
Figure 1 Article selection flow chart.
DOI: https://doi.org/10.4414/smw.2020.20193
confidence interval
diffuse cutaneous systemic sclerosis
Institute for Work and Health (Institut universitaire romand de Santé au Travail)
limited cutaneous systemic sclerosis
odds ratio
systemic sclerosis
Swiss National Accident Insurance Fund (Schweizerische Unfallversicherungsanstalt)
Systemic sclerosis (SSc) is a rare autoimmune disease of unknown aetiology. It is more common among women and some ethnic minorities [1], with a prevalence varying between 31 and 277 per million in Europe [2]. Three main features characterise the pathogenesis of SSc: fibroblast dysfunction resulting in fibrosis, vasculopathy and the production of autoantibodies against various cellular antigens [3]. The disease’s three main clinical expressions are limited cutaneous systemic sclerosis (lcSSc), diffuse cutaneous systemic sclerosis (dcSSc), and systemic sclerosis without scleroderma. Each is characterised by different clinical manifestations and the production of different antibodies [4], representing a major diagnostic challenge to physicians. The gold standard classification criteria are the 2013 American College of Rheumatology (ACR) / European League Against Rheumatism (EULAR) criteria [5].
Although the aetiology of systemic sclerosis is not yet completely understood, it is now admitted that it is a multifactorial disease involving a gene–environment interaction [6]. Indeed, several environmental factors are suspected of contributing to the disease’s development, including infectious diseases (Helicobacter pylori, cytomegalovirus…), smoking and certain drugs (bleomycin). Epidemiological studies have also identified several occupational factors, such as exposure to silica, solvents or vibration [7–10]. Although SSc is not currently on the list of occupational diseases recognised by the International Labour Organization [11], recent studies have led several European countries to include SSc in their lists of compensable occupational diseases [12] or at least to begin discussing its addition to those lists [13].
The present article aims to demonstrate which patients are likely to have SSc recognised as an occupational disease and to describe the main types of occupational exposure related to systemic sclerosis, with reference to Switzerland’s occupational disease recognition system. To achieve these aims, we present the cases of five patients with systemic sclerosis who were referred for occupational pathology consultations at the Institute for Work and Health (IST). After reviewing the recent literature, we summarised the possible conditions necessary for patients in Switzerland who have systemic sclerosis to be recognised as having an occupational disease. We also identified the red flags that physicians should look out for to identify eligible patients.
We report on five patients referred for occupational pathology consultations between 2011 and 2017 by their physicians. They were all suffering from systemic sclerosis, with features matching the 2013 ACR/EULAR criteria, and had a suspected occupational exposure to solvents and/or silica. In each case, the consultation was followed by a literature review to determine whether there was enough support to declare the patient’s case to his or her occupational health insurance company. We present a synthesis of the relevant literature published in the last 20 years. The search was performed using the PubMed database for articles published between January 1997 and October 2018 with the terms “scleroderma”, “systemic sclerosis”, “occupation”, “occupational exposure”, “solvent”, “organic solvent”, and “silica”. The first search found 453 articles. After the exclusion of publications in languages other than French or English, and non-pertinent articles after reviewing their titles, 109 articles were selected. We then performed an abstract review and a bibliography review, and after excluding case reports and animal studies, 68 articles were selected for a full article review. Figure 1 summarises the article selection procedure.

Figure 1 Article selection flow chart.
Based on the literature review, we established a list of red flags which physicians could use to identify patients who had suffered occupational exposure to silica or a solvent.
Five patients suffering from systemic sclerosis were referred for an occupational pathology consultation between 2011 and 2017. Table 1 summarises their main characteristics.
Table 1 Case descriptions.
| Sex | Female | Male | Male | Male | Male | |
| Age (years) | 62 | 51 | 38 | 51 | 56 | |
| Diagnosis | lcSSc | dcSSc | Overlap syndrome | dcSSc | lcSSc | |
| Age at diagnosis (years) | 57 | 50 | 38 | 50 | 26 | |
| Latency (years) | 27 | 27 | 8 | 35 | 6 | |
| Occupation | Laboratory technician, Hairdresser | Sanitary and heating installer, foundry worker | Waterproofing specialist, sanitary and heating installer | Bricklayer | Painter | |
| Occupational exposures | Solvents | 14 years | 13 years | 7 years | 21 years | 2–6 years |
| Silica | – | 23 years | 7 years | 21 years (important), 5 years (less) | – | |
| Welding fumes | – | 11 years | – | – | – | |
| Epoxy resin | – | 11 years | 7 years | 4 years | – | |
| Hair dyes | 2 years | – | – | – | – | |
| Vibration | – | – | – | – | – | |
| Declared as an occupational disease |
Yes | Yes | Yes | Yes | No | |
| Recognised as an occupational disease | Yes | No | Yes | No | No | |
dcSSc = limited cutaneous systemic sclerosis; lcSSC = diffuse cutaneous systemic sclerosis Occupations in bold type correspond to the most relevant occupational exposure.
A 62-year-old woman was referred for an occupational pathology consultation at the IST in 2011 after having been diagnosed as suffering from lcSSc five years before, when she was 57. She had worked as a hairdresser for 2 years, from age 16, where she permed, dyed and highlighted hair. She subsequently worked for 1 year as a pharmaceutical industry laboratory assistant, although she could not recall any specific exposure, and then as a salesperson in a dairy for another year. She then worked in a match factory for 12 years and may have been exposed to paraffin wax. Her most relevant occupational exposure occurred during her next job as a laboratory technician, where she regularly used about 2 L of organic solvents (methanol, toluene, chloromethane, and chloroform) per day for 14 years while carrying out chromatography analyses. There was no proper ventilation in the laboratory for the first 2 years. She described dizziness and nausea on workdays, especially in the afternoons or evenings. A team of occupational hygienists from the IST performed an experimental exposure simulating the patient’s description of her main activity. The simulation monitored the concentrations of methanol and toluene in a closed room as the contaminants evaporated from a glass beaker. The results confirmed significant exposure to solvents; however it was under the 8-hour exposure limit.
