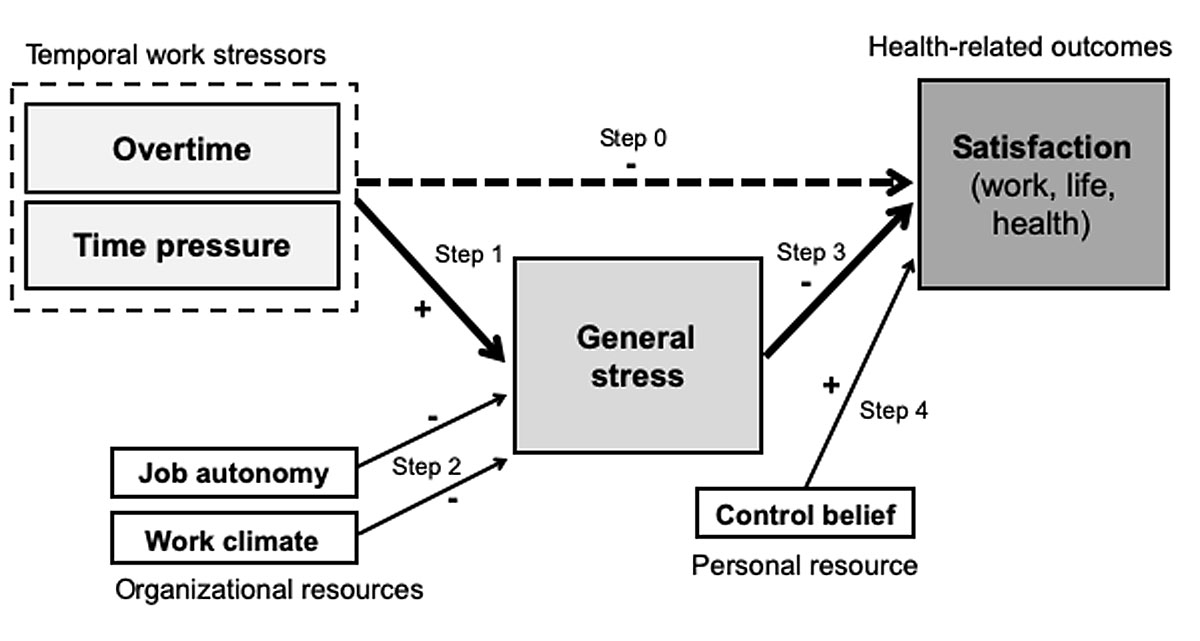
Figure 1 Explanatory model for the prediction of health and well-being among health professionals.
DOI: https://doi.org/10.4414/smw.2020.20175
Working conditions in hospitals are often characterised as stressful and detrimental to health [1, 2]. In addition to stress, which is prevalent in health professions, general working conditions also have a considerable impact on employees’ job satisfaction. Health professionals are exposed to a number of physical and psychological stresses and strains [3]. Challenges are diverse and involve physical demands (e.g., heavy lifting, standing or sitting for long periods) [4], rotating in shift work [5–7], high responsibility, and frequent interruptions and disturbances at work [8, 9]. Other challenges include role ambiguity [10], patients’ concerns and expectations [11, 12], and experiences of violence or other social conflicts at work [13]. Importantly, the limited time available for interacting with patients who suffer from multiple chronic conditions (multimorbidity) is one of the key issues [14]. A recent Swiss study documented how internal medicine residents spend their time at work and found high work compression: for every hour the residents interacted with patients, they spent an average of 5 hours on other tasks [15]. About half the workday was spent using a computer. Another study reported that physicians are constantly exposed to high time pressure, with additional stress due to overtime [16]. Another problem is that these burdens on health professionals can lead to negative consequences that compound the existing time pressure. Physicians frequently report sleep problems (sleep deprivation and fragmentation) [17], which arise from a set of work demands, such as umpteen night or weekend shifts, irregular and long extra hours, and research activities during leisure time. Some researchers also refer to physicians’ fatigue [18, 19], which has potential negative consequences on resident health, safety, well-being or patient care [17].
