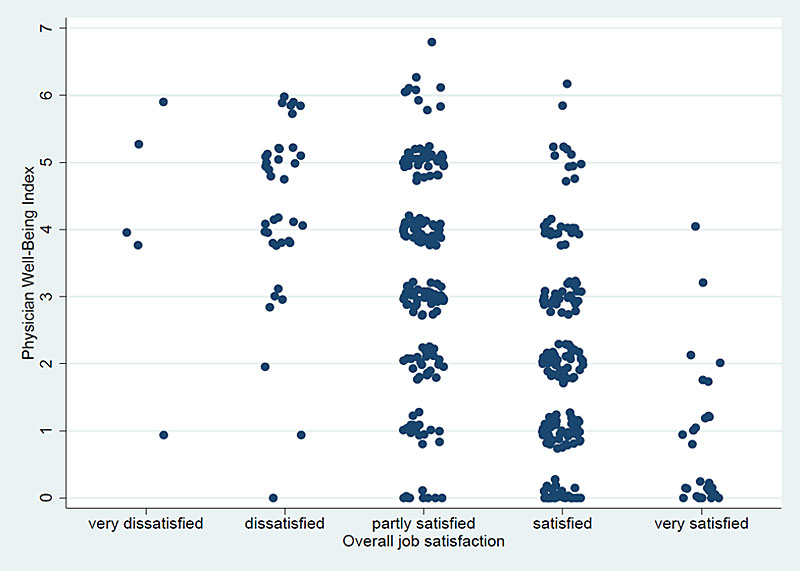
Panel A: Overall job satisfaction.
DOI: https://doi.org/10.4414/smw.2020.20255
Physician well-being, defined as the optimal interaction of practice efficiency, culture of wellness and personal resilience [1], has become an increasing concern in recent years. In the US, more than 40% of physicians suffer from burnout, and in a national survey of Swiss primary care practitioners about one third presented moderate-degree burnout [2, 3]. Physician well-being is not only associated with empathy and the quality of work relationships [4]; doctors with a reduced well-being may also have a higher prevalence of suicidal ideation [5–7] and motor vehicle accidents [8]. Well-being also has a direct impact on patient care, as it influences workplace productivity and efficiency [9–11], quality of care [12] and patient satisfaction and safety [13–15]. Given its association with patient safety, physician well-being has been recommended as a quality indicator [9].
Development research has demonstrated that the period around 30 years of age, during which physicians usually complete their residency training, is “a time to complete early adulthood with pursuit of aspirations, establishment of a niche in society, and raising a family” [16, 17]. However, residency training is also a challenging and stressful period [4]. Intense work demands, limited control and the potential for work-home interference may predispose resident physicians to burnout [18]. Moreover, burnout appears to be particularly prevalent in primary care specialties [19, 20], due to the high administrative workload and patient complexity [21, 22].
To our knowledge, the well-being of general internal medicine (GIM) residents in Switzerland has never been studied. We therefore aimed to evaluate the well-being, as well as associated personal and work-related factors, of Swiss GIM residents in a representative sample. We hypothesised that a substantial proportion of Swiss GIM residents experience a reduced well-being and that this is associated with several personal and work-related factors.
We conducted an electronic survey in GIM residents working in the inpatient services at all five Swiss university hospitals and in eight high-volume non-university teaching hospitals in June 2018. These hospitals covered both the German- and French-speaking parts of Switzerland. Swiss GIM residents undergo five years of in- and outpatient training, consisting of three years of mandatory basic training in GIM and two years of elective training in various other medical specialties. We chose these hospitals because they employ a large number of GIM residents, thus increasing the sample size and efficiency of our survey and based on previous collaborative relationships. The head physicians of the 13 GIM divisions were invited to participate in the study, and they all allowed their residents to take the survey. The ethics committee of the canton of Bern waived the need for ethical approval/informed consent because our project was not within the scope of the Swiss Federal Act on Research on Human Beings.
We developed an anonymous online survey tool using the REDCap™ software [23]. To reduce the completion time of the survey and to minimise nonresponse and measurement errors, we chose a user-friendly web design and provided German and French language versions of the survey. The survey tool was successfully tested in a pilot study with ten residents from Bern University Hospital, and survey completion was estimated to require four to five minutes. We then obtained the email addresses of all 880 residents working in the 13 participating GIM divisions. We sent an email containing an invitation to participate, a brief description of the survey goals and a web link to the online survey to all 880 residents. Four email reminders (at 7, 14, 21 and 28 days after the initial invitation to participate) were sent out to all participants. To ensure privacy, completed responses could not be linked to individual email addresses. After completion of the survey, residents’ email addresses were deleted from the database by a blinded statistician.
The survey included three parts: (1) the collection of personal and work-related characteristics, (2) completion of the seven-item Physician Well-Being Index (PWBI), and (3) assessment of job satisfaction, recent suicidal ideation, self-reported medical errors and intention to leave clinical practice.
We collected the following personal and work-related characteristics previously described as associated with well-being or burnout: age [24, 25], sex [25, 26], language [27], relationship status [28], partner working as a healthcare professional [24, 29], having children [24, 25], years of postgraduate training [24], level of employment in %, average working hours per week [30, 31], number of night shifts per month [32, 33], percentage of time spent on administrative tasks on an average working day [34], perception of doing rewarding/meaningful work (“Please estimate how many hours you spend in a typical day at work on activities that you find personally rewarding”; 0–2.5 hours, 2.5–5 hours, 5–7.5 hours and ≥7.5 hours) [35], sense of vocation (“For me, the practice of medicine is a vocation”; 5-point Likert scale from 1 “strongly disagree” to 5 “strongly agree”) [36], willingness to become a physician again (5-point Likert scale from 1 “not at all” to 5 “absolutely”) [37], satisfaction with quality of training (5-point Likert scale from 1 “very dissatisfied” to 5 “very satisfied”) [38], satisfaction with the electronic medical record (EMR) (5-point Likert scale from 1 “very dissatisfied” to 5 “very satisfied”) [39], satisfaction with personal job autonomy (5-point Likert scale from 1 “very dissatisfied” to 5 “very satisfied”) [40], and satisfaction with current income (3-point Likert scale from 1 “dissatisfied” to 3 “completely satisfied”) [41].
