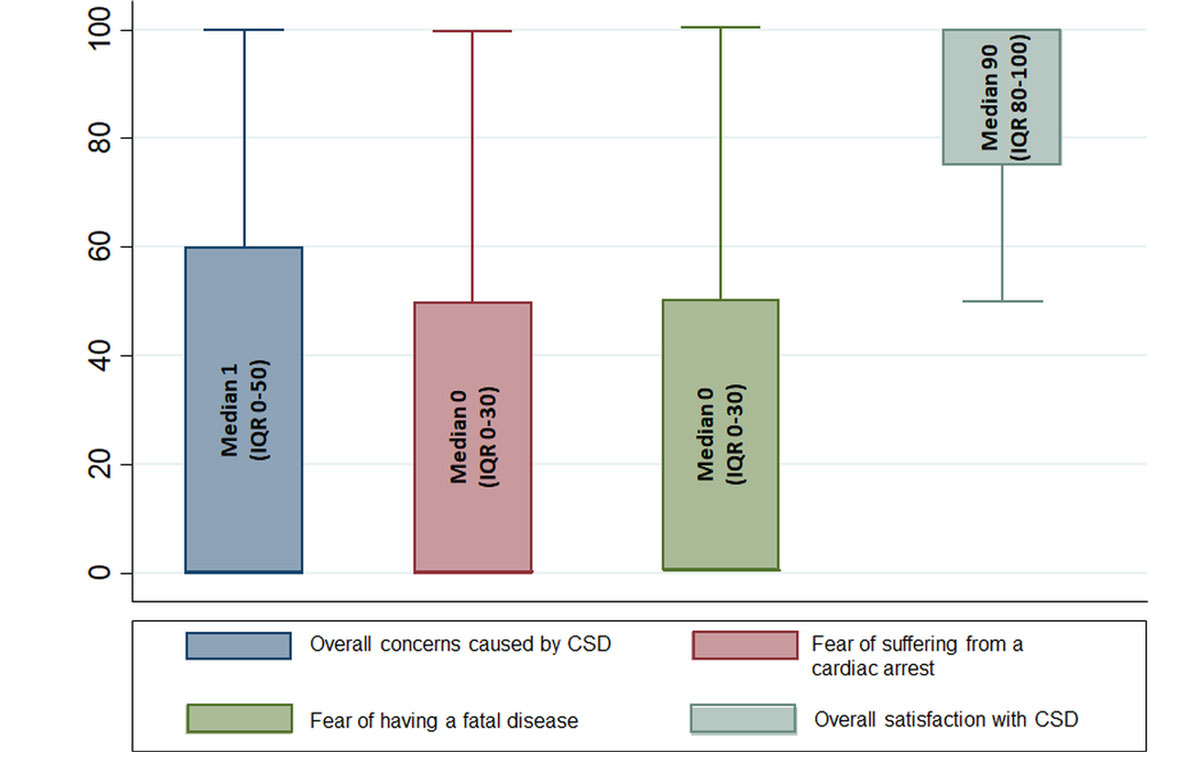
Figure 1a Box plots with median values of patients’ rating of different concerns caused by and satisfaction with communication during code status discussions. CSD = code status discussion
DOI: https://doi.org/10.4414/smw.2020.20194
Code status discussions are a cornerstone of patient-centred medicine and part of what is considered high quality care. A code status determines a patient’s preferences regarding the emergency treatments in case of a cardiac or respiratory arrest. Patients can choose between life-prolonging resuscitation measures (including defibrillation, chest compression and intubation) and palliative therapy focused on the comfort of patients. Conducting a code status discussion is important for understanding patients’ preferences and values in order to act in a patient’s best interest in case of a life-threatening scenario. According to the guidelines of the Swiss Academy of Medical Sciences, these discussions should at best, be conducted upon or shortly after admission, enabling patients to actively participate in the decision making process [1].
However, several challenges to the current practice of code status discussions have been reported including the high complexity of medical information as well as individual perspectives and preferences of both physicians and patients. Furthermore, prior studies have found that physicians show a lack of communication skills and report feeling unprepared when conducting code status discussions [2–6]. The poor quality of code status discussions may also result from clinicians finding it difficult to talk about death and dying [7–9]. Physicians often do not provide enough information about the measures and outcomes of cardiopulmonary resuscitation (CPR). As a result, many patients have misconceptions regarding their chance of survival as well as the likelihood for a good neurological outcome after receiving CPR [10–12]. This information, however, is essential for patients to make an informed decision regarding their code status. A patient’s decision regarding “Do Not Resuscitate” (DNR) code status, which is a legal order to withhold cardiopulmonary resuscitation (CPR) or advanced cardiac life support in case of a cardiac arrest or respiratory failure, has important medical and socioeconomic consequences, such as resource allocation or length of stay in critical care [13, 14]. Still, there is a lack of information about code status discussions during in-hospital care with few systematic studies investigating these issues.
For this study, we conducted a survey to understand current practices and perceptions of code status discussions among patients and physicians. We hypothesised that physicians often omit code status discussion and determine a code status without consulting the patient. With regard to patients, we hypothesised that a substantial proportion of patients’ preferences differs from documented code status and that, in general, code status discussions might lead to patient anxiety and concerns.
This survey was conducted between May and July 2018.
We approached newly hospitalised patients in the Departments of Internal Medicine, Orthopaedics, Cardiac and Vascular Surgery at the University Hospital of Basel in the first two weeks of July 2018.