Shortage of personnel and the increasing lack of qualified health professionals (young talents vs leaving the profession) are well-known problems. The European NEXT study in which 10 EU countries took part investigated the causes of early retirement from the nursing profession. The study found a clear link between unfavourable working conditions and intended retirement [20]. A survey estimated the proportion of physicians (Swiss medical graduates of the diploma years 1980 to 2009) who had left patient care to be almost 13% [21]. For physicians who changed professions before becoming specialists, workload demands were the most reported reason for leaving [21]. Women left patient care more frequently and earlier than their male colleagues as a result of a higher work-life imbalance.
Work-related stressors and buffering resources make up the framework conditions that can have a positive and/or negative impact on the health of the working population. A recent meta-analysis showed the relationship between long working hours and impact on health. The risk of stroke (33%) was increased for long working hours (significant for 55 hours per week and longer) compared with normal working hours [22]. The longer the working week, the stronger the association was. Behavioural risk factors such as lack of exercise or unhealthy living conditions (e.g., smoking, alcohol) were discussed as confounders [23]. Long and maximum working hours often allow little to almost no time for other activities that take place outside work in life. Increasingly, there has been a change and a demand for a better balance between work, leisure and family life [24]. Acute or chronic stress results when there is an imbalance between stressors, resources and coping strategies. Based on the job demand-control model of the American sociologist Robert Karasek, it is assumed that a high job strain is the result of high job demands on the one hand and limited job autonomy on the other [25]. In addition to this concept, the job demands-resources model proposes that working conditions should be categorised into demands and resources [26]. Accordingly, health-promoting resources at the workplace, such as high job autonomy, a good working atmosphere and collegiality, should counter given pressures [27, 28]. Moreover, personality characteristics are of growing research interest. Some authors consider control beliefs as a relevant resource for stress management [29]. The psychosocial construct of control belief was developed by Rotter [30] in the 1960s as characteristic of an individual’s learned expectations.
The improvement of working conditions or rather the reduction of certain workloads should be systematically researched [1, 31, 32], especially regarding health professionals’ satisfaction with life and individual health beyond work. Working conditions relevant for the health and well-being of hospital employees have been investigated in the Swiss survey “Work and Health in Hospital”; burnout [33], informal caregiving and other work-privacy conflicts were examined in preceding studies of that survey [34, 35].
This study aimed to assess the impact of temporal work stressors (overtime, time pressure) on the health and well-being of health professionals (satisfaction with work, life and health). We investigated whether general stress mediates this relationship and whether organisational (job autonomy, work climate) and personal resources (control belief) diminish the consequences of such stressors on work, life and health satisfaction.
The following research questions were addressed:
Cross-sectional data from an employee survey (conducted in 2015/16) on working conditions and health among hospital employees in German-speaking Switzerland (n = 1840) were used. The study population was restricted to 1232 health professionals with information on all variables of interest. Overall, the response rate was slightly over 40%. The anonymous questionnaire contained 100 questions concerning different work, health or life domains (e.g., working conditions, personal resources, health and well-being). The data were from five hospitals, including one university hospital, one cantonal hospital, one district hospital and two rehabilitation clinics. Hospitals varied in size from around 480 to 2200 employees. Survey participation was voluntary and anonymous. This completely anonymous survey required no ethics approval. The survey data do not allow any conclusion about the identity of the respondents.
Measures of two different aspects of temporal workload were used as exposure variables: overtime and time pressure. Overtime was assessed by the self-reported number of extra hours worked during a standard week, ranging from 0 to 1–2, to 3–5, to 6–10 and to more than 10 extra hours per week. Time pressure was measured by a single Likert-scaled item: “Due to the heavy workload, there is often a lot of time pressure.” Survey respondents were asked to what extent they agreed or disagreed with the statement, with four suggested responses ranging from 0 (“completely disagree”) to 3 (“completely agree”).
For organisational resources, scales on job autonomy and work climate were used, which were taken from the Copenhagen Psychosocial Questionnaire (COPSOQ) by Kristensen, Hannerz, Høgh and Borg [36]. To assess job autonomy, a multiple-item measure was used. The scale contained eight questions (e.g., “Can you influence the amount of work assigned to you?”), with response options ranging from 0 to 4 (“never/almost never”, “seldom”, “sometimes”, “often”, “always”). Other items used were: being able to decide when to take a break, being able to decide with whom to work with or being able to take holidays more or less as wished, etc. Sum scores of 0 to 8 were classified as a “low”, 9–16 as a “moderate”, 17–24 as a “high”, and 25–32 as a “very high” level of job autonomy.