We assessed physician well-being using a version of the PWBI that has been specifically adapted for residents [5]. The seven-item questionnaire covers six dimensions, including burnout, depression, stress, fatigue, and mental and physical quality of life during the last month. Respondents are asked to answer seven yes/no questions and received a score from 0–7 (one point for each item answered “yes”), with higher scores indicating a decrease in well-being. Previous versions of the PWBI have shown evidence of content-related and internal structure validity, as well as reliability [42, 43]. A threshold score of ≥5 points has a sensitivity of 70% and a specificity of 79% for identifying residents with a low mental quality of life, and increases the likelihood of high fatigue, suicidal ideation and self-perceived medical error [5]. Although the Maslach Burnout Inventory (MBI) is considered the reference standard to measure burnout, its length limits its usability. The PWBI quantifies burnout using single-item measures for the subdomains emotional exhaustion and depersonalisation which are adapted from the full MBI [43]. Single-item measures for emotional exhaustion and depersonalisation have been shown to exhibit strong associations with key outcomes, such as suicidality, and provide meaningful information on burnout [44, 45]. Because no German or French versions of the PWBI were available, we performed a forward-backward translation from the English version of the PWBI into German and French, according to previously published recommendations on the cross-cultural adaptation of self-report measures [46]. First, two independent native German and French speakers performed forward translations from the original English version into German and French. Second, two native English speakers performed backward translations into English. A committee of three experts reviewed all the translations and reached a consensus on any discrepancies.
We assessed overall job satisfaction using a single-item measure (“Overall, how satisfied are you with your job?”) that was rated on a 5-point Likert scale (from 1 “very dissatisfied” to 5 “very satisfied”) [47]. Although single-item scales for measuring job satisfaction are frequently criticised [48], evidence suggests that there are acceptable corrected mean correlations between single-item and multi-item satisfaction measures, and that single-item measures have a reasonable test-retest reliability [49]. Furthermore, we assessed recent suicidal ideation and perceived medical errors by asking simple yes/no questions (“During the past 12 months, have you had thoughts of taking your own life?”, “Are you concerned you have made any major medical errors in the last three months?”), as has been done previously in other studies [5, 6, 50]. Finally, the residents’ intention to leave clinical practice was assessed similarly to in a previous study [37] by asking “How much do you currently wish you could leave clinical practice?” The answer was rated on a 5-point Likert scale (from 1 “not at all” to 5 “absolutely”).
In descriptive analyses, we assessed the personal and work-related characteristics of the respondents, the mean PWBI score, and the proportion of residents with a PWBI score of ≥5, indicating a reduced well-being. In the case of missing values, we used simple imputations using the median value, as has been done previously [51].
We performed multivariable logistic mixed-effects regressions to explore the associations of personal and work-related factors with well-being. The outcome variable was reduced well-being, measured as a binary variable (PWBI score of ≥5). Predictor variables included personal (age, sex, language, relationship status, partner working as a healthcare professional and having children) and work-related (years of postgraduate training, level of employment, working hours, administrative workload, rewarding work hours per day, satisfaction with training quality, satisfaction with EMR, satisfaction with personal job autonomy and satisfaction with income) factors. To restrict the number of predictor variables, we decided not to include “night shifts per month” (somewhat redundant with “working hours per week”), “vocation” (not modifiable), and “willingness to become a physician again” (bidirectional causality) in the model. Due to the correlated nature of data within hospitals, we introduced a random intercept for hospitals in the mixed-effects models.
We used Spearman’s rank correlation coefficient to examine the relationships between the PWBI and job satisfaction, recent suicidal ideation, self-reported medical errors and intention to leave clinical practice. A correlation coefficient from 0 to ±0.1 indicates a negligible, from ±0.10 to ±0.39 a weak, from ±0.40 to ±0.69 a moderate, from ±0.70 to ±0.89 a strong, and from ±0.90 to ±1.00 a very strong correlation [52]. All analyses were done using Stata 14.2 [53].
Overall, 472 residents out of the 880 invited responded to our survey (response rate 54%). Of these, 20 returned a form with no information other than language and demographic variables, and two returned an incomplete PWBI questionnaire, leaving a final sample of 450 residents. The respondents’ characteristics are shown in table 1.
Table 1 Personal characteristics.
| Characteristic |
Respondents (N = 450)*
n (%) or median (IQR) |
|---|---|
| Age, years | 30 (28; 31) |
| Female sex | 276 (61) |
| Language | |
| German | 245 (54) |
| French | 205 (46) |
| Relationship status | |
| Single | 102 (23) |
| In a relationship | 252 (56) |
| Married | 96 (21) |
| Partner working as a healthcare professional | 167 (37) |
| Having children | 65 (14) |
IQR = interquartile range *Two respondents had missing values for “partner working as a healthcare professional”.
Almost all the participants worked full-time (table 2), with a median of 55 working hours per week and three night shifts per month. Residents indicated that they spend 70% of their time on administrative tasks during an average working day, and 52% spent less than 2.5 hours per day on activities that they find personally rewarding. Twenty-one percent reported that they would rather not or would not at all become physicians again. Only 5% were dissatisfied with the quality of training in their division, but 36% were dissatisfied or very dissatisfied with the hospital EMR. Eighty-nine percent were at least partially satisfied with their personal job autonomy, and 90% with their current income. Nine percent were dissatisfied or very dissatisfied with their job in general.