The patient finally worked until she was 61 years old without further significant exposure. Thus, she was probably exposed to organic solvents for 14 years (including 2 years involving significant exposure) and to hair dyes for 2 more years. The diagnosis of SSc was made 27 years after her first exposure to solvents, and her first symptom clearly related to SSc was Raynaud’s phenomenon, which appeared 10 years after the first exposure. The Swiss National Accident Insurance Fund (SUVA) recognised this patient’s SSc as an occupational disease after considering her exposure to solvents.
A 51-year-old man was referred for an occupational pathology consultation in 2012. He had been diagnosed with dcSSc at the age of 50. He had worked as a salesperson in a tool shop for 4 years and then done 2 years of military service without significant exposure. He then worked as a sanitary and heating technician for 11 years, mainly installing water pipelines but also using a jackhammer to make holes in walls, comprising about one third of his working time. He also degreased pipes using various organic solvents and sometimes welded them. He was therefore likely to have been exposed to silica, asbestos and vibration, and to a lesser extent to solvents and welding fumes. He subsequently worked as a foundry worker for 16 years. For 4 years, he worked exclusively on straightening and cleaning foundry pieces using trichloroethylene. For 9 years, he continued in that role for one third of his working time and spent the other two thirds of this working time sandblasting. He described using personal protection equipment (anti-dust mask, leather gloves, and earplugs) sporadically. After the consultation, a workplace visit to the foundry by an occupational physician and industrial hygienists concluded that there was significant exposure to silica and trichloroethylene. Throughout his career, he was therefore probably exposed to silica for 23 years, to organic solvents (mainly trichloroethylene) for 13 years, and to epoxy resins and vibration for 11 years. The first clinical manifestation of SSc appeared 23 years after the first significant exposure and the diagnosis was made after 27 years. The patient was still exposed at the time of diagnosis. SUVA refused to recognise this patient’s dcSSc as an occupational disease.
A 38-year-old patient was referred for an occupational pathology consultation in 2015 after he had been diagnosed a few months previously with an overlap syndrome with clinical features of SSc, Sjögren syndrome and rheumatoid arthritis. He had first worked for 6 years as a sanitary and heating technician, and then for 5 as a sanitary and heating business manager. He subsequently worked as a waterproofing specialist for 7 years, until he was 37, when he stopped because of his medical condition. During this period, he polished surfaces with a grinder or a polishing machine for thre -quarters of his working time. He rarely did sanding operations, but prepared and applied epoxy resin. He also had to clean tools and surfaces, mainly using about 2 L of toluene and 1 L of acetone per working day, sometimes in confined workplaces. After the consultation, a workplace visit by an occupational physician and industrial hygienists discovered significant exposure to toluene, silica and epoxy resins.
The patient had therefore been significantly exposed to silica and organic solvents, mainly toluene and acetone, with 7 years of continuous exposure followed by 6 years of intermittent exposure. He was also exposed to epoxy resin for 7 years. The first clinical manifestations of an autoimmune disease appeared 7 years after his first recognised exposure, and a diagnosis of SSc was made 1 year later. SUVA recognised this patient’s SSc as an occupational disease after considering his occupational exposure to solvents.
A 51-year-old patient was referred for an occupational pathology consultation in 2017 after he had been diagnosed with dcSSc 2 years earlier. He initially worked for 16 years for the same employer as an apprentice bricklayer, then as a bricklayer, and finally as foreman. After that, he worked in two other places as a construction foreman, for 4 years and 10 months, respectively. During these periods, he was probably exposed to silica dust and possibly to organic solvents, even though it could not be established which solvents or at what intensities of exposure. Between 2002 and 2006, he worked as a logistician and maintenance technician and was exposed intermittently to silica. Since 2007, he had worked as a paramedic without any relevant exposure. Over his whole career, he was exposed to silica for 21 years and then intermittently for 5 years. He was exposed to solvents intermittently for 21 years, and to epoxy resins for 4 years. The first clinical manifestation of SSc appeared 34 years after his first exposure and 8 years after his last exposure to silica, and the diagnosis was made one year later. SUVA refused to recognise this patient’s condition as an occupational disease.
A 56-year-old patient was referred for an occupational pathology consultation in 2017 after he had been diagnosed with lcSSc at the age of 26 years. In the 30 years preceding the consultation, he had had no medical follow-up. Thirty-six years previously, he had worked as a cabinetmaker for 3 years, and he reported daily exposure to paints, including some containing lead and organic solvents. He was also exposed to wood dust during this period. He was unable to remember the names of the different products. He subsequently worked as a painter and decorator, and described exposure to paint (synthetics, acrylics), large amounts of solvents (especially turpentine spirits), and maybe to asbestos and silica, although to a lesser extent. The diagnosis of SSc was made 2 to 4 years after his first exposure to solvents. The patient was not given a recommendation to seek recognition of his lcSSC as an occupational that the patient had used, the unusually short latency, the lack of any medical follow-up that might describe the disease’s evolution, and the fact that, as he was self-employed, he had not been covered by an insurance policy for occupational diseases.
An association between occupational exposure to silica dust and SSc has been suspected since 1914 [14]. Since then, more and more epidemiological studies have confirmed this association, including 12 in the last 20 years. Among the eight case-control studies we analysed for this review, six found a statistically significant excess of risk, with odds ratios (ORs) ranging from 1.39 to 10.4 [15–22]. Three of four cohort studies showed positive relative risk (RR) ranging from 7.4 to 37 [23–26]. These studies considered patients from the USA or Europe. A recent meta-analysis by Rubio et al. [27] analysed these studies plus 10 other older studies, including grey literature. All the studies examined had a quality score above five on the Newcastle-Ottawa Scale, allowing the authors to conclude that the combined risk of the 15 case-control studies (1336 patients) was 2.81 (95% confidence interval [CI] 1.86–4.23; p <0.001) and was 3.06 (95% CI 1.90–4.91; p <0.001) for male patients. For the four cohort studies, incorporating 247,563 patients, the overall RR was 17.52 (95% CI 5.98–51.37; p <0.001). These results confirmed an earlier meta-analysis performed by McCormic et al. [28] on three cohort studies, nine case-control studies and four mortality studies. McCormic et al. found similar results, with a combined overall RR of 3.20 (95% CI 1.89–5.43). The RRs for case-control and cohort studies were estimated at 2.24 (95% CI 1.65–3.31) and 15.49 (95% CI 4.54–52.87), respectively. Figure 2 summarises these results.