The University Hospital Basel is the fifth largest hospital in Switzerland, caring for approximately 38,000 patients annually. All patients were approached within the first three days after admission through a face-to-face interview. Answers were typed into an online questionnaire created on surveymonkey.com.
The questionnaire used for the patient survey was developed by an interdisciplinary team (physicians and nurses experienced in emergency and critical care medicine as well as psychologists) based on relevant publications and information obtained during clinical encounters with hospitalised patients.
Some of the items in the questionnaire focused on individuals’ perceptions and expectations regarding code status discussion as well as psychosocial effects.
Answer formats were predominantly dichotomous categories (‘yes’ or ‘no’), for example, when asking for patients’ perception of physicians influencing code status decisions. Other questions used ratings on a visual analogue scale (VAS) from 0–100 (‘strongly disagree’ to ‘strongly agree’), e.g., “overall concerns caused by code status discussion”, “fear of suffering from a cardiac arrest”, “fear of having a fatal disease” and “overall satisfaction with code status discussion” . The German version is available from the authors on request. Electronic patient records were available for all included patients.
Additionally, we contacted heads of different medical clinics in the German-speaking part of Switzerland. Twenty-six heads signalled support, whereupon we sent an email containing a link to a separate online survey created on surveymonkey.com to 597 physicians. All participating physicians were involved in clinical care of patients.
Similar to the patient survey, the physician survey was also developed by an interdisciplinary team. Questions focused on current practices of code status discussions, e.g. perceived optimal timing or duration of code status discussion as well as communicative challenges and potential conflicts. Items in the questionnaire included “self-confidence in conducting a code status discussion”, “perceived fears of patients”, “perceived comprehension of patients”, “perceived influence of patient’s culture on code status decision-making” and “perceived influence of patient’s religion on code status decision-making”, each rated on a VAS 0-100.
English translations of the questionnaires are provided in appendix 1.
The primary outcome of this survey was a fuller comprehension of the prevalence of code status discussions as recalled by patients. We queried whether patient recalled having had a code status discussion (yes / no / do not remember) and their preference for treatment in case of a cardiac arrest, such as “cardiopulmonary resuscitation” (yes/no), “intubation” (yes/no), “medical circulatory support” (yes/no) or “do not know”.
Secondary outcomes included information on the results of the code status discussions, such as preference for resuscitation or DNR, intubation and intensive care treatment. Also, we investigated whether these preferences were in alignment with the documented code status in the patient record. Furthermore, we asked patients whether they have an advance directive (AD) and assessed whether these were documented in the electronic patient record. If an AD was present, we asked patients what direction was given regarding cardiopulmonary resuscitation and evaluated if it was in alignment with the documented code status in the patient record. Additionally, we asked patients about possible concerns and fears (e.g., fear of suffering from a cardiac arrest or fear of having a fatal disease), overall satisfaction and comprehension related to the code status discussion.
We further asked physicians, whether they had ever determined a DNR code status without consulting the patient. We asked physicians to estimate the level of patients’ concern stemming from the code status discussion, the patients’ comprehension regarding the code status, the influence of culture and religion on patients’ code status preferences, and their own confidence in conducting a code status discussion. These responses were recorded on a VAS from 0 to 10. Furthermore, we enquired whether they had experienced conflicts with patients or relatives because of the code status discussion.
Finally, we investigated the outcomes according to age, gender, and medical discipline.
We used descriptive statistics to characterise our study population including medians and interquartile ranges (IQR) for continuous variables in both patient as well as physician data. Counts and proportions were evaluated for binary and categorical variables using chi-square tests. Also, Wilcoxon rank-sum tests were used to investigate differences in continuous data. We also investigated patient data using analyses of variance (ANOVA). A p-value <0.05 was considered significant and all tests were two-sided. We performed all statistical analyses and designed tables using STATA 15.1.
Of 153 approached patients, 145 patients agreed to participate in our survey, of which 89 were male (61.4%) and 56 (38.6%) female. Characteristics of the patient cohort are presented in table 1a.
Table 1 a: Patients’ characteristics (n = 145).
| Gender | Female | 56 (38.6%) |
| Male | 89 (61.4%) | |
| Age (years) | ≤30 | 2 (1.4%) |
| 31–40 | 4 (2.8%) | |
| 41–50 | 12 (8.3%) | |
| 51–60 | 19 (13.1%) | |
| 61–70 | 31 (21.4%) | |
| 71–80 | 40 (27.6%) | |
| 81–90 | 33 (22.8%) | |
| ≥91 | 4 (2.8%) | |
| Hospitalisation site | Internal medicine | 78 (53.8%) |
| Surgical units | 67 (46.2%) | |
| AD = advance directive; CS = code status; CSD = code status discussion | ||
In total, 258 of the 597 (43.2%) physicians that had been approached, participated in the online survey, of whom 130 (50.4%) were male, 123 (47.7%) female and five (1.9%) participants did not specify their gender. A total of 46.5% were junior doctors (residents), 27.7% were senior physicians and 25.8% were consultants. Characteristics of the physician cohort are presented in table 1b.
