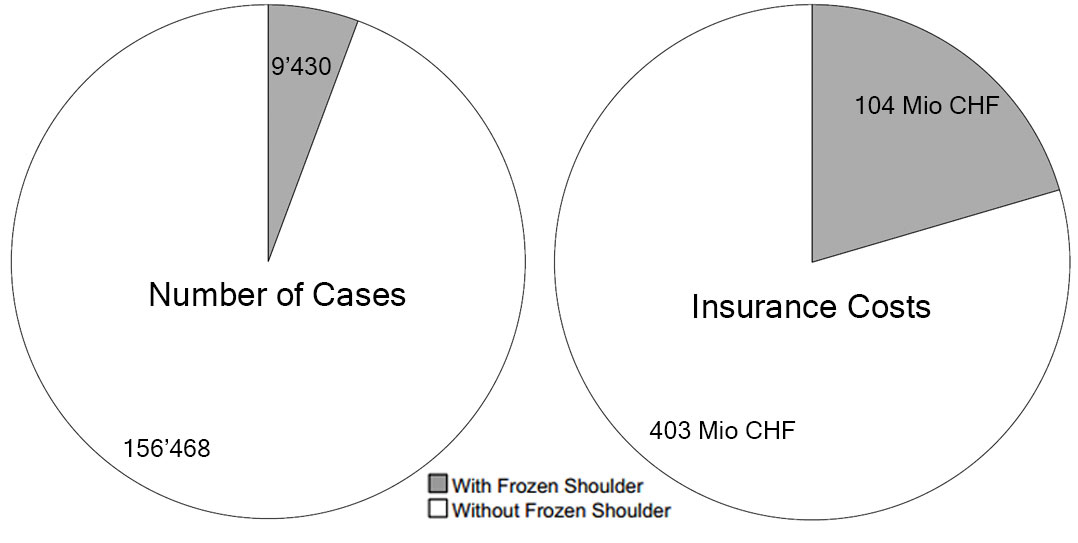
Figure 1 Comparison of the number of shoulder cases (left pie chart) to insurance costs (right pie chart) in the years 2008–2010 (extrapolated) for patients with frozen shoulder (grey piece) and without frozen shoulder (white piece).
DOI: https://doi.org/10.4414/smw.2020.20188
Adhesive capsulitis or frozen shoulder are two synonymously used terms for a stiff shoulder that either occurs after an injury or after shoulder surgery or is idiopathic. However, its aetiology and pathogenesis are not fully understood and therefore therapeutic options are limited, leaving many affected patients with a prolonged period of intense shoulder pain. The average duration of the disease is 18 months with courses of 6–60 months being described [1, 2]. Although the exact pathogenesis of the disease remains unclear, certain risk factors have been identified: The best-known correlated factors were found to be the two endocrine disorders diabetes mellitus and hypothyroidisms [3–6]. Since the disease is self-limiting in the vast majority of cases and not everybody with a frozen shoulder is seen by a healthcare professional, valid epidemiological data are limited. The prevalence of idiopathic frozen shoulder was reported to be as high as 5% [7] or 2.4/1000/year [8], and the occurrence of pathological postoperative stiffness after shoulder surgery ranges from 5–33% in the literature [9]. Since a limited phase of postoperative shoulder stiffness is part of the natural healing process, especially after rotator cuff surgery, the reported numbers might be falsely low. The long course of the disease is often associated with an inability to return to work and/or sports. Particularly in the heavy labour population, this may cause long periods of sick leave and high related indirect costs.
For Switzerland, no current epidemiological data with respect to frozen shoulder-induced direct and indirect costs to the national healthcare system are available. The primary aim of this study was to analyse the frequency, cost and sick leave sequelae of posttraumatic pathological shoulder stiffness in the Swiss population. Secondarily, we analysed demographic risk factors associated with the occurrence of posttraumatic frozen shoulder.
The study was designed as a retrospective cohort study. All acknowledged accidents with shoulder injuries as their main traumatic diagnosis covered by the Swiss Accident Insurance Law from registration years 2008 to 2015 were the base set for this study. Exposure (trauma) and control variables (age, gender) were recorded at baseline (registration). The participants were then followed up over time to observe the incidence of frozen shoulder or outcomes.
For some analyses, the base set is restricted to fewer years because of the availability of outcome data, as described below.
Data from the Statistical Service for the Swiss National Accident Insurance (SSUV) were used for this study. This registry covers all work and leisure time accidents insured under the Swiss Accident Insurance Law. According to this law, the insurance is compulsory for all employees and all those temporarily unemployed in Switzerland, a total workforce of close to 4 million people (SSUV, 2018). The SSUV registry is an anonymous database, as described previously [10, 11]. Coding, which is accident-centred, not person-centred, is by specialised coding staff and based on the case files. Medical diagnoses are in the database only for a representative sample, with weighting or projection factors in the range from 1 to 20. Datasets with International Classification of Diseases, 10th Revision (ICD-10) codes are available for cases registered as from 2008, and the database status after completion of the coding for 2015 was used.
Accidents with shoulder injuries were selected by means of the ICD-10 code of their main trauma diagnosis using the Barrell matrix [12] (or S4* and M84.3* codes).
