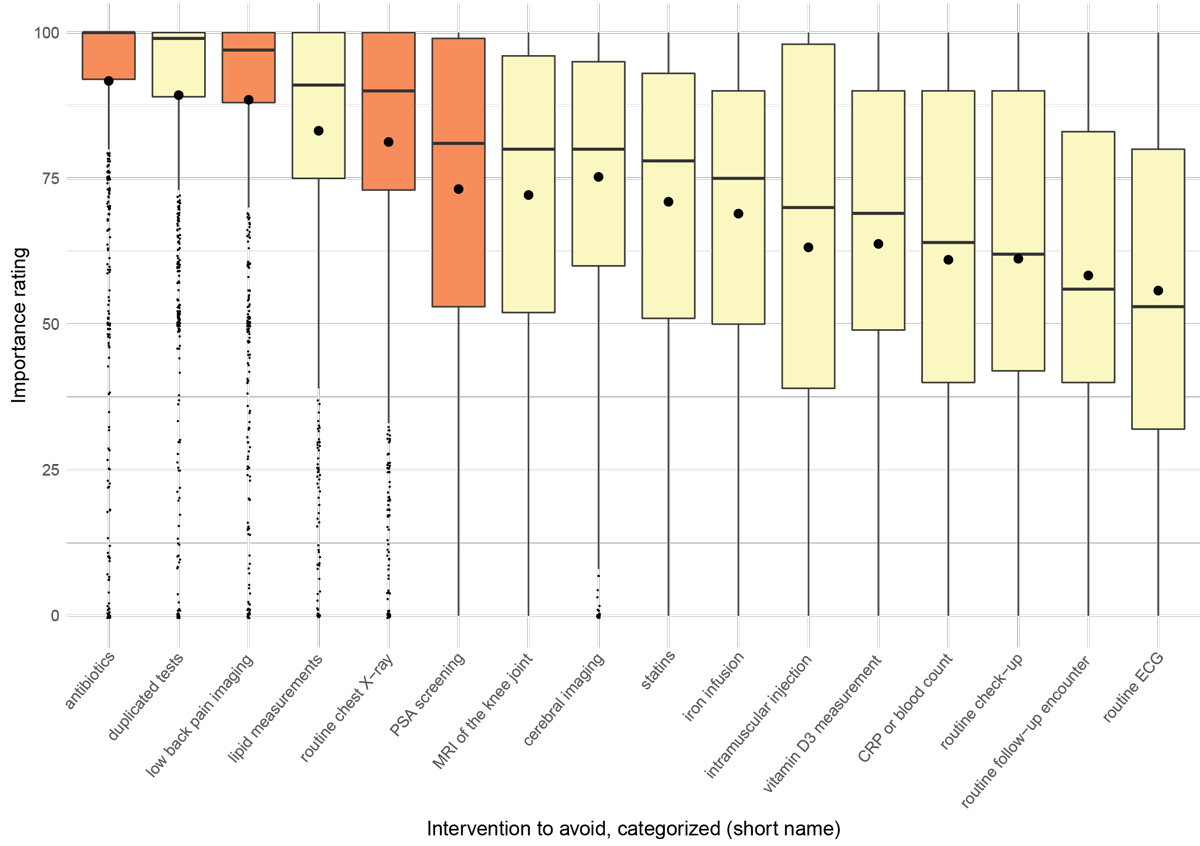
Figure 1 Boxplots of importance ratings on a numeric scale 0–100 from survey round two (highlighted: RIAs that correspond to the 2014 SGAIM top 5 recommendations for ambulatory internal medicine [3]; large dots: means; small dots: outliers).
The three most frequently named RIAs were: (1) use of antibiotics in viral infections, (2) imaging of the lower spine as first-line diagnostic procedure in unspecific low-back pain, and (3) routine chest X-ray as part of a check-up, before elective surgery or in viral upper airway infections (table 2).
