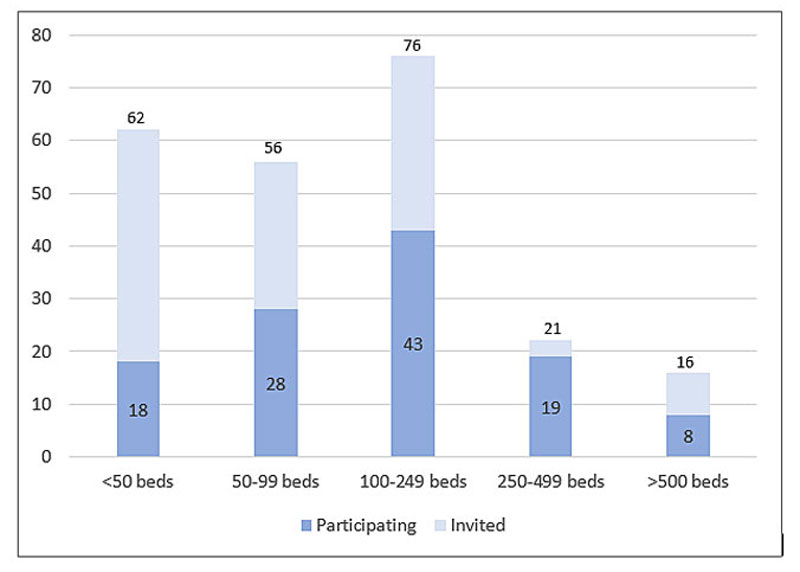
Figure 1 Invited and participating hospitals by number of beds.
DOI: https://doi.org/10.4414/smw.2020.20278
Patient safety is a primary concern of every hospital and its workforce. Combined with the direct harm hospital care errors cause patients, the responsible care professionals commonly suffer lasting psychological damage. However, although hospitals understandably devote tremendous energy to returning the affected patients to health, they tend to focus less on the recovery of these second victims.
Following a patient safety incident, the concepts of medical error, defined as “an unintended act (either of omission or commission) or one that does not achieve its intended outcome” [1] or more tangible “that was a threat to patient wellbeing and should not happen” [2] and adverse event – “an injury caused by medical management (rather than the underlying disease) and that prolonged hospitalisation, produced a disability at the time of discharge, or both” – play important roles [3]. Our 2018 review of hospital studies revealed that one patient in ten is affected by at least one adverse event, half of which are deemed preventable [4]. Supporting this finding, a 2019 meta-analysis determined that around 6% of patients are exposed to preventable harm in medical care [5].
A 2019 study in 32 Dutch hospitals reported that 85.6% of surveyed physicians and nurses had been involved in at least one patient safety incident during their career [6]. Those who are “involved in an unanticipated adverse patient event, in a medical error and/or a patient related injury and become victimised in the sense that the provider is traumatised by the event” [7] are known as “second victims”. According to a systematic review, the prevalence of second victims after an adverse event varied from 10.4% up to 43.3% [8].
Second victims can be impacted physically, emotionally and professionally (table 1). Possible reactions include feelings of guilt [9–13], fear of repeating the error, losing their job, or of legal consequences [10–12], burn-out, loss of confidence, sleep disorders [10, 12–14], problematic medication use, excessive alcohol consumption [15], turnover intentions [15, 16], and absenteeism [16]. Persons involved in one adverse event show an increased risk of later involvement in others, suggesting that lingering symptoms may manifest as parts of reciprocal cycles, contributing to future suboptimal patient care and error [17]. Because of the weight of potential outcomes, it is crucial that second victims receive systematic support. On the individual level, Seys et al. observed that, although discussions with peers about the event process and the emotional aftermath are much appreciated, further support should also be provided by specially trained managers, supervisors or therapists. In addition, following an event it is vital that professional support be offered as quickly as possible.
Table 1 Medical error!
| It’s an intense morning in the Med-Surg unit. One of Nurse Gina’s patients, Mr Schmidt, is in severe pain. Following his analgesic prescription, Gina administers intravenously a 5 mg dose of hydromorphone. Filling in the patient record, she sees the previous dosage. It was 0.5 mg. Mr Schmidt’s life is in danger! Blocked by rising panic, shame and dread, her thoughts race in circles. But Mr Schmidt is already unconscious, his breathing laboured. From the door, Gina shouts to Doris, her unit supervisor, for help. Even as Doris is grabbing the rescue kit, she’s on the line to Robert, the attending physician. Working fast, Robert and Doris neutralise the overdose. Gently but firmly, Doris tells Gina to take a break and regain her composure. When Mr Schmidt regains consciousness, Robert and Doris inform him about the error, their countermeasures and the remaining steps. After lunch, Doris speaks with Gina. After a supportive clarifying discussion, Gina asks Doris to accompany her as she apologises personally to Mr Schmidt. He reacts with patience and understanding. Alongside the support of her ward manager and the attending physician, this nurse’s open conversation with the patient helps her deal with her feelings of guilt and self-doubt. Later, discussions with her team leader, her colleagues, and the staff psychologist will allow her and the hospital to use this event to improve patient safety. Three months later, Gina has recovered her confidence and continues working as a nurse. Now, though, she is aware not only that mistakes can materialise in an instant, but that they can happen to anyone. She also knows first-hand how collegial support has helped her, as an error’s second victim, to cope, recover and go back to helping patients. |
At the institutional level, beginning from the detection of an adverse event, second victim support must encompass a clear process that includes improving or replacing failing systems, along with actions to support all involved persons. Each institution’s support system should include training for support personnel, allow referrals to specialists, assure confidentiality regarding the affected health professionals and be available 24/7 [8].