Table 1b Physicians’ characteristics (n = 258).
| Gender | Male | 130 (50.4%) |
| Female | 123 (47.7%) | |
| Not specified | 5 (1.9%) | |
| Age | ≤30 | 61 (23.9%) |
| 31–40 | 109 (42.7%) | |
| 41–50 | 53 (20.8%) | |
| 51–60 | 26 (10.2%) | |
| ≥61 | 6 (2.4%) | |
| Position | Resident | 119 (46.5%) |
| Senior physician | 71 (27.7%) | |
| Consultant | 66 (25.8%) | |
| Medical field | Internal medicine / neurology | 97 (37.9%) |
| Accident and emergency / intensive care | 64 (25.0%) | |
| Surgical departments | 39 (15.2%) | |
| Haematology/oncology | 32 (12.5%) | |
| Geriatric medicine | 24 (9.4%) |
Of 145 patients, 49 (33.8%) recalled having had a code status discussion, 89 (61.4%) reported not having had such a discussion and seven (4.8%) did not remember. We found significant differences between age groups in terms of the prevalence of recalled code status discussions (χ2 (8) = 17.7, p = 0.02). One out of 18 (5.6%) patients below the age of 51 recalled having had a discussion, while four out of 19 (21.1%) patients between 51 and 60 years, ten out of 31 (32.2%) patients between 61 and 70 years, 18 out of 40 (45%) patients between 71 and 80 years, and 16 out of 37 (43.2%) patients over 80 years reported having had such a discussion. When comparing the different hospitalisation sites, the prevalence of reported code status discussion in the Clinic for Internal Medicine was higher than in the surgical departments, with 34 out of 78 (43.6%) medical patients having had a code status discussion, compared to 15 out of 67 (22.4%) surgical patients (χ2 (2) = 7.29, p = 0.03) (table 2).
Table 2 Reported outcomes.
| Primary outcome: code status discussion | Statistical value | P value | |||
|
Occurence of CSD (as indicated by patient, n = 145)
|
Yes | No | Do not remember | ||
| 49 (33.8%) | 89 (61.4%) | 7 (4.8%) | |||
| Interaction CSD with age (n = 145) | Yes | No | Don't know | χ2 (8) = 17.7 | 0.02 |
| <51 (n = 18) | 1 (5.6%) | 17 (94.4%) | 0 (0.0%) | ||
| 51‒60 (n = 19) | 4 (21.1%) | 15 (78.9%) | 0 (0.0%) | ||
| 61‒70 (n = 31) | 10 (32.2%) | 18 (58.1%) | 3 (9.7%) | ||
| 71‒80 (n = 40) | 18 (45.0%) | 19 (47.5%) | 3 (7.5%) | ||
| >80 (n = 37) | 16 (43.2%) | 20 (54.1%) | 1 (2.7%) | ||
| Interaction CSD with medical field (n = 145) | Yes | No | Do not remember | χ2 (2) = 7.29 | 0.03 |
| Internal medicine (n = 78) | 34 (43.6%) | 40 (51.3%) | 4 (5.1%) | ||
| Surgical (n = 67) | 15 (22.4%) | 48 (71.6%) | 4 (6%) | ||
| Secondary outcomes: patients | |||||
|
Code status according to database (n = 145)
|
Yes | No | No status documented | ||
| 99 (68%) | 33(23%) | 13 (9%) | |||
| Results of code status discussions reported by patients who recalled CSD | |||||
|
Decision regarding resucitation (n = 45*)
|
Yes | No | Do not remember | ||
| 26 (57.8%) | 12 (26.7%) | 7 (15.6%) | |||
|
Decision in accordance with database (n = 38, patients that recalled decision)
|
Yes | No | Not documented | ||
| 28 (73.7%) | 9 (23.7%) | 1 (2.6%) | |||
| Interaction code status decision and age (n = 45*) | Yes | No | Do not remember | χ2(8) = 17.0 | 0.03 |
| <51 (n = 1) | 1 (100.0%) | 0 (0.0%) | 0 (0%) | ||
| 51‒60 (n = 4) | 3 (75.0%) | 0 (0.0%) | 1 (25.0%) | ||
| 61‒70 (n = 9) | 8 (88.9%) | 1 (11.1%) | 0 (0.0%) | ||
| 71‒80 (n = 16) | 10 (62.5%) | 2 (12.5%) | 4 (25.0%) | ||
| >80 (n = 15) | 4 (26.7%) | 9 (60.0%) | 2 (13.3%) | ||
|
Decision regarding intubation (n = 45*)
|
Yes | No | Do not remember | ||
| 11 (24.4%) | 15 (33.3%) | 19 (42.3%) | |||
|
Decision regarding ICU (n = 45*)
|
Yes | No | Do not remember | ||
| 22 (48.9%) | 6 (13.3%) | 17 (37.8%) | |||
| Advanced directives | |||||
|
Advanced directive present (n = 145)
|
Yes | No | |||
| 63 (43.4%) | 82 (56.6%) | ||||
|
Choice resuscitation according to AD (n = 145)
|
Full code | DNR | Do not remember | ||
| 26 (41.3%) | 20 (31.7%) | 17 (27%) | |||
| Interaction AD and age (n = 145) | AD present | AD not present | χ2(4) = 22.9 | <0.0001 | |
| <51 (n = 18) | 2 (11.1%) | 16 (88.9%) | |||
| 51‒60 (n = 19) | 6 (31.6%) | 13 (68.4%) | |||
| 61‒70 (n = 31) | 9 (29.0%) | 22 (71.0%) | |||
| 71‒80 (n = 40) | 20 (50.0%) | 20 (50.0%) | |||
| >80 (n = 37) | 26 (70.3%) | 11 (29.7%) | |||