To measure work climate, six items on the self-rated working atmosphere with colleagues, feeling of being part of a collective, etc. were used, with response options ranging from 0 to 4 (“never/almost never”, “seldom”, “sometimes”, “often”, “always”). Sum scores of 0–12 were classified as a “poor”, 13–15 as a “moderate”, 16–18 as a “good”, and 19–24 as a “very good” work climate.
Control belief (internal locus of control) was assessed with the two items “I am in control of my life” and “If I make an effort, I will succeed” as used in the brief version of the IE-4 scale [37]. Response options ranged from 0 to 3 (“doesn't apply at all”, “applies somewhat”, “applies mostly”, “applies completely”).
The outcome variables used were general stress and satisfaction with work, life and health. General stress was indicated by answering the unspecified question [38]: “Stress describes a state in which a person feels strained, restless, nervous, anxious or unable to sleep at night because his or her thoughts are agitated. Do you currently experience this kind of stress, and to what extent?” Response options ranged from 0 to 4 (“feel no stress”, “feel minor stress”, “feel moderate stress”, “feel strong stress”, “feel very strong stress”).
Satisfaction with work, life and health in general was measured by a single question each: “How satisfied are you in general with your work/life/health?” Each question was rated on an 11-point response scale from 0 (“not satisfied at all”) to 10 (“completely satisfied”). The single question about satisfaction with work stems from the Swiss Health Survey (SHS) conducted in 2012 by the Swiss Federal Statistical Office [39]. The questions on satisfaction with health and life were available from the survey Statistics on Income and Living Conditions (SILC) [40].
Age (surveyed across five age groups: <25, 25–34, 35–44, 45–54, and 55+ years), gender, and job status were considered as control variables. Job status was measured as two categories: regular staff vs supervisory staff. The question was derived from the Swiss Household Panel (SHP), an ongoing longitudinal study in Switzerland [41].
For the statistical analyses, IBM SPSS Statistics (v. 25; SPSS Inc, Chicago, IL) was used. Data analyses were carried out for all health professionals and stratified for nurses and physicians. Descriptive statistics of all measures were generated. Dichotomous variables were dummy coded. Significance levels were reported. The job autonomy, work climate and control belief scales, with their sum scores ranging from 0–32 (job autonomy; eight items; Cronbach’s alpha 0.8), from 0–24 (work climate; six items; Cronbach’s alpha 0.6) and from 0–6 (internal locus of control; two items; Cronbach’s alpha 0.5), were used for more differentiated linear regression analyses. To compare the relative importance of each coefficient in the regression model, standardised beta coefficients were reported. The beta coefficient for a regression denotes the slope, that is, by how much the target variable (dependent variable) increases by an additional unit of the influencing variable (independent variable). If the beta coefficient is negative, the interpretation is that for every unit increase in the influencing variable (e.g., overtime), the independent variable (e.g., job satisfaction) will decrease by the beta coefficient value. In this context, standardised means that beta coefficients have standard deviations as their units (z-scores for comparability also in the case of different units of variables).
The association between temporal work stressors and general stress and satisfaction with work, life, and health as outcomes was assessed by using stepwise multiple linear regression analyses. Figure 1 presents the explanatory model underlying the hypothesised relationships.
