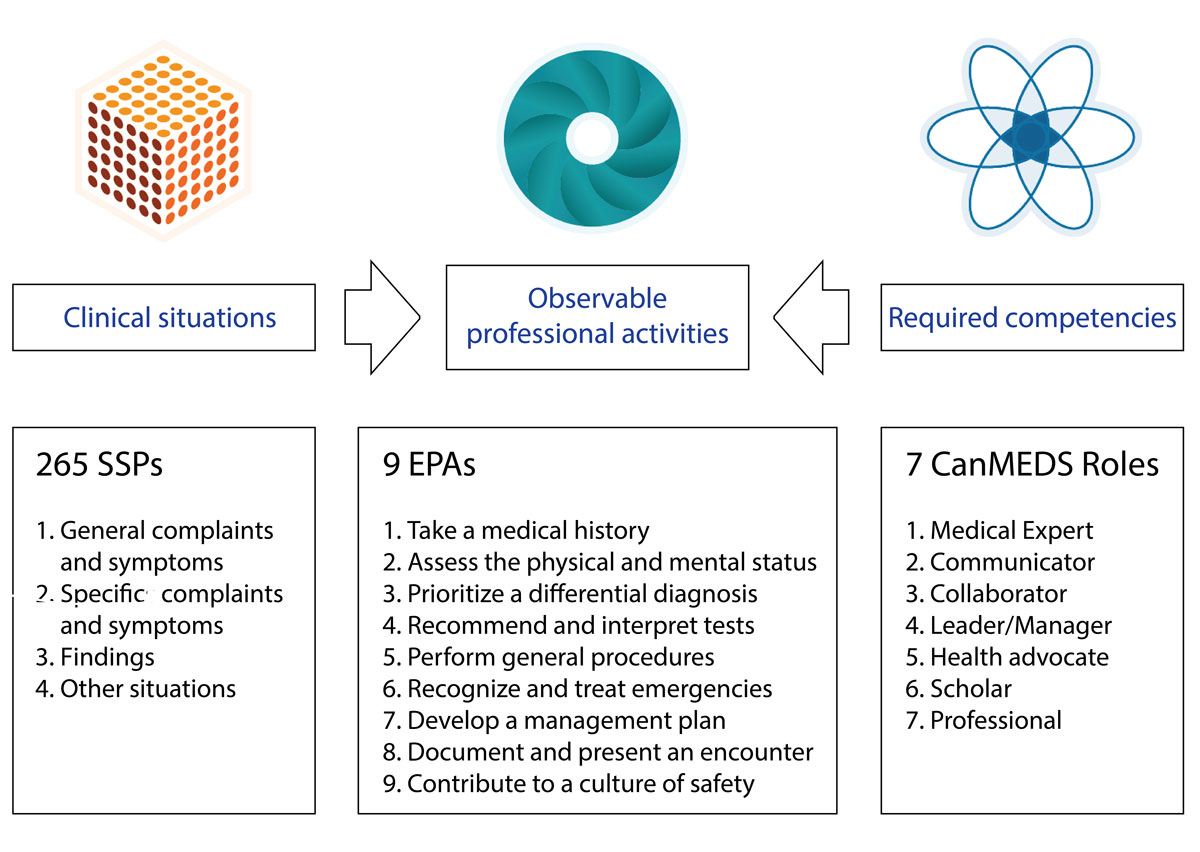
Figure 1 PROFILES is composed of three main sections: CanMEDS roles, entrustable professional activities (EPAs) and situations as starting point (SSPs).
DOI: https://doi.org/10.4414/smw.2020.20201
Over the last two decades, medical education has been progressively moving towards the model of competency-based medical education (CBME) in order to ensure that physicians are trained to meet the challenges of medicine in the 21st century [1]. Frank and colleagues defined CBME as an “approach to preparing physicians for practice that is fundamentally oriented to graduate outcome abilities and organised around competencies derived from an analysis of societal and patient needs. It de-emphasises time-based training and promises greater accountability, flexibility, and learner-centeredness” [2]. The medical curriculum should be designed by working backwards from the desired outcomes and implementing the appropriate teaching and learning activities and assessment strategies. The CanMEDS framework, describing the competencies that a physician has to be able to develop with respect to the seven roles he or she has to master to meet the healthcare needs of the population, has been widely adopted around the world, including in Switzerland [3].
Several international initiatives have been developed to promote the implementation of CBME, mainly at the level of postgraduate education. However, the transition to competencies as the underlying design principle of medical training programmes has turned out to be very challenging, in particular, because competencies are often difficult to evaluate with the currently used approaches to workplace-based assessment [4]. Recognising the need for an additional conceptual framework to connect the assessment of competencies with the reality of the medical profession and to provide operational tools for clinical supervisors to evaluate the level of competence of their trainees, ten Cate proposed the concept of entrustable professional activities (EPAs) [5]. EPAs are professional activities that a supervisor can entrust a trainee to execute autonomously once he or she has developed the relevant competencies. The introduction of EPAs is expected to promote the shift to CBME by creating a more practice-oriented model of competencies that is directly applicable to curriculum design and in particular to assessment [6].
One key factor for a successful transition towards CBME is its seamless implementation across the continuum of education, training and practice [7]. The need for a better alignment of undergraduate and postgraduate training, and therefore a progressive development of competencies, has led to the adaptation of the EPA-based approach to undergraduate medical education (UME). The main principles underlying EPAs are also applicable to UME learners, and it has been suggested that the implementation of EPAs in this context requires the development of UME-specific EPAs and an adaptation of the entrustment scale [8]. Over the last few years, an increasing number of medical schools have started to implement CBME, and in particular EPAs, within their undergraduate curricula either at the level of individual institutions or in the context of nationwide initiatives [9–11]. Several of these pilot projects have been particularly well documented, resulting in the identification of some guiding principles with respect to the introduction of EPAs into UME [12, 13].