Table 2 The 16 most frequently named RIAs from round one (Ʃn = 472 = 43.9% of N = 1074 RIAs), ranked by frequency.
| Recommendations of intervention to avoid (RIAs) |
Frequency
n (%N) |
|---|---|
| Use of antibiotics in viral infections (e.g., upper airway infections of viral origin) | 76 (7.1%) |
| Imaging of the lower spine as first-line diagnostic procedure in unspecific low back pain | 70 (6.5%) |
| Routine chest x-ray as part of a check-up before surgery or in viral upper airway infections | 44 (4.1%) |
| Check-up in healthy, young or asymptomatic subjects | 35 (3.3%) |
| Routine follow-up encounters (e.g., with orthopaedists, cardiologists) after interventions | 26 (2.4%) |
| ECG during check-ups or before surgery | 26 (2.4%) |
| Treatment with iron via infusion without previous oral treatment | 24 (2.2%) |
| PSA screening as a routine (e.g., without shared decision making) | 22 (2.0%) |
| Vitamin D3 measurement as a routine | 21 (2.0%) |
| CRP or white blood cell count without consequences, e.g., in in viral infections | 21 (2.0%) |
| Lipid measurements without consequences, e.g., in in old patients | 21 (2.0%) |
| MRI of the knee in knee pain without a previous conservative treatment unless in case of a locked knee joint | 20 (1.9%) |
| Duplicated tests (e.g., laboratory tests, ECG, x-ray) because of unavailable test results or medical records | 17 (1.6%) |
| Statins for old patients | 17 (1.6%) |
| Intramuscular injection in acute lower back pain | 16 (1.5%) |
| Cerebral imaging in chronic headache or head injury without neurological red flags | 16 (1.5%) |
ECG = electrocardiography; PSA = prostate-specific antigen; CRP = C-reactive protein; MRI = magnetic resonance imaging.
The three RIAs (out of the 16 RIAs sent out in round two) rated as most important were: (1) use of antibiotics in viral infections (mean 91.7, SD 18.6), (2) duplicated tests (e.g., laboratory tests, ECG, x-ray) due to unavailable test results or medical records (mean 89.3, SD 19.9), and (3) imaging in unspecific low back pain as a first-line diagnostic procedure (mean 88.5, SD 19.9) (figure 1 and appendix 2).
In the logistic regression of round one data, we found no association between participants’ characteristics (table 1) and RIA suggestions, with one exception: older GPs were less likely to suggest the avoidance of intramuscular injections for acute lower back pain (for 10-year increase of age: odds ratio 0.28, 95% confidence interval 0.14–0.52; p <0.001) (appendix 3). In the linear regression of round two data, female gender and working in a hospital setting or in a non-German language region were independently associated with changes in the importance ratings of several RIAs (appendix 4). A sensitivity analysis excluding hospital-based GPs showed that the importance ranking did not change for the first three ranks and to a minor degree in the other 13 ranks (appendix 5).
In this nationwide two-round online Delphi survey Swiss GPs developed RIAs in a bottom-up approach based on importance for their daily practice. Overall, GPs suggested 1074 interventions. Out of the 16 most frequently named RIAs, 13 were concordant with “Choosing Wisely” RIAs from at least one international list [2, 3, 18–21]. Accordingly, RIAs on ranks one, three, four and five were concordant with the T5L (fig. 1), which indicates that the T5L topics as well as the existing “Choosing Wisely” RIAs are perceived as meaningful and important by Swiss GPs at present.
Four out of five GPs declared that they know the T5L, a proportion substantially higher than previously reported by Selby et al. (62%) [22]. Of note, in our regression analyses, we found no significant differences between GPs who knew the T5L and those unaware of it with regard to suggesting any of the 16 most frequently mentioned RIAs (appendix 3). This indicates that the RIAs provided by the participating GPs were based on their own experiences and beliefs rather than just echoing the T5L RIAs.
Similarly, frequencies of suggestions and importance ratings of RIAs were hardly associated with any of the other GPs characteristics, which supports the robustness of our main findings. There were a few exceptions: For example, avoiding intramuscular injections in acute lower back pain was less frequently suggested with increasing age of GPs, probably because of a different perception of harm versus benefit of this intervention in the different age groups. Gender, language region and practice setting were independently associated with changes in the importance ratings of several RIAs ranked on places 4 to 16 (for details, see appendices 3 and 4). For example, female GPs were more likely to give a high importance rating for the RIA iron infusions as first-line treatment for iron deficiency, whereas hospital-based GPs were less likely to do so compared to the average study population.