Table 2 Work-related factors.
| Characteristic |
Respondents (N = 450)*
n (%) or median (IQR) |
|---|---|
| Years of postgraduate training, no. | 4 (3; 5) |
| Level of employment | |
| 100% | 431 (96) |
| 80% | 4 (1) |
| 60% | 2 (0) |
| 50% | 13 (3) |
| Working hours per week†, no. | 55 (50; 60) |
| Night shifts per month‡, no. | 3 (0; 5) |
| Administrative workload§, % | 70 (60; 80) |
| Rewarding work hours per day¶, no. | |
| >7.5 | 5 (1) |
| 5.0–7.5 | 27 (6) |
| 2.5–5.0 | 183 (41) |
| 0–2.5 | 235 (52) |
| Medicine as a vocation | |
| Completely agree | 76 (17) |
| Rather agree | 166 (37) |
| Partially agree | 129 (29) |
| Rather disagree | 55 (12) |
| Strongly disagree | 22 (5) |
| Would become physician again | |
| Absolutely | 102 (23) |
| Probably | 158 (35) |
| Don’t know | 97 (22) |
| Rather not | 77 (17) |
| Not at all | 16 (4) |
| Satisfaction with training quality | |
| Very satisfied | 71 (16) |
| Satisfied | 261 (58) |
| Partially satisfied | 94 (21) |
| Dissatisfied | 23 (5) |
| Very dissatisfied | 0 (0) |
| Satisfaction with electronic medical record | |
| Very satisfied | 37 (8) |
| Satisfied | 120 (27) |
| Partially satisfied | 132 (29) |
| Dissatisfied | 88 (20) |
| Very dissatisfied | 70 (16) |
| Satisfaction with personal job autonomy | |
| Very satisfied | 29 (6) |
| Satisfied | 236 (52) |
| Partially satisfied | 141 (31) |
| Dissatisfied | 34 (8) |
| Very dissatisfied | 5 (1) |
| Satisfaction with income | |
| Completely satisfied | 234 (52) |
| Partially satisfied | 47 (10) |
| Dissatisfied | 169 (38) |
IQR = interquartile range. * One respondent had missing values for “working hours per week”, one for “night shifts per month”, two for “medicine as a vocation”, one for “satisfaction with training quality”, three for “satisfaction with electronic medical record”, five for “satisfaction with personal job autonomy”. † Average working hours per week during the last three months. ‡ Number of night shifts per month during the last six months. § Percentage of time spent on administrative tasks on an average working day during the last three months. ¶ Hours spent on activities that one finds personally rewarding in a typical day at work.
Overall, 31% of residents were concerned about having made a major medical error during the last three months, and 4% reported suicidal thoughts during the last year (table 3). Thirty-four percent wished to leave clinical practice at least sometimes.
Table 3 Practice-related outcomes.
| Characteristic |
Respondents (N = 450)*
n (%) or median (IQR) |
|---|---|
| Overall job satisfaction | |
| Very satisfied | 29 (6) |
| Satisfied | 189 (42) |
| Partially satisfied | 183 (41) |
| Dissatisfied | 38 (8) |
| Very dissatisfied | 5 (1) |
| Major medical errors† | 139 (31) |
| Suicidal ideation‡ | 16 (4) |
| Intention to leave clinical practice | |
| Not at all | 158 (35) |
| Rather not | 141 (31) |
| Sometimes | 108 (24) |
| Rather yes | 30 (7) |
| Absolutely | 12 (3) |
IQR = interquartile range * Six respondents had missing values for “overall job satisfaction”, one for “major medical errors”, one for “suicidal ideation”, and one for “intention to leave clinical practice”. † Being concerned about having made any major medical errors during the last three months. ‡ Having had thoughts of taking one’s own life during the last 12 months.
The mean PWBI score was 2.7 (standard deviation 1.7). Nineteen percent of residents had a score of ≥5 points, indicating a reduced well-being (table 4). Sixty percent felt burned out from work (emotional exhaustion) during the last month, 47% were worried that their work was hardening them emotionally (depersonalisation), and 32% reported both symptoms. Fifty-seven percent indicated that they were bothered by emotional problems, and 42% felt that things they had to do were piling up so high that they could not overcome them.
Table 4 Physician Well-Being Index (PWBI).
| Items of the PWBI* |
Endorsing item (N = 450)
n (%) |
|---|---|
| Have you felt burned out from your work? | 268 (60) |
| Have you worried that your work is hardening you emotionally? | 211 (47) |
| Have you often been bothered by feeling down, depressed or hopeless? | 135 (30) |
| Have you fallen asleep while stopped in traffic or driving? | 14 (3) |
| Have you felt that all the things you had to do were piling up so high that you could not overcome them? | 191 (42) |
| Have you been bothered by emotional problems (anxious, depressed, or irritable)? | 258 (57) |
| Has your physical health interfered with your ability to do your daily work at home and/or away from home? | 138 (31) |
| No. of items present | n (%) |
| 0 | 57 (13) |
| 1 | 75 (17) |
| 2 | 80 (18) |
| 3 | 78 (17) |
| 4 | 74 (16) |
| 5 | 67 (15) |
| 6 | 18 (4) |
| 7 | 1 (0) |
* During the last month
After adjustment, the likelihood of a reduced well-being increased by 19% per year of age (odds ratio [OR] 1.19, 95% confidence interval [CI] 1.05–1.34) (table 5). Residents with children were significantly less likely to show a reduced well-being than residents without children (OR 0.12, 95% CI 0.03–0.51). The likelihood of a reduced well-being increased by 4% for every additional hour worked per week (OR 1.04, 95% CI 1.01–1.07). Respondents who spent less than 2.5 hours per work day on activities that they find personally rewarding were almost four times more likely to have a reduced well-being (OR 3.73, 95% CI 2.01–6.92). Although residents who had low satisfaction with the quality of their training (OR 1.64, 95% CI 0.56–4.84) and their personal job autonomy (OR 2.24, 95% CI 0.96–5.23) were also somewhat more likely to experience a reduced well-being, and those with a partner working as a healthcare professional (OR 0.54, 95% CI 0.28–1.06) were somewhat less likely to have a reduced well-being, these associations failed to reach statistical significance. Female sex, relationship status, years of postgraduate training, level of employment, administrative workload, satisfaction with the EMR and income were not associated with well-being.