| Interaction AD and gender (n = 145) | AD present | AD not present | χ2(1) = 5.27 | 0.02 | |
| Female (n = 56) | 31 (55.4%) | 25 (44.6%) | |||
| Male (n = 89) | 32 (36.0%) | 57 (64.0%) | |||
|
Presence of AD in database (n = 63)
|
Yes | No | |||
| 40 (63.5%) | 23 (36.5%) | ||||
|
AD in database in accordance with documented CS (n = 40)
|
Yes | No | |||
| 24 (60.0%) | 16 (40.0%) | ||||
| AD in accordance with database interacting with age (n = 40) | Correct status | Incorrect status | |||
| <51 (n = 1) | 1 (100.0%) | 0 (0.0%) | |||
| 51‒60 (n = 2) | 2 (100.0%) | 0 (0.0%) | |||
| 61‒70 (n = 6) | 6 (100.0%) | 0 (0.0%) | |||
| 71‒80 (n = 15) | 5 (33.3%) | 10 (66.7%) | |||
| >80 (n = 16) | 10 (62.5%) | 6 (37.5%) | |||
| Perceived communication by patients (median and IQR) | |||||
|
Patient's perception that physician wielded influence on CS decision (n = 42)
|
Yes | No | |||
| 3 (7.1%) | 39 (92.9%) | ||||
| Secondary outcomes: physicians | |||||
| Defining code status | |||||
|
Physicians who reported having set DNR without discussion (n = 257)
|
Yes | No | |||
| 186 (72.4%) | 71 (27.6%) | ||||
| Interaction for DNR without discussion and reported conflict (n = 257) | Reported conflict | No reported conflict | χ2(1) = 11.0 | <0.01 | |
| DNR set to no without a discussion (n = 186) | 116 (62.4%) | 70 (37.6%) | |||
| DNR never set to no without a discussion (n = 71) | 28 (39.4%) | 43 (60.6%) | |||
| Interaction for DNR without discussion and position (n = 255) | DNR without talk | no DNR without talk | χ2(1) = 4.01 | 0.05 | |
| Junior doctors (n = 118) | 78 (66.1%) | 40 (33.9%) | |||
| Senior phyiscians and consultants (n = 137) | 106 (77.4%) | 31 (22.6%) | |||
| Perceived challenges | |||||
| Interaction for confidence in conducting a CSD and position (n = 253) | Mean | Standard deviation | F (2, 250) = 24.61 | <0.0001 | |
| Junior doctors (n = 116) | M = 69.3 | SD = 17.1 | |||
| Senior phyiscians (n = 71) | M = 80.6 | SD = 12.0 | |||
| Consultants (n = 66) | M = 83.7 | SD = 12.3 | |||
| Interaction for confidence in conducting a CSD and gender (n = 253) | Median | Interquartile range | Z = 3.03 | <0.01 | |
| Male (n = 130) | Mdn = 80.0 | (71, 90) | |||
| Female (n = 123) | Mdn = 74.5 | (66, 86) | |||
| Interaction for frequency of reported conflicts and gender (n = 253) | Reported conflict | No reported conflict | χ2(1) = 5.16 | 0.02 | |
| Male (n = 130) | 64 (49.2%) | 66 (50.8%) | |||
| Female (n = 123) | 78 (63.4%) | 45 (36.6%) | |||
| AD = advance directive; CS = code status; CSD = code status discussion * missing data for four patients |
|||||
Patients recalling having had a code status discussion were asked about their preference for CPR. Of those, 26 (57.8%) preferred a full code status, 12 (26.7%) preferred not to have CPR and seven patients (15.6%) were not able to recall their code status decision. Of the patients who recalled the code status discussion, 28 out of 38 (73.7%) cases showed congruency between the documented code status and the patient’s preference, while in nine (23.7%) cases it differed. In one patient, the code status was not documented.
Out of 145 patients, 63 (43.4%) had ADs. Of these 63 patients, 17 patients (27.0%) were not able to recall the decision regarding life-sustaining treatment documented in the AD. In 16 out of the 40 (40.0%) patients, who had an AD, the patient’s preference documented in the AD did not match the code status documented in the patient record. We also found a gender difference with 31 out of 56 (55.4%) women having an advance directive compared to 32 out of 89 (36.0%) male patients.
In 23 out of 63 (36.5%) patients who reported having an AD in place, the AD was not noted in the patient record.
Twelve of 145 patients reported having developed general concerns due to the code status discussion (50 or more on a 0–100 scale, median 1, IQR 0–50), and seven patients rated their fear of a sudden cardiac arrest as 50 or more (median 0, IQR 0–30).
Concerning satisfaction with the code status discussion, 29 patients rated 70 or more on a 0–100-scale (median 90, IQR 80–100). The results are shown in figure 1a.