In 2018, Switzerland introduced a completely revised version of its national outcomes reference framework for the undergraduate medical curriculum named PROFILES (Principal Relevant Objectives and Framework for Integrative Learning and Education in Switzerland) [14]. In accordance with the evolution in the field of medical education described above, this new framework elaborated by the Joint Commission of the Swiss medical schools (SMIFK/CIMS) is based on the pragmatic approach of using EPAs to facilitate the shift towards CBME. PROFILES defines the endpoint of the undergraduate curriculum by describing what a resident needs to know and needs to be able to do on his/her first day of residency. This approach lays the groundwork for students to be able to make an efficient transition from undergraduate to postgraduate medical training. Anchored in the Federal Act on the University Medical Professions (MedBG/LPMéd), PROFILES represents a binding document for all Swiss undergraduate medical schools and determines the content of the Federal Licencing Examination.
PROFILES is composed of three main sections: a set of competencies made up of the relevant knowledge, skills and attitudes and adapted from the CanMEDS framework; nine entrustable professional activities (EPAs) that the students have to master at least to the level of distant, on-demand supervision; and 265 generic clinical situations (situations as starting point, or SSPs) which cover the common symptoms, complaints and findings that a resident should be able to manage with respect to all age groups and in any type of setting (fig. 1). Switzerland is one of the first countries to introduce a legally binding national framework that uses EPAs as a cornerstone for determining the undergraduate medical education curricula, representing a profound change in the way medical training has to be organised at each medical school. Given that the introduction of CBME and EPAs is a complex process that has implications at many levels, ranging from nationwide issues to local considerations, the Swiss medical schools have decided to adopt a collaborative approach. In this paper we describe the process put in place at a national level to frame the necessary conditions for the implementation of the PROFILES framework. Sharing this approach should be of interest to the international community of medical educators and medical schools involved in similar large-scale processes, as well as teachers, students and other stakeholders involved in medical education in Switzerland.
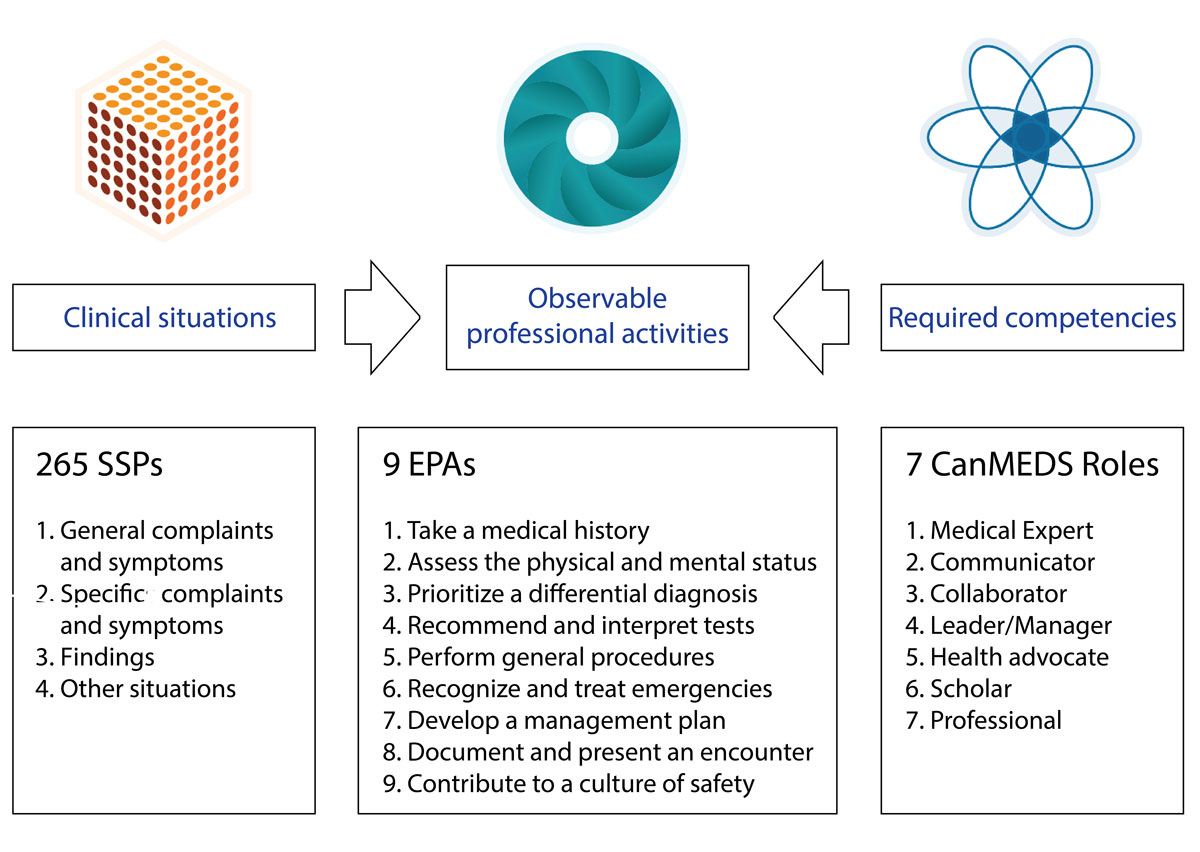
Figure 1 PROFILES is composed of three main sections: CanMEDS roles, entrustable professional activities (EPAs) and situations as starting point (SSPs).