Table 5 Associations between personal or work-related factors and reduced well-being*.
| Factors | Adjusted † OR (95% CI) | p-value |
|---|---|---|
| Age, per year | 1.19 (1.05–1.34) | 0.005 |
| Female sex | 1.60 (0.87–2.95) | 0.134 |
| French language | 1.30 (0.70–2.38) | 0.405 |
| Married or in a relationship | 0.84 (0.43–1.63) | 0.604 |
| Partner working as a healthcare professional | 0.54 (0.28–1.06) | 0.073 |
| Having children | 0.12 (0.03–0.51) | 0.004 |
| Years of postgraduate training, per year | 0.94 (0.76–1.17) | 0.568 |
| Level of employment, per 10% | 0.90 (0.57–1.44) | 0.671 |
| Working hours per week, per hour‡ | 1.04 (1.01–1.07) | 0.016 |
| Administrative workload, per 10%§ | 0.97 (0.80–1.17) | 0.759 |
| <2.5 rewarding work hours per day¶ | 3.73 (2.01–6.92) | <0.001 |
| Low satisfaction with training quality‖ | 1.64 (0.56–4.84) | 0.370 |
| Low satisfaction with electronic medical record‖ | 1.29 (0.72–2.30) | 0.392 |
| Low satisfaction with personal job autonomy‖ | 2.24 (0.96–5.23) | 0.061 |
| Low satisfaction with income** | 0.97 (0.43–2.20) | 0.936 |
OR = odds ratio; CI = confidence interval * Reduced well-being was defined as a PWBI score of ≥5. † Adjustments were made for all other variables. ‡ Average working hours per week during the last three months. § Percentage of time spent on administrative tasks on an average working day during the last three months. ¶ Hours spent on activities that one finds personally rewarding in a typical day at work. ‖ Dichotomised as high (“very satisfied”, “satisfied” or “partially satisfied”) versus low (“dissatisfied” or “very dissatisfied”). ** Dichotomised as high (“completely satisfied” or “partially satisfied”) versus low (“dissatisfied”).
We found statistically significant, albeit weak to moderate, correlations between the PWBI and overall job satisfaction (rs [Spearman’s rho] = −0.54, p <0.001), medical errors (rs = 0.18, p <0.001), suicidal ideation (rs = 0.12, p = 0.009) and intention to leave clinical practice (rs = 0.38, p <0.001). Scatterplots of the relationships between the PWBI and practice-related outcomes are shown in the appendix 1.
Our survey demonstrates that a substantial proportion of Swiss GIM residents suffer from a reduced well-being or distress, or have career choice regret. Spending few work hours on activities that are perceived as rewarding and number of hours worked were the most significant modifiable predictors of reduced well-being. A reduced level of well-being was correlated with low job satisfaction, the perception of having committed major medical errors, suicidal ideation and the wish to leave clinical practice.
In a survey of US residents from all specialties, 16% had a reduced well-being based on the PWBI, 70% felt burned out, and 65% expressed emotional problems [5]. In surveys of US GIM residents, 15% reported having an impaired quality of life, 43–52% had at least one symptom of burnout, and career choice regret was present in 12% [54, 55]. Swiss residents usually do not have educational debts (a predictor for physician burnout) [54], enjoy a relatively strictly enforced 50-hour work week and, according to our survey, are generally satisfied with their job, including their training, autonomy and income. Yet the prevalence of distress among Swiss GIM residents seems to be at least as high as in the US. A potential explanation for the high prevalence of distress may lie in overly rigid duty hour regulations, which were originally introduced to mitigate resident fatigue and to improve patient safety. However, an average shift length of 10 hours may simply not suffice to accomplish the multiple tasks required in a teaching hospital, and may result in a dense and stressful work schedule, overtime and frequent hand-offs [56–58].
The perception of having few personally rewarding work hours was the strongest predictor of reduced well-being in our analysis. Over half the participants reported having only 0–2.5 personally rewarding work hours a day. Physicians who spend <20% of their work on the activity they find most meaningful are nearly three times more likely to feel burned out [59, 60]. Physicians usually perceive direct patient care as the most meaningful aspect and activity of their work [59]. A recent time-motion study demonstrated that Swiss GIM residents spend an average of only 1.7 hours per day with patients and about 5.2 hours (about half the workday) using computers [61]. Although the burden of administrative tasks and EMR use has been found to contribute to physician dissatisfaction and burnout in prior studies [34, 39, 62–64], we did not find an association between well-being and time spent on administrative tasks or satisfaction with the EMR. However, Swiss residents are usually not involved in coding for billing purposes or documenting quality indicators, and administrative and medical activities are increasingly delegated to non-physician staff. Whether such teamwork-based approaches will bring residents back to patient bedsides and increase resident satisfaction must be explored further.
Not surprisingly, longer working hours were significantly associated with a reduced well-being in our study and in others [30, 31]. As more restrictive regulation of work hours to below 50 hours per week would likely result in an even more packed work schedule [56–58], we believe that organisational measures, such as the reduction of redundancies and the delegation of administrative tasks to non-physician personnel, should be prioritised over further work hour restrictions [65, 66]. Whether more flexible duty hours would improve well-being is uncertain. Studies from US surgical and internal medicine residency programs have demonstrated that duty hour flexibility may not necessarily translate into better medical education outcomes or resident satisfaction [67, 68]. However, these results may not be generalisable to Swiss residency programs, as Switzerland has much more restrictive duty hour regulations than the US (50 vs 80 hours per week). Therefore, whether more flexible duty hour models could improve Swiss GIM residents’ well-being must be examined in future studies.
Although the first year of residency is known to be especially stressful [69], postgraduate training years was not associated with well-being, whereas older residents were more likely to have a reduced well-being in our study. A potential explanation is that lifestyle issues tend to become more important with increasing age [70]. Residents with a partner working as a healthcare professional, and especially those who have children, were less likely to experience distress. In contrast to prior studies demonstrating that having young children and being in a relationship with someone working as a healthcare professional are risk factors for burnout [24, 25, 29], our findings indicate that Swiss GIM residents do not appear to experience a conflict between job and family life.