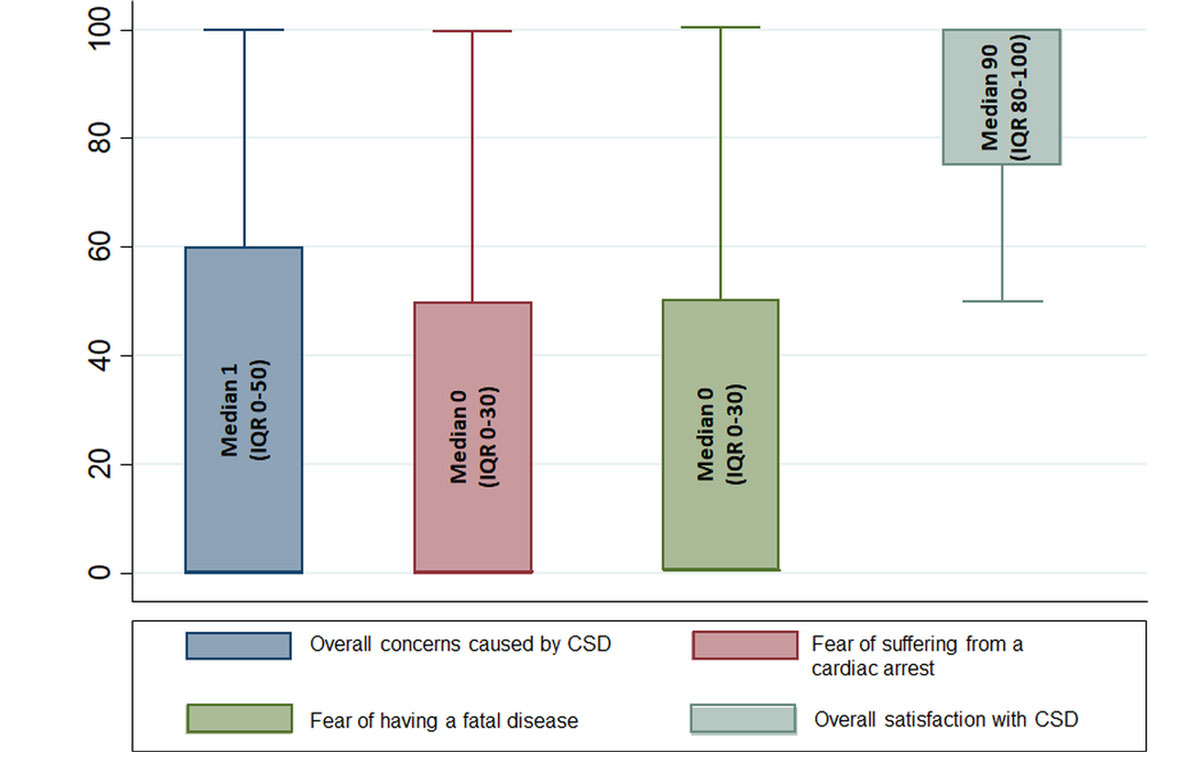
Figure 1a Box plots with median values of patients’ rating of different concerns caused by and satisfaction with communication during code status discussions. CSD = code status discussion
Only three of 42 (7.1%) patients felt that the physician wanted to persuade them to a certain code status.
Of 257 physicians, 186 (72.4%) recalled having set a code status to DNR without prior discussion with the patient at least once. Physicians that determined a DNR status without patient consultation were more likely to report conflicts with patients and relatives regarding the code status (116 of 186, 62.4%) compared to those that had discussed a DNR code status with patients (28 of 71, 39.4%; χ2 (1) = 11.0, p <0.001).
One hundred and forty-seven of 256 (57.4%) physicians estimated patients’ concern following code status discussions 50 or above on a 0–100 scale, median 60 (IQR 40–75). There was no significant difference regarding medical field, gender, or hierarchy of the physician. Furthermore, 49% (125 out of 256) of physicians rated patients’ comprehension to be more than 50 on a 0-100 scale (median 50, IQR 40–70) (fig. 1b).
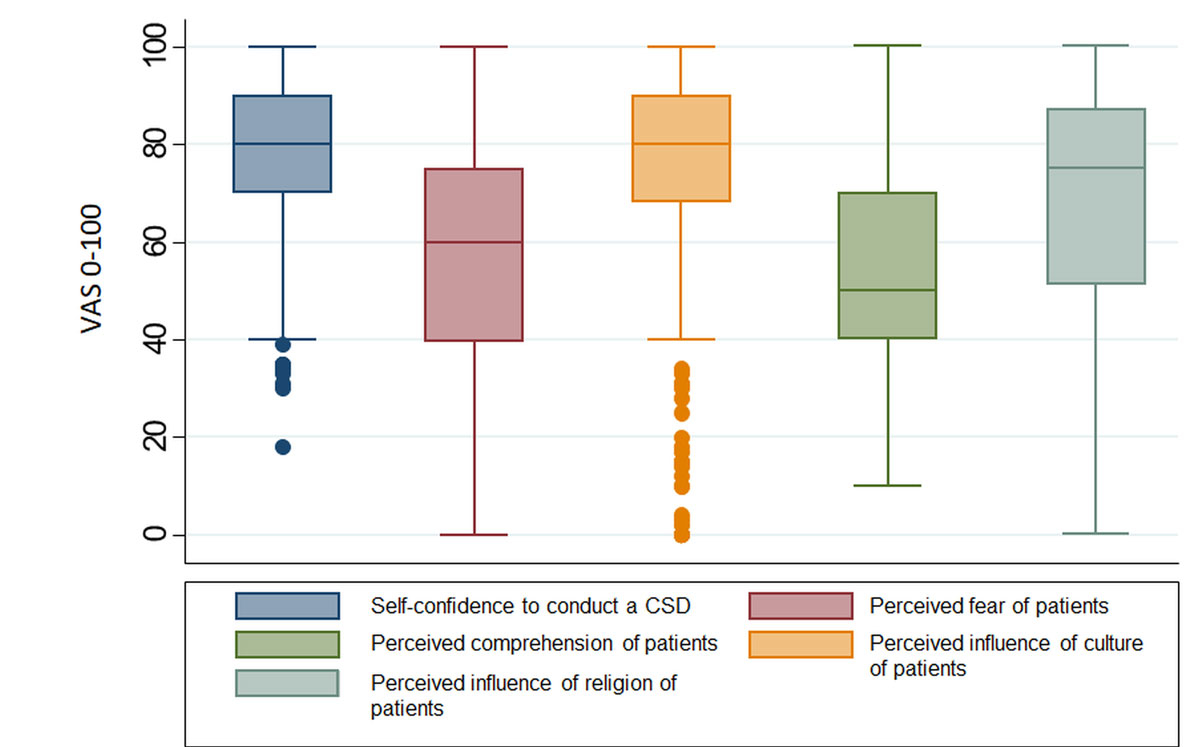
Figure 1b Box-plots with median values of physicians’ rating of perceived own self-confidence to conduct a code status discussion as well as perceived challenges of code status discussions. CSD = code status discussion
The results of our survey showed 195 of 256 (76.2%) physicians rated the influence of religion on code status decisions to be more than 50 on a 0–100 scale (median 75, IQR 51–87), while 213 of 257 (82.9%) physicians rated the influence of culture to be more than 50 on a 0–100 scale, median 80 (IQR 68–90).