The necessity of setting up a collaborative, nationwide approach to the implementation of PROFILES results from a number of different political and educational reasons. Switzerland is a confederation and many aspects, including education, are governed at the state (canton) level. Cantons have the authority and full autonomy to run their universities. Even with a national licensing examination and a national reference framework, all Swiss medical schools have developed their medical curricula independently. A collaborative approach is, therefore, the preferred way to develop synergies at the national level and to share the multiple implementation experiences. The recent literature emphasises the importance of developing a shared understanding of the concepts underlying CBME and EPAs and their implications for teaching and learning [15].
Medical schools are positioned within a complex system that places great importance on governance [16]. Their undergraduate curricula are not only situated within a University but also within a health care system [17]. This is particularly true for CBME-based programmes that focus on meeting the health need priorities of the local population and involve many stakeholders such as governmental ministries, self-regulated professional organisations, accreditation bodies, hospitals and other health systems, as well as the public. In addition to involving many different stakeholders, a shift to CBME is a complex intervention impacting not only on pedagogical issues but also depending on many other aspects of the local context [6]. This includes, for example, the local history and culture of medical teaching and learning, the current curriculum, the number of students who are trained, and the relationship between the medical school and the teaching hospital(s).
In order to implement the changes necessary to adapt its curriculum to a new reference framework, a medical school has to consider several “generic” elements in addition to the local context and the existing curriculum [18]. This includes knowledge on effective processes of curriculum design and the current thinking about the nature of professional practice, and, importantly, also perspectives and new ideas from the national arena as well as the international community. Considering the significant challenges associated with the transition to PROFILES, the vice-deans of education of the faculties of medicine decided to establish a Swiss Working Group for PROFILES Implementation (SWGPI), composed of delegates of the medical faculties and the Federal Licensing Examination, with the following mandate:
As a first step, the SWGPI developed a PROFILES implementation guide, which aims to inspire and support the Swiss medical schools to rethink seminal aspects of their curricula by presenting guiding principles and best practices [19]. The non-binding approach of a guide rather than a rule-book was necessary to provide a shared conceptual framework while at the same time respecting the autonomy of each medical school by allowing them to adapt the implementation process to their specific context and challenges. The implementation guide was written mainly with two readerships in mind: the leaders and the members of the local medical school groups in charge of implementing PROFILES, and the teams of professional educators supporting this process. It will also be useful to any person involved or interested in the process, including teachers, students and administrative staff, to give them an overview of the future developments of teaching and learning at Swiss medical schools.
The SWGPI adopted a stepwise approach for the elaboration of the guide. A thorough review of the scientific literature allowed the identification of key factors that have to be considered while implementing a competency- and EPA-based curriculum. We extended the literature-based analysis by contacting leaders publishing in the field and attending workshops at international meetings dedicated to CBME. An analysis of our national particularities complemented our approach. A draft version of the guide was distributed to the different stakeholders and the revised version was subsequently validated by the group of vice-deans of education and the SMIFK/CIMS. The SWGPI then organised a national meeting to present and discuss the guide with further representatives of the Swiss medical schools, students and representatives from postgraduate education.
The SWGPI identified a number of key factors that are important to successfully implement a competency- and EPA-based undergraduate curriculum. These factors include the design and governance of the curriculum, the assessment system and the entrustment process, the teacher training programme (faculty development), and the systematic mapping of the curriculum as well as the students’ learning experiences during their clinical immersion using an e-portfolio. The transition towards CBME requires a strong leadership for change, and should be accompanied by an appropriate evaluation of the implementation process.
The organisation of the curricular elements underlying CBME is guided by the competencies needed for optimal patient care. The performance of an EPA at the required level of autonomy requires the mastery of a combination of several competencies within the context of a clinical situation. Although competencies may be trained independently during the curriculum, students have to be able to integrate them for the management of a clinical task.
To allow students to learn in a way that is coherent with the way they will use their competencies in clinical practice, they have to be exposed to an integrated curriculum. The concept of integration is inconsistently used in medical education and has at least two broad dimensions [20]. Horizontal integration refers to the teaching of different disciplines in the same module or around the same theme, rather than in parallel or sequential modules. The use of clinical situations (SSPs) as a guiding principle for curriculum design strongly encourages horizontal integration. Vertical integration is a longitudinal concept that applies to the curriculum as a whole, combining fundamental sciences with clinical sciences, an early and longitudinal immersion of the students within an authentic clinical environment and a progressive increase of clinical responsibility. A vertically integrated curriculum promotes the efficient integration of knowledge, skills and attitudes that the students need to learn to master the different EPAs, and facilitates professional identity formation (“to think, act, and feel like a physician”) [21].
All medical schools have to verify and if necessary adapt and/or redesign the specific learning goals of each learning activity to make sure that they are aligned with PROFILES. The changes required to adapt a medical undergraduate curriculum can occur at two different, not mutually exclusive, levels [22]. Pedagogical reforms largely preserve existing curricular content and focus on adapting the curricular organisation and changing the teaching methods towards more active learning principles. By contrast, content reforms aim to change significant portions of the existing curriculum to make room for more relevant material. The implementation of a competency-based framework such as PROFILES requires increasingly learner-centred pedagogical approaches as well as significant changes at the level of the content that is taught, and the perspective into which this content is integrated.
An efficient curricular governance structure is needed to decide on all curricular elements such as content, teaching methods and assessment strategies, and to ensure appropriate coordination. This is particularly important to avoid the risk of progressive curricular bloating by the continuous addition of content in the absence of proportional deletions [16].