Scott et al. estimated that roughly 60% of second victims receive enough support from work colleagues (peers) or at the departmental level to avoid symptoms. However, another 30% need support from specially trained supporters and 10% need professional counselling [18].
Based on all available evidence regarding adverse events’ negative repercussions on health professionals, current Swiss national guidelines characterise a clear set of aims, recommended organisational structures and desirable features of institutional policy to support involved health professionals [19, 20]. In the US, programmes such as the National Institutes for Health (NIH) “Medically Induced Trauma Support Services” (MITSS) [21], the forYou Team programme of the University of Missouri Health Care [18] and the Johns-Hopkins “Resilience in Stressful Events” (RISE) programme [22] have been designed to tackle the problem from different angles.
In general, the core elements of these programmes include a strong focus on the target organisation’s internal culture, an evaluation of its vigilance regarding possible second victims, the realisation of a multi-disciplinary support team, clear formulation of relevant policies, a clear statement concerning responsibilities and characteristics of support programs, training of supporters, and development of a strategy to inform employees about the program [18, 21, 23].
However, regardless of the broad base of evidence in favour of such systematic approaches, not all institutions offer distinct programmes. In 2015, White et al. reported that 73.6% of 575 healthcare facilities offered support programmes for second victims, with 7.3% more planning to implement one [24]. The same year, 71% of hospitals in Spain offered no support programme for second victims [25], and where such programmes were available, no reports regarding their effectiveness were available [26].
In Switzerland, the current prevalence of second victim support falls somewhere between those of the US and Spain. Swiss acute care hospitals acknowledge its importance for minimising negative impacts on health professionals, for maintaining high care quality and for enhancing patient safety, but information on which ones offer it and details of its use are scarce. Therefore, the purpose of this study was to obtain information on whether and how Swiss hospitals are dealing with health professionals who are involved in a medical error or adverse event.
To address these purposes, working with a variety of Swiss acute care, psychiatric, rehabilitation and speciality institutions, we aimed (1) to identify any general organisational structures and processes in place to support second victims, and (2) to explore which Swiss hospitals offer specific systematic second victim support programmes.
For this cross-sectional, multi-centre survey study, acute care and university hospitals, psychiatric hospitals, as well as the rehabilitation and speciality clinics named on the Swiss Hospitals Association (H+) hospital list [27] were eligible. It included 231 hospitals across Switzerland (German-speaking region: 176; French-speaking region: 43; Italian-speaking region: 12). Of that number, 74 (32%) belonged to hospital groups.
To assess how Swiss hospitals support their health professionals after an adverse event, a 13-item self-developed questionnaire (appendix 1) was used. Three items addressed hospital characteristics, such as type (according to the H+ categories), size (number of beds) and membership in a hospital group. The eight items regarding hospital policies and activities of supporting health professionals who became second victims are based on the NIH MITSS organisational assessment tool for clinician support [28], and the University of Missouri forYou Health Care Team programme [18]. Item responses included “yes”, “no”, “planned” or “I don’t know”, and (for one only) “depending on”. Additionally, comments could be added as free text at the end of the questionnaire. Respondents could reply anonymously or voluntarily state their contact details for potential information exchange.
After face validity of the initial German language questionnaire was established by experts in the field, including the study authors, the questionnaire was translated into French and Italian by native speakers and cross-checked for comprehensibility.
In October 2018, an invitation for study participation, including a hyperlink to the online survey, was e-mailed to the quality managers or chief operating officers of the 231 eligible hospitals. A reminder was sent to non-respondents after 3 weeks. Six weeks after the initial invitation, the survey was closed.
The completed questionnaires were first checked for completeness and plausibility of the responses. Five responses proved ambiguous. Therefore, if the responses could not be clarified based on written comments, identifiable respondents were contacted.
All survey responses were included in the data analysis using the R statistics program, version 3.5.3 [29]. Descriptive analyses were performed on frequencies and percentages, while comparisons regarding hospital size and type used Fisher’s exact test.
The Ethics Committee Northwest and Central Switzerland (EKNZ) exempted the study from review and approved the survey as ethically acceptable (BASEC Req-2018-00668).
Of the 231 invited hospitals’ quality managers or chief executive officers, 116 (German: 88, French: 20, Italian: 8) completed the questionnaire – a response rate of 50.2% (table 2). More than a third of participating hospitals were medium-sized (100–249 beds) (fig. 1); 55 (47.4%) indicated membership in a hospital group. The participating hospitals accurately reflect the Swiss hospital landscape in terms of type, size and language region (fig. 2).