Sociodemographic information on age (at the time of injury), gender and the year of registration was retrieved from the database, as well as the cases’ main traumatic diagnoses. These diagnoses were grouped if fewer than 200 cases were in the analysis data set, by cropping the last digits of the ICD-10 code. The resulting diagnosis groups used are given in appendix 1, together with sampling and extrapolation procedures. Cases with an additional frozen shoulder diagnosis are identified by the M75.0 diagnostic code. The duration of work incapacity (number of days lost) due to the accident was determined from insurance expenditure data for the first 2 years after registration of the accident. Cases with more than 90 days lost were considered long-term cases; very-long-term cases had incapacity of more than 360 days (so they are a subset of the long-term cases). Owing to the follow-up period necessary for this measurement, this classification was only available for cases with registration between 2008 and 2014.
Healthcare and treatment costs, as well as total insurance expenses, were retrieved from insurance expenditure data. Since the costs of such accidents are incurred over a long period, these costs were measured over a 5-year follow-up period starting with the registration year. Owing to the follow-up period necessary for this measurement, costs were only available for cases with registration between 2008 and 2010.
Sociodemographics: For age, mean values and standard errors were calculated. Significance of differences between groups was tested with t-Test. For categories the chi2 test was applied.
Incidence analysis: The probability of developing a frozen shoulder was analysed through multivariate logistic regression for de-confounding. The input parameters age, age2 (age squared), age3 (age cubed), year of registration, gender, and main diagnosis group were added stepwise to the model with a 0.05 significance level as entry threshold. By inclusion of higher powers of the age variable, possible non-linear age dependencies was taken into account.
Effect of frozen shoulder on work incapacity: The probability of being a long-term (or very-long-term) case was analysed by univariate statistics and through multivariate logistic regression for each main diagnosis group independently. As described above, this analysis used cases with registration between 2008 and 2014 only, because of the follow-up period necessary. The input parameters age, age2, gender, age-gender, frozen shoulder, and age-frozen shoulder were added stepwise to the model with a 0.05 significance level as entry threshold. The odds ratio between cases with and without frozen shoulder, corrected for the other input parameters in the model, quantifies the effect of frozen shoulder on the probability of becoming a (very-) long-term case.
Effect of frozen shoulder on costs: Analysis concerning costs used cases registered between 2008 and 2010 only owing to the follow-up period, and cases with a total healthcare expenditures of less than CHF 100 were omitted from the cost analysis. The impact of frozen shoulder on costs was analysed with a multivariate regression analysis as well, for each main diagnosis group independently. Costs were log10-transformed for use as a dependent variable, and the input parameters age, age2, gender, year of registration and frozen shoulder were added stepwise to the model. The cost ratio between cases with and without frozen shoulder, corrected for the other input parameters in the model, quantifies the additional effect of the frozen shoulder.
For all regression calculations, age 40 years was used instead of age to avoid offset effects. For the same reason, we used the year of registration 2010 in regression calculations.
SAS software version 9.3 (SAS Institute Inc., Cary, NC, USA) was used for statistical analysis throughout the study, and a significance level of 0.05 was used.
A total of 27,184 patients had a shoulder injury coded as a main injury and were selected for analysis, extrapolating to 456,926 cases over the 8-year period. The number of cases with frozen shoulder was projected to 22,228 cases over this 8-year period (table 1). Figure 1 illustrates the relatively small number of frozen shoulder cases accounting for an inappropriately high amount of insurance costs.
Table 1 Patient characteristics with number of observations with shoulder injuries as main diagnosis in sample database (raw cases, unweighted) and extrapolation for total incidences (weighted for projection).
| Total | Without frozen shoulder | With frozen shoulder | |||||
|---|---|---|---|---|---|---|---|
| Unweighted | Extrapolated | Unweighted | Extrapolated | Unweighted | Extrapolated | ||