It is well known that the assessment culture influences how and what students learn [23]. The achievement of the defined learning goals will depend to a large extent on the assessment approaches put in place, rather than just the content and organisation of the curriculum.
An appropriate blend of different assessment methods is required to capture the full spectrum of the knowledge, skills and attitudes developed by the students. The choice of assessment methods must consider all the three components of PROFILES: CanMEDS competencies, EPAs and SSPs. Consequently, in order to make sure that all components of PROFILES are sufficiently covered, a thoroughly designed assessment plan encompassing the entire programme has to be developed and aligned with the curriculum. The concept of programmatic assessment has the potential to optimise both assessment for learning and assessment for decision making about learner progress [24]. According to this approach, the individual assessments made over a defined period mainly serve to provide information on the learner’s performance. Such low-stake formative assessments are not primarily used to make pass/fail decisions, but to help the students to identify their strengths and weaknesses and to adapt their learning process accordingly. High-stake summative decisions such as promotion to the next year are then taken at the programme level by collecting many assessments from a variety of different methods, such as standardised knowledge and skills tests as well as assessment data from the authentic clinical workplace including EPAs, and meaningfully aggregating them across competencies. The implementation of a competency-based curriculum will only be successful if it is aligned to such a multi-dimensional assessment concept. Personal learning tools such as e-portfolios are increasingly used to collect the different formative assessments and to document as well as evaluate the students’ learning progress [25].
The entrustment of professional activities is a complex process integrating multiple data sources. One of the key elements to evaluating the autonomy level of a trainee for entrustment is direct observation during clinical activities, reinforcing the need for students to be immersed in an authentic clinical environment.
Rather than being an observed level of competence, an entrustment decision corresponds to a judgement (or risk-assessment) with respect to a student’s future capability and performance. Or in other words: how far can we trust a student to take care of a patient on his or her own. Accordingly, an entrustment decision cannot be made based on a single data point or observation; it rather requires a process of repeated and diverse longitudinal observations to capture the progressive development of entrustment along with the different levels of autonomy [8]. To operationalise this entrustment decision process, a two-stage approach is proposed based on the programmatic assessment approach [26]:
Such a two-step approach creates the necessary separation of the teaching role of the clinical supervisors from the summative entrustment decision made by the medical school. Despite this separation of roles, one of the major challenges with respect to the entrustment process results from the difficulty of clinical supervisors to consistently endorse their expected teaching role. If clinical supervisors feel unprepared and/or unwilling to document and report unsatisfactory trainee performance it will eventually lead to a “failure to fail” [27]. In order to counteract this phenomenon, medical schools will be required to establish an assessment system and create a culture that enables clinical supervisors to document the performance of learners correctly and honestly, and provide remediation opportunities for students who experience failure [28].
Although many aspects are important for the successful implementation of PROFILES, the evolution of the assessment system, which includes the entrustment process, towards a programmatic assessment approach is probably the most essential one. The necessary adaptations will require significant effort from the medical schools, but also appropriate measures in the clinical environment (hospital and ambulatory) to protect sufficient time for teaching, supervision and formative assessment.
Faculty development, or “teaching the teachers”, is considered to be one of the prerequisites for the successful introduction of CBME [29]. The implementation of PROFILES, therefore, requires the deployment of a well-structured, longitudinal faculty development programme that takes into account all institutional stakeholders, and provides opportunities for cumulative learning, practice and feedback from peers. Given the multiple roles attributed to the teachers and clinicians, efficient training will need the programmes to be specifically tailored to the different target publics.
The pedagogical core competencies every medical teacher should possess will not be sufficient to support the comprehensive implementation of a PROFILES-based curriculum: faculty should also be able to situate their teaching activity within a global vision of the curriculum, have a solid understanding of the concepts underlying PROFILES and embrace their role as evaluators in the new context built around the notion of entrustment. Several authors have recently proposed to use EPAs to train teachers in medical education (for example Walsh and colleagues [30]). The development of such fundamental teaching activities would guide the structure and content of faculty development workshops, while allowing the teachers at the same time to experience themselves the concept of EPAs.
The introduction of PROFILES should not only focus on curriculum design and faculty development, but also on the quality of the overall learning and teaching culture. This includes rewarding the excellence of teachers in promotion procedures, in particular the ones being actively involved in the governance of the curriculum, and providing institutional incentives for clinicians to engage in the supervision of students [31].
In order to ensure that a particular curriculum exposes the students to all relevant learning experiences, both the structured teaching activities designed by the medical school (planned curriculum) and the clinical situations to which an individual student is exposed during his or her clinical placements (experienced curriculum) have to be mapped to PROFILES. The establishment of a curriculum mapping system and the integration of an e-portfolio are therefore important processes to support the implementation of a CBME curriculum, and would benefit from a shared approach ideally based on common informatics tools (fig. 2).