Physicians’ confidence in their skills to conduct a code status discussion was rated on a scale from 0 to 100 and demonstrated a significant difference between junior doctors (median 71, IQR 60–81) and senior physicians/consultants (median 85, IQR 75–90) (p <0.001).
There was a significant difference between male, median 80 (IQR 71–90) and female doctors, median 74.5 (IQR 66–86; p <0.01) when evaluating their confidence in their skills in conducting a code status discussion. Significant differences were also found when comparing the frequency of conflicts between male and female physicians and their patients (χ2 (1) = 5.16, p = 0.02). Male physicians (49.2%) reported fewer conflicts than female (63.4%). There was no significant gender difference between male and female doctors to set a DNR without patient consultation.
The main findings of our survey investigating code status discussions during hospitalisation are threefold. First, a majority (61.4%) of patients did not recall having had a code status discussion, though in 91% a code status was documented in their record. Generally, a code status discussion is recommended to be conducted with all patients, as up to 2–3% of hospitalised patients will suffer from a cardiac arrest during their hospitalization [15]. In the case of older patients above 61 years of age, for whom clinical deteriorations or complications are more likely to occur, we found that 67% of patients did not recall having had a code status discussion. In addition, one in six patients could not remember having made a decision during the code status discussion, which might suggest that no proper code status discussion took place or that patients could not remember it.
Second, patients hospitalised in the medical ward were twice as likely to recall having had a code status discussion compared to patients hospitalised on surgical wards. In the perioperative setting, code status discussions are becoming more complex due to medical and ethical issues. With the progress of medicine, more surgical interventions are being performed on older and sicker patients [16].
In the case of interventions with a high risk for complications such as heart surgery, a patient’s choice for a DNR code status might generate a conflict between providing a potential curative intervention and respecting the patient’s choice foregoing resuscitation [17, 18]. In surgery, invasive treatments such as endotracheal intubation, intravenous catecholamines or heart-lung machines are usually performed concurrently and older patients are more susceptible to complications. Even more, complications of severity up to a cardiac arrest are at times directly related to the effects of surgery and anaesthesia. Therefore, over the last decades, hospitals have implemented rigid policies to limit invasive interventions if a DNR status is present [19, 20]. If, nevertheless an invasive procedure is warranted, such as a hip replacement in case of a hip fracture, physicians sometimes unilaterally override a DNR status [21], which might be a reason for the lower amount of code status discussions in the present sample of surgical patients. However, as patients with a witnessed perioperative cardiac arrest have a better prognosis for both survival and neurologic outcome, it is recommended that physicians should initiate a discussion with the patient to find an individual approach and evaluate whether an existing DNR status should be suspended perioperatively as resuscitation efforts might still be in their best interest [17, 22, 23]. In our survey, we found that junior doctors felt less confident than their senior colleagues. Thus, training programmes on how to communicate code status information might help to better prepare younger physicians for such discussions.
Third, despite a majority of patients not recalling having had a code status discussion, 91% of patients had a code status documented in the medical electronic chart. On the one hand, this finding could reflect that patients simply did not remember the code status discussion, indicating a rather unclear mode of communication in terms of both the goal and the content of the discussion by physicians. On the other hand, it could also suggest that physicians documented a code status based on a presumption of patients’ wishes without formally discussing these issues with the patient. In line with this, almost three-quarters of interviewed physicians reported having determined a DNR status without prior patient discussion at least once. Interestingly, these physicians were more likely to report conflicts with patients and relatives regarding code status decisions. It is possible that through the omission or unclear communication of the code status discussion, the patient’s actual preference was misunderstood. Correspondingly, in almost one quarter of patients, there was a discrepancy between the patient’s code status preference expressed in our survey and the documented code status in the medical record. This finding is in line with other studies reporting a discordance between patients’ preferences and determined code status in 20% of hospitalised patients [24].
This study also demonstrated that a third of ADs were not adequately documented in the database and thus not available for the medical team. Similar to the code status discussions, we found discordance in 40% of patients between documented code status and patients’ preferred treatment in case of an emergency as documented in ADs. This was especially prevalent in the older age group that consisted of patients between 71 and 80 years of age, for whom clinical deteriorations are more likely. In this group, 67% of ADs did not match the documented code status. Moreover, 27% of our patients did not know their decision regarding life sustaining treatment documented in their AD. Established electronic health records as well as better accessibility and availability of ADs might further improve this deficiency [25].