Table 2 Invited and participating hospitals*.
| Hospital type |
Invited hospitals
n = 231 |
Participating hospitals n = 116 | Response rates (%) |
|---|---|---|---|
| University | 7 | 7 | 100 |
| Acute care | 109 | 58 | 50 |
| Psychiatric | 40 | 16 | 40 |
| Rehabilitation | 42 | 14 | 33.3 |
| Speciality | 34 | 21 | 61.8 |
Descriptive statistics (frequencies) applied. * 231 hospitals across Switzerland were included (German-speaking region: 176; French-speaking region: 43; Italian-speaking region: 12). Of that number, 74 (32%) belong to hospital groups.
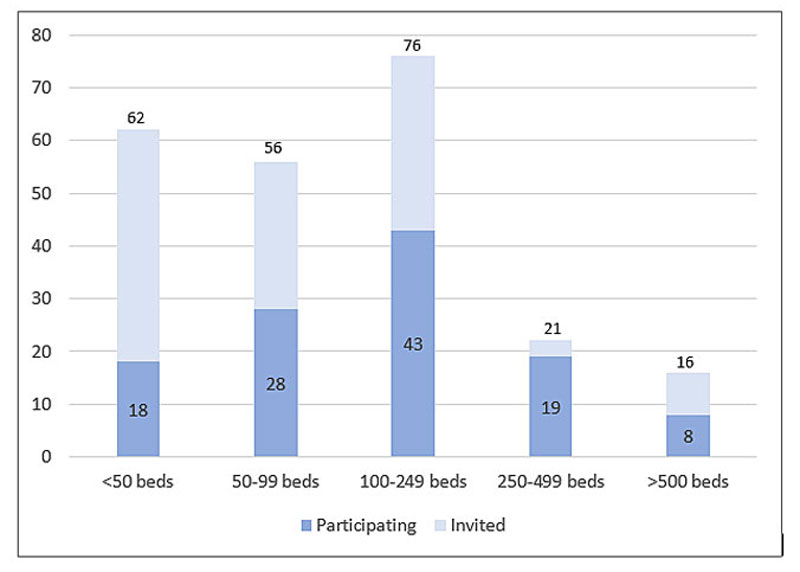
Figure 1 Invited and participating hospitals by number of beds.
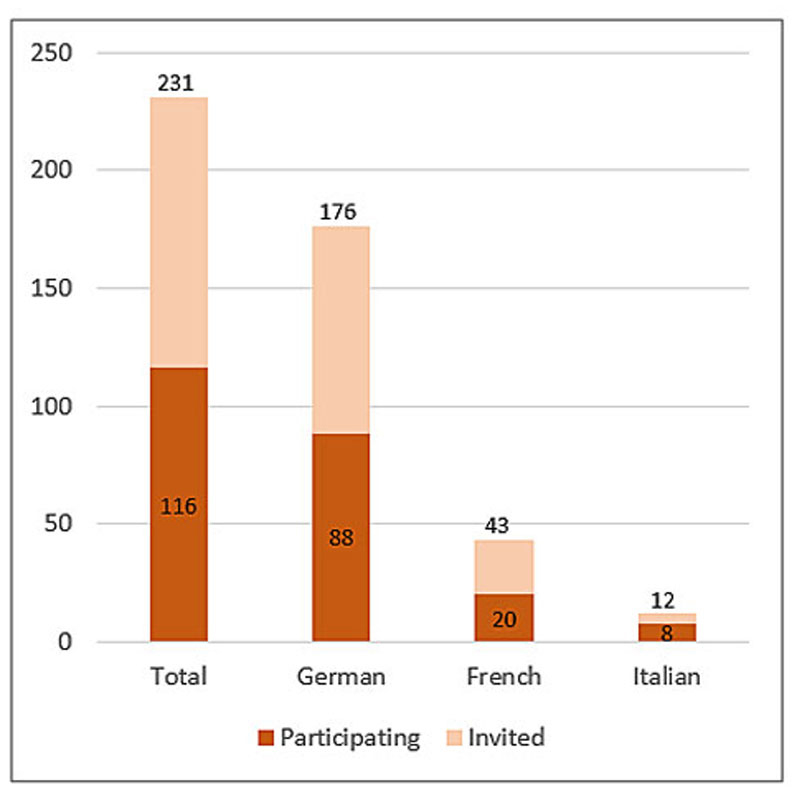
Figure 2 Invited and participating hospitals by language region.
Nearly 83% of respondents indicated that their health professionals were requested to inform their superiors about adverse events. In the Italian-speaking region, all eight hospitals reported asking their health professionals to do so. Overall, roughly 85% reported providing support offers for second victims; however, of those, only 60.3% reported informing their medical staff about such offers. Hospitals in the German-speaking region were least likely to do so (56.8%, compared with 70.0% in the French speaking region and 75.0% in the Italian speaking region).
