Recommendations for the admission of patients with COVID-19 to intensive care and intermediate care units (ICUs and IMCUs)
DOI: https://doi.org/10.4414/smw.2020.20227
Swiss Society of Intensive Care Medicine
Basic principles
- Equal care for COVID-19 and non-COVID-19 patients, with the usual criteria for hospitalisation and admission of non-COVID-19 patients remaining valid.
- Consideration of the potential individual benefit of a stay in an ICU or IMCU for each patient, according to the general guidelines of the Swiss Academy of Medical Sciences (SAMS) (Intensive-care interventions, 2013) and the specific guidelines in the event of an influx of patients during severe epidemics (COVID-19 pandemic: triage for intensive-care treatment under resource scarcity, 2020).
- Consideration of available resources such as qualified personnel, specific equipment and specially defined locations in order to avoid capacity overload.
- Wherever possible, spatial consolidation of COVID-19 patients in separated treatment areas to limit the spread of infection in the hospital.
- Implementation of processes to support the healthcare staff in view of a rapidly increasing workload or an overload
- Early identification of patients requiring hospitalisation and possible further triage (see next section)
- Difficult triage decisions should be made jointly in an interdisciplinary / interprofessional team. If possible, obtain a second opinion from a physician not involved in care of the patient under discussion, in order to reduce the emotional burden associated with the decision and to protect those responsible for triage.
- It is recommended to document the triage decisions in writing in every hospital.
Categories of patients with COVID-19 infection requiring admission to a hospital
Self-sufficient patients, no additional oxygen administration required, no organ failure:
- Return home
- Medical checkup by the attending physician after 24–48 hours, depending on the condition
Patients requiring hospital care or oxygen administration, but without severity criteria (see next section):
- Hospitalisation on a ward, if possible defined as COVID-19 ward with usual supervision
- Oxygen administration via nasal cannula/probe, maximum 4 l/min, with intermittent monitoring of oxygen saturation and breathing frequency 3-4 times per day
- Periodic medical evaluation of the clinical course for a timely decision on further action (escalation vs return home)
Patients who require oxygen therapy and continuous monitoring of vital parameters (at least SpO2, ideally blood pressure, heart rate and respiratory rate):
- Hospitalisation in an intermediate care (IMCU) or high dependency unit (HDU)
- Oxygen administration via nasal cannula/probe, Venturi mask or reservoir mask (max. 15 l/min, no nasal high-flow device)
- The use of high-flow oxygen therapy and non-invasive ventilation is not recommended in general and outside of an intensive care unit (risk of aerosols and of rapid deterioration in the case of system failure)
Patients with increasing organ dysfunction (e.g., increasing respiratory failure)
- Transfer to the intensive care unit, if possible into a special COVID-19 area
Criteria to determine inpatient management line
Individual patient characteristics must always be considered:
- Frailty and comorbidities (medical history of the patient)
- Patient wishes, advance directive / advance care planning (ACP) or information from the authorised representative
Table 1 summarises a decision support system for patient assessment.
Table 1 Decision support for patient assessment using the modified Early warning score (adapted from [1]).
|
Parameter
|
3
|
2
|
1
|
0
|
1
|
2
|
3
|
| Age |
|
|
|
<65 |
|
|
>65 |
| Respiratory frequency (/min) |
<9 |
|
9‒11 |
12‒20 |
|
21‒24 |
>25 |
| Oxygen saturation under room air (%) |
<92 |
92‒93 |
94‒95 |
>95 |
|
|
|
| Oxygen supply necessary |
|
Yes |
|
No |
|
|
|
| Systolic blood pressure (mm Hg) |
<91 |
91‒100 |
101‒110 |
111‒219 |
|
|
>219 |
| Pulse (/min) |
<41 |
|
41‒50 |
51‒90 |
91‒110 |
111‒130 |
>132 |
| Consciousness |
|
|
|
Normal |
|
|
Confused, lethargic, coma |
| Temperature (°C) |
<35.1 |
|
35.1‒36.0 |
36.1‒38.0 |
38.1‒39.0 |
>39.0 |
|
Inpatient management according to the Early Warning Score (EWS)
Early warning score (adjusted, see [1]):
- 0‒4 points: hospitalisation without special additional supervision
- 5‒6 points (or ≥3 points in one parameter): intermediate care unit (IMCU) or monitoring unit/room
- >6 points: intensive care unit (ICU)
Possible clinical course of disease
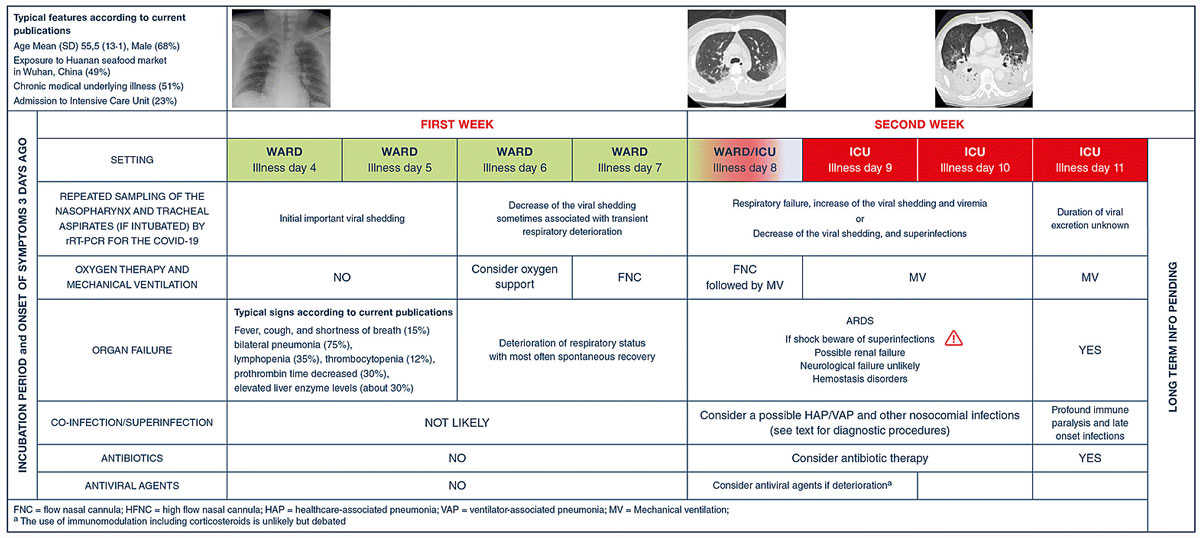
Patients can go through several phases in the disease. It is important to keep track of the clinical course according to the following scheme (fig. 1).