Figure 2 Results of studies about systemic sclerosis and silica. CI = confidence interval
The strong statistical associations found in these epidemiological studies are not the only arguments for a causal relationship. Indeed, some of these studies have found dose-response gradients [7, 19], and data from experimental studies argue for the biological plausibility of a relationship [29, 30]. We did not find enough data in the literature to assess exposure duration or exposure intensity thresholds. In fact, a relationship was found even for exposure durations shorter than 6 years [29]. It is also interesting to add that a review by Freire et al. [30] described the main clinical difference between SSc patients with or without exposure to silica. Patients exposed to silica tended to be male, had a diffuse form of SSc, showed Scl70 antibodies and suffered more often from interstitial lung disease [30].
Solvents are one of the most frequent chemical occupational exposures [31]. Associations between occupational exposure to solvents and systemic sclerosis have also been studied for decades. Indeed, after the first description in 1957 [32], numerous epidemiological studies have reported that solvent exposure may cause SSc. Nine case studies [15, 16, 18, 19, 33–37] and five meta-analyses [27, 38–41] examining this association were identified in our literature review. Seven of the nine case-control studies published in the last 20 years showed significant associations, with ORs ranging from 1.7 to 3.2 [15, 16, 18, 33–36].
The meta-analysis by Aryal et al. [38] included seven case-control studies and one cohort study, and had an overall RR of 2.91 (95% CI 1.60–5.30). According to the authors, it showed significant heterogeneity, which was attributed to the design of the studies. In 2007, Kettaneh et al. [39] published another meta-analysis of 11 reports covering a total of 1291 cases drawn mainly from European countries (8 out of 11) and found an overall OR reaching 2.41 (95%CI 1.73–3.37). The risk of SSc among men exposed to solvents was found to be higher among men exposed to solvents than among women (p = 0.03). In 2012, Barragan et al. [40] also conducted a meta-analysis dealing with the association between organic solvent exposure and autoimmune disease. This included eight case studies about SSc and resulted in an OR of 2.52 (95% CI 1.24–5.14). In 2016, Zhao et al. [41] published a meta-analysis of 14 case-control studies and calculated an overall OR of 2.07 (95% CI 1.55–2.78), with ORs of 5.28 (95% CI 3.48–8.05) for men and 1.62 (95% CI 1.34–1.96) for women. The most recent meta-analysis by Rubio et al. [27] included 13 case-control studies with the mid-cohort years ranging from 1983 to 2006; it comprised 2107 patients and had a quality score above six on the Newcastle-Ottawa Scale; its overall OR was 2.00 (95% CI 1.32–3.02), the OR for men was 2.40 (95% CI 1.44–4.01) and for women was 2.01 (95% CI 1.66–2.44). Figure 3 summarises all these results. Interestingly, the results found by Kutting et al. [37] contrasted with the other studies. This can be explained by the fact that their study compared patients who had SSc with patients who had multiple sclerosis, which is also an autoimmune disease with implied environmental factors. One might therefore wonder whether the exposures examined in that study could also be involved in the development of multiple sclerosis, which might explain the OR below one.
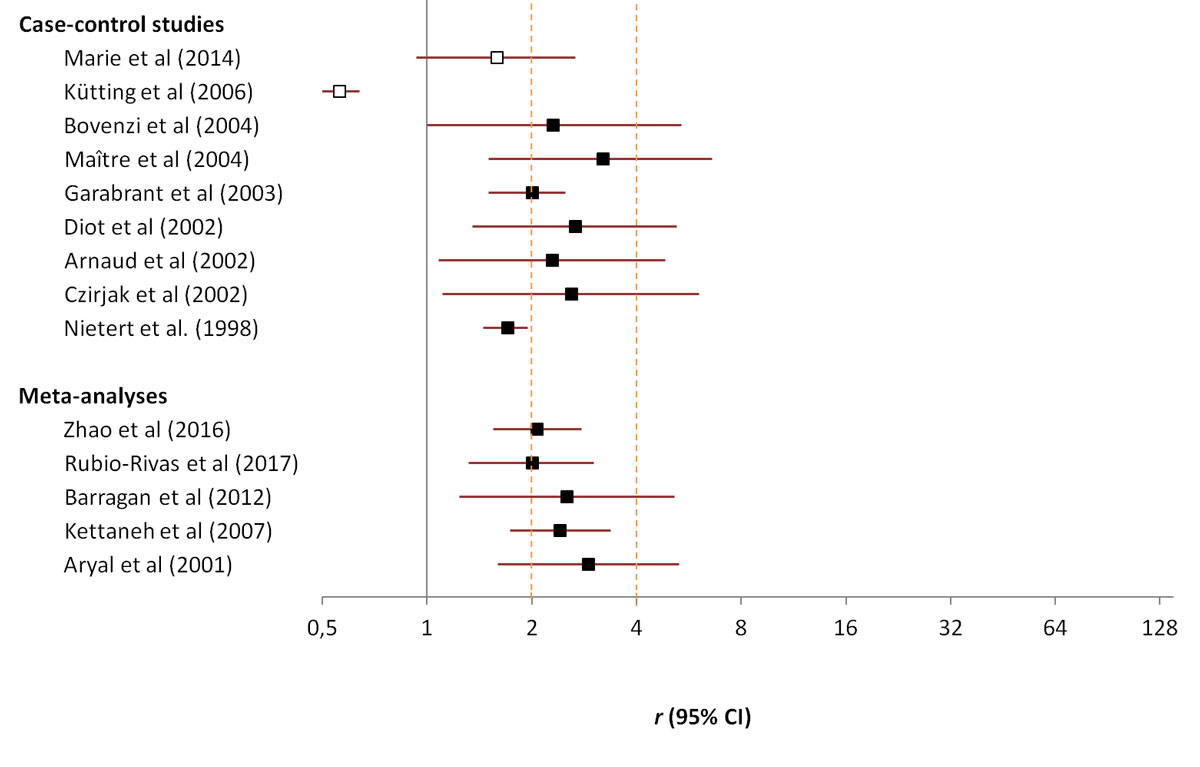
Figure 3 Results of studies about systemic sclerosis and solvents. CI = confidence interval
Some of these studies tried to examine specific solvent exposures [16, 19, 33, 36, 41]. The meta-analysis performed by Zhao et al. [41] also included a subgroup analysis which showed significant associations between SSc and several specific solvents: aromatic solvents, with an OR of 2.07 (95% CI 1.21–6.09); trichloroethylene, with an OR of 2.07 (95% CI 1.34–3.17); halogenated solvents, with an OR of 1.49 (95% CI 1.12–1.99); and ketones, with an OR of 4.20 (95% CI 2.19–8.06). Most of these studies did not take into account the levels and durations of exposure, and we did not find enough data to assess an exposure threshold in terms of duration or intensity. Marie et al. [42] showed that exposure to solvents could be a predictive parameter of SSc severity. Patients exposed to solvents showed significantly higher rates of the diffuse form of SSc, digital ulcers, interstitial lung disease, myocardial dysfunction and cancer [42]. The same study described how patients exposed to solvents showed more Scl70 antibodies than controls. Even though the biological mechanisms that trigger SSc in a solvent-exposure scenario remain unclear, several studies have suggested its biological plausibility [8, 43, 44].