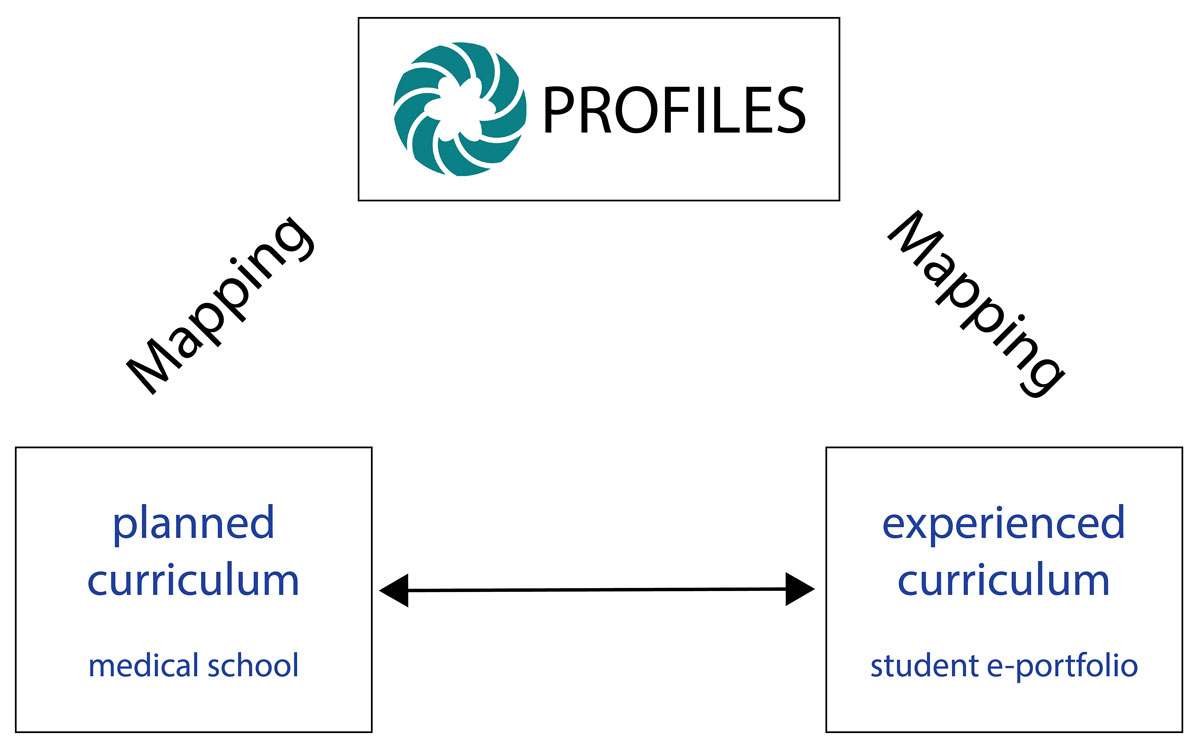
Figure 2 Alignment of curricular mapping and the student e-portfolio to the PROFILES competency framework.
Each medical school has to be able to ensure that the planned curriculum covers all the elements of PROFILES and successfully aligns teaching and assessment over the whole 6-year programme. Teachers have to be able to situate their teaching activities within the curriculum as a whole, and students have to be able to connect a particular class to the other theoretical and practical courses of the programme. The transition towards PROFILES must, therefore, be supported by a systematic approach of curriculum mapping, linking curricular content and learning activities to the learning goals derived from PROFILES. Such a mapping will provide the transparency necessary for students, teachers and the medical school to know what is taught and/or should be learned by when and how.
Given the large amount of data making up a medical curriculum, the centralisation of all the relevant information in an informatics platform will be an essential prerequisite for an efficient mapping process within each medical school. Once in place, the mapping tool will also greatly facilitate the governance of the curriculum, for example by allowing the dynamic visualisation of specific elements based on keyword searches. The collaborative development of a curriculum mapping approach also has the potential to facilitate the exchange of information between the different medical schools in Switzerland, allowing them to learn from each other’s strengths and weaknesses [32]. This exchange would be supported by a shared approach with respect to the dimensions used to map the curriculum.
The successful implementation of a competency-based curriculum combined with multidimensional assessments (mainly in the context of clinical immersion) requires that students become active players in their learning: although the medical school can plan a curriculum that is aligned with PROFILES, only the students themselves can ensure that the experienced curriculum exposes them to all the relevant clinical situations. The longitudinal integration of a learning e-portfolio, supported by a mentoring programme, is thought to be necessary for students to be able to monitor and guide their individual learning progress towards the expectations of PROFILES. In contrast to logbooks, which simply document that a learning activity has taken place, e-portfolios are designed as flexible, learner-centred systems. They help the students to collect evidence of the development of competence over time by aggregating all the different types of formative assessments, to reflect on their learning process, to plan learning goals and to interact with their teachers [33]. As is the case with curriculum mapping, the medical schools should endeavour to elaborate a common framework underlying the documentation of student learning with respect to the different components of PROFILES.
The introduction of any significant curricular change requires a clearly defined governance structure and a strong institutional leadership including champions embracing the planned change [16]. The implementation, but also the subsequent phase of maintenance, should be led and coordinated by a group involving different stakeholders including students. It will be essential to get all stakeholders on board and actively involve the key members of the faculty in all the phases of curriculum design and maintenance, such as the representatives of the disciplines and members of the different teaching and assessment committees. The use of known approaches to change management would facilitate the transition to PROFILES [34].
The teachers directly involved in the organisation of the curriculum, the students and all the teachers/clinical supervisors have to be informed about the changes resulting from the introduction of PROFILES. An efficient communication process will be key to coordinate the complex information flow within the individual medical schools. For example, faculty members teaching basic sciences might fear that this new competency-oriented framework will reduce the importance of these disciplines. They must be reassured that basic sciences remain an essential, explicit foundation of a PROFILES-based medical curriculum, and that students have to be able to integrate basic and clinical sciences during their entire learning process.
The nationwide implementation of a new competency framework will lead to significant changes within the curricula of the different medical schools, and also have an impact on the institutional teaching and learning culture. In order to monitor and further improve the quality of the resulting training programmes it will be important to implement efficient quality assurance procedures early in the process. While student evaluation of teaching is already frequently used, additional outcomes from other stakeholders must be considered, such as teachers, other health care providers and patients.