| Year | 2008 | 3433 | 52,339 | 2915 | 49,199 | 518 | 3140 |
| 2009 | 3632 | 56,604 | 3189 | 53,482 | 443 | 3122 | |
| 2010 | 3641 | 56,955 | 3228 | 53,787 | 413 | 3168 | |
| 2011 | 3487 | 55,699 | 3120 | 52,577 | 367 | 3122 | |
| 2012 | 3457 | 56,961 | 3160 | 54,365 | 297 | 2596 | |
| 2013 | 3419 | 59,773 | 3180 | 57,520 | 239 | 2253 | |
| 2014 | 3147 | 59,349 | 2984 | 56,963 | 163 | 2386 | |
| 2015 | 2968 | 59,246 | 2845 | 56,805 | 123 | 2441 | |
| Gender | Male | 19,419 | 321,310 | 17,570 | 305,819 | 1849 | 15,491 |
| Female | 7765 | 135,616 | 7051 | 128,879 | 714 | 6737 | |
| Age category (years) |
00–19 | 1478 | 29,009 | 1463 | 28,804 | 15 | 205 |
| 20–29 | 4666 | 89,862 | 4546 | 88,298 | 120 | 1564 | |
| 30–39 | 4875 | 89,976 | 4604 | 86,532 | 271 | 3444 | |
| 40–49 | 6679 | 113,991 | 5962 | 107,042 | 717 | 6949 | |
| 50–59 | 6842 | 99,505 | 5827 | 92,296 | 1015 | 7209 | |
| 60–99 | 2628 | 34,282 | 2205 | 31,446 | 423 | 2836 | |
| NA | 16 | 301 | 14 | 280 | 2 | 21 | |
| Main diagnosis | S40 Superficial injury of shoulder and upper arm | 8821 | 173,817 | 8516 | 168,838 | 305 | 4979 |
| S42 Fracture of shoulder and upper arm | 3837 | 56,866 | 3464 | 54,517 | 373 | 2349 | |
| S43 Dislocation and sprain of joints and ligaments of shoulder girdle | 5172 | 98,652 | 4943 | 95,326 | 229 | 3326 | |
| S46.0 Injury of muscles and tendons of the rotator cuff of shoulder | 3879 | 45,926 | 2949 | 39,277 | 930 | 6649 | |
| S46.1 Injury of muscle, fascia and tendon of long head of biceps | 2523 | 26,615 | 1889 | 22,960 | 634 | 3655 | |
| S46.x Other injury of muscle, fascia and tendon at shoulder and upper arm level | 898 | 16,991 | 883 | 16,805 | 15 | 186 | |
| S4x Other injury of shoulder and upper arm | 1989 | 36,797 | 1933 | 36,133 | 56 | 664 | |
| Other | 65 | 1262 | 44 | 842 | 21 | 420 | |
| Total | 27,184 | 456,926 | 24,621 | 434,698 | 2563 | 22,228 | |
| NA = not available | |||||||
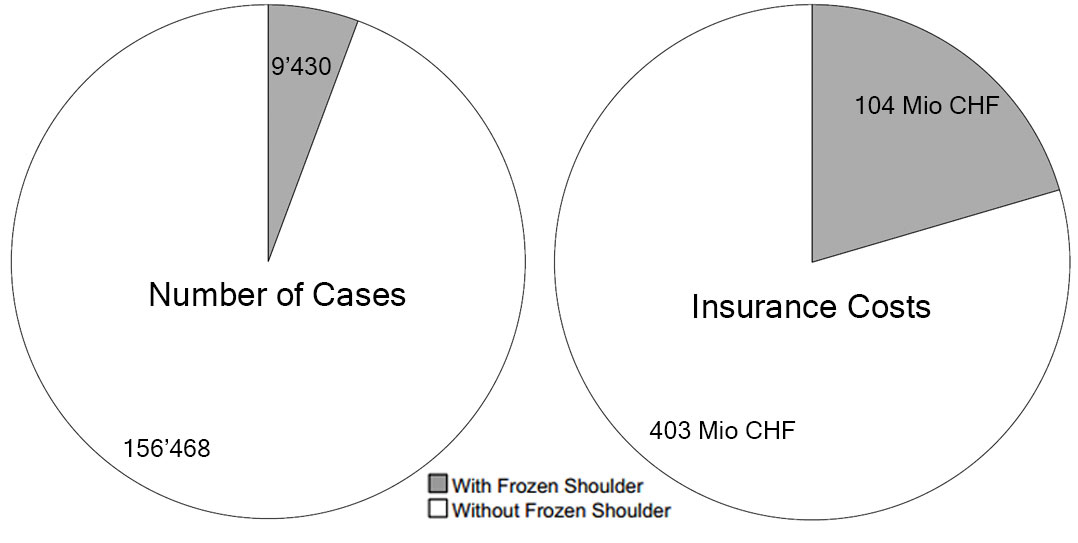
Figure 1 Comparison of the number of shoulder cases (left pie chart) to insurance costs (right pie chart) in the years 2008–2010 (extrapolated) for patients with frozen shoulder (grey piece) and without frozen shoulder (white piece).
Primarily, the incidence of different main diagnoses by age and gender were analysed. More than two thirds of shoulder injuries were in male patients, reflecting the higher proportion of male employees in the Swiss workforce. Table 2 shows the distribution of age and gender, which is quite different between the different main diagnoses. So-called superficial injuries of the shoulder and upper arm (S40), including bruises and scratches, are relatively frequent in women; injuries of muscles, fasciae or long head of biceps tendon (S46.1) have a high proportion in males, and occur at a higher average age.
Table 2 Age and gender of accident victims for cases with shoulder injuries as main diagnosis. For age, mean values and standard deviation are given with p-values from t-tests. For gender, percentage of female accident victims in the subgroups are indicated with p-values from chi2-tests.
| Main diagnosis | Age of accident victim (years) | Female accident victims | ||||
|---|---|---|---|---|---|---|
| Without frozen shoulder | With frozen shoulder | p-value | Without frozen shoulder | With frozen shoulder | p-value | |
| S40 Superficial injury of shoulder and upper arm | 39.8 ± 13.3 | 46.3 ± 12.1 | <0.001 | 36.9 | 34.4 | <0.001 |
| S42 Fracture of shoulder and upper arm | 41.7 ± 14.0 | 48.6 ± 09.9 | <0.001 | 28.6 | 38.2 | <0.001 |
| S43 Dislocation and sprain of joints and ligaments of shoulder girdle | 37.1 ± 12.9 | 43.7 ± 11.6 | <0.001 | 22.3 | 37.2 | <0.001 |
| S46.0 Injury of muscles and tendons of the rotator cuff of shoulder | 47.8 ± 11.8 | 49.3 ± 10.4 | <0.001 | 26.3 | 26.1 | 0.42 |
| S46.1 Injury of muscle, fascia and tendon of long head of biceps | 47.3 ± 12.2 | 49.4 ± 10.2 | <0.001 | 18.4 | 17.3 | 0.09 |
| S46.x Other injury of muscle, fascia and tendon at shoulder and upper arm level | 41.2 ± 12.8 | 46.7 ± 06.1 | <0.001 | 20.8 | 53.8 | <0.001 |
| S4x Other injury of shoulder and upper arm | 39.4 ± 13.1 | 45.0 ± 11.4 | <0.001 | 31.6 | 42.8 | <0.001 |
| Other | 41.8 ± 12.3 | 47.0 ± 13.4 | <0.001 | 38.1 | 33.3 | 0.10 |
| Total | 40.6 ± 13.5 | 47.5 ± 11.2 | <0.001 | 29.6 | 30.3 | <0.001 |
The distribution of shoulder injury diagnoses by gender was different for cases with frozen shoulder as compared with cases without frozen shoulder. After accidents with shoulder dislocation and/or sprain of ligaments (S43), 22% of the cases without frozen shoulder, but 37% of the cases with frozen shoulder, were women. The average age of patients with frozen shoulder was higher than that of the patients without frozen shoulder for all diagnosis groups.