Thirty-one per cent of all hospitals reported that one or more of their supervisory staff were trained to deal with second victims. The prevalence of hospitals with such staff available varied considerably across the three language regions – 100% in the Italian-speaking, 45% in the French-speaking and 22% in the German-speaking region.
Affected professionals’ participation in the disclosure process also varied strongly. Sixty-four (55.2%) respondents declared that such participation depended on the circumstances and 15 (12.9%) stated that the professionals were generally present. Included in these groups, seven respondents specified that participation depended partly on the patient’s wishes and partly on the affected health professional’s emotional condition and ability to participate. Nineteen (16.4%) reported that health professionals were never present and the remaining 18 (15.5%) indicated that they did not know whether health professionals were present.
Respondents also added three further aspects that they considered influential: the nature of the error, the level of harm experienced by the patient and the department (table 3).
Table 3 Hospitals support for health professionals after an adverse event (n=116).
|
No
% (n) |
Yes
% (n) |
Planned
% (n) |
Don’t know
% (n) |
|
|---|---|---|---|---|
| Health professionals are informed about support offers by the institution | 26.7 (31) |
60.3 (70) |
7.8 (9) |
5.2 (6) |
| Health professionals involved in an adverse event are asked to inform superiors | 8.6 (10) |
82.8 (96) |
1.7 (2) |
6.9 (8) |
| Notation in personal file of involved health professional | 66.4 (77) |
12.9 (15) |
0 (0) |
20.7 (24) |
| Superiors are trained for support of second victims | 50.0 (58) |
31.0 (36) |
8.6 (10) |
10.3 (12) |
| Superiors are asked to approach health professionals after an adverse event | 16.4 (19) |
73.3 (85) |
2.6 (3) |
7.8 (9) |
| A standard or guideline for second victim support exists | 50.0 (58) |
31.9 (37) |
11.2 (13) |
6.9 (8) |
Descriptive statistics (frequencies and percentages) applied.
The number of second victim support offers ranged from none to several options. Possible avenues included peer support, the services of a staff physician or psychological counselling. Eighteen hospitals (15.5%) offered no support, whereas 61 (52.9%) stated that “other persons” supported second victims (table 4).
Table 4 Hospitals specific support offers for their health professionals*.
|
Total
n (%) |
Hospital size (number of beds) | |||||
|---|---|---|---|---|---|---|
|
<50
n |
50–99
n |
100–249
n |
250–500
n |
>500
n |
||
| Staff physician | 37 (31.9) | 4 | 4 | 15 | 11 | 3 |
| Psychologist | 48 (41.4) | 7 | 9 | 17 | 10 | 5 |
| Pastoral worker | 36 (31.0) | 0 | 3 | 18 | 13 | 2 |
| Trained peers | 46 (39.7) | 6 | 11 | 18 | 8 | 3 |
| Lawyer | 31 (26.7) | 0 | 2 | 15 | 12 | 2 |
| Other persons | 61 (52.9) | 11 | 11 | 20 | 15 | 4 |
Descriptive statistics (frequencies and percentages) applied. * Multiple response options. Eighteen (15.5%) hospitals indicated no support offer.
In total, 37 (31.9%) hospitals reported having guidelines in place on how to support second victims and 58 (50.0%) reported having no guideline. In the remaining 20, either guidelines were planned or the respondent had no knowledge of them (table 5).
Table 5 Comparison within hospital types on whether a guideline exists (n = 116).
| Hospital type |
No (58) / I don’t know (8)
n = 66 |
Yes (37) / planned (13)
n = 50 |
|---|---|---|
| % (n) | % (n) | |
| University | 57.1 (4) | 42.9 (3) |
| Acute care | 51.7 (30) | 48.3 (28) |
| Psychiatric | 62.5 (10) | 37.5 (6) |
| Rehabilitation | 78.6 (11) | 21.4 (3) |
| Speciality | 52.4 (11) | 47.6 (10) |
Descriptive statistics (frequencies and percentages) applied, including Fisher’s exact test. No/I don’t know and yes/planned responses for guidelines in the different hospital types and comparison in percentages within the hospital types categories.
Among the hospitals whose respondents answered “yes” or “planned”, university hospitals, acute care hospitals and specialised clinics were more likely to have implemented guidelines than psychiatric hospitals and rehabilitation clinics; however, these associations were not statistically significant (table 5).
Comparison using Fisher’s exact test showed a significant relationship (p = 0.035) between hospital size and the implementation of guidelines: guidelines were more likely to exist in larger hospitals, except for in the smallest hospitals (table 6).
Table 6 Comparison relating hospital size to existence of guidelines (n = 116).
|
Hospital size
(number of beds) |
No (58) / I don’t know (8)
n = 66 |
Yes (37) / Planned (13)
n = 50 |
|---|---|---|
| % (n) | % (n) | |
| <50 | 50 (9) | 50 (9) |
| 50–99 | 64.3 (18) | 35.7 (10) |
| 100–249 | 67.4 (29) | 32.6 (14) |
| 250–500 | 26.3 (5) | 73.7 (14) |
| >500 | 62.5 (5) | 37.5 (3) |
Descriptive statistics (frequencies and percentages) applied, including Fisher’s exact test. No/I don’t know and yes/planned responses for guidelines in the different hospital sizes, comparison in percentages and absolute numbers.