Epoxy resins are mainly used in construction, and exposure has been considered a risk factor for SSc since 1980 [45], although only a few studies have examined the association. For this review, we analysed two case-control studies [16, 19] and one meta-analysis [27]. Diot et al. [16] published a case-control study involving 80 SSc patients, 6 of whom had been exposed to epoxy resins, with an overall OR of 4.24 (95% CI 1.03–17.44). Marie et al. [19] reported only one case of exposure to epoxy resins, failing to find a significant association with SSc, and with an OR of 3.03 (95% CI 0.02–12.6). Rubio et al. [27] reported the first meta-analysis on the association between SSc and epoxy resin exposure. They considered four case-control studies and found a significant overall association, with an overall OR of 2.97 (95% CI 2.31–3.83), an OR for women of 1 (95%CI 0.02–12.72) and an OR for men of 2.92 (95% CI 2.26–3.78). Figure 4 summarises these results.

Figure 4 Results of studies about systemic sclerosis and epoxy resins. CI = confidence interval
Welding activities generate fumes that are a complex mixture of potentially harmful particles and gases. The composition of welding fumes may include a variety of metal compounds (e.g., iron, chrome aluminium, arsenic, beryllium, lead and manganese) and gases (argon, nitrogen, carbon dioxide, carbon monoxide and hydrogen fluoride gases). In the last 20 years, four case-control studies [16, 18, 19, 37] and one meta-analysis [27] have investigated the association between welding fumes exposure and SSc. Among the case-control studies, only two found significant results. Using 80 cases and 160 controls, Diot et al. [16] calculated an OR of 3.74 (95% CI 1.06–13.18) and more recently, with 100 cases and 300 controls, Marie et al. [19] calculated an OR of 2.60 (95% CI 1.15–5.81).
In 2017, Rubio et al. [27] examined the same four studies in a meta-analysis, reporting an overall nonsignificant OR of 1.02 (95% CI 0.78–1.78), a significant OR for men of 5.87 (95% CI 2.26–3.78) and a nonsignificant OR for women of 1.52 (95% CI 0.36–6.49). These results, summarised in figure 5, suggest a potential association between exposure to welding fumes and SSc among men.

Figure 5 Results of studies about systemic sclerosis and welding fumes. CI = confidence interval
Several other occupational chemical exposures, such as pesticides, have also been suspected to induce SSc. In the last 20 years, however, two case-control studies failed to find a significant association [18, 19, 27]. Based on these studies, and a third older case-control study, a recent meta-analysis [27] did not find a significant association, with an OR of 1.02 (95% CI 0.78–1.32). A few studies have also analysed the link between hair dyes and SSc, but without significant results [18, 19, 27].
Vinyl chloride disease and toxic oil syndrome have many clinical similarities to SSc [10, 27, 46–48], but because of their important clinical and biological differences, they should be considered more as SSc-like disorders [27].
Occupational chemical exposures were not alone in being suspected of inducing SSc. Indeed, hand-transmitted vibration is associated with an increase in the signs and symptoms of neurological and vascular disorders [49, 50]. The Raynaud phenomenon is, for example, a symptom associated with hand-arm vibration exposure [50] and it is often one of the first clinical manifestations of SSc [3]. However, the possible relationship between hand vibration exposure and SSc is still being discussed. A recent review published by Wang et al. [49] combined the data from five studies with nonsignificant results and obtained a nonsignificant OR of 2.4 (95% CI 0.4–14.0).
The diagnosis of a disease’s occupational origin can be a challenge for the physicians in charge of follow-up care. Indeed, establishing an occupational history is time-consuming, and requires specialised knowledge and skills in occupational medicine. Even with these skills and knowledge, it is hard to interpret individual cases in the light of the literature alone and to decide whether those cases meet the criteria for recognition as an occupational disease. To help physicians detect which patients with SSc could have undergone significant occupational exposure (silica and solvents), we have established a list of red flags. The questions about silica exposure come from a standard questionnaire used for the diagnosis of occupational pulmonary diseases [51] and the questions about solvent exposure were identified in the various cases of occupational exposure considered in the studies [18, 19, 36] described in the present article. Table 2 summarises these questions.