The risk of developing frozen shoulder depends on age and the main diagnosis of the shoulder injury (fig. 2 and supplementary fig. S1 in appendix 2). Logistic regression disentangled the influence of age and gender on the incidence rates of the different traumata on one hand from the probability of developing a frozen shoulder on the other hand. It revealed a strong age-dependency of the probability to develop frozen shoulder (supplementary table S1): Other factors being equal, the risk of developing frozen shoulder after shoulder injury is 10 times higher for a 50-year-old person than for a 30-year old person with the same type of injury.
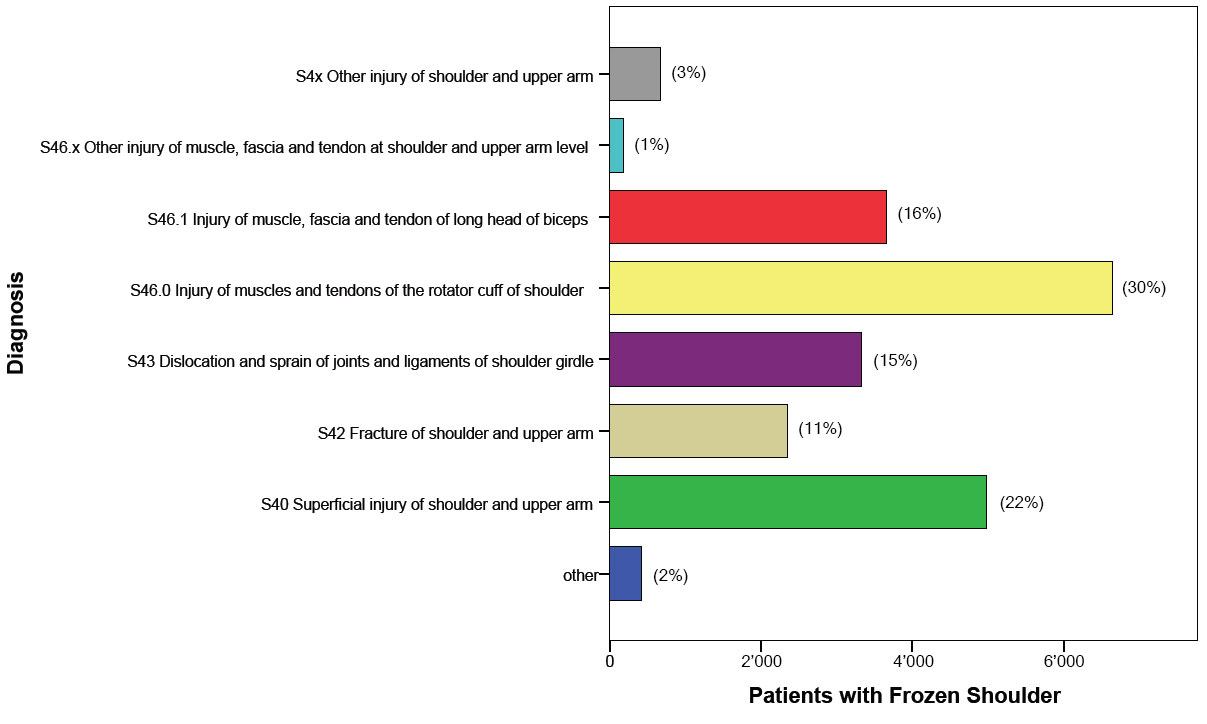
Figure 2 Patients with frozen shoulder (2008–2015, extrapolated) separated by traumatic main diagnosis according to ICD-10.
Traumata associated with a high frozen shoulder risk were not necessarily those ranking high by frozen shoulder incidence: for example, the risk of frozen shoulder was 5 times lower after S40 main diagnoses compared with the risk after S46.0 injuries. However, the absolute number of S40 injuries was high, and so one out of five cases of frozen shoulder were a complication after a “simple” S40 superficial injury of shoulder and upper arm.
Univariate analysis showed that with frozen shoulder a higher fraction of cases led to long-term absence (more than 90 days off work) or very-long-term absence (more than 360 days off work). Of all patients with shoulder injuries, 9.4% were long-term cases, increasing to 30.8% for cases with frozen shoulder, and very-long-term cases rising from 1.3% to 9.7% when frozen shoulder was diagnosed. Depending on the trauma, these fractions vary within a broad range. For cases with S40 main trauma, the proportion of long-term cases was 6 times higher when additional frozen shoulder was observed (fig. 3 and table 3).
