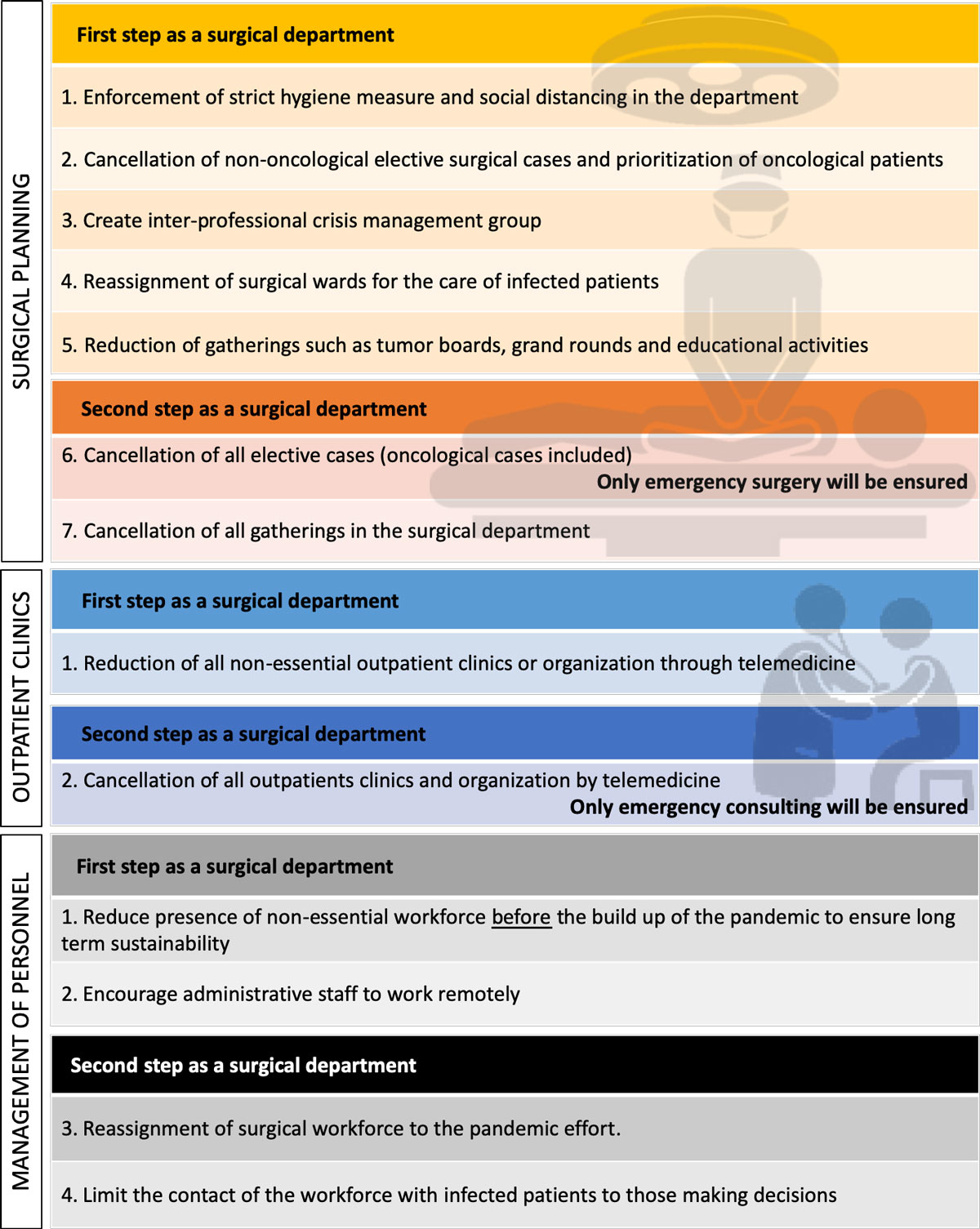
Figure 1 Blueprint for a response of a surgical department to a viral pandemic.