A recent paper from van Melle and colleagues [35] proposes a framework for the study and the evaluation of the implementation of a CBME-based curriculum, based on five core components that have to be “constructively aligned”: outcome competencies, sequenced progression, tailored learning experiences, competency focused instruction, and programmatic assessment. Such an approach to programme evaluation based on guiding principles, rather than a predefined list of specific evaluation criteria, provides the flexibility required to reach a deeper understanding of CBME programmes and of the conditions under which they work most effectively, while leaving at the same time enough flexibility to account for the local context. The coordinated use of a common framework to evaluate the implementation of PROFILES within the different medical schools in Switzerland, combined with the curriculum mapping process, would be an excellent basis to learn from each other and to be able to compare the different curricula. The systematic use of an internationally established evaluation framework would also provide a sound basis for future research on the implementation and impact of PROFILES in Switzerland.
The changes resulting from the introduction of a new competency framework have to be reflected at the level of the national licensing exam. In this respect the Federal Licencing Examination (FLE) plays a key role to guarantee an adequate quality and comparability of medical education across Switzerland. In its current format, the centrally managed and locally administered FLE is composed of an applied clinical knowledge exam composed of multiple-choice questions based on clinical vignettes and a practical clinical skills exam in the format of an objective structured clinical examination (OSCE) [36].
With EPAs being the main innovative element of PROFILES, the FLE and its clinical skills component is well positioned. Professional activities listed in the EPA chapter such as take a medical history, assess the physical and mental status of the patient and perform general procedures are akin to the tasks already assigned to candidates in the OSCE part of the FLE. Other activities that are emphasised in PROFILES, such as case presentation, emergency management and communication in challenging situations, will have to be adequately strengthened. Moreover, the notion of entrustment should be integrated into the evaluation of the candidates while performing the respective tasks in the setting of the exam. The increased focus of PROFILES on clinical reasoning will also require the applied clinical knowledge part of the exam to be complemented with other test formats to better capture this dimension, such as key-feature and long-menu questions [37, 38].
The assessment of all facets of medical competence and the entrustment process are the primary task of the medical schools and represent the first step of certification by providing a Master degree that enables the students to take the FLE. The role of the FLE is to check, on the basis of a representative sample of applied knowledge and professional tasks, whether the individual candidate possesses the necessary knowledge, skills and attitudes. The assessment system of the medical schools and the FLE complement each other: the strength of the longitudinal assessment during the medical school is the incorporation of evaluation data from the authentic clinical setting, whereas the strength of a standardised FLE is the quality of test material developed by medical content and assessment methodology experts in an iterative process.
There is an important pre-assessment effect of licensing examinations that is going beyond the individual student but influences medical schools at large [39, 40]. It is therefore not surprising that an increasing number of countries are considering the introduction of national licensing examinations including a clinical skills part [41]. Based on years of experience with licensing examinations in the USA and Canada, Melnick summarises their value as follows: “equity of common standards, external audit providing transparency and accountability, providing a bounded environment for innovation, providing data for evidence-based education and regulation, encouraging evidence-based workforce mobility and fostering high quality assessment” [42].
The nationwide, collaborative approach to define strategies and conditions for the implementation of a new national outcomes reference framework for the undergraduate medical curriculum has allowed the SWGPI to develop a shared conceptual understanding of the implications of PROFILES, summarised in the form of a guide. This guide is currently being used in the different medical schools to support the local implementation efforts. The integration of members of the FLE working groups has established a regular exchange between the ongoing work within the medical schools and the national process piloting the FLE, thereby ensuring that the future developments at these two different levels will be coordinated.
The common approach has already generated important synergies, for example at the level of curriculum mapping and the use of e-portfolios. Several medical schools have adopted the same mapping tool, and a Swiss mapping community is starting to develop. This process will lead to a clearer appreciation of the challenges ahead and strengthen the movement towards using common processes to document, visualise and exchange information relative to the current and future undergraduate medical curricula.
The first national meeting organised by the SWGPI around the distribution of the PROFILES guide has allowed to identify several areas that will require particular attention, such as the assessment of CanMEDS competencies and EPAs during the clinical elective year and the establishment of a shared approach towards faculty development. The SWGPI has the mandate to continue its work, promoting the relevant initiatives together with the larger Swiss medical education community.
The implementation of a competency-based medical curriculum is a complex process that requires careful thought, efficient governance and a step-wise approach. Some of the key aspects to be considered have been described above. Taking a long-term view, it is worth pointing out that CBME might reach its full potential when elements of time-independent education are integrated into a curriculum [43]. In such a scenario, the duration of the training of a particular student is variable and depends on how fast he or she develops the necessary competences and is considered “entrustable” for the relevant clinical activities. Such a training programe requires significant curricular flexibility able to manage the differences in the development of individual learners, and an adequate balance between longitudinal placements and exposure to a sufficient set of different clinical learning environments.
The efforts required by the Swiss medical schools to implement PROFILES can only be sustained if the accreditation body embraces the concepts put forward by this new framework. It is therefore important that the standards used in the accreditation process be adapted in the future to make sure that they are fully aligned with the new dimensions introduced by PROFILES and its underlying CBME framework.