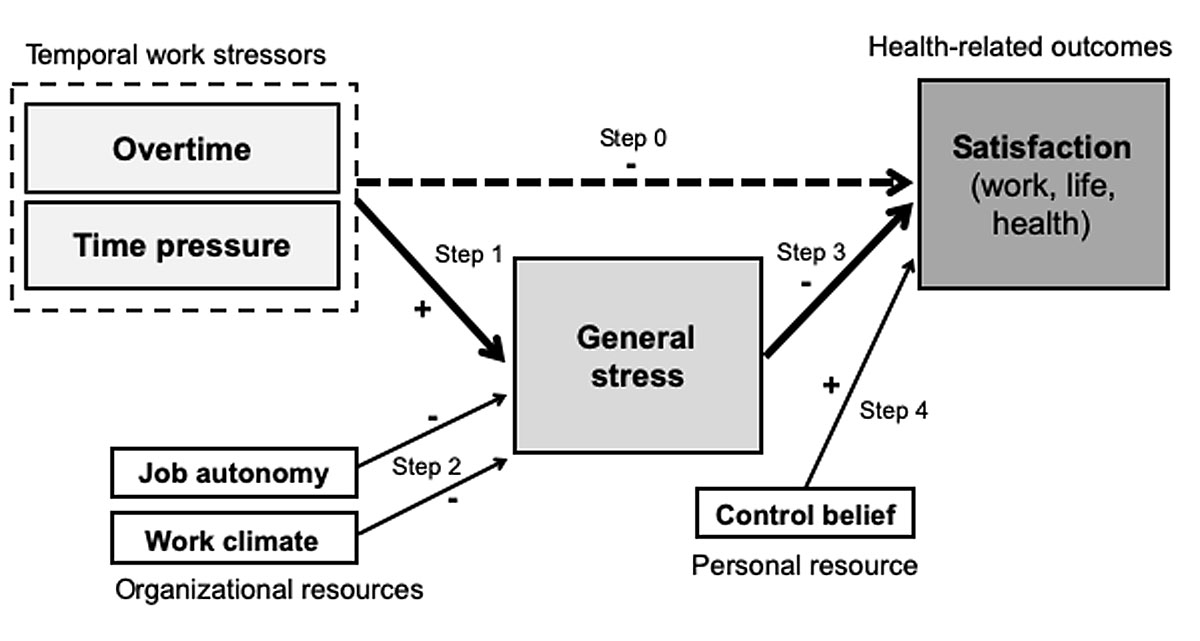
Figure 1 Explanatory model for the prediction of health and well-being among health professionals.
Step 0 estimated the relationship between overtime and time pressure (as independent or exposure variables) and satisfaction with work, life and health (as outcome variables). In step 1 of the regression analyses, the relationship between overtime and time pressure was estimated as independent or exposure variables and general stress as the dependent variable. Step 2 was analysis of the correlation between the variables job autonomy / work climate and general stress. This step was necessary to test whether the organisational resources can buffer the potential negative effects of the temporal work stressors on general stress. Next (in step 3), general stress was included as exposure variable to investigate the extent to which general stress is associated with the satisfaction outcomes. In step 4, control belief was included to test whether it is a personal resource with regard to satisfaction and the other variables in the model. In all steps, age, gender and job status were controlled for. By performing this five-step regression analyses it was possible to test for general stress as a potential mediator in this association. Mediation analyses followed the approach by Baron and Kenny [42]. A mediator variable is a variable that is related to both the independent and the dependent variable. To support mediation, the following conditions must be met (with overtime and time pressure as the two independent variables):
Mediation is described as complete if the prediction of the independent variable is no longer significant after inclusion of the mediator in the regression model. Partial mediation has to be considered if the effect on the dependent variable is only reduced.
The majority of the final study sample (table 1) were health professionals including nurses (57%), physicians (18%), and therapists, midwives, medical or technical personnel (24%). At the time of the survey, 66% of the physicians and 55% of the nursing professionals were between 25 and 44 years old. Almost 35% of the physicians interviewed were male. Nurses were predominantly female (more than 90%). Higher occupational positions were found in 59% of the physicians and 18% of the nursing professionals.
Table 1 Demographic characteristics of all health professionals and among nurses and physicians.
|
Nurses
(n = 705) |
Physicians
(n = 222) |
All health professionals
(n = 1232) |
||
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Age groups, years | <25 | 72 (10.2) | 2 (0.9) | 81 (6.6) |
| 25–34 | 214 (30.4) | 72 (32.7) | 400 (32.6) | |
| 35–44 | 171 (24.3) | 74 (33.6) | 326 (26.5) | |
| 45–54 | 162 (23.0) | 45 (20.5) | 273 (22.2) | |
| 55+ | 85 (12.1) | 27 (12.3) | 148 (12.1) | |
| Gender | Female | 662 (94.4) | 145 (65.3) | 1071 (87.2) |
| Male | 39 (5.6) | 77 (34.7) | 157 (12.8) | |
| Job status | Ordinary employees (regular staff) | 573 (81.5) | 90 (40.9) | 893 (73.0) |
| Superiors, managers (supervisory staff) | 130 (18.5) | 130 (59.1) | 330 (27.0) | |
Regular overtime of 6 and more hours per week was reported by almost one third of the interviewed physicians (table 2). Usually no overtime was reported by approximately 37% of the nurses and less than 19% of all physicians. Time pressure was reported by 86% of physicians and 79% of the nurses. As expected, high levels of job autonomy were significantly more frequently reported by physicians (nearly 40%) than by nurses (exactly 20%). Work climate was largely classified as good or very good by about four fifths of the study sample. Internal control beliefs were expressed by the majority of the health professionals. Overall, 19% of the physicians and 14% of the nurses reported a very high level of general stress. Less than 20% of all health professionals mentioned no general stress. Satisfaction with life was rated similarly by the respective groups, whereas satisfaction with health was rated as lower by nurses.