This is not surprising, as factors such as gender and cultural background often affect healthcare providers’ opinions on health issues [23], and a hospital-based working place has a different patient population associated with a different focus on interventions (and interventions to avoid).
The majority of our set of 16 most frequently mentioned RIAs are well-known in the “Choosing Wisely” literature. Use of antibiotics in viral infections – the RIA suggested most frequently and rated highest in our sample – reflects the call for a prudent use of antibiotics facing the antibiotic resistance challenge [24, 25]. This RIA was published at an early stage of the US “Choosing Wisely” campaign [2], and taken up by many societies as well as by an ongoing campaign of the Swiss Federal Authorities [26]. The second most important RIA in the view of GPs was a process quality issue, namely duplicated tests (e.g., laboratory tests, ECG, x-rays) due to unavailable test results or medical records. This is a major global challenge for health systems, as the 2016 Commonwealth Fund Survey revealed. Tackling coordination deficiencies between healthcare providers, particularly in transition settings, is promising for improving healthcare quality [27]. Remarkably, there is no corresponding RIA on any of the international “Choosing Wisely” lists including the T5L. An explanation may be that improving poor coordination between healthcare providers is a healthcare system issue on an organisational level rather than an individual behavioural level, and therefore it is difficult to demand responsibility from individuals. However, there are a few mentions in the “Choosing Wisely” literature, restricted to specific conditions. For example, the Society of American Family Physicians recommends not duplicating genetic testing in specific conditions [28]. Other recommendations question repeated blood tests, such as at a high frequency, among critical care patients during their hospitalisation [29, 30]. There are initiatives on the way that call for tackling duplicate testing, mainly by recommending optimisation of information technology techniques for data exchange [31].
Imaging overuse with its inherent danger of overdiagnosis and subsequent overtreatment (e.g., unnecessary surgery) seems to be another major concern among front-line GPs. This RIA was taken up on several “Choosing Wisely” lists at an early stage of the campaigns [3, 32], including the T5L. Lipid measurements without consequences, such as in old patients who will not benefit from any treatment even when high lipid levels are found, was another prominent RIA among the GPs in our study, but only on one of the international lists [21] and not on the T5L. Interrelated with this issue, the RIA statins for old patients was rated as relatively important in our study sample and recommended before on “Choosing Wisely” lists [2], but not on the T5L. Although the debate is still ongoing, patients older than 70 years do not benefit from treatment with statins in primary prevention (in terms of mortality) according to a recent meta-analysis [33].
Involving front-line GPs from the very beginning in the development of RIAs is a methodological strength of our study and complementary to the usual development procedure of “Choosing Wisely” lists driven by expert panels [9–11]. We found a considerable overlap between the RIAs developed by the two different methods (“bottom-up” approach versus usual expert-driven approach). Therefore, our work validates the usual methodological approach, but it also allowed development of new RIAs not published on previous “Choosing Wisely” lists. Furthermore, by using a stringent prioritisation procedure at two time points (round one: asking for two suggestions perceived as most important; round two: quantitative rating by importance), we think that we captured GPs’ perceptions of RIAs to a high degree.
As a limitation in terms of generalisability, the response rates were relatively low (especially in round one). However, the study population seemed representative for the Swiss GP population, with the exception of gender, language region and practice location (table 1), and the response rates were in line with usual response rates of surveys among GPs recently published [34–36]. As another limitation, GPs who are generally more interested in overuse and care quality issues may have been more likely to participate than GPs without this focus (responder bias).
Most RIA suggestions from GPs were concordant with previously published RIAs, independently of GPs knowledge of these and reflecting their high clinical relevance. In addition, our study revealed some more relevant topics and may help to develop future “Choosing Wisely” recommendations, with the final goal to reduce low-value care.
Appendix 1: CHERRIES Guideline Checklist for surveys
Appendix 2: Most frequent recommendations to avoid
Appendix 3: Logistic regression models for mentions of RIA categories (survey round one)
Appendix 4: Linear regression models for RIA category importance ratings (survey round two)
Appendix 5: Frequencies and importance of interventions to avoid
The appendices are available in a separate file at https://smw.ch/article/doi/smw.2020.20283.