In their comments, five respondents referred to the Critical Incident Reporting System (CIRS) as a possibility to report errors that result in no harm. One hospital’s respondent stated that she and her colleagues were not aware of any institutional support after an error, adding that efficient support usually comes from a good team and concluding that support depends of the contacted person. Another referred to the Swiss Patient Safety Foundation (“Patientensicherheit Schweiz”) and one cited the UK National Health Service’s “incident decision tree” [30] as the bases of their in-house guidelines.
This cross-sectional multi-centre study focused on how Swiss hospitals support health professionals who become second victims of adverse events. Roughly half of the contacted institutions participated in the online survey and provided information on their organisational structures and processes. Structured support programmes or guidelines for affected professionals were reported in almost a third of the hospitals regardless of type but were most common among very small and large hospitals.
Swiss hospitals incorporate several aspects of organisational support for second victims. Most respondents (just under 83%) reported that their institutions’ healthcare professionals are instructed to report adverse events to their supervisors. This rate is in line with a 2013 study on error disclosure standards in university and acute care hospitals, in which 75% of institutions reported that they either had such policies in place or would be implementing them soon [31].
According to our survey data, nearly two thirds of institutions inform their health professionals of existing support offers. Although this is a good first step towards providing effective support, placing the impetus on second victims to seek and accept support is problematic: a 2017 study found that, according to patient safety representatives’ estimates, fewer than 50% of health professionals would be willing to access support. Reasons mentioned included uncertainty about the goal of the support, a perceived punitive and blame-focussed institutional culture, fear of social stigma and personal shame [32]. In another study, Swiss anaesthesiologists stated that their institutions did not support them adequately after medical errors. They were interested in psychological counselling, but they indicated that lack of time and concerns that the psychological support would be recorded in their personal files were substantial barriers [33]. It therefore appears crucial that clinical leaders proactively approach affected health professionals following adverse events to offer support.
Most of the surveyed Swiss hospitals have a variety of support offers in place for second victims, including a range of specialists who can be contacted as necessary. Also, more than half of participating hospitals mentioned using “other persons” as supporting persons, but did not elaborate. One possible explanation is that supervisors were not a choice option and “trained peers” were thought of simply as co-workers. Still, even though second victims sometimes perceive their co-workers as unhelpful or non-supportive, they more often appreciate their emotional support [34].
A few hospitals mentioned filing adverse events in the affected persons’ personnel records and staff members’ concerns about negative personal consequences of documentation are known [14]. As this increases the risk that adverse events will simply go unreported, programmes supporting the development and implementation of second victim support guidelines recommend not adding health professionals’ involvement in adverse events to their personal records [21].
The majority of Swiss hospitals instruct their health professionals to report adverse events to their supervisors, thereby maximising the possibility of appropriate support both for the affected patient and for the second victim. Trained supervisors could improve this support by increasing their knowledge of the second victim phenomenon. However, only 31% of surveyed hospitals indicated that they actively train superiors in second victim support. Therefore, received levels of support very likely depend on the individual knowledge and engagement of whichever supervisor happens to be on duty at the time of the event. Other authors stated that when nurses reported errors, they received emotional support such as comfort or sharing experiences, but were also confronted with silence from managers and colleagues, or the gravity of their mistakes was downplayed. Only a minority actually received constructive support from managers [12]. Supporting this finding that second victims rarely received support, Scott et al. (2010) noted that what support affected staff did receive came more often from peers and colleagues than from supervisory personnel [18]. When second victims were questioned regarding their reluctance to talk to superiors, commonly cited factors included leadership behaviour, the nature of the reporting system, and the hospital culture [35]. On the positive side, the fact that nearly three quarters of Swiss hospitals asked their superiors to approach health professionals after an error can be interpreted as an important sign of willingness to support their workforce.
The matter of whether affected health professionals participate in adverse event disclosure sessions with patients was reported as dependent on the situation in more than half of the responses. Furthermore, patients understandably want to be informed about what has happened and why. It is known that in the adverse event disclosure process, it is crucial that involved health professionals and the hospital decide how the patient should be informed and by whom. This process requires a vigorous multidisciplinary team discussion on topics including diagnoses, consequences and decision on how to further engage [36].
The majority of Swiss hospitals have not implemented second victim guidelines. This corresponds, for example, with observations in Spanish hospitals [25], but contrasts with American ones, the majority of which have such guidelines in place [24]. We can suggest two possible reasons for this shortfall in the Swiss context: (1) in the USA, nationwide recommendations for organisational structures to support second victims were formulated in 2010 [20]; and (2) information on content, development and implementation processes for second victim support programmes are openly accessible [21].