Table 2 Red flags for physicians attempting to determine exposure to solvents or silica.
| Exposure to silica | Have you worked in construction or stonework? (masonry work, bricklaying, tiling, cement making, demolition, tunnel, shaft and gallery construction, mining, quarrying, slate work, stone cutting) |
| Have you worked as a dental technician? (manufacturing dental prostheses or implants) | |
| Have you worked with refractory materials in the glass, porcelain, faience, pottery, rubber, or ceramics industries or in a foundry? | |
| Have you worked with silica to produce abrasive materials or used angle grinders containing silica? | |
| Exposure to solvents | Have you worked in construction or the repair of ships, aircraft, or motor vehicles? |
| Have you worked in the production or use of paints, cement, adhesives, dyes, inks, varnishes, or chemicals containing toluene and xylene? | |
| Have you worked in metallurgy? | |
| Have you worked in the watchmaking industry? | |
| Have you worked in the petrochemical industry or chemical industry? | |
| Have you worked in leather, shoe, or imitation leather manufacturing? | |
| Have you worked in the manufacturing of refined oils or essential oils? | |
| Have you worked in the printing industry? | |
| Have you worked in the laundry, dyeing, or cleaning industry? | |
| Have you worked in the production of plastics, tyres, rubber, or electronic components? | |
| Have you worked in the production or extraction of solvents? |
Switzerland’s occupational disease recognition system is founded on a law and ordinance that together define a list of occupational exposures and resultant diseases that are eligible for recognition. If the patient’s exposure or disease is included in this list, recognition is possible if this disease can be proven to have been caused predominantly by the pursuit of an occupational activity. In other cases, where exposures or diseases are not on the recognised list, the disease must be proven to have been caused wholly, or clearly predominantly, in the pursuit of an occupational activity. SUVA has issued recommendations on the interpretation of the law for multifactorial diseases. An occupational exposure will be accepted as the predominant cause or the overwhelming cause of the disease if the scientific literature demonstrates that its attributable fraction of risk is above 50% (the RR in the literature is >2) or 75% (RR >4), respectively. This result came from the attributable fraction estimated by Miettinnen [52]. Occupational diseases, therefore, must be distinctly or uniquely linked to a particular type of workplace exposure.
These criteria are used by SUVA’s occupational medicine department to make decisions on injured or sick workers insured with them, or when private insurance companies seek their advice. There are multiple benefits for patients whose diseases are recognised as being of occupational origin. First, medical care or treatment will be paid for entirely by the insurance company (SUVA or private insurance companies) with no extra financial cost to the patient. They will also benefit from further measures, such as insurance pensions for a maximum of 3 years, if their disease prevents them from working. The general impact of disease recognition in terms of visibility, disease prevention, and employee protection is also very important. When a particular substance is recognised as being related to an occupational disease, there is greater incentive to find an alternative substance or to implement a regulatory measure to reduce workers’ exposure.
Currently systemic sclerosis is not on the list of recognised occupational diseases in Switzerland. Silica exposure is the most commonly discussed risk in the literature, yet it is not even on the accident insurance ordinance’s list of occupational exposures. Despite the significant associations found in case-control studies, SUVA’s criterion for recognition (the OR has to be >4) is only met when cohort studies are considered. Given that silica is associated with several different diseases including silicosis, lung cancer and rheumatoid arthritis [13, 53], it is surprising that silica itself is not on the list of occupational exposure substances. It is also important to point out that according to SUVA’s factsheet [53], Erasmus syndrome – described as an association between silicosis and systemic sclerosis or an association between silicosis and mixed connective tissue disease – is considered an occupational disease. In light of all these elements, we suggest that SSc should be recognised as an occupational disease in any context involving exposure to silica, even in the absence of silicosis. Although accident insurers may suggest changes to the list, it is ultimately the Federal Council that makes the final decision. However, the exposure threshold, in terms of duration and quantity, and the latency for the development of systemic sclerosis are not yet accurately known.
Several organic solvents can be found on the occupational exposures list. The overall OR for organic solvent exposure varied between 2.01 and 2.91, depending on the meta-analysis [27, 38–41], and reached 5.28 for men in the recent meta-analysis by Zhao et al. [41]. However, nearly all of these results concerned case-reports alone. Following the subgroup analysis carried out by Zhao et al. [41], a significant association with an OR >2 was considered for trichloroethylene, which is on the list. Zhao et al. [41] also reported a significant association between SSc and ketones, with an OR >4. Consequently, SSc following a significant exposure to one of these solvents could also be eligible for recognition, especially for men. Results for the other solvents are currently not sufficient proof for recognition; thus, it will be necessary to continue research in this field to produce more subgroup analyses and to better evaluate for specific solvents. It could also be interesting to launch cohort studies to strengthen evidence of the causal link between solvents and systemic sclerosis and to assess exposure thresholds and disease latency.
Epoxy resins are also on the list of occupational exposures, and the most recent meta-analysis [27] calculated an OR >2, a result that could enable recognition of SSc induced by epoxy resin exposure as an occupational disease. However, the data are based only on case-control studies and the number of cases is still low. More results are therefore needed before a definite conclusion can be drawn.
Welding fumes are not currently on the list of recognised exposures. In the latest meta-analysis [27], the overall OR was <4, although with an OR for men of >5 it could be eligible for recognition as an occupational disease. However, as with epoxy resins, there are only a few case-control studies, and more studies are needed. Table 3 summarises the different occupational risks eligible for recognition.