Table 2 Temporal work stressors, organisational and personal resources, general stress and satisfaction among health professionals.
|
Nurses
(n = 705) |
Physicians
(n = 222) |
All health professionals
(n = 1232) |
||||
|---|---|---|---|---|---|---|
| Mean (SD) | n (%) | Mean (SD) | n (%) | Mean (SD) | n (%) | |
| Overtime hours | ||||||
| No regular overtime (0) | 256 (37.3) | 40 (18.5) | 396 (32.9) | |||
| 1–2 long hours/week (1) | 308 (44.8) | 51 (23.6) | 491 (40.8) | |||
| 3–5 long hours/week (2) | 104 (15.1) | 55 (25.5) | 207 (17.2) | |||
| 6+ long hours/week (3, 4) | 19 (2.8) | 70 (32.4) | 109 (9.1) | |||
| Time pressure | ||||||
| Fully disagree (0) | 2.0 (0.72) | 13 (1.9) | 2.1 (0.64) | 1 (0.5) | 2.0 (0.72) | 24 (2.0) |
| Disagree (1) | 135 (19.3) | 30 (13.7) | 256 (20.9) | |||
| Agree (2) | 380 (54.2) | 128 (58.4) | 660 (53.9) | |||
| Fully agree (3) | 173 (24.7) | 60 (27.4) | 284 (23.2) | |||
| Job autonomy | 12.4 (4.95) | 15.2 (5.81) | 14.0 (5.64) | |||
| Low (0–8) | 152 (22.1) | 28 (13.1) | 204 (17.0) | |||
| Moderate (9–16) | 398 (57.8) | 101 (47.4) | 620 (51.7) | |||
| High (17–24) | 126 (18.3) | 69 (32.4) | 323 (26.9) | |||
| Very high (25–32) | 12 (1.7) | 15 (7.0) | 52 (4.3) | |||
| Work climate | 18.2 (2.85) | 17.3 (3.18) | 17.8 (2.99) | |||
| Poor (0–12) | 22 (3.2) | 15 (6.9) | 50 (4.2) | |||
| Moderate (13–15) | 89 (12.9) | 40 (18.3) | 205 (17.0) | |||
| Good (16–18) | 254 (36.7) | 86 (39.4) | 443 (36.8) | |||
| Very good (19–24) | 327 (47.3) | 77 (35.3) | 506 (42.0) | |||
| General stress | 1.4 (0.97) | 1.6 (1.02) | 1.5 (0.99) | |||
| Never (0) | 126 (18.8) | 35 (16.3) | 213 (18.1) | |||
| Low (1) | 229 (34.2) | 71 (33.0) | 394 (33.4) | |||
| Medium (2) | 83 (33.5) | 69 (32.1) | 397 (33.7) | |||
| (Very) high (3, 4) | 7 (13.5) | 40 (18.6) | 175 (14.8) | |||
| Control belief (internal) | 4.4 (1.09) | 4.3 (1.20) | 4.4 (1.13) | |||
| Low (0–2) | 28 (4.0) | 13 (5.9) | 58 (4.8) | |||
| Moderate (3, 4) | 337 (48.2) | 124 (56.1) | 614 (50.3) | |||
| High (5, 6) | 334 (47.8) | 84 (38.0) | 549 (45.0) | |||
| Satisfaction with work | 7.6 (1.38) | 7.7 (1.52) | 7.6 (1.39) | |||
| Low (0–5) | 62 (8.8) | 23 (10.5) | 102 (8.3) | |||
| Medium (6–8) | 480 (68.1) | 130 (59.4) | 812 (66.1) | |||
| High (9, 10) | 163 (23.1) | 66 (30.1) | 315 (25.6) | |||
| Satisfaction with life | 7.7 (1.50) | 7.6 (1.53) | 7.7 (1.49) | |||
| Low (0–5) | 57 (8.1) | 18 (8.1) | 98 (8.0) | |||
| Medium (6–8) | 427 (60.6) | 140 (63.1) | 760 (61.7) | |||
| High (9, 10) | 221 (31.3) | 64 (28.8) | 373 (30.3) | |||
| Satisfaction with health | 7.2 (1.80) | 7.5 (1.69) | 7.3 (1.79) | |||
| Low (0–5) | 121 (17.2) | 29 (13.1) | 203 (16.5) | |||
| Medium (6–8) | 425 (60.3) | 128 (57.7) | 729 (59.2) | |||
| High (9, 10) | 159 (22.6) | 65 (29.3) | 299 (24.3) | |||
Due to missing values, percentages do not add up to 100.