A low satisfaction with job autonomy tended to increase the risk of reduced well-being in our study. Autonomy, with greater control over the pace and content of clinical work, and the provision of an appropriate learning environment with adequate supervision support are key factors for professional satisfaction [10, 71]. Experiencing sufficient autonomy in their various professional roles as learners and caregivers is important to residents [72]. The personalisation of residency training and the development of GIM entrustable professional activities (EPAs), which allow supervisors to make competency-based decisions about the responsibilities that can be entrusted to a resident, may improve that resident’s feeling of autonomy and well-being [72–74].
As physician well-being is associated with quality of care, patient safety and physician health [12, 14, 15, 75], hospitals have an ethical obligation to improve physician well-being, for example by providing adequate support structures and staffing levels. Given the costs associated with burnout, turnover, lost revenue due to loss of productivity, and the downstream costs related to patient safety problems, investments in physician well-being may well be cost-effective [76].
Our study has potential limitations. First, the response rate of our survey was 54%. While a higher rate would have been desirable, our response rate compares well with those of previous surveys conducted in GIM residents (8–77%) [4, 5, 54, 77]. As we included a broad range of large Swiss teaching hospitals, we believe that our sample is representative of such hospitals. However, our results may not be generalisable to residency training programs in smaller hospitals. Second, while we explored the associations between a broad range of personal and work-related factors and well-being, we could not examine other potential predictors, such as infrastructural factors (e.g., office space). Third, because of the cross-sectional design of our survey, we could not establish the causality of any relationships. Finally, as in all surveys, our results are subject to self-reporting bias.
Our survey shows a distressed Swiss GIM resident workforce. About 20% of Swiss GIM residents suffer from a reduced well-being or career choice regret, and a substantial proportion show symptoms of emotional exhaustion and depersonalisation. Two potentially modifiable factors, a low number of rewarding work hours and longer working hours, were associated with reduced well-being. Given the human and financial costs of physician distress to both patients and physicians, healthcare organisations have an ethical and professional responsibility to preserve and improve physician well-being, for instance by providing adequate support structures and staffing levels.
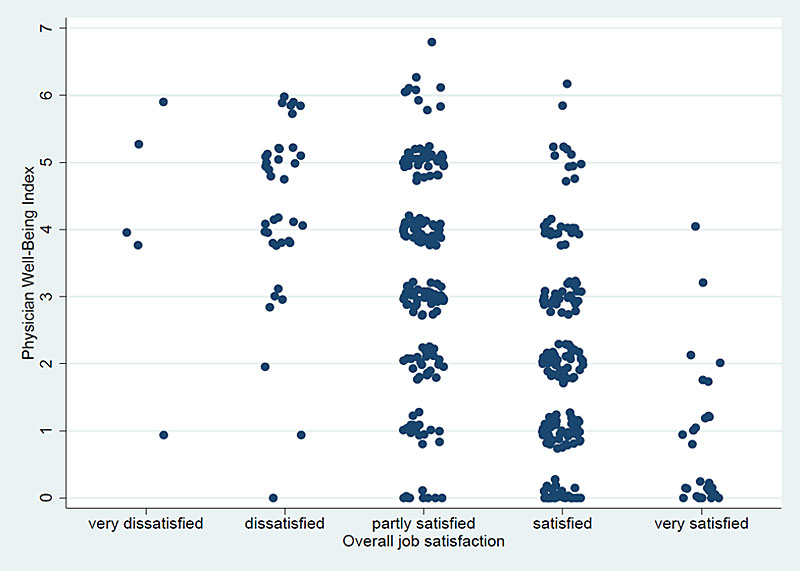
Panel A: Overall job satisfaction.

Panel B: Major medical errors.

Panel C: Suicidal ideation.

Panel D: Intention to leave clinical practice.
The Physician Well-Being Index was kindly provided by MedEd Web Solutions and the Mayo Clinic. We thank Maxime Schmutz for his support in providing a French version of the survey.
This study was supported by a grant from the Swiss Society of General Internal Medicine (SGAIM) Foundation. The sponsor had no role in study design, data collection, site monitoring, data analysis, data interpretation or writing of the manuscript.
The authors declare that they have no conflicts of interest.
1Bohman B, Dyrbye L, Sinsky Ch, Linzer M, Olson K, Babott S. Physician Well-Being: The Reciprocity of Practice Efficiency, Culture of Wellness, and Personal Resilience 2017 [updated 2017 April 26; cited 2019 June 30]. Available from: https://catalyst.nejm.org/physician-well-being-efficiency-wellness-resilience/
2 Shanafelt TD , West CP , Sinsky C , Trockel M , Tutty M , Satele DV , et al. Changes in Burnout and Satisfaction With Work-Life Integration in Physicians and the General US Working Population Between 2011 and 2017. Mayo Clin Proc. 2019;94(9):1681–94. doi:.https://doi.org/10.1016/j.mayocp.2018.10.023
3 Goehring C , Bouvier Gallacchi M , Künzi B , Bovier P . Psychosocial and professional characteristics of burnout in Swiss primary care practitioners: a cross-sectional survey. Swiss Med Wkly. 2005;135(7-8):101–8.
4 Shanafelt TD , West C , Zhao X , Novotny P , Kolars J , Habermann T , et al. Relationship between increased personal well-being and enhanced empathy among internal medicine residents. J Gen Intern Med. 2005;20(7):559–64. doi:.https://doi.org/10.1007/s11606-005-0102-8
5 Dyrbye LN , Satele D , Sloan J , Shanafelt TD . Ability of the physician well-being index to identify residents in distress. J Grad Med Educ. 2014;6(1):78–84. doi:.https://doi.org/10.4300/JGME-D-13-00117.1
6 Dyrbye LN , Satele D , Sloan J , Shanafelt TD . Utility of a brief screening tool to identify physicians in distress. J Gen Intern Med. 2013;28(3):421–7. doi:.https://doi.org/10.1007/s11606-012-2252-9
7 Dyrbye LN , Thomas MR , Massie FS , Power DV , Eacker A , Harper W , et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334–41. doi:.https://doi.org/10.7326/0003-4819-149-5-200809020-00008
8 West CP , Tan AD , Shanafelt TD . Association of resident fatigue and distress with occupational blood and body fluid exposures and motor vehicle incidents. Mayo Clin Proc. 2012;87(12):1138–44. doi:.https://doi.org/10.1016/j.mayocp.2012.07.021
9 Wallace JE , Lemaire JB , Ghali WA . Physician wellness: a missing quality indicator. Lancet. 2009;374(9702):1714–21. doi:.https://doi.org/10.1016/S0140-6736(09)61424-0
10 Friedberg MW , Chen PG , Van Busum KR , Aunon F , Pham C , Caloyeras J , et al. Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. Rand Health Q. 2014;3(4):1.