The authors would like to thank the members of the Swiss Working Group for PROFILES Implementation for the stimulating collaboration and their insightful comments on this manuscript. Pierre-André Michaud provided valuable advice during the writing process. We are particularly grateful to the vice-deans of education for their continuing support and their commitment to a collaborative approach towards the implementation of PROFILES in Switzerland.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Carraccio CL , Englander R . From Flexner to competencies: reflections on a decade and the journey ahead. Acad Med. 2013;88(8):1067–73. doi:.https://doi.org/10.1097/ACM.0b013e318299396f
2 Frank JR , Mungroo R , Ahmad Y , Wang M , De Rossi S , Horsley T . Toward a definition of competency-based education in medicine: a systematic review of published definitions. Med Teach. 2010;32(8):631–7. doi:.https://doi.org/10.3109/0142159X.2010.500898
3Royal College of Physicians and Surgeons of Canada [Internet]. CanMEDS Framework. [Cited 2019 June 30.] Available from: http://www.royalcollege.ca/rcsite/canmeds/canmeds-framework-e
4 Holmboe ES , Batalden P . Achieving the Desired Transformation: Thoughts on Next Steps for Outcomes-Based Medical Education. Acad Med. 2015;90(9):1215–23. doi:.https://doi.org/10.1097/ACM.0000000000000779
5 ten Cate O . Entrustability of professional activities and competency-based training. Med Educ. 2005;39(12):1176–7. doi:.https://doi.org/10.1111/j.1365-2929.2005.02341.x
6 Holmboe ES . Competency-Based Medical Education and the Ghost of Kuhn: Reflections on the Messy and Meaningful Work of Transformation. Acad Med. 2018;93(3):350–3. doi:.https://doi.org/10.1097/ACM.0000000000001866
7 Carraccio C , Englander R , Van Melle E , Ten Cate O , Lockyer J , Chan MK , et al.; International Competency-Based Medical Education Collaborators. Advancing Competency-Based Medical Education: A Charter for Clinician-Educators. Acad Med. 2016;91(5):645–9. doi:.https://doi.org/10.1097/ACM.0000000000001048
8 Chen HC , van den Broek WE , ten Cate O . The case for use of entrustable professional activities in undergraduate medical education. Acad Med. 2015;90(4):431–6. doi:.https://doi.org/10.1097/ACM.0000000000000586
9 ten Cate O , Graafmans L , Posthumus I , Welink L , van Dijk M . The EPA-based Utrecht undergraduate clinical curriculum: Development and implementation. Med Teach. 2018;40(5):506–13. doi:.https://doi.org/10.1080/0142159X.2018.1435856
10 Englander R , Flynn T , Call S , Carraccio C , Cleary L , Fulton TB , et al. Toward Defining the Foundation of the MD Degree: Core Entrustable Professional Activities for Entering Residency. Acad Med. 2016;91(10):1352–8. doi:.https://doi.org/10.1097/ACM.0000000000001204
11 https://afmc.ca/medical-education/entrustable-professional-activities-epas; accessed on 30.06.2019
12 Lomis K , Amiel JM , Ryan MS , Esposito K , Green M , Stagnaro-Green A , et al.; AAMC Core EPAs for Entering Residency Pilot Team. Implementing an Entrustable Professional Activities Framework in Undergraduate Medical Education: Early Lessons From the AAMC Core Entrustable Professional Activities for Entering Residency Pilot. Acad Med. 2017;92(6):765–70. doi:.https://doi.org/10.1097/ACM.0000000000001543
13 Murray KE , Lane JL , Carraccio C , Glasgow T , Long M , West DC , et al.; Education in Pediatrics Across the Continuum (EPAC) Study Group. Crossing the Gap: Using Competency-Based Assessment to Determine Whether Learners Are Ready for the Undergraduate-to-Graduate Transition. Acad Med. 2019;94(3):338–45. doi:.https://doi.org/10.1097/ACM.0000000000002535
14 Michaud PA , Jucker-Kupper P , The P ; The Profiles Working Group. The “Profiles” document: a modern revision of the objectives of undergraduate medical studies in Switzerland. Swiss Med Wkly. 2016;146:w14270. doi:.https://doi.org/10.4414/smw.2016.14270
15 Meyer EG , Chen HC , Uijtdehaage S , Durning SJ , Maggio LA . Scoping Review of Entrustable Professional Activities in Undergraduate Medical Education. Acad Med. 2019;94(7):1040–9. doi:.https://doi.org/10.1097/ACM.0000000000002735
16 Casiro O , Regehr G . Enacting Pedagogy in Curricula: On the Vital Role of Governance in Medical Education. Acad Med. 2018;93(2):179–84. doi:.https://doi.org/10.1097/ACM.0000000000001774
17 Frenk J , Chen L , Bhutta ZA , Cohen J , Crisp N , Evans T , et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–58. doi:.https://doi.org/10.1016/S0140-6736(10)61854-5
18 Bordage G , Harris I . Making a difference in curriculum reform and decision-making processes. Med Educ. 2011;45(1):87–94. doi:.https://doi.org/10.1111/j.1365-2923.2010.03727.x
19Swiss Working Group for PROFILES Implementation. An implementation guide for the Swiss medical schools. 2019 [cited 2019 November 28]. Available from: https://www.profilesmed.ch/sections/ressources
20 Hays R . Integration in medical education: what do we mean? Educ Prim Care. 2013;24(3):151–2. doi:.https://doi.org/10.1080/14739879.2013.11494358
21Merton RK. Some preliminaries to a sociology of medical education. In: Merton RK, Reader LG, Kendall PL, editors. The Student Physician: Introductory Studies in the Sociology of Medical Education. Cambridge, Mass: Harvard University Press; 1957: p. 3–79.