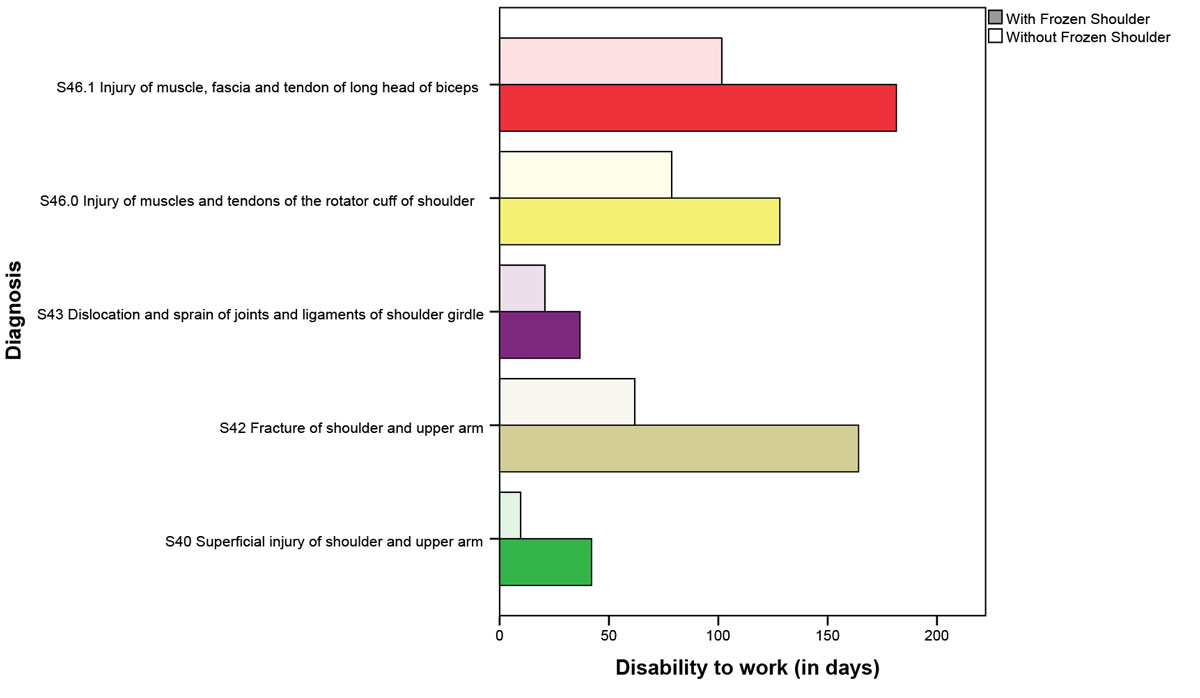
Figure 3 Inability to work separated by diagnosis according to ICD-10 for patients with frozen shoulder (dark bar) and without frozen shoulder (light bar) from 2008–2014 (extrapolation).
Table 3 Inability to work in percentage for patients with frozen shoulder (FS) and without frozen shoulder (without FS) in long-term cases (>90 days) and very-long-term cases (>360 days) separated by main diagnosis. The factor between the two is the respective odds ratio (OR).
| Main diagnosis | Long-term cases | Very-long-term cases | ||||
|---|---|---|---|---|---|---|
| Without frozen shoulder | With frozen shoulder | OR | Without frozen shoulder | With frozen shoulder | OR | |
| S40 Superficial injury of shoulder and upper arm | 2.1% | 13.0% | 6.2 | 0.2% | 1.9% | 9.5 |
| S42 Fracture of shoulder and upper arm | 18.5% | 57.6% | 3.1 | 2.1% | 12.8% | 6.1 |
| S43 Dislocation and sprain of joints and ligaments of shoulder girdle | 5.2% | 12.1% | 2.3 | 0.4% | 3.6% | 9.0 |
| S46.0 Injury of muscles and tendons of the rotator cuff of shoulder | 29.2% | 36.6% | 1.3 | 5.0% | 13.2% | 2.6 |
| S46.1 Injury of muscle, fascia and tendon of long head of biceps | 38.3% | 54.4% | 1.4 | 6.8% | 19.9% | 2.9 |
In order to separate the confounding effects of the trauma, age and gender on work incapacity, on one hand, from the influence of the frozen shoulder complication on the other hand, we used multiple logistic regression. The sociodemographic factors and effects of trauma diagnosis were taken into account by the respective estimates, whereas the estimates for frozen shoulder isolated the influence of an additional frozen shoulder. The effect of frozen shoulder was large and highly significant: For S40 diagnosis, the estimate for prediction of long-term-cases was 1.85 and the effect size was 6.4 (supplementary table S2 in appendix 2). The effect size found with multivariate regression was comparable to the ratio found in the univariate analysis. In other words, for a 40-year-old male patient with a main diagnosis S40, the risk of running into a long-term work absence was 6 times higher when frozen shoulder was diagnosed.
As for the duration of work incapacity, shoulder injury cases without frozen shoulder have significantly lower total insurance costs, by a factor of 4, and treatment costs, by a factor of almost 3 (fig. 4).