As outlined, a multiple linear regression analysis was conducted. The results were tested for multicollinearity. The absolute value of Pearson’s correlation was close to 0.31 for the independent variables overtime and time pressure, indicating that collinearity is unlikely to exist.
As table 3 shows, temporal work stressors were found to strongly predict general stress symptoms among health professionals (β = 0.25) and particularly physicians (β = 0.30), independently of the observed stress-buffering effects of organisational resources such as job autonomy (β = −0.09) or work climate (β = −0.22). Overtime was not significantly related to physicians’ general stress, but high time pressure was (β = 0.37). The beta coefficient of 0.37 means that for each one-unit increase in the predictor variable (time pressure), the outcome variable (general stress) will increase by 0.37 units. Results further revealed that job autonomy was not a significant predictor for general stress in physicians. The data also showed that a better work climate in general was related to less general stress in all health professionals.
Table 3 Explaining general stress among health professionals - results of a stepwise multiple linear regression analysis (steps 1 and 2).
| Dependent or outcome variable |
General stress
(not at all to a very large extent 0–4) |
Nurses
(n = 705) |
Physicians
(n = 222) |
All health professionals
(n = 1232) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | Step 1 | Step 2 | Step 1 | Step 2 | ||||||||
| beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | ||
| Independent or exposure variables | Overtime hours (0–10+) | 0.15 | 0.000 | 0.13 | 0.001 | 0.06 | 0.402 | 0.02 | 0.740 | 0.14 | 0.000 | 0.11 | 0.000 |
| Time pressure (0–3) | 0.30 | 0.000 | 0.23 | 0.000 | 0.37 | 0.000 | 0.30 | 0.000 | 0.30 | 0.000 | 0.25 | 0.000 | |
| Intervening variables | Job autonomy (sum score 0–32) | – | −0.14 | 0.001 | – | −0.11 | 0.141 | – | −0.09 | 0.005 | |||
| Work climate (sum score 0-–4) | – | −0.19 | 0.000 | – | −0.27 | 0.000 | – | −0.22 | 0.000 | ||||
| Control variables | Gender (male) | −0.05 | 0.160 | −0.04 | 0.302 | −0.09 | 0.188 | −0.09 | 0.207 | −0.05 | 0.115 | −0.03 | 0.263 |
| Age (<25, 25–34, 35–44, 45–54, 55+) | 0.00 | 0.917 | −0.01 | 0.785 | −0.15 | 0.059 | −0.09 | 0.296 | −0.01 | 0.636 | −0.02 | 0.433 | |
| Job status (with supervisory position) | −0.07 | 0.084 | −0.01 | 0.740 | 0.18 | 0.026 | 0.14 | 0.086 | −0.03 | 0.294 | −0.01 | 0.808 | |
| Adjusted R square | 0.135 | 0.191 | 0.152 | 0.222 | 0.124 | 0.180 | |||||||
| No. cases in model | 642 | 622 | 202 | 194 | 1131 | 1091 | |||||||
Moreover, associations between temporal work stressors (predictors) and satisfaction with work, life, and health (outcomes) turned out to be mostly indirect, mediated by general stress (tables 4a–c ). General stress, in turn, was observed to (most) strongly predict domain-specific satisfaction (β = −0.17 to −0.34), sometimes only surpassed by resources such as work climate or internal control belief. Explained variance of the three satisfaction outcomes in the fully specified regression or explanatory models ranged between 14% and 45% depending on the (sub-)sample (nurses, physicians, all health professionals) or the outcome. Organisational resources (job autonomy and work climate) were found to have little to no buffering effect in relation to life satisfaction as an outcome, except in physicians (table 4b). Control belief was a strong and independent personal resource in particular for satisfaction of all health professionals with their life and health (table 4c) in general (β = 0.25/0.21).