However, as in Switzerland, US hospitals face continual challenges regarding funding, perceived stigma, concerns about confidentiality and lack of interest, all of which have been identified as barriers to the development of second victim support programmes [32]. In Swiss hospitals potential barriers include the lack of a firm legal foundation and the strong regional autonomy of the healthcare system (leading to inter-cantonal fragmentation), as well as a lack of commitment and sense of responsibility among hospital leaders to shed light on the issue and take action.
Notably, at the federal level, in 2006, the Swiss Patient Safety Foundation initiated a comprehensive package of evidence-based information on how to disclose and communicate adverse events to patients and families [37], as well as essentials, including training courses, on how to deal with involved healthcare professionals to mitigate negative outcomes on their health and professional life [38]. Our study revealed that acute care hospitals in Switzerland are more likely than rehabilitation and speciality clinics to use second victim guidelines.
This is probably partly a result of to the greater risk of acute care patients being affected by serious adverse events, given the complexity of medical procedures and personnel interactions compared with other care settings [4], and partly of greater sensitisation of acute care hospital leadership. As most second victim literature and related support programmes are based on acute care hospital studies and reports, the comparative shortage of information focussing on other settings such as psychiatric or rehabilitation clinics might result in less awareness of the second victim phenomenon in those contexts. For instance, one of the responding psychiatric clinics commented that the subject of second victim support had recently popped up because of a harmful incident and was currently perceived as important.
Even the process of participating in the study was perceived as having a positive outcome. One responding university hospital noted that, by revealing a blind spot in their institutional processes, our survey fostered a sense that a guideline would improve support for affected health professionals.
Evidence that second victim programmes support health professionals remains far from abundant. Still, in her study, Van Gerven concluded that, although a support team or a support protocol had no significant influence on individual outcomes after an adverse event, an organisational culture based on respect and support positively influenced the psychological impact on involved health professionals [39].
By structuring information about procedures in defined situations such as an adverse event, second victim support programmes help bring order to difficult and stressful situations. In hospitals without guidelines for second victim support, it is likely that second victims will go unidentified, meaning preventable health risks for the involved healthcare professional will go unrecognised and untreated. Where no guidelines are implemented, the quality of any available support depends entirely on who provides it, their awareness and knowledge of the second victim phenomenon and its possible long-term repercussions on the affected individual. In such cases, middle- and long-term support is likely to be either missing or difficult to access. By informing affected persons about support offers at any time of the day and designating qualified contact persons, hospital programmes provide immediate support, which is considered important to minimise second victims’ symptoms and promote their recovery [40].
Finally, some of the participating Swiss hospitals reported working with a Critical Incident Reporting System (CIRS) to collect information about medical errors and near misses. CIRS is a system to report information on events resulting on no harm to patients and to report only events without potential legal prospective. Events leading to patient harm need to be reported in a different manner [41]. There is no doubt that a CIRS is a valuable tool to recognise patient safety issues and might also be a protective factor for potential second victims; however, because CIRS reports are usually anonymous, they are not suitable to initiate targeted support to health professionals.
This study shows for the first time the current situation of organisational structures and existing guidelines for second victim support in Swiss hospitals. Other studies have focussed mainly on acute care settings, whereas our sample also included psychiatric hospitals and rehabilitation clinics. These are certainly strengths. Still, certain limitations need to be considered. For example, considering that Swiss hospitals are increasingly collaborating on diverse levels in hospital groups, we tried, if possible, to address individual hospitals separately, or asked for individual responses from each. Responses from hospital groups would reveal existing policies but would not identify variations in individual hospital cultures, in-hospital penetration of second victim support or its effectiveness in terms of relief for the affected health professionals. Also, the survey was sent to quality managers and chief operating officers, leaving open the question as to whether they could answer for their entire institutions.
Swiss hospitals are generally aware of the issue of second victims and dedicated support offers are generally prevalent, but these often lack coherence. This lack of structure bears the risk that, following adverse events, the support available to health professionals will be inadequate in terms either of quantity or of quality. As related guidelines are not widely implemented, a clear commitment from Swiss hospital executive leaders, as well as from health authorities at the national and cantonal levels could foster widespread Swiss adoption of systematic second victim support.
The appendix is available as a separate file at https://smw.ch/article/doi/smw.2020.20278.