DOI: https://doi.org/10.4414/smw.2020.20241
With the COVID-19 pandemic, we are experiencing a crisis unprecedented in modern times. Hospitals are the cornerstones of our healthcare systems, but they are vulnerable institutions that frequently already operate at near-surge capacity under normal circumstances. Protracted outbreaks can easily overwhelm their capacity. Preparedness will require the engagement of the entire health community and healthcare assets from across the spectrum of care.
SARS-CoV-2 can cause infections ranging from a mild common cold to acute respiratory distress syndrome. Initial reports suggest that between 5 and 12% of confirmed SARS-CoV-2 infections necessitate intensive care unit (ICU) admission, including mechanical ventilation in most patients [1]. All ICU resources such as physicians, nurses and ventilators are key in the management of this epidemic.
At first sight, surgery appears to be only peripherally affected by this pandemic. However, the surgical department plays a key role in the response to this crisis. Herein, we aim to provide a blueprint for a general surgery department’s response to this current pandemic crisis and also future events of similar magnitude.
The current outbreak of the COVID-19 pandemic is unprecedented in modern times. However, the world has seen previous viral epidemics with major impacts on the functioning of hospitals and surgical departments. The Spanish flu is known as the deadliest event in human history with about one third of the world’s population affected by this acute respiratory tract infection and an estimated death toll of 50 million [2]. During September of 1918, under circumstances unimaginable today, doctors of the American Army cared for thousands of patients with influenza who poured in daily. Storerooms, officer’s messes and wards caring for non-life-threatening patients were re-allocated for the care of soldiers afflicted by the Spanish flu. Patients were isolated in special units after 48 hours spent in an observation ward. Most of the care was delivered by personnel who were not fully trained because of the acute shortage of doctors and nurses [3]. This situation is now seen in Italy, where retired physicians have been called back into clinical activity. When the pandemic eventually spread to the American continent, nonpharmaceutical interventions such as school closures, cancellation of public gatherings, quarantine and isolation helped cities to reduce the excess mortality [4]. In Toronto during 2003, severe acute respiratory syndrome (SARS) infected 196 patients and 38 of these patients required critical care. This outbreak led to a 10-day closure of 38% of ICU beds in the tertiary setting in Toronto [5]. The loss of ICU capacity led to the cancellation of surgery that would have required postoperative ICU monitoring, such as cardiovascular surgery, major abdominal surgery or transplantation. Importantly, 16 healthcare workers developed SARS, 7 requiring ICU care. This emphasises the importance of protecting those who are taking care of infected patients.
We can learn a lot from the past, and strategies such as the Pandemic Influenza Plan of the US Centers for Disease Control and Prevention (CDC) are important [6]. Nevertheless, the characteristics of every pandemic are different, and prepared plans need to be adapted. An epidemic usually leaves some time for decision makers to implement and adapt pre-established plans when the epidemic starts to unfold. However, one needs to take measures early and resolutely, and surgical departments and their resources play an important role.
We have identified three key areas of intervention as a surgical department:
We propose a plan of action that consists of two different phases (fig. 1). The first phase is to be released when the pandemic starts to build up. The second phase is to be released in the circumstance that the first measures fail to address the peak of the pandemic.