Table 3 Odds ratios for main occupational exposure implied in systemic sclerosis in Rubio et al. [27] and the possibility of recognition.
| Type of exposure | Overall OR (95% CI) | OR for women (95% CI) | OR for men (95% CI) | Included in the ordinance | Possibility of recognition as an occupational disease |
|---|---|---|---|---|---|
| Silica | 2.81 (1.86–4.23) | 2.10 (1.24–3.55) | 3.06 (1.90–4.91) | No | Recognition (see Discussion) |
| Solvents | 2.00 (1.32–3.02) | 2.01 (1.66–2.44) | 2.40 (1.44–4.01) | Yes | Recognition |
| Epoxy resins | 2.97 (2.31–3.83) | 1 (0.02–12.72) | 2.92 (2.26–3.78) | Yes | More data needed |
| Pesticides | 1.02 (0.78–1.32) | 3.06 (0.22–43.34) | 1.02 (0.79–1.33) | No | More data needed |
| Welding fumes | 1.29 (0.44–3.74) | 1.52 (0.36–6.49) | 5.87 (2.49–13.86) | No | More data needed |
CI = confidence interval; OR = odds ratio
It seems important to highlight that for the exposures considered in this article, with the exception of pesticides, that although SSc is more prevalent among women, the ORs are higher among men. This constitutes a prime argument to strengthen referrals to the Swiss National Accident Insurance Fund when men are affected.
Finally, among the five patients who came for a consultation at the IST, four were considered eligible for recognition owing to their exposure to silica, solvents or both, and two of them were given positive answers from SUVA, both for exposure to solvents. None of the patients exposed to silica alone obtained recognition for an occupational disease, despite the arguments of IST’s occupational physicians.
We did not perform a systematic literature review, nor did we perform a quality analysis and classification of the articles selected. We limited ourselves to articles published over the last 20 years and this choice could be criticised as occupational exposure’s potential role in systemic sclerosis was first described in 1914 [14]. Most of the studies included are retrospective and can lack detailed exposure information. Moreover, it remains very difficult to assess exposure levels and to define thresholds, in either time or quantity of exposure. It is also difficult to establish latency between initial exposure and the first symptoms of the disease. Systemic sclerosis is a rare disease, and positive associations have been established mainly in case-control studies with only a few cohort studies. This makes a causal link between SSc and some less frequently reported exposure scenarios (e.g., with epoxy resins or welding fumes) difficult to prove.
The recent literature has found strong associations between occupational exposure to silica and solvents and the development of systemic sclerosis. We believe that physicians should suggest that patients with proven occupational exposure to relevant contaminants should declare systemic sclerosis as an occupational disease to their health insurance company and to the Swiss National Accident Insurance Fund. Thus it is essential for physicians to screen patients with SSc for relevant exposure, for several reasons: first, physicians should consider the potential insurance benefits that recognition would bring the patient, and second, screening can help to identify cases where patients suffering from scleroderma should be assigned a safer workstation or job. Our list of red flags could be used during a consultation for SSc to identify those patients who should make an occupational accident declaration to their insurance company and perhaps be referred for an occupational disease consultation. The question of exposure thresholds and latency will probably be important avenues for future research and will hopefully be addressed in upcoming publications. However, we conclude that updating Switzerland’s list of occupational diseases and exposures seems entirely justified with regard to the recognition of systemic sclerosis as an occupational disease for patients with proven occupational exposure to silica.
We thank all the patients who made this publication possible. We also thank Dr Victor Dorribo, Dr Patricia Mosset, Dr Vanessa Oracion, Dr Jacques Pralong, and Dr Gaetan Rivier, who conducted some of the patient interviews. We are also grateful to the team of hygienists who carried out the workplace visits or simulations, to Mr Darren Hart who assisted with translation and to Hedi Radhouane who helped finalise the figures.
The authors report no financial support and no potential conflicts of interest relevant to this article.
1 D’Cruz D . Autoimmune diseases associated with drugs, chemicals and environmental factors. Toxicol Lett. 2000;112-113:421–32. doi:.https://doi.org/10.1016/S0378-4274(99)00220-9
2 Barnes J , Mayes MD . Epidemiology of systemic sclerosis: incidence, prevalence, survival, risk factors, malignancy, and environmental triggers. Curr Opin Rheumatol. 2012;24(2):165–70. doi:.https://doi.org/10.1097/BOR.0b013e32834ff2e8
3 Gabrielli A , Avvedimento EV , Krieg T . Scleroderma. N Engl J Med. 2009;360(19):1989–2003. doi:.https://doi.org/10.1056/NEJMra0806188
4 Denton CP , Khanna D . Systemic sclerosis. Lancet. 2017;390(10103):1685–99. doi:.https://doi.org/10.1016/S0140-6736(17)30933-9
5 van den Hoogen F , Khanna D , Fransen J , Johnson SR , Baron M , Tyndall A , et al. 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League against Rheumatism collaborative initiative. Arthritis Rheum. 2013;65(11):2737–47. doi:.https://doi.org/10.1002/art.38098
6 Tsou PS , Sawalha AH . Unfolding the pathogenesis of scleroderma through genomics and epigenomics. J Autoimmun. 2017;83:73–94. doi:.https://doi.org/10.1016/j.jaut.2017.05.004
7 De Martinis M , Ciccarelli F , Sirufo MM , Ginaldi L . An overview of environmental risk factors in systemic sclerosis. Expert Rev Clin Immunol. 2016;12(4):465–78. doi:.https://doi.org/10.1586/1744666X.2016.1125782
8 Marie I , Gehanno JF . Environmental risk factors of systemic sclerosis. Semin Immunopathol. 2015;37(5):463–73. doi:.https://doi.org/10.1007/s00281-015-0507-3
9 Miller FW , Alfredsson L , Costenbader KH , Kamen DL , Nelson LM , Norris JM , et al. Epidemiology of environmental exposures and human autoimmune diseases: findings from a National Institute of Environmental Health Sciences Expert Panel Workshop. J Autoimmun. 2012;39(4):259–71. doi:.https://doi.org/10.1016/j.jaut.2012.05.002
10 Mora GF . Systemic sclerosis: environmental factors. J Rheumatol. 2009;36(11):2383–96. doi:.https://doi.org/10.3899/jrheum.090207
11International Labour Organization. ILO List of Occupational Diseases (revised 2010). Geneva, Switzerland: ILO; 2010. p. 8.