11 Firth-Cozens J , Greenhalgh J . Doctors’ perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997;44(7):1017–22. doi:.https://doi.org/10.1016/S0277-9536(96)00227-4
12 DeVoe J , Fryer GE, Jr , Hargraves JL , Phillips RL , Green LA . Does career dissatisfaction affect the ability of family physicians to deliver high-quality patient care? J Fam Pract. 2002;51(3):223–8.
13 Weng HC , Hung CM , Liu YT , Cheng YJ , Yen CY , Chang CC , et al. Associations between emotional intelligence and doctor burnout, job satisfaction and patient satisfaction. Med Educ. 2011;45(8):835–42. doi:.https://doi.org/10.1111/j.1365-2923.2011.03985.x
14 Shanafelt TD , Balch CM , Bechamps G , Russell T , Dyrbye L , Satele D , et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251(6):995–1000. doi:.https://doi.org/10.1097/SLA.0b013e3181bfdab3
15 Wen J , Cheng Y , Hu X , Yuan P , Hao T , Shi Y . Workload, burnout, and medical mistakes among physicians in China: A cross-sectional study. Biosci Trends. 2016;10(1):27–33. doi:.https://doi.org/10.5582/bst.2015.01175
16 Levinson DJ . A conception of adult development. Am Psychol. 1986;41(1):3–13. doi:.https://doi.org/10.1037/0003-066X.41.1.3
17 Raj KS . Well-Being in Residency: A Systematic Review. J Grad Med Educ. 2016;8(5):674–84. doi:.https://doi.org/10.4300/JGME-D-15-00764.1
18 Thomas NK . Resident burnout. JAMA. 2004;292(23):2880–9. doi:.https://doi.org/10.1001/jama.292.23.2880
19 Shanafelt TD , Boone S , Tan L , Dyrbye LN , Sotile W , Satele D , et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–85. doi:.https://doi.org/10.1001/archinternmed.2012.3199
20 Faber DA , Joshi S , Ebell MH . US Residency Competitiveness, Future Salary, and Burnout in Primary Care vs Specialty Fields. JAMA Intern Med. 2016;176(10):1561–3. doi:.https://doi.org/10.1001/jamainternmed.2016.4642
21 Freeborn DK . Satisfaction, commitment, and psychological well-being among HMO physicians. West J Med. 2001;174(1):13–8. doi:.https://doi.org/10.1136/ewjm.174.1.13
22 Shanafelt TD , Sloan JA , Habermann TM . The well-being of physicians. Am J Med. 2003;114(6):513–9. doi:.https://doi.org/10.1016/S0002-9343(03)00117-7
23 Harris PA , Taylor R , Thielke R , Payne J , Gonzalez N , Conde JG . Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi:.https://doi.org/10.1016/j.jbi.2008.08.010
24 Shanafelt TD , Balch CM , Bechamps GJ , Russell T , Dyrbye L , Satele D , et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250(3):463–71. doi:.https://doi.org/10.1097/SLA.0b013e3181ac4dfd
25 Soler JK , Yaman H , Esteva M , Dobbs F , Asenova RS , Katic M , et al.; European General Practice Research Network Burnout Study Group. Burnout in European family doctors: the EGPRN study. Fam Pract. 2008;25(4):245–65. doi:.https://doi.org/10.1093/fampra/cmn038
26 Dyrbye LN , Shanafelt TD , Balch CM , Satele D , Sloan J , Freischlag J . Relationship between work-home conflicts and burnout among American surgeons: a comparison by sex. Arch Surg. 2011;146(2):211–7. doi:.https://doi.org/10.1001/archsurg.2010.310