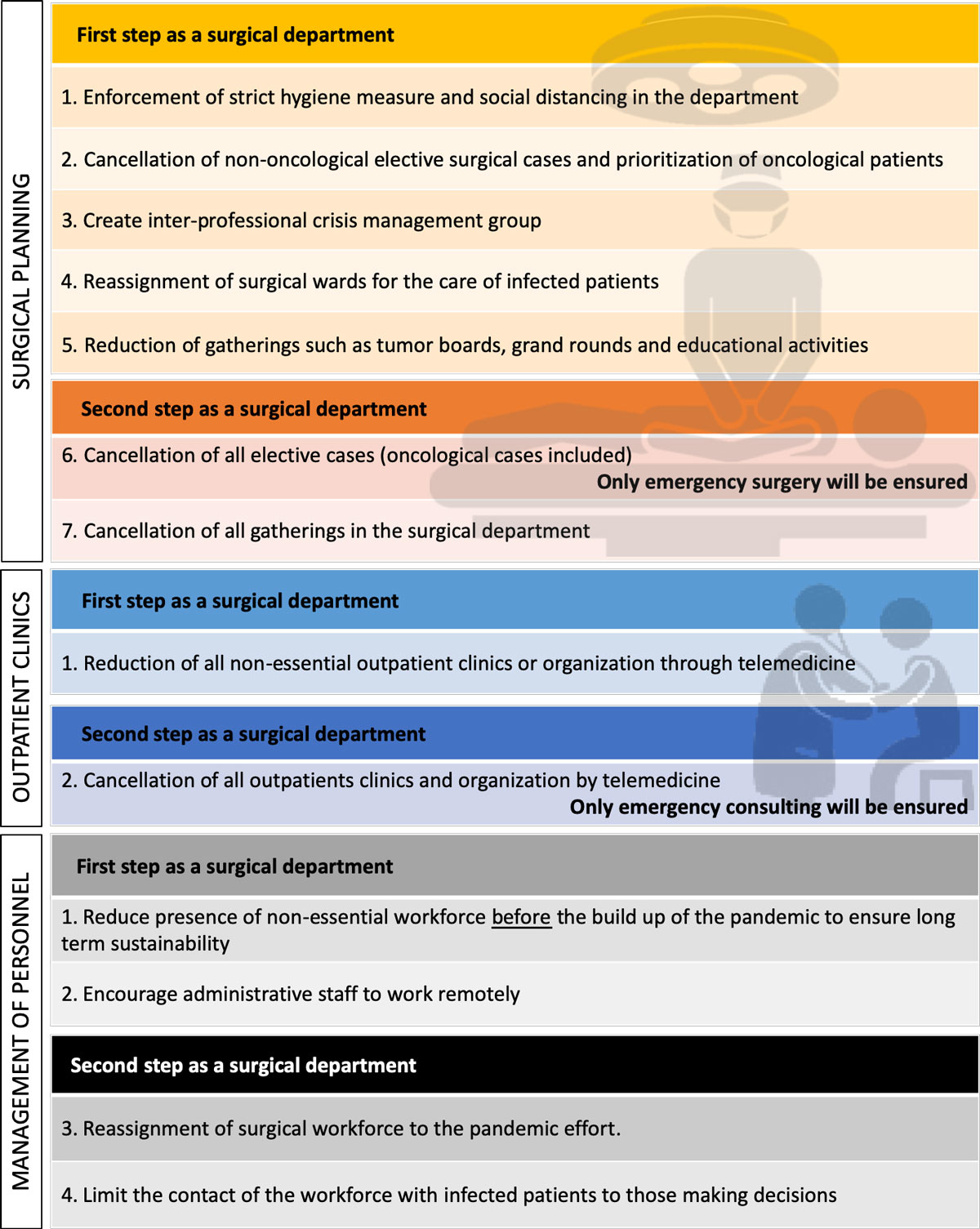
Figure 1 Blueprint for a response of a surgical department to a viral pandemic.
Crisis management groups involving decision makers from different professional groups should be created early to allow for fast transmission of critical information at the institutional level. Alternative treatment plans for surgical indications should be established as soon as the pandemic becomes a possibility. Oncological procedures should be anticipated in order to decrease their load on the system later on.
The American College of Surgeons recommends as a first step that elective surgical cases for nononcological indications should be cancelled early on [7]. Emergent surgery should be maintained and surgical cases for oncological indications prioritised before the arrival of the first COVID-positive patients in the ICU. Gatherings within the surgical department should be minimised to slow down the spread amongst healthcare workers.
In a second phase, all elective cases could be cancelled, including those with oncological indications. When possible, alternative treatments should be explored, including neoadjuvant chemotherapy or radiation therapy. Also, gatherings should be avoided altogether.
Once the epidemic has subsided, elective surgical activity should be increased slowly, and oncological indications prioritised according to a pre-established plan. During this phase, a surgical department should pay special attention to minimising exhaustion of the workforce and allowing for ample recuperation in order to avoid a crisis after the crisis.
The operating room (OR) represents a possible site of transmission and measures need to be taken to reduce this risk [8]. OR management should increase the turnaround time to allow enough time for hygiene measures and disinfection. A separate OR tract for surgery in patients suspected or confirmed to have COVID-19 should be designated. Ideally, this OR is equipped with a separate ventilation system. Furthermore, the training of OR personnel in the use of respirators, fitting of N95 masks and issue of personal goggles early in the pandemic is essential.