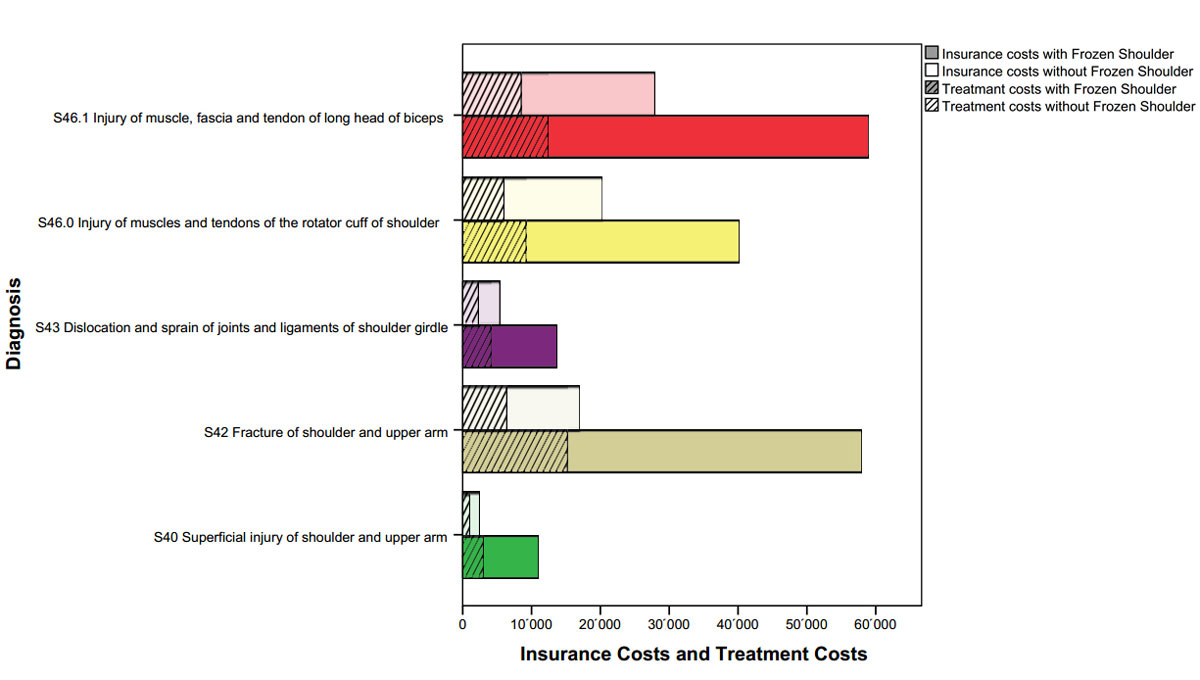
Figure 4 Average treatment costs are shown shaded as a part of the insurance costs for patients with frozen shoulder (dark bar) and without frozen shoulder (light bar) from the years 2008–2010 (extrapolation) with 5 years follow-up.
However, cost distributions were quite skewed, rather resembling a log-normal distribution. In order to isolate the effects of the frozen shoulder as complication, multiple regressions on log-transformed cost data were used. Again, the sociodemographic factors and effects of trauma diagnosis were taken into account in the respective estimates. With these effects eliminated, the estimated β FS for the frozen shoulder parameter directly represented the cost effect of a frozen shoulder patient. This multiplicative factor between cases with or without frozen shoulder was F FS = exp(β FS).
Table 4 shows that the effect of frozen shoulders on cost was a factor between 1.6 and 3.9, depending on the diagnosis group.
Table 4 Logistic regression estimate for the effect on the total insurance expenditures and on treatment costs, standardised for a 40-year-old male.
| Main diagnosis |
Insurance costs in CHF
(5-years of follow-up) |
Treatment costs in CHF
(5-years fof ollow-up) |
||
|---|---|---|---|---|
| Estimate | Effect coefficient | Estimate | Effect coefficient | |
| S40 Superficial injury of shoulder and upper arm | 0.59 ± 0.06 | 3.9 | 0.51 ± 0.05 | 3.2 |
| S42 Fracture of shoulder and upper arm | 0.44 ± 0.07 | 2.7 | 0.37 ± 0.07 | 2.4 |
| S43 Dislocation and sprain of joints and ligaments of shoulder girdle | 0.28 ± 0.09 | 1.9 | 0.29 ± 0.08 | 1.9 |
| S46.0 Injury of muscles and tendons of the rotator cuff of shoulder | 0.21 ± 0.04 | 1.6 | 0.19 ± 0.04 | 1.6 |
| S46.1 Injury of muscle, fascia and tendon of long head of biceps | 0.31 ± 0.06 | 2.0 | 0.24 ± 0.05 | 1.7 |
It can be assumed that the factor (F FS-1) represents the increase of costs due to the frozen shoulder complication. The difference in respective costs per case (CHF 34,000 with frozen shoulder as opposed to CHF 8000 without frozen shoulder) was of the same order of magnitude. By multiplying the annual incidence rates (of roughly 3000 cases per year, see table 1) with the CHF 26,000 difference in costs per case, we found annual costs of CHF 78 million per year for all frozen shoulders in the Swiss compulsory accident insurance system. Although only 1 in 20 shoulder injury cases had a frozen shoulder, within these shoulder injury cases 1 in 6 Swiss francs were spent for the diagnosis of frozen shoulder.
The entire Swiss healthcare system, for a population of 8 million, produces costs of about CHF 70 billion every year, whereof 2 billion (1.5%) are trauma related treatment costs of cases covered by the Swiss Accident Insurance Law (UVG) (SSUV, 2018). The total insurance costs of these cases amount to CHF 4.5 billion per year, and 15% CHF (670 million) thereof are for shoulder injuries. Given the fact that a posttraumatic or postoperative frozen shoulder is “just” a complication of a various underlying pathologies, its impact can be devastating not only from the patient’s perspective but also from a socioeconomic standpoint.
The presented data reveal that the diagnosis of a frozen shoulder is associated with a massive increase in treatment and total insurance costs, as well as a considerable increase in work incapacity. Depending on the index diagnosis, patient who developed frozen shoulder were unable to work between 1.6–4.4 times longer than patients with the same injury who were untroubled by frozen shoulder. When we looked at patients with long-term absences (>90 days) the risk for patients with frozen shoulder was 3.3 times higher. Even worse was the risk for very long-term work incapacity (>360 days), with odds higher by a factor of 7.5 for patients suffering from frozen shoulder. When these data were compared with return-to-work duration after a common injury such as lower leg fracture (SSUV), frozen shoulder patients had a longer time off work although ambulation is not impaired.