12Industrial Injuries Advisory Council. Position paper 42: Occupational exposure to crystalline silica and its relation to connective tissue diseases. London, UK: IIAC; 2018. p. 32.
13INRS (Institut national de recherche et de sécurité). Tableaux des maladies professionnelles Régime général tableau 25: Affections dues à la silice cristalline, aux silicates cristallins, au graphite ou à la houille. 2018 [accessed 2018 July 18]; Available from: http://www.inrs.fr/publications/bdd/mp/tableau.html?refINRS=RG%2025.
14 Bramwell B . Diffuse scleroderma: its frequency; its occurrence in stonemasons; its treatment by fibrolysin—elevations of temperature due to fibrolysin injections. Edinburgh Med J. 1914;12:387–401.
15 Bovenzi M , Barbone F , Pisa FE , Betta A , Romeo L , Tonello A , et al. A case-control study of occupational exposures and systemic sclerosis. Int Arch Occup Environ Health. 2004;77(1):10–6. doi:.https://doi.org/10.1007/s00420-003-0462-5
16 Diot E , Lesire V , Guilmot JL , Metzger MD , Pilore R , Rogier S , et al. Systemic sclerosis and occupational risk factors: a case-control study. Occup Environ Med. 2002;59(8):545–9. doi:.https://doi.org/10.1136/oem.59.8.545
17 Englert H , Small-McMahon J , Davis K , O’Connor H , Chambers P , Brooks P . Male systemic sclerosis and occupational silica exposure-a population-based study. Aust N Z J Med. 2000;30(2):215–20. doi:.https://doi.org/10.1111/j.1445-5994.2000.tb00810.x
18 Maître A , Hours M , Bonneterre V , Arnaud J , Arslan MT , Carpentier P , et al. Systemic sclerosis and occupational risk factors: role of solvents and cleaning products. J Rheumatol. 2004;31(12):2395–401.
19 Marie I , Gehanno JF , Bubenheim M , Duval-Modeste AB , Joly P , Dominique S , et al. Prospective study to evaluate the association between systemic sclerosis and occupational exposure and review of the literature. Autoimmun Rev. 2014;13(2):151–6. doi:.https://doi.org/10.1016/j.autrev.2013.10.002
20 Thompson AE , Pope JE . Increased prevalence of scleroderma in southwestern Ontario: a cluster analysis. J Rheumatol. 2002;29(9):1867–73.
21 Zachariae H , Bjerring P , Søndergaard KH , Halkier-Sørensen L . [Occupational systemic sclerosis in men]. Ugeskr Laeger. 1997;159(18):2687–9. Article in Danish.
22 Ziegler V , Enderlein G , Mehlhorn J , Conrad K . Retrospective epidemiological analysis of the relation between progressive systemic scleroderma and the exposure to quartz dust out of uranium ore mining in East Germany. Zentralbl Arbeitsmed. 1997;47:7–13.
23 Brown LM , Gridley G , Olsen JH , Mellemkjaer L , Linet MS , Fraumeni JF, Jr . Cancer risk and mortality patterns among silicotic men in Sweden and Denmark. J Occup Environ Med. 1997;39(7):633–8. doi:.https://doi.org/10.1097/00043764-199707000-00008
24 Makol A , Reilly MJ , Rosenman KD . Prevalence of connective tissue disease in silicosis (1985-2006)-a report from the state of Michigan surveillance system for silicosis. Am J Ind Med. 2011;54(4):255–62. doi:.https://doi.org/10.1002/ajim.20917
25 Mehlhorn J , Enderlein G , Conrad K , Ziegler V . Analysis for the association between progressive systemic scleroderma exposure to quartz dust and silicosis in East German uranium mining. Zentralbl Arbeitsmed. 1999;49:134–47.
26 Rosenman KD , Moore-Fuller M , Reilly MJ . Connective tissue disease and silicosis. Am J Ind Med. 1999;35(4):375–81. doi:.https://doi.org/10.1002/(SICI)1097-0274(199904)35:4<375::AID-AJIM8>3.0.CO;2-I
27 Rubio-Rivas M , Moreno R , Corbella X . Occupational and environmental scleroderma. Systematic review and meta-analysis. Clin Rheumatol. 2017;36(3):569–82. doi:.https://doi.org/10.1007/s10067-016-3533-1
28 McCormic ZD , Khuder SS , Aryal BK , Ames AL , Khuder SA . Occupational silica exposure as a risk factor for scleroderma: a meta-analysis. Int Arch Occup Environ Health. 2010;83(7):763–9. doi:.https://doi.org/10.1007/s00420-009-0505-7
29 Dospinescu P , Jones GT , Basu N . Environmental risk factors in systemic sclerosis. Curr Opin Rheumatol. 2013;25(2):179–83. doi:.https://doi.org/10.1097/BOR.0b013e32835cfc2d
30 Freire M , Alonso M , Rivera A , Sousa A , Soto A , Gómez-Sousa JM , et al. Clinical peculiarities of patients with scleroderma exposed to silica: A systematic review of the literature. Semin Arthritis Rheum. 2015;45(3):294–300. doi:.https://doi.org/10.1016/j.semarthrit.2015.06.004
31 Clerc F , Bertrand N , Vincent R . TEXAS: a Tool for EXposure ASsessment-Statistical models for estimating occupational exposure to chemical agents. Ann Occup Hyg. 2015;59(3):277–91.
32 Reinl W . [Scleroderma caused by trichloroethylene effects]. Zentralbl Arbeitsmed. 1957;7(3):58–60. Article in German.