Outpatient clinics allow contact between patients and surgeons, providing an opportunity to discuss conditions and treatment options. However, in the case of a pandemic, patients risk becoming infected when travelling to the hospital, or even when in contact with a physician. Outpatient clinics should be reduced to a minimum early on and organised by telemedicine whenever possible. When the pandemic reaches a particular hospital in full force, these clinics should be cancelled and patients should be communicated with by phone or email.
Healthcare workers play a key role in the response to any pandemic crisis and they are on the frontline of the fight against the infection. A key goal should be to maintain long-term sustainability of the pandemic response. Unfortunately, healthcare workers have a high risk of becoming infected themselves, which can drastically reduce the ability of a department to function normally [5]. One measure is to allow physical contact with an infected patient only by the person who is capable of making decisions, in order to protect junior team members. Whenever possible, non-essential medical personnel should stay at home, to ensure enough manpower when the peak of the epidemic is reached. All non-medical personnel should be encouraged to work remotely to help with childcare during school closures and protect family members.
When the peak of the pandemic is reached, departments most affected by the pandemic may need more manpower to care for the increase in patients. A surgical department should be ready to reassign medical personnel to the care of infected patients, all while making sure enough personnel are available to maintain an emergency surgical service.
Importantly, all members of the surgical department need to have the opportunity to communicate concerns or ideas to the senior management via email, encrypted messaging or social media.
The COVID-19 outbreak calls upon all of us to directly or indirectly support our healthcare systems in order to provide the best possible care to patients and avoid its collapse. The surgical department needs to be involved early in the planning of a pandemic response, to anticipate the prioritisation of care of patients. The surgical department should gradually reduce elective surgical activity as the pandemic starts to rise, while prioritising patients needing oncological surgery. During the peak of the pandemic, resources need to be redirected to the pandemic effort, while maintaining the capacity to care for surgical emergencies even during a prolonged crisis. The management of the workforce is essential. Members not absolutely necessary for the functioning of the department should stay at home to ensure the sustainability of the effort over a prolonged pandemic. The response to this current crisis may serve as a blueprint to improve and speed up the reaction to future viral pandemic events.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Wu Z , McGoogan JM . Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020. Published online February 25, 2020. doi:.https://doi.org/10.1001/jama.2020.2648
2 Murray CJL , Lopez AD , Chin B , Feehan D , Hill KH . Estimation of potential global pandemic influenza mortality on the basis of vital registry data from the 1918-20 pandemic: a quantitative analysis. Lancet. 2006;368(9554):2211–8. doi:.https://doi.org/10.1016/S0140-6736(06)69895-4
3Reports of the surgeon general of the army 1919.
4 Markel H , Lipman HB , Navarro JA , Sloan A , Michalsen JR , Stern AM , et al. Nonpharmaceutical interventions implemented by US cities during the 1918-1919 influenza pandemic. JAMA. 2007;298(6):644–54. Published online August 09, 2007. doi:.https://doi.org/10.1001/jama.298.6.644
5 Fowler RA , Lapinsky SE , Hallett D , Detsky AS , Sibbald WJ , Slutsky AS , et al.; Toronto SARS Critical Care Group. Critically ill patients with severe acute respiratory syndrome. JAMA. 2003;290(3):367–73. Published online July 17, 2003. doi:.https://doi.org/10.1001/jama.290.3.367
6Pandemic Influenza Plan CDC. 2017 [13.03.2020]. Available from: https://www.cdc.gov/flu/pandemic-resources/pdf/pan-flu-report-2017v2.pdf.
7American College of Surgeons. COVID-19: Recommendations for Management of Elective Surgical Procedures 2020 [15 March 2020]. Available from: https://www.facs.org/about-acs/covid-19/information-for-surgeons.
8 Wong J , Goh QY , Tan Z , Lie SA , Tay YC , Ng SY , et al. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anaesth. 2020. Published online March 13, 2020. doi:.https://doi.org/10.1007/s12630-020-01620-9
Contributed equally
No financial support and no other potential conflict of interest relevant to this article was reported.