We like to thank all participating GPs for their worthy contribution to this study.
The study was supported by a grant of the Swiss Society of General Internal Medicine (SGAIM) Foundation. There was no influence by the sponsor on methodology, results nor publication policy.
The authors declare that they have no competing interests.
1 Parchman ML , Henrikson NB , Blasi PR , Buist DS , Penfold R , Austin B , et al. Taking action on overuse: Creating the culture for change. Healthc (Amst). 2017;5(4):199–203. doi:.https://doi.org/10.1016/j.hjdsi.2016.10.005
2 https://www.choosingwisely.org (accessed 2019 December 13)
3 https://www.smartermedicine.ch (accessed 2019 December 13)
4 Selby K , Gaspoz JM , Rodondi N , Neuner-Jehle S , Perrier A , Zeller A , et al. Creating a list of low-value health care activities in Swiss primary care. JAMA Intern Med. 2015;175(4):640–2. doi:.https://doi.org/10.1001/jamainternmed.2014.8111
5 Santa JS . Communicating information about “what not to do” to consumers. BMC Med Inform Decis Mak. 2013;13(S3, Suppl 3):S2. doi:.https://doi.org/10.1186/1472-6947-13-S3-S2
6 Rosenberg A , Agiro A , Gottlieb M , Barron J , Brady P , Liu Y , et al. Early trends among seven recommendations from the choosing wisely campaign. JAMA Intern Med. 2015;175(12):1913–20. doi:.https://doi.org/10.1001/jamainternmed.2015.5441
7 Hasson H , Nilsen P , Augustsson H , Ingvarsson S , Korlén S , von Thiele Schwarz U . To do or not to do-balancing governance and professional autonomy to abandon low-value practices: a study protocol. Implement Sci. 2019;14(1):70. doi:.https://doi.org/10.1186/s13012-019-0919-x
8 Robert G , Harlock J , Williams I . Disentangling rhetoric and reality: an international Delphi study of factors and processes that facilitate the successful implementation of decisions to decommission healthcare services. Implement Sci. 2014;9(1):123. doi:.https://doi.org/10.1186/s13012-014-0123-y
9 Grady D , Redberg RF , Mallon WK . How should top-five lists be developed?: what is the next step? JAMA Intern Med. 2014;174(4):498–9. doi:.https://doi.org/10.1001/jamainternmed.2013.8272
10 Schuur JD , Carney DP , Lyn ET , Raja AS , Michael JA , Ross NG , et al. A top-five list for emergency medicine: a pilot project to improve the value of emergency care. JAMA Intern Med. 2014;174(4):509–15. doi:.https://doi.org/10.1001/jamainternmed.2013.12688
11 Atkinson P , Lang E , Mackenzie M , Hiranandani R , Lys R , Laupacis M , et al. CJEM Debate Series: #ChoosingWisely - The Choosing Wisely campaign will not impact physician behaviour and choices. CJEM. 2018;20(2):170–5. doi:.https://doi.org/10.1017/cem.2017.402
12 Neuner-Jehle S , Senn O , Rosemann T . Neue „Choosing wisely“ Empfehlungen zu unangemessenen medizinischen Interventionen: Sicht von Schweizer Hausärzten [New “choosing wisely” recommendations of inappropriate interventions: The perspective of Swiss general practitioners]. Z Evid Fortbild Qual Gesundhwes. 2016;118-119:82–6. German. doi:.https://doi.org/10.1016/j.zefq.2016.09.001
13Turoff M, Hiltz S. Computer based Delphi processes. In: Adler M, Ziglio, E, editors. Gazing into the Oracle: The Delphi Method and its Application to Social Policy and Public Health. London: Jessica Kingsley Publishers; 1995. pp 56–88.
14SurveyMonkey Inc. San Mateo, California, USA, https://www.surveymonkey.com (accessed 2019 December 13)
15Swiss Medical Association (Foederatio Medicorum Helveticorum) Physicians’ Statistics. 2018, available from: https://www.fmh.ch (accessed 2019 December 13)
16Braun V, Clarke V. Thematic analysis. In: Cooper, editor. Handbook of research methods in psychology. Washington DC: APA books; 2012. pp 57–71.