33 Nietert PJ , Sutherland SE , Silver RM , Pandey JP , Knapp RG , Hoel DG , et al. Is occupational organic solvent exposure a risk factor for scleroderma? Arthritis Rheum. 1998;41(6):1111–8. doi:.https://doi.org/10.1002/1529-0131(199806)41:6<1111::AID-ART19>3.0.CO;2-J
34 Czirják L , Kumánovics G . Exposure to solvents in female patients with scleroderma. Clin Rheumatol. 2002;21(2):114–8. doi:.https://doi.org/10.1007/PL00011216
35 Arnaud J . Sclérodermie et facteurs professionnels et de l’environnement: études cas-témoins à partir d’interrogatoires individuels. Arch Mal Prof. 2002;63:144.
36 Garabrant DH , Lacey JV, Jr , Laing TJ , Gillespie BW , Mayes MD , Cooper BC , et al. Scleroderma and solvent exposure among women. Am J Epidemiol. 2003;157(6):493–500. doi:.https://doi.org/10.1093/aje/kwf223
37 Kütting B , Uter W , Drexler H . Is occupational exposure to solvents associated with an increased risk for developing systemic scleroderma? J Occup Med Toxicol. 2006;1(1):15. doi:.https://doi.org/10.1186/1745-6673-1-15
38 Aryal BK , Khuder SA , Schaub EA . Meta-analysis of systemic sclerosis and exposure to solvents. Am J Ind Med. 2001;40(3):271–4. doi:.https://doi.org/10.1002/ajim.1098
39 Kettaneh A , Al Moufti O , Tiev KP , Chayet C , Tolédano C , Fabre B , et al. Occupational exposure to solvents and gender-related risk of systemic sclerosis: a metaanalysis of case-control studies. J Rheumatol. 2007;34(1):97–103.
40 Barragán-Martínez C , Speck-Hernández CA , Montoya-Ortiz G , Mantilla RD , Anaya JM , Rojas-Villarraga A . Organic solvents as risk factor for autoimmune diseases: a systematic review and meta-analysis. PLoS One. 2012;7(12):e51506. doi:.https://doi.org/10.1371/journal.pone.0051506
41 Zhao JH , Duan Y , Wang YJ , Huang XL , Yang GJ , Wang J . The Influence of Different Solvents on Systemic Sclerosis: An Updated Meta-analysis of 14 Case-Control Studies. J Clin Rheumatol. 2016;22(5):253–9. doi:.https://doi.org/10.1097/RHU.0000000000000354
42 Marie I , Menard JF , Duval-Modeste AB , Joly P , Dominique S , Bravard P , et al. Association of occupational exposure with features of systemic sclerosis. J Am Acad Dermatol. 2015;72(3):456–64. doi:.https://doi.org/10.1016/j.jaad.2014.11.027
43 Wang G , Wang J , Ansari GAS , Khan MF . Autoimmune potential of perchloroethylene: Role of lipid-derived aldehydes. Toxicol Appl Pharmacol. 2017;333:76–83. doi:.https://doi.org/10.1016/j.taap.2017.08.009
44 Cooper GS , Makris SL , Nietert PJ , Jinot J . Evidence of autoimmune-related effects of trichloroethylene exposure from studies in mice and humans. Environ Health Perspect. 2009;117(5):696–702. doi:.https://doi.org/10.1289/ehp.11782
45 Yamakage A , Ishikawa H , Saito Y , Hattori A . Occupational scleroderma-like disorder occurring in men engaged in the polymerization of epoxy resins. Dermatologica. 1980;161(1):33–44. doi:.https://doi.org/10.1159/000250328
46 Marie I . Sclérodermie systémique et exposition professionnelle : vers une extension de la reconnaissance de maladie professionnelle en 2014? [Systemic sclerosis and occupational exposure: towards an extension of legal recognition as occupational disorder in 2014?]. Rev Med Interne. 2014;35(10):631–5. Article in French. doi:.https://doi.org/10.1016/j.revmed.2014.04.002
47 Granel B , Zemour F , Lehucher-Michel MP , Moulin P , Disdier P , Durand JM , et al. Évaluation de l’exposition toxique professionnelle de patients atteints de sclérodermie systémique. Revue de la littérature et résultat d’un auto-questionnaire [Occupational exposure and systemic sclerosis. Literature review and result of a self-reported questionnaire]. Rev Med Interne. 2008;29(11):891–900. Article in French. doi:.https://doi.org/10.1016/j.revmed.2008.03.013
48 Magnant J , Diot E . Sclérodermie systémique: épidémiologie et facteurs environnementaux [Systemic sclerosis: epidemiology and environmental factors]. Presse Med. 2006;35(12 Pt 2):1894–901. Article in French. doi:.https://doi.org/10.1016/S0755-4982(06)74923-5
49 Wang YJ , Huang XL , Yan JW , Wan YN , Wang BX , Tao JH , et al. The association between vibration and vascular injury in rheumatic diseases: a review of the literature. Autoimmunity. 2015;48(1):61–8. doi:.https://doi.org/10.3109/08916934.2014.947477
50 Nilsson T , Wahlström J , Burström L . Hand-arm vibration and the risk of vascular and neurological diseases-A systematic review and meta-analysis. PLoS One. 2017;12(7):e0180795. doi:.https://doi.org/10.1371/journal.pone.0180795
51SPLF-SFMT. Questionnaire de repérage des expositions professionnelles: Chez les sujets atteints de cancer bronchiques primaires. Dossier Santé au travail. 2009 [cited 2018 September 18]. Available from: http://splf.fr/wp-content/uploads/2014/08/eDossier-sante-2.df.
52 Miettinen OS . Proportion of disease caused or prevented by a given exposure, trait or intervention. Am J Epidemiol. 1974;99(5):325–32. doi:.https://doi.org/10.1093/oxfordjournals.aje.a121617
53Stöhr S, Jost M. Factsheet Siliose. Lucerne, Switzerland: SUVA; 2012.
The authors report no financial support and no potential conflicts of interest relevant to this article.