The authors would like to thank Elisa Dolci, Cornel Schiess, Prof. Dr Maria Katapodi, and Chang Ming for their support in the preparation of the study proposal and Dr. Kris Denhaerynck for statistical advises.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Leape LL . Error in medicine. JAMA. 1994;272(23):1851–7. doi:.https://doi.org/10.1001/jama.1994.03520230061039
2 Makeham MAB , County M , Kidd MR , Dovey SM . An international taxonomy for errors in general practice: a pilot study. Med J Aust. 2002;177(2):68–72. doi:.https://doi.org/10.5694/j.1326-5377.2002.tb04668.x
3 Brennan TA , Leape LL , Laird NM , Hebert L , Localio AR , Lawthers AG , et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324(6):370–6. doi:.https://doi.org/10.1056/NEJM199102073240604
4 Schwendimann R , Blatter C , Dhaini S , Simon M , Ausserhofer D . The occurrence, types, consequences and preventability of in-hospital adverse events - a scoping review. BMC Health Serv Res. 2018;18(1):521. doi:.https://doi.org/10.1186/s12913-018-3335-z
5 Panagioti M , Khan K , Keers RN , Abuzour A , Phipps D , Kontopantelis E , et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: systematic review and meta-analysis. BMJ. 2019;366:l4185. doi:.https://doi.org/10.1136/bmj.l4185
6 Vanhaecht K , Seys D , Schouten L , Bruyneel L , Coeckelberghs E , Panella M , et al.; Dutch Peer Support Collaborative Research Group. Duration of second victim symptoms in the aftermath of a patient safety incident and association with the level of patient harm: a cross-sectional study in the Netherlands. BMJ Open. 2019;9(7):e029923. doi:.https://doi.org/10.1136/bmjopen-2019-029923
7 Scott SD , Hirschinger LE , Cox KR , McCoig M , Brandt J , Hall LW . The natural history of recovery for the healthcare provider “second victim” after adverse patient events. Qual Saf Health Care. 2009;18(5):325–30. doi:.https://doi.org/10.1136/qshc.2009.032870
8 Seys D , Wu AW , Van Gerven E , Vleugels A , Euwema M , Panella M , et al. Health care professionals as second victims after adverse events: a systematic review. Eval Health Prof. 2013;36(2):135–62. doi:.https://doi.org/10.1177/0163278712458918
9 Ajri-Khameslou M , Abbaszadeh A , Borhani F . Emergency Nurses as Second Victims of Error: A Qualitative Study. Adv Emerg Nurs J. 2017;39(1):68–76. doi:.https://doi.org/10.1097/TME.0000000000000133
10 Rassin M , Kanti T , Silner D . Chronology of medication errors by nurses: accumulation of stresses and PTSD symptoms. Issues Ment Health Nurs. 2005;26(8):873–86. doi:.https://doi.org/10.1080/01612840500184566
11 Crigger NJ , Meek VL . Toward a theory of self-reconciliation following mistakes in nursing practice. J Nurs Scholarsh. 2007;39(2):177–83. doi:.https://doi.org/10.1111/j.1547-5069.2007.00164.x
12 Schelbred AB , Nord R . Nurses’ experiences of drug administration errors. J Adv Nurs. 2007;60(3):317–24. doi:.https://doi.org/10.1111/j.1365-2648.2007.04437.x
13 Delacroix R . Exploring the experience of nurse practitioners who have committed medical errors: A phenomenological approach. J Am Assoc Nurse Pract. 2017;29(7):403–9. doi:.https://doi.org/10.1002/2327-6924.12468
14 McLennan SR , Engel-Glatter S , Meyer AH , Schwappach DL , Scheidegger DH , Elger BS . The impact of medical errors on Swiss anaesthesiologists: a cross-sectional survey. Acta Anaesthesiol Scand. 2015;59(8):990–8. doi:.https://doi.org/10.1111/aas.12517
15 Van Gerven E , Vander Elst T , Vandenbroeck S , Dierickx S , Euwema M , Sermeus W , et al. Increased risk of burnout for physicians and nurses involved in a patient safety incident. Med Care. 2016;54(10):937–43. doi:.https://doi.org/10.1097/MLR.0000000000000582
16 Burlison JD , Quillivan RR , Scott SD , Johnson S , Hoffman JM . The Effects of the Second Victim Phenomenon on Work-Related Outcomes: Connecting Self-Reported Caregiver Distress to Turnover Intentions and Absenteeism. J Patient Saf. 2016. doi:.https://doi.org/10.1097/PTS.0000000000000301
17 Schwappach DL , Boluarte TA . The emotional impact of medical error involvement on physicians: a call for leadership and organisational accountability. Swiss Med Wkly. 2009;139(1-2):9–15.
18 Scott SD , Hirschinger LE , Cox KR , McCoig M , Hahn-Cover K , Epperly KM , et al. Caring for our own: deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf. 2010;36(5):233–40. doi:.https://doi.org/10.1016/S1553-7250(10)36038-7
19Conway J, Federico F, Stewart K, Campbell M. Respectful Mangagemnt of Serious Clinical Adverse Events (Second Editon). IHI Innovation Series white paper. Cambridge, Massachusetts: Institute for Healthcare Improvement; 2011.
20National Quality Forum. Safe Practices for Better Healthcare - 2010. Update: A Consensus Report. Washington, DC: NQF; 2010.