17R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing V, Austria. 2008; ISBN 3-900051-07-0. https://www.R-project.org (accessed 2019 December 13)
18 https://www.choosingwiselycanada.org (accessed 2019 December 13)
19 https://www.choosingwisely.co.uk (accessed 2019 December 13)
20 https://www.klug-entscheiden.com (accessed 2019 December 13)
21 https://www.choosingwisely.org.au (accessed 2019 December 13)
22 Selby K , Cornuz J , Cohidon C , Gaspoz JM , Senn N . How do Swiss general practitioners agree with and report adhering to a top-five list of unnecessary tests and treatments? Results of a cross-sectional survey. Eur J Gen Pract. 2018;24(1):32–8. doi:.https://doi.org/10.1080/13814788.2017.1395018
23 Henderson JT , Weisman CS . Physician gender effects on preventive screening and counseling: an analysis of male and female patients’ health care experiences. Med Care. 2001;39(12):1281–92. doi:.https://doi.org/10.1097/00005650-200112000-00004
24 Smith SM , Fahey T , Smucny J , Becker LA . Antibiotics for acute bronchitis. Cochrane Database Syst Rev. 2017;6(6):CD000245.
25 Spinks A , Glasziou PP , Del Mar CB . Antibiotics for sore throat. Cochrane Database Syst Rev. 2013;(11):CD000023.
26 https://www.star.admin.ch/star/en/home.html (accessed 2019 December 13)
27 Osborn R , Squires D , Doty MM , Sarnak DO , Schneider EC . In new survey of eleven countries, US adults still struggle with access to and affordability of health care. Health Aff (Millwood). 2016;35(12):2327–36. doi:.https://doi.org/10.1377/hlthaff.2016.1088
28 https://www.aafp.org/afp/recommendations/viewRecommendation.htm?recommendationId=281 (accessed 2020 April 29)
29 https://www.choosingwisely.org/clinician-lists/american-association-blood-banks-serial-blood-counts-on-clinically-stable-patients (accessed 2020 April 29)
30 https://www.choosingwisely.org/clinician-lists/critical-care-societies-collaborative-regular-diagnostic-tests (accessed 2020 April 29)
31 Procop GW , Yerian LM , Wyllie R , Harrison AM , Kottke-Marchant K . Duplicate laboratory test reduction using a clinical decision support tool. Am J Clin Pathol. 2014;141(5):718–23. doi:.https://doi.org/10.1309/AJCPOWHOIZBZ3FRW
32 Rao VM , Levin DC . The overuse of diagnostic imaging and the Choosing Wisely initiative. Ann Intern Med. 2012;157(8):574–6. doi:.https://doi.org/10.7326/0003-4819-157-8-201210160-00535
33 Cholesterol Treatment Trialists’ Collaboration. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. 2019;393(10170):407–15. doi:.https://doi.org/10.1016/S0140-6736(18)31942-1
34 Price S , Spencer A , Medina-Lara A , Hamilton W . Availability and use of cancer decision-support tools: a cross-sectional survey of UK primary care. Br J Gen Pract. 2019;69(684):e437–43. doi:.https://doi.org/10.3399/bjgp19X703745
35 Breedvelt JJF , Zamperoni V , Kessler D , Riper H , Kleiboer AM , Elliott I , et al. GPs’ attitudes towards digital technologies for depression: an online survey in primary care. Br J Gen Pract. 2019;69(680):e164–70. doi:.https://doi.org/10.3399/bjgp18X700721
36 Hall LH , Johnson J , Watt I , O’Connor DB . Association of GP wellbeing and burnout with patient safety in UK primary care: a cross-sectional survey. Br J Gen Pract. 2019;69(684):e507–14. doi:.https://doi.org/10.3399/bjgp19X702713
SNJ and OS conceived the study. MM organised the survey. TG calculated the statistics and drafted tables and figures. SNJ drafted the manuscript. All authors contributed to the selection of round two items in consensus and to the interpretation of results. The manuscript was read and approved by all authors.
The study was supported by a grant of the Swiss Society of General Internal Medicine (SGAIM) Foundation. There was no influence by the sponsor on methodology, results nor publication policy.
The authors declare that they have no competing interests.