Communication deficiencies during code status discussions are not a new phenomenon, but have already been shown in a trial over 20 years ago [26]. The earlier study suggested that patients were not adequately informed regarding the benefits and risks of life-sustaining treatments. Similar to their results, this study found that a majority of patients did not discuss their preference regarding resuscitation attempts with their physician or did not recall a code status discussion. Furthermore, although not assessed in this study, previous studies found that the public’s estimation of functional outcome of cardiopulmonary resuscitation is generally too optimistic [27, 28].
A recent meta-analysis investigated the associations between communication interventions during code status discussions with patients’ knowledge and code status decisions [29]. The study found that videos used as decision aids were effective in increasing patients’ knowledge regarding CPR. As better-informed patients are more likely to actively participate in the decision-making process, the implementation of videos might facilitate code status discussions and overcome any shortcomings in communication. Particularly in surgical disciplines, hospital policy should also ensure that the perioperative workflow better accommodates code status discussions. Moreover, junior doctors might benefit from communication workshops focusing on how to explore patients’ values and goals of care during code status discussion and how to identify patients at risk of poor decision-making.
We are aware of several limitations of our survey. First, a significant limitation of the study is recall bias for the primary endpoint. Many complicating patient-related factors can impact code status discussions. We did not collect information on factors such as altered mental status at the time of admission, severity of presenting symptoms or urgency of admission (i.e. elective admit for a planned surgery versus medical emergency such as myocardial infarction).
Second, the physicians interviewed for this study were not specifically the treating physicians involved in the care of the interviewed patients. A further study should include physicians directly involved in the care of patients to better understand mismatched perceptions. Also, the response rate to our online survey was only around 50%, with notable lack of participation from physicians in surgical departments. Presumably, the physicians that participated in our survey, had a greater affinity for the topic of code status discussions, constituting a bias to our results.
Third, this is a single centre survey in only two departments which limits the generalisability of the results. Fourth, the sample size was relatively small, lowering the effect size of results. Fifth, as the data is based on patient’s recall, we did not further assess whether code status was not remembered by patients or simply had not taken place. Also, the prevalence of ADs in our patient sample was higher than in the normal Swiss population [30], suggesting a possible selection bias towards patients with poorer health conditions or patients with higher education, who are more likely to have an AD. Finally, we do not know, whether potential differences in health status between patients from internal medicine and surgery might partially explain the findings of our study. Furthermore, research should use validated questionnaires to assess patients’ perception regarding their quality of decision-making as well as predictors for a DNR code status such as culture or religious belief.
In conclusion, a majority of patients do not recall having had a proper code status discussion during the hospital stay and physicians frequently omit such discussions, thereby, potentially failing to attend to patients’ code status preferences. Consequent implementation of code status discussions upon hospitalisation, usage of decision aids, illustrating complex medical information and physician training regarding code status discussion might improve quality of patient-centred care.
The appendix is available in a separate file at: https://smw.ch/article/doi/smw.2020.20194.
No financial support and no other potential conflict of interest relevant to this article were reported.
Prof. Sabina Hunziker, MD MPH
1Wissenschaften SAdM (SAMW). Reanimationsentscheidungen. 2017.
2 Margolis B Blinderman C de Meritens AB Chatterjee-Paer S Ratan RB Prigerson HG Educational Intervention to Improve Code Status Discussion Proficiency Among Obstetrics and Gynecology Residents. Am J Hosp Palliat Care. 2018;35(4):724–30. doi:.https://doi.org/10.1177/1049909117733436
3 Sulmasy DP Sood JR Ury WA . Physicians’ confidence in discussing do not resuscitate orders with patients and surrogates. J Med Ethics. 2008;34(2):96–101. doi:.https://doi.org/10.1136/jme.2006.019323
4 Rosenberg LB Greenwald J Caponi B Doshi A Epstein H Frank J Confidence with and Barriers to Serious Illness Communication: A National Survey of Hospitalists. J Palliat Med. 2017;20(9):1013–9. doi:.https://doi.org/10.1089/jpm.2016.0515
5 Mills LM Rhoads C Curtis JR . Medical Student Training on Code Status Discussions: How Far Have We Come? J Palliat Med. 2016;19(3):323–5. doi:.https://doi.org/10.1089/jpm.2015.0125
6 Syed AA Almas A Naeem Q Malik UF Muhammad T . Barriers and perceptions regarding code status discussion with families of critically ill patients in a tertiary care hospital of a developing country: A cross-sectional study. Palliat Med. 2017;31(2):147–57. doi:.https://doi.org/10.1177/0269216316650789
7 Edlich RF Kübler-Ross E . On death and dying in the emergency department. J Emerg Med. 1992;10(2):225–9. doi:.https://doi.org/10.1016/0736-4679(92)90231-H