Mean treatment costs and total insurance costs for patients with shoulder injuries without frozen shoulder ranged from CHF 1020–8500 and CHF 2450–27,900, respectively. Average costs per shoulder case tripled from CHF 8000 per case to CHF 34,000 when frozen shoulder was diagnosed. The factor by which costs soared when frozen shoulder was involved varied between 1.6 and 3.9, depending on the main diagnosis group: for diagnosis groups with low average costs, the extra costs of frozen shoulder are higher in relation to the costs which are expected without frozen shoulder. Thus, additional costs per single case of frozen shoulder are of the same order of magnitude as, for example, total costs for a fracture of the lower leg, for which average total insurance costs of CHF 25,000 and treatment costs of CHF 11,000 per case are observed (SSUV). We identified patient’s age as an independent risk factor for developing frozen shoulder with an approximately 10-fold higher risk in a 50-year-old patient compared with an injured person at age 30.
As the healthcare costs presented in this study are based on the 3000 registered patients with adhesive capsulitis in the Swiss Accident Registry only, the expenses for all patients with a painful stiff shoulder, including idiopathic frozen shoulders, can only be estimated by taking the yearly incidence of 2.4 patients per 1000 inhabitants into account [8]. Spending way over a CHF 100 million for this medical condition every year is of course a true burden for the Swiss healthcare system.
The findings of our analysis are subject to some limitations. Identification of cases with frozen shoulders relied on diagnoses in medical records. The definitions used may vary among physicians [13], and the extrapolated incidence in our study reflects the diagnoses in the medical records with all their inaccuracies. Our base set may cover half of the Swiss population, but is limited to employed workers. Validity of our findings for working populations of other countries can be limited because of different structures of workforces, economies, or healthcare systems. Furthermore, the impact of frozen shoulder on costs and consequences may depend on many factors that were not been available for our study; for example, manual and over-head work will be hampered far more by frozen shoulder. Unfortunately, since the first description of frozen shoulder by the French surgeon Simon-Emmanuel Duplay in 1872, as “peri-arthrite scapulo-humerale et des raideur de l’epaule” [14], understanding and treatment of this afflictive pathology lacks true progress. Not only to help the affected patients, but also to address the immense socioeconomic impact of frozen shoulder to the healthcare system in Switzerland and everywhere else, a considerable effort in basic and clinical research is needed to improve the status quo.
Frozen shoulder is a very expensive complication after a variety of shoulder injuries which leads to prolonged inability to work when compared to patients without developing posttraumatic or postoperative shoulder stiffness. Apart from the individual agony caused by this condition, frozen shoulder elicits costs of over CHF 100 million and more than a hundred thousand days of sick leave every year – a true burden for the Swiss healthcare system.
This description was first published in: Pain Medicine. 2019;20(8):1559–69. doi:https://doi.org/10.1093/pm/pnz030.
The registry of the Statistical Service for Swiss National Accident Insurance (SSUV) covers all accidents insured under the compulsory Swiss Accident Insurance Law. It comprises approximately 700,000 accidents per year.
The database contains selected variables with administrative data (like the date of the accident, age and gender of the victim, economic branch of the employer, daily allowances and costs) for all cases of the basic set. Additional structured data (like activity at the time of the accident, involved items, course of the accident events, and diagnoses for injuries and health consequences) are obtained by a dedicated team of coding personnel. Coding is done based on the case files.
For financial reasons, obtaining all this additional information for the complete data set is not feasible. Therefore, the statistics are based on a representative sample of the accidents. This sampling method consists of two strata:
Stratum A: Because of their substantial financial impact, all cases with pensions and all occupational disease cases are fully covered. These only account for about 2% of the cases but include more than half of all costs.
Stratum B: From the rest of the cases, a random sample is selected with a given probability that corresponds to the desired sample set. Since 1993, the sampling rate has been set at 5%, which means that every 20th accident is included in the statistic.
To extrapolate the results from the sample, the cases were multiplied by the reciprocal of the sample rate (the extrapolation factor). Since 1993, the cases of the sample have been weighted by a factor of 20. Pensions and occupational diseases are weighted by a factor of 1.
For example, when 420 sample cases from stratum B and 53 pension cases from stratum A are available for a given type of accident, they are extrapolated to (420 × 20) + (53 × 1) = 8453 cases.
It is important to note, that this number represents an unbiased estimate, and the precision of the estimation is based on a random sample, which introduces additional variance. The precision of the results from the 5% sample depends on the size N of the estimated number of cases. With an increasing number of cases, the results are more precise. The relative estimation error or the mean deviation of the projected sample results from the full set is approximately proportional to 1/√N.
Estimation of quantities, for example average costs per case, is possible in an unbiased way likewise. Costs are extrapolated by multiplication of the case costs in the sample with the cases’ corresponding weighting factors.
For example, six cases from the 5% sample of stratum B and costs per case of USD 2000 and one pension case from stratum A with costs of USD 200,000 will result in extrapolated total costs of (6 × 2000 × 20) + (200,000 × 1) = 440,000 USD.
The extrapolated number of cases here would be (6 × 20 + 1) = 121 cases. The average cost is 440,000/(6 × 20 + 1) = 3636 USD.
Scattering of the observed quantities leads to an estimation error (standard error), depending on standard deviation and sample size. These errors have to be calculated for each stratum separately, and then be combined according to the error propagation rules in order to calculate the standard error of the estimate. As the sample size increases, a more precise estimate of the average cost is possible. The precision of estimations can often be improved by combining several years.