27 Arigoni F , Bovier PA , Sappino AP . Trend of burnout among Swiss doctors. Swiss Med Wkly. 2010;140:w13070.
28 Castelo-Branco C , Figueras F , Eixarch E , Quereda F , Cancelo MJ , González S , et al. Stress symptoms and burnout in obstetric and gynaecology residents. BJOG. 2007;114(1):94–8. doi:.https://doi.org/10.1111/j.1471-0528.2006.01155.x
29 Dyrbye LN , Shanafelt TD , Balch CM , Satele D , Freischlag J . Physicians married or partnered to physicians: a comparative study in the American College of Surgeons. J Am Coll Surg. 2010;211(5):663–71. doi:.https://doi.org/10.1016/j.jamcollsurg.2010.03.032
30 Buddeberg-Fischer B , Klaghofer R , Stamm M , Siegrist J , Buddeberg C . Work stress and reduced health in young physicians: prospective evidence from Swiss residents. Int Arch Occup Environ Health. 2008;82(1):31–8. doi:.https://doi.org/10.1007/s00420-008-0303-7
31 Marchalik D , Brems J , Rodriguez A , Lynch JH , Padmore J , Stamatakis L , et al. The Impact of Institutional Factors on Physician Burnout: A National Study of Urology Trainees. Urology. 2019;131:27–35. doi:.https://doi.org/10.1016/j.urology.2019.04.042
32 Embriaco N , Azoulay E , Barrau K , Kentish N , Pochard F , Loundou A , et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med. 2007;175(7):686–92. doi:.https://doi.org/10.1164/rccm.200608-1184OC
33 Cheng WJ , Cheng Y . Night shift and rotating shift in association with sleep problems, burnout and minor mental disorder in male and female employees. Occup Environ Med. 2017;74(7):483–8. doi:.https://doi.org/10.1136/oemed-2016-103898
34 Rao SK , Kimball AB , Lehrhoff SR , Hidrue MK , Colton DG , Ferris TG , et al. The Impact of Administrative Burden on Academic Physicians: Results of a Hospital-Wide Physician Survey. Acad Med. 2017;92(2):237–43. doi:.https://doi.org/10.1097/ACM.0000000000001461
35 Tak HJ , Curlin FA , Yoon JD . Association of Intrinsic Motivating Factors and Markers of Physician Well-Being: A National Physician Survey. J Gen Intern Med. 2017;32(7):739–46. doi:.https://doi.org/10.1007/s11606-017-3997-y
36 Yoon JD , Daley BM , Curlin FA . The Association Between a Sense of Calling and Physician Well-Being: A National Study of Primary Care Physicians and Psychiatrists. Acad Psychiatry. 2017;41(2):167–73. doi:.https://doi.org/10.1007/s40596-016-0487-1
37 Pantenburg B , Luppa M , König HH , Riedel-Heller SG . Burnout among young physicians and its association with physicians’ wishes to leave: results of a survey in Saxony, Germany. J Occup Med Toxicol. 2016;11(1):2. doi:.https://doi.org/10.1186/s12995-016-0091-z
38 Msaouel P , Keramaris NC , Tasoulis A , Kolokythas D , Syrmos N , Pararas N , et al. Burnout and training satisfaction of medical residents in Greece: will the European Work Time Directive make a difference? Hum Resour Health. 2010;8(1):16. doi:.https://doi.org/10.1186/1478-4491-8-16
39 Shanafelt TD , Dyrbye LN , Sinsky C , Hasan O , Satele D , Sloan J , et al. Relationship Between Clerical Burden and Characteristics of the Electronic Environment With Physician Burnout and Professional Satisfaction. Mayo Clin Proc. 2016;91(7):836–48. doi:.https://doi.org/10.1016/j.mayocp.2016.05.007
40 Grembowski D , Ulrich CM , Paschane D , Diehr P , Katon W , Martin D , et al. Managed care and primary physician satisfaction. J Am Board Fam Pract. 2003;16(5):383–93. doi:.https://doi.org/10.3122/jabfm.16.5.383
41 Amiri M , Khosravi A , Eghtesadi AR , Sadeghi Z , Abedi G , Ranjbar M , et al. Burnout and its Influencing Factors among Primary Health Care Providers in the North East of Iran. PLoS One. 2016;11(12):e0167648. doi:.https://doi.org/10.1371/journal.pone.0167648
42 Dyrbye LN , Schwartz A , Downing SM , Szydlo DW , Sloan JA , Shanafelt TD . Efficacy of a brief screening tool to identify medical students in distress. Acad Med. 2011;86(7):907–14. doi:.https://doi.org/10.1097/ACM.0b013e31821da615
43 Dyrbye LN , Szydlo DW , Downing SM , Sloan JA , Shanafelt TD . Development and preliminary psychometric properties of a well-being index for medical students. BMC Med Educ. 2010;10(1):8. doi:.https://doi.org/10.1186/1472-6920-10-8
44 West CP , Dyrbye LN , Satele DV , Sloan JA , Shanafelt TD . Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012;27(11):1445–52. doi:.https://doi.org/10.1007/s11606-012-2015-7
45 West CP , Dyrbye LN , Sloan JA , Shanafelt TD . Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009;24(12):1318–21. doi:.https://doi.org/10.1007/s11606-009-1129-z
46 Beaton DE , Bombardier C , Guillemin F , Ferraz MB . Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25(24):3186–91. doi:.https://doi.org/10.1097/00007632-200012150-00014
47 Wada K , Arimatsu M , Higashi T , Yoshikawa T , Oda S , Taniguchi H , et al. Physician job satisfaction and working conditions in Japan. J Occup Health. 2009;51(3):261–6. doi:.https://doi.org/10.1539/joh.O8023
48Steger MF, Dik BJ, Shim Y. Assessing meaning and satisfaction at work. In: Lopez SJ, Snyder CR (eds). The Oxford Handbook of Positive Psychology Assessment. 2nd edition. Oxford: Oxford University Press. 2009.
49 Wanous JP , Reichers AE , Hudy MJ . Overall job satisfaction: how good are single-item measures? J Appl Psychol. 1997;82(2):247–52. doi:.https://doi.org/10.1037/0021-9010.82.2.247
50 Shanafelt TD , Balch CM , Dyrbye L , Bechamps G , Russell T , Satele D , et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146(1):54–62. doi:.https://doi.org/10.1001/archsurg.2010.292
51 Faller N , Stalder O , Limacher A , Bassetti S , Beer JH , Genné D , et al. Frequency of use and acceptability of clinical prediction rules for pulmonary embolism among Swiss general internal medicine residents. Thromb Res. 2017;160:9–13. doi:.https://doi.org/10.1016/j.thromres.2017.09.028
52 Schober P , Boer C , Schwarte LA . Correlation Coefficients: Appropriate Use and Interpretation. Anesth Analg. 2018;126(5):1763–8. doi:.https://doi.org/10.1213/ANE.0000000000002864
53StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP.