8 Robinson MA . Informing the family of sudden death. Am Fam Physician. 1981;23(4):115–8.
9 Barnett MM Fisher JD Cooke H James PR Dale J . Breaking bad news: consultants’ experience, previous education and views on educational format and timing. Med Educ. 2007;41(10):947–56. doi:.https://doi.org/10.1111/j.1365-2923.2007.02832.x
10 Tulsky JA Chesney MA Lo B . How do medical residents discuss resuscitation with patients? J Gen Intern Med. 1995;10(8):436–42. doi:.https://doi.org/10.1007/BF02599915
11 Jordan K Elliott JO Wall S Saul E Sheth R Coffman J . Associations with resuscitation choice: Do not resuscitate, full code or undecided. Patient Educ Couns. 2016;99(5):823–9. doi:.https://doi.org/10.1016/j.pec.2015.11.027
12 Fischer GS Tulsky JA Rose MR Siminoff LA Arnold RM . Patient knowledge and physician predictions of treatment preferences after discussion of advance directives. J Gen Intern Med. 1998;13(7):447–54. doi:.https://doi.org/10.1046/j.1525-1497.1998.00133.x
13 Kanoti GA Gombeski WR Jr Gulledge AD Konrad D Collins R Medendorp SV . The effect of do-not-resuscitate orders on length of stay. Cleve Clin J Med. 1992;59(6):591–4. doi:.https://doi.org/10.3949/ccjm.59.6.591
14 De Jonge KE Sulmasy DP Gold KG Epstein A Harper MG Eisenberg JM The timing of do-not-resuscitate orders and hospital costs. J Gen Intern Med. 1999;14(3):190–2. doi:.https://doi.org/10.1046/j.1525-1497.1999.00312.x
15 Kolte D Khera S Aronow WS Palaniswamy C Mujib M Ahn C Regional variation in the incidence and outcomes of in-hospital cardiac arrest in the United States. Circulation. 2015;131(16):1415–25. doi:.https://doi.org/10.1161/CIRCULATIONAHA.114.014542
16 Partridge JS Harari D Dhesi JK . Frailty in the older surgical patient: a review. Age Ageing. 2012;41(2):142–7. doi:.https://doi.org/10.1093/ageing/afr182
17 Truog RD Waisel DB Burns JP . Do-not-resuscitate orders in the surgical setting. Lancet. 2005;365(9461):733–5. doi:.https://doi.org/10.1016/S0140-6736(05)17999-9
18 Scott TH Gavrin JR . Palliative surgery in the do-not-resuscitate patient: ethics and practical suggestions for management. Anesthesiol Clin. 2012;30(1):1–12. doi:.https://doi.org/10.1016/j.anclin.2012.02.001
19 Rabkin MT Gillerman G Rice NR . Orders not to resuscitate. N Engl J Med. 1976;295(7):364–6. doi:.https://doi.org/10.1056/NEJM197608122950705
20 Optimum care for hopelessly ill patients. A report of the Clinical Care Committee of the Massachusetts General Hospital. N Engl J Med. 1976;295(7):362–4. doi:.https://doi.org/10.1056/NEJM197608122950704
21 Waisel DB Simon R Truog RD Baboolal H Raemer DB . Anesthesiologist management of perioperative do-not-resuscitate orders: a simulation-based experiment. Simul Healthc. 2009;4(2):70–6. doi:.https://doi.org/10.1097/SIH.0b013e31819e137b
22 Sprung J Warner ME Contreras MG Schroeder DR Beighley CM Wilson GA Predictors of survival following cardiac arrest in patients undergoing noncardiac surgery: a study of 518,294 patients at a tertiary referral center. Anesthesiology. 2003;99(2):259–69. doi:.https://doi.org/10.1097/00000542-200308000-00006
23 Kazaure HS Roman SA Rosenthal RA Sosa JA . Cardiac arrest among surgical patients: an analysis of incidence, patient characteristics, and outcomes in ACS-NSQIP. JAMA Surg. 2013;148(1):14–21. doi:.https://doi.org/10.1001/jamasurg.2013.671
24 Young KA Wordingham SE Strand JJ Roger VL Dunlay SM . Discordance of Patient-Reported and Clinician-Ordered Resuscitation Status in Patients Hospitalized With Acute Decompensated Heart Failure. J Pain Symptom Manage. 2017;53(4):745–50. doi:.https://doi.org/10.1016/j.jpainsymman.2016.11.010
25Indra P, Frey B. eHealth und Elektronisches Patientendossier. Tribune. August 2017:4-5.
26 The SUPPORT Principal Investigators . A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). JAMA. 1995;274(20):1591–8. doi:.https://doi.org/10.1001/jama.1995.03530200027032
27 Adams DH Snedden DP . How misconceptions among elderly patients regarding survival outcomes of inpatient cardiopulmonary resuscitation affect do-not-resuscitate orders. J Am Osteopath Assoc. 2006;106(7):402–4.
28 Jones GK Brewer KL Garrison HG . Public expectations of survival following cardiopulmonary resuscitation. Acad Emerg Med. 2000;7(1):48–53. doi:.https://doi.org/10.1111/j.1553-2712.2000.tb01891.x
29 Becker C Lecheler L Hochstrasser S Metzger KA Widmer M Thommen EB Association of Communication Interventions to Discuss Code Status With Patient Decisions for Do-Not-Resuscitate Orders: A Systematic Review and Meta-analysis. JAMA Netw Open. 2019;2(6):e195033. doi:.https://doi.org/10.1001/jamanetworkopen.2019.5033
30 Vilpert S Borrat-Besson C Maurer J Borasio GD . Awareness, approval and completion of advance directives in older adults in Switzerland. Swiss Med Wkly. 2018;148:w14642. doi:.https://doi.org/10.4414/smw.2018.14642
Contributed equally to this work
No financial support and no other potential conflict of interest relevant to this article were reported.
Prof. Sabina Hunziker, MD MPH