22 Stevens CD . Repeal and Replace? A Note of Caution for Medical School Curriculum Reformers. Acad Med. 2018;93(10):1425–7. doi:.https://doi.org/10.1097/ACM.0000000000002219
23 Harrison CJ , Könings KD , Dannefer EF , Schuwirth LW , Wass V , van der Vleuten CP . Factors influencing students’ receptivity to formative feedback emerging from different assessment cultures. Perspect Med Educ. 2016;5(5):276–84. doi:.https://doi.org/10.1007/s40037-016-0297-x
24 van der Vleuten CP , Schuwirth LW , Driessen EW , Dijkstra J , Tigelaar D , Baartman LK , et al. A model for programmatic assessment fit for purpose. Med Teach. 2012;34(3):205–14. doi:.https://doi.org/10.3109/0142159X.2012.652239
25Frank JR, Mann K, Keely M. Portfolios and logbooks. In: Bandiera G, Sherbino J, Frank JR, editors. The CanMEDS assessment tools handbook. An introductory guide to assessment methods for the CanMEDS competencies. Ottawa: The Royal College of Physicians and Surgeons of Canada; 2006: p. 32–5.
26 Van Der Vleuten CPM , Schuwirth LWT , Driessen EW , Govaerts MJB , Heeneman S . Twelve Tips for programmatic assessment. Med Teach. 2015;37(7):641–6. doi:.https://doi.org/10.3109/0142159X.2014.973388
27 Mak-van der Vossen M . ‘Failure to fail’: the teacher’s dilemma revisited. Med Educ. 2019;53(2):108–10.
28 Yepes-Rios M , Dudek N , Duboyce R , Curtis J , Allard RJ , Varpio L . The failure to fail underperforming trainees in health professions education: A BEME systematic review: BEME Guide No. 42. Med Teach. 2016;38(11):1092–9. doi:.https://doi.org/10.1080/0142159X.2016.1215414
29 Dath D , Iobst W . The importance of faculty development in the transition to competency-based medical education. Med Teach. 2010;32(8):683–6. doi:.https://doi.org/10.3109/0142159X.2010.500710
30 Walsh A , Koppula S , Antao V , Bethune C , Cameron S , Cavett T , et al. Preparing teachers for competency-based medical education: Fundamental teaching activities. Med Teach. 2018;40(1):80–5. doi:.https://doi.org/10.1080/0142159X.2017.1394998
31 Irby DM , O’Sullivan PS . Developing and rewarding teachers as educators and scholars: remarkable progress and daunting challenges. Med Educ. 2018;52(1):58–67. doi:.https://doi.org/10.1111/medu.13379
32 Fritze O , Lammerding-Koeppel M , Boeker M , Narciss E , Wosnik A , Zipfel S , et al. Boosting competence-orientation in undergraduate medical education - A web-based tool linking curricular mapping and visual analytics. Med Teach. 2019;41(4):422–32. doi:.https://doi.org/10.1080/0142159X.2018.1487047
33 Driessen E . Do portfolios have a future? Adv Health Sci Educ Theory Pract. 2017;22(1):221–8. doi:.https://doi.org/10.1007/s10459-016-9679-4
34 Sklar DP . Implementing Curriculum Change: Choosing Strategies, Overcoming Resistance, and Embracing Values. Acad Med. 2018;93(10):1417–9. doi:.https://doi.org/10.1097/ACM.0000000000002350
35 Van Melle E , Frank JR , Holmboe ES , Dagnone D , Stockley D , Sherbino J ; International Competency-based Medical Education Collaborators. A Core Components Framework for Evaluating Implementation of Competency-Based Medical Education Programs. Acad Med. 2019;94(7):1002–9. doi:.https://doi.org/10.1097/ACM.0000000000002743
36 Guttormsen S , Beyeler C , Bonvin R , Feller S , Schirlo C , Schnabel K , et al. The new licencing examination for human medicine: from concept to implementation. Swiss Med Wkly. 2013;143:w13897. doi:.https://doi.org/10.4414/smw.2013.13897
37 Hrynchak P , Glover Takahashi S , Nayer M . Key-feature questions for assessment of clinical reasoning: a literature review. Med Educ. 2014;48(9):870–83. doi:.https://doi.org/10.1111/medu.12509
38 Huwendiek S , Reichert F , Duncker C , de Leng BA , van der Vleuten CPM , Muijtjens AMM , et al. Electronic assessment of clinical reasoning in clerkships: A mixed-methods comparison of long-menu key-feature problems with context-rich single best answer questions. Med Teach. 2017;39(5):476–85. doi:.https://doi.org/10.1080/0142159X.2017.1297525
39 Gilliland WR , La Rochelle J , Hawkins R , Dillon GF , Mechaber AJ , Dyrbye L , et al. Changes in clinical skills education resulting from the introduction of the USMLE step 2 clinical skills (CS) examination. Med Teach. 2008;30(3):325–7. doi:.https://doi.org/10.1080/01421590801953026
40 Hauer KE , Teherani A , Kerr KM , O’Sullivan PS , Irby DM . Impact of the United States Medical Licensing Examination Step 2 Clinical Skills exam on medical school clinical skills assessment. Acad Med. 2006;81(10, Suppl):S13–6. doi:.https://doi.org/10.1097/01.ACM.0000236531.32318.02
41 Swanson DB , Roberts TE . Trends in national licensing examinations in medicine. Med Educ. 2016;50(1):101–14. doi:.https://doi.org/10.1111/medu.12810
42 Melnick DE . Licensing examinations in North America: is external audit valuable? Med Teach. 2009;31(3):212–4. doi:.https://doi.org/10.1080/01421590902741163
43 Teunissen PW , Kogan JR , Ten Cate O , Gruppen LD , Lingard LA . Learning in Practice: A Valuation of Context in Time-Variable Medical Training. Acad Med. 2018;93(3S):S22–6. doi:.https://doi.org/10.1097/ACM.0000000000002070
No financial support and no other potential conflict of interest relevant to this article was reported.