21 Pratt S , Kenney L , Scott SD , Wu AW . How to develop a second victim support program: a toolkit for health care organizations. Jt Comm J Qual Patient Saf. 2012;38(5):235–40, 193. doi:.https://doi.org/10.1016/S1553-7250(12)38030-6
22 Edrees H , Connors C , Paine L , Norvell M , Taylor H , Wu AW . Implementing the RISE second victim support programme at the Johns Hopkins Hospital: a case study. BMJ Open. 2016;6(9):e011708. doi:.https://doi.org/10.1136/bmjopen-2016-011708
23 Edrees H , Wu A . The aftermath of medical errors: Supporting our second victim colleagues. Int J Qual Health Care. 2016;28(suppl 1):65. doi:.https://doi.org/10.1093/intqhc/mzw104.103
24 White AA , Brock DM , McCotter PI , Hofeldt R , Edrees HH , Wu AW , et al. Risk managers’ descriptions of programs to support second victims after adverse events. J Healthc Risk Manag. 2015;34(4):30–40. doi:.https://doi.org/10.1002/jhrm.21169
25 Mira JJ , Lorenzo S , Carrillo I , Ferrús L , Pérez-Pérez P , Iglesias F , et al.; Research Group on Second and Third Victims. Interventions in health organisations to reduce the impact of adverse events in second and third victims. BMC Health Serv Res. 2015;15(1):341. doi:.https://doi.org/10.1186/s12913-015-0994-x
26 Edrees HH , Morlock L , Wu AW . Do Hospitals Support Second Victims? Collective Insights From Patient Safety Leaders in Maryland. Jt Comm J Qual Patient Saf. 2017;43(9):471–83. doi:.https://doi.org/10.1016/j.jcjq.2017.01.008
27H+ Die Spitäler der Schweiz. Mitgliederverzeichnis 2018 Available from: http://www.hplus.ch/de/servicenav/ueber_uns/mitglieder/mitgliederverzeichnis/nocache/1/.
28Medically Induced Trauma Support Services (MITSS). MITTS Organizational Assessment Tool For Clinicaian Support 2017 Available from: http://mitss.org/.
29R: A Language and Environment for Statistical Computing [Internet]. R Foundation for Statistical Computing. 2017. Available from: https://www.R-project.org/.
30Meadows S, Baker K, Butler J. Advances in Patient Safety The Incident Decision Tree: Guidelines for Action Following Patient Safety Incidents. In: Henriksen K, Battles JB, Marks ES, Lewin DI, editors. Advances in Patient Safety: From Research to Implementation (Volume 4: Programs, Tools, and Products). Rockville (MD): Agency for Healthcare Research and Quality (US); 2005.
31 McLennan S , Engel S , Ruhe K , Leu A , Schwappach D , Elger B . Implementation status of error disclosure standards reported by Swiss hospitals. Swiss Med Wkly. 2013;143:w13820. doi:.https://doi.org/10.4414/smw.2013.13820
32 Edrees HH , Wu AW . Does One Size Fit All? Assessing the Need for Organizational Second Victim Support Programs. J Patient Saf. 2017. doi:.https://doi.org/10.1097/PTS.0000000000000321
33 McLennan SR , Engel-Glatter S , Meyer AH , Schwappach DL , Scheidegger DH , Elger BS . The impact of medical errors on Swiss anaesthesiologists: a cross-sectional survey. Acta Anaesthesiol Scand. 2015;59(8):990–8. doi:.https://doi.org/10.1111/aas.12517
34 Cabilan CJ , Kynoch K . Experiences of and support for nurses as second victims of adverse nursing errors: a qualitative systematic review. JBI Database Syst Rev Implement Reports. 2017;15(9):2333–64. doi:.https://doi.org/10.11124/JBISRIR-2016-003254
35 Vrbnjak D , Denieffe S , O’Gorman C , Pajnkihar M . Barriers to reporting medication errors and near misses among nurses: A systematic review. Int J Nurs Stud. 2016;63:162–78. doi:.https://doi.org/10.1016/j.ijnurstu.2016.08.019
36Birks Y, Harrison R, Bosanquet K, Hall J, Harden M, Entwistle V, et al. An exploration of the implementation of open disclosure of adverse events in the UK: a scoping review and qualitative exploration. Southampton (UK): Health Services and Delivery Research; 2014.
37Wenn etwas schief geht [Internet]. Stiftung für Patientensicherheit. 2006. Available from: https://www.patientensicherheit.ch/fileadmin/user_upload/3_Bildung/KOM-Kurse/1_SR_1_Wenn_etwas_schief_geht_D_160725_.pdf.
38Schwappach D, Hochreutener A-M, von Laue N, Frank O. Täter als Opfer. Zurich: Stiftung für Patientensicherheit Schweiz; 2010
39 Van Gerven E , Bruyneel L , Panella M , Euwema M , Sermeus W , Vanhaecht K . Psychological impact and recovery after involvement in a patient safety incident: a repeated measures analysis. BMJ Open. 2016;6(8):e011403. doi:.https://doi.org/10.1136/bmjopen-2016-011403
40 Scott SD , McCoig MM . Care at the point of impact: Insights into the second-victim experience. J Healthc Risk Manag. 2016;35(4):6–13. doi:.https://doi.org/10.1002/jhrm.21218
41Aktionsbündnis Patientensicherheit, Platform Patientensicherheit, Patientensicherheit Schweiz. Einrichtung und erfolgreicher Betrieb eines Berichts- und Lernsystems (CIRS). Handlungsempfehlung für stationäre Einrichtungen im Gesundheitswesen. Berlin: 2016.
No financial support and no other potential conflict of interest relevant to this article was reported.