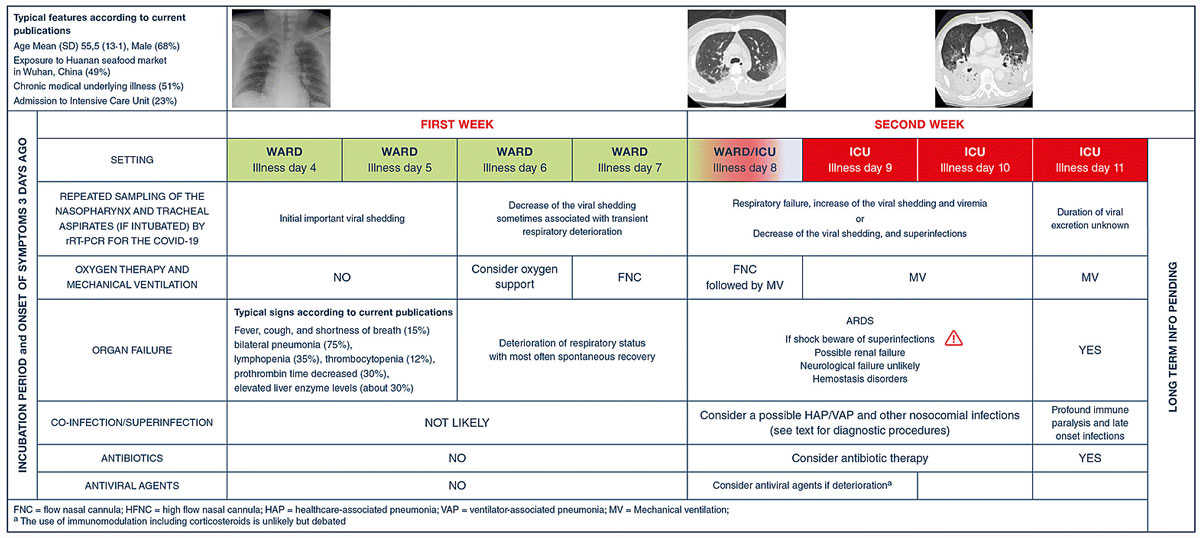
Figure 1 Global picture of severe cases. From [2]: Bouadma L, Lescure FX, Lucet JC, Yazdanpanah Y, Timsit JF. Severe SARS-CoV-2 infections: practical considerations and management strategy for intensivists. Intensive Care Med. 2020 Feb 26 [Epub ahead of print]. © 2020 Springer-Verlag GmbH Germany. Reprinted by permission from Springer Nature.
The following factors have been associated with a greater risk of developing ARDS and may also help in the assessment [3]:
- age >65 years
- fever >39 °C
- lymphopenia and neutropenia
- lactate dehydrogenase (LDH) increase
- increased D-dimers
- interleukin-6 (if available)
Swiss Society of Intensive Care Medicine, c/o IMK Institut für Medizin und Kommunikation AG, Münsterberg 1 , CH-4001 Basel,
References
1
Liao
X
Wang
B
Kang
Y
. Novel coronavirus infection during the 2019-2020 epidemic: preparing intensive care units-the experience in Sichuan Province, China. Intensive Care Med. 2020;46(2):357–60. doi:.https://doi.org/10.1007/s00134-020-05954-2
2
Bouadma
L
Lescure
FX
Lucet
JC
Yazdanpanah
Y
Timsit
JF
. Severe SARS-CoV-2 infections: practical considerations and management strategy for intensivists. Intensive Care Med. 2020 Feb 26; Epub ahead of print. doi:.https://doi.org/10.1007/s00134-020-05967-x
3
Wu
C
Chen
X
Cai
Y
Xia
J
Zhou
X
Xu
S
Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020 Mar 13; Epub ahead of print. doi:.https://doi.org/10.1001/jamainternmed.2020.0994