54 West CP , Shanafelt TD , Kolars JC . Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306(9):952–60. doi:.https://doi.org/10.1001/jama.2011.1247
55 Dyrbye LN , Burke SE , Hardeman RR , Herrin J , Wittlin NM , Yeazel M , et al. Association of Clinical Specialty With Symptoms of Burnout and Career Choice Regret Among US Resident Physicians. JAMA. 2018;320(11):1114–30. doi:.https://doi.org/10.1001/jama.2018.12615
56 Wayne DB , Arora VM . Duty hour reform and internal medicine residency training: no time to lose. J Gen Intern Med. 2009;24(10):1169–70. doi:.https://doi.org/10.1007/s11606-009-1093-7
57 Bolster L , Rourke L . The Effect of Restricting Residents’ Duty Hours on Patient Safety, Resident Well-Being, and Resident Education: An Updated Systematic Review. J Grad Med Educ. 2015;7(3):349–63. doi:.https://doi.org/10.4300/JGME-D-14-00612.1
58 Sen S , Kranzler HR , Didwania AK , Schwartz AC , Amarnath S , Kolars JC , et al. Effects of the 2011 duty hour reforms on interns and their patients: a prospective longitudinal cohort study. JAMA Intern Med. 2013;173(8):657–62, discussion 663. doi:.https://doi.org/10.1001/jamainternmed.2013.351
59 Shanafelt TD , West CP , Sloan JA , Novotny PJ , Poland GA , Menaker R , et al. Career fit and burnout among academic faculty. Arch Intern Med. 2009;169(10):990–5. doi:.https://doi.org/10.1001/archinternmed.2009.70
60 West CP , Dyrbye LN , Shanafelt TD . Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516–29. doi:.https://doi.org/10.1111/joim.12752
61 Wenger N , Méan M , Castioni J , Marques-Vidal P , Waeber G , Garnier A . Allocation of Internal Medicine Resident Time in a Swiss Hospital: A Time and Motion Study of Day and Evening Shifts. Ann Intern Med. 2017;166(8):579–86. doi:.https://doi.org/10.7326/M16-2238
62 Linzer M , Poplau S , Babbott S , Collins T , Guzman-Corrales L , Menk J , et al. Worklife and Wellness in Academic General Internal Medicine: Results from a National Survey. J Gen Intern Med. 2016;31(9):1004–10. doi:.https://doi.org/10.1007/s11606-016-3720-4
63 Sinsky CA , Dyrbye LN , West CP , Satele D , Tutty M , Shanafelt TD . Professional Satisfaction and the Career Plans of US Physicians. Mayo Clin Proc. 2017;92(11):1625–35. doi:.https://doi.org/10.1016/j.mayocp.2017.08.017
64 Gardner RL , Cooper E , Haskell J , Harris DA , Poplau S , Kroth PJ , et al. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc. 2019;26(2):106–14. doi:.https://doi.org/10.1097/SLA.0b013e3181ac4dfd
65 Linzer M , Poplau S , Grossman E , Varkey A , Yale S , Williams E , et al. A Cluster Randomized Trial of Interventions to Improve Work Conditions and Clinician Burnout in Primary Care: Results from the Healthy Work Place (HWP) Study. J Gen Intern Med. 2015;30(8):1105–11. doi:.https://doi.org/10.1007/s11606-015-3235-4
66 Olson K , Marchalik D , Farley H , Dean SM , Lawrence EC , Hamidi MS , et al. Organizational strategies to reduce physician burnout and improve professional fulfillment. Curr Probl Pediatr Adolesc Health Care. 2019;49(12):100664. doi:.https://doi.org/10.1016/j.cppeds.2019.100664
67 Desai SV , Asch DA , Bellini LM , Chaiyachati KH , Liu M , Sternberg AL , et al.; iCOMPARE Research Group. Education Outcomes in a Duty-Hour Flexibility Trial in Internal Medicine. N Engl J Med. 2018;378(16):1494–508. doi:.https://doi.org/10.1056/NEJMoa1800965
68 Bilimoria KY , Chung JW , Hedges LV , Dahlke AR , Love R , Cohen ME , et al. National Cluster-Randomized Trial of Duty-Hour Flexibility in Surgical Training. N Engl J Med. 2016;374(8):713–27. doi:.https://doi.org/10.1056/NEJMoa1515724
69 Levey RE . Sources of stress for residents and recommendations for programs to assist them. Acad Med. 2001;76(2):142–50. doi:.https://doi.org/10.1097/00001888-200102000-00010
70 Naylor RA , Reisch JS , Valentine RJ . Factors related to attrition in surgery residency based on application data. Arch Surg. 2008;143(7):647–51, discussion 651–2. doi:.https://doi.org/10.1001/archsurg.143.7.647
71 Gregory S , Demartini C . Satisfaction of doctors with their training: evidence from UK. BMC Health Serv Res. 2017;17(1):851. doi:.https://doi.org/10.1186/s12913-017-2792-0
72 Lases SS , Slootweg IA , Pierik EGJM , Heineman E , Lombarts MJMH . Efforts, rewards and professional autonomy determine residents’ experienced well-being. Adv Health Sci Educ Theory Pract. 2018;23(5):977–93. doi:.https://doi.org/10.1007/s10459-018-9843-0
73 Taylor DR , Park YS , Smith CA , Karpinski J , Coke W , Tekian A . Creating Entrustable Professional Activities to Assess Internal Medicine Residents in Training: A Mixed-Methods Approach. Ann Intern Med. 2018;168(10):724–9. doi:.https://doi.org/10.7326/M17-1680
74 ten Cate O , Chen HC , Hoff RG , Peters H , Bok H , van der Schaaf M . Curriculum development for the workplace using Entrustable Professional Activities (EPAs): AMEE Guide No. 99. Med Teach. 2015;37(11):983–1002. doi:.https://doi.org/10.3109/0142159X.2015.1060308
75 Klein J , Grosse Frie K , Blum K , von dem Knesebeck O . Burnout and perceived quality of care among German clinicians in surgery. Int J Qual Health Care. 2010;22(6):525–30. doi:.https://doi.org/10.1093/intqhc/mzq056
76 Han S , Shanafelt TD , Sinsky CA , Awad KM , Dyrbye LN , Fiscus LC , et al. Estimating the Attributable Cost of Physician Burnout in the United States. Ann Intern Med. 2019;170(11):784–90. doi:.https://doi.org/10.7326/M18-1422
77 Cribari M , Holzer BM , Battegay E , Minder CE , Zimmerli LU . What makes internal medicine attractive for the millennial generation? A survey of residents in internal medicine in Switzerland. Swiss Med Wkly. 2018;148:w14696. doi:.https://doi.org/10.4414/smw.2018.14696
This study was supported by a grant from the Swiss Society of General Internal Medicine (SGAIM) Foundation. The sponsor had no role in study design, data collection, site monitoring, data analysis, data interpretation or writing of the manuscript.
The authors declare that they have no conflicts of interest.