Table S1 Logistic regression estimates for age, gender, year of registration and main diagnosis from a model for the risk to develop a frozen shoulder complication.
| Estimate | p-value | ||
|---|---|---|---|
| Parameter | Intercept | −5.062 | <0.0001 |
| Age | 0.113 | <0.0001 | |
| Age2 | −0.00122 | <0.0001 | |
| Year of registration | −0.083 | <0.0001 | |
| Female gender | 0.108 | <0.0001 | |
| Main diagnosis | S40 Superficial injury of shoulder and upper arm | −0.589 | <0.0001 |
| S42 Fracture of shoulder and upper arm | −0.238 | <0.0001 | |
| S43 Dislocation and sprain of joints and ligaments of shoulder girdle | −0.301 | <0.0001 | |
| S46.0 Injury of muscles and tendons of the rotator cuff of shoulder | 0.979 | <0.0001 | |
| S46.1 Injury of muscle, fascia and tendon of long head of biceps | 0.942 | <0.0001 | |
Table S2 Logistic regression estimates (± standard error) showing the effect of frozen shoulder on the probability to be a long-term or very-long-term case, standardised for 40-year-old male.
| Main diagnosis | Model for long-term-cases | Model for very-long-term-cases | ||
|---|---|---|---|---|
| Estimate | Effect coefficient | Estimate | Effect coefficient | |
| S40 Superficial injury of shoulder and upper arm | 1.85 ± 0.03 | 6.4 | 2.00 ± 0.08 | 7.4 |
| S42 Fracture of shoulder and upper arm | 1.62 ± 0.03 | 5.0 | 1.68 ± 0.04 | 5.3 |
| S43 Dislocation and sprain of joints and ligaments of shoulder girdle | 0.99 ± 0.04 | 2.7 | 2.09 ± 0.07 | 8.1 |
| S46.0 Injury of muscles and tendons of the rotator cuff of shoulder | 0.23 ± 0.02 | 1.3 | 0.92 ± 0.03 | 2.5 |
| S46.1 Injury of muscle, fascia and tendon of long head of biceps | 0.53 ± 0.02 | 1.7 | 1.09 ± 0.03 | 3.0 |
Figure S1 Percentage of cases developing frozen shoulder by diagnosis group and age category.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Hand C , Clipsham K , Rees JL , Carr AJ . Long-term outcome of frozen shoulder. J Shoulder Elbow Surg. 2008;17(2):231–6. doi:.https://doi.org/10.1016/j.jse.2007.05.009
2 Vastamäki H , Kettunen J , Vastamäki M . The natural history of idiopathic frozen shoulder: a 2- to 27-year followup study. Clin Orthop Relat Res. 2012;470(4):1133–43. doi:.https://doi.org/10.1007/s11999-011-2176-4
3 Bridgman JF . Periarthritis of the shoulder and diabetes mellitus. Ann Rheum Dis. 1972;31(1):69–71. doi:.https://doi.org/10.1136/ard.31.1.69
4 Cakir M , Samanci N , Balci N , Balci MK . Musculoskeletal manifestations in patients with thyroid disease. Clin Endocrinol (Oxf). 2003;59(2):162–7. doi:.https://doi.org/10.1046/j.1365-2265.2003.01786.x
5 Lo SF , Chu SW , Muo CH , Meng NH , Chou LW , Huang WC , et al. Diabetes mellitus and accompanying hyperlipidemia are independent risk factors for adhesive capsulitis: a nationwide population-based cohort study (version 2). Rheumatol Int. 2014;34(1):67–74. doi:.https://doi.org/10.1007/s00296-013-2847-4
6 Milgrom C , Novack V , Weil Y , Jaber S , Radeva-Petrova DR , Finestone A . Risk factors for idiopathic frozen shoulder. Isr Med Assoc J. 2008;10(5):361–4.
7 Hsu JE , Anakwenze OA , Warrender WJ , Abboud JA . Current review of adhesive capsulitis. J Shoulder Elbow Surg. 2011;20(3):502–14. doi:.https://doi.org/10.1016/j.jse.2010.08.023
8 van der Windt DA , Koes BW , de Jong BA , Bouter LM . Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis. 1995;54(12):959–64. doi:.https://doi.org/10.1136/ard.54.12.959
9 Huberty DP , Schoolfield JD , Brady PC , Vadala AP , Arrigoni P , Burkhart SS . Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy. 2009;25(8):880–90. doi:.https://doi.org/10.1016/j.arthro.2009.01.018
10 Scholz-Odermatt S . Die UVG-Medizinstatistik im Internet. Med Mitt. 2008;79:124–32. Available at: https://core.ac.uk/download/pdf/33062329.pdf
11 Scholz-Odermatt SM , Luthi F , Wertli MM , Brunner F . Direct Health Care Cost and Work Incapacity Related to Complex Regional Pain Syndrome in Switzerland: A Retrospective Analysis from 2008 to 2015. Pain Med. 2019;20(8):159–69. doi:.https://doi.org/10.1093/pm/pnz030
12 Fingerhut LA , Warner M . The ICD-10 injury mortality diagnosis matrix. Inj Prev. 2006;12(1):24–9. doi:.https://doi.org/10.1136/ip.2005.009076
13 Kobayashi T , Karasuno H , Sano H , Hamada J , Takase K , Tamai K , et al. Representative survey of frozen shoulder questionnaire responses from the Japan Shoulder Society: What are the appropriate diagnostic terms for primary idiopathic frozen shoulder, stiff shoulder or frozen shoulder? J Orthop Sci. 2019;24(4):631–5. doi:.https://doi.org/10.1016/j.jos.2018.12.012
14 Duplay S . De la periarthrite scapulohumerale. Rev Frat D Trav De Med. 1896;53:226.
No financial support and no other potential conflict of interest relevant to this article was reported.