Table 4a Explaining job satisfaction among health professionals – results of a stepwise multiple regression analysis (step 0, steps 3 and 4)
| Dependent or outcome variable |
Satisfaction with work
(0–10 rating scale, 10 = completely satisfied) |
Nurses
(n = 705) |
Physicians
(n = 222) |
All health professionals
(n = 1232) |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Step 0 | Step 3 | Step 4 | Step 0 | Step 3 | Step 4 | Step 0 | Step 3 | Step 4 | |||||||||||
| beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | ||
| Independent or exposure variables | Overtime hours (0–10+) | −0.08 | 0.041 | −0.01 | 0.775 | −0.02 | 0.665 | −0.18 | 0.010 | −0.09 | 0.168 | −0.09 | 0.168 | −0.11 | 0.001 | −0.04 | 0.171 | 0.05 | 0.105 |
| Time pressure (fully disagree to fully agree 0–3) | −0.27 | 0.000 | −0.13 | 0.001 | −0.13 | 0.001 | −0.24 | 0.000 | −0.06 | 0.339 | −0.06 | 0.340 | −0.24 | 0.000 | −0.10 | 0.001 | −0.10 | 0.001 | |
| Mediating or intervening variables | General stress (not at all to a very large extent 0–4) | – | −0.19 | 0.000 | −0.17 | 0.000 | – | −0.29 | 0.000 | −0.28 | 0.000 | – | −0.23 | 0.000 | −0.21 | 0.000 | |||
| Job autonomy (sum score 0–32) | – | 0.18 | 0.000 | 0.17 | 0.000 | – | 0.17 | 0.009 | 0.17 | 0.010 | – | 0.18 | 0.000 | 0.17 | 0.000 | ||||
| Work climate (sum score 0–24) | – | 0.30 | 0.000 | 0.28 | 0.000 | – | 0.36 | 0.000 | 0.34 | 0.000 | – | 0.28 | 0.000 | 0.26 | 0.000 | ||||
| Control belief (sum score 0–6) | – | – | 0.13 | 0.000 | – | – | 0.05 | 0.390 | – | – | 0.13 | 0.000 | |||||||
| Control variables | Gender (male) | 0.03 | 0.415 | 0.02 | 0.643 | 0.02 | 0.584 | 0.05 | 0.456 | 0.01 | 0.828 | 0.02 | 0.767 | 0.04 | 0.204 | 0.01 | 0.614 | 0.02 | 0.548 |
| Age (<25, 25–34, 35–44, 45–54, 55+) | 0.08 | 0.030 | 0.10 | 0.005 | 0.10 | 0.003 | 0.22 | 0.005 | 0.15 | 0.027 | 0.15 | 0.033 | 0.11 | 0.000 | 0.13 | 0.000 | 0.14 | 0.000 | |
| Job status (with supervisory position) | 0.06 | 0.142 | −0.03 | 0.420 | −0.04 | 0.263 | 0.06 | 0.427 | 0.12 | 0.104 | 0.12 | 0.082 | 0.12 | 0.000 | 0.05 | 0.08 | 0.05 | 0.076 | |
| Adjusted R square | 0.091 | 0.285 | 0.300 | 0.153 | 0.452 | 0.452 | 0.098 | 0.289 | 0.304 | ||||||||||
| No. cases in model | 677 | 622 | 617 | 206 | 192 | 191 | 1179 | 1089 | 1080 | ||||||||||
Table 4b Explaining satisfaction with life among health professionals – results of a stepwise multiple linear regression analysis (step 0, step 3 and 4).
| Dependent or outcome variable |
Satisfaction with life
(0–10 rating scale, 10 = completely satisfied) |
Nurses
(n = 705) |
Physicians
(n = 222) |
All health professionals
(n = 1232) |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Step 0 | Step 3 | Step 4 | Step 0 | Step 3 | Step 4 | Step 0 | Step 3 | Step 4 | |||||||||||
| beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | ||
| Independent or exposure variables | Overtime hours (0–10+) | −0.07 | 0.098 | −0.01 | 0.842 | −0.02 | 0.611 | −0.08 | 0.263 | −0.01 | 0.876 | −0.03 | 0.662 | −0.05 | 0.099 | 0.01 | 0.690 | 0.00 | 0.985 |
| Time pressure (fully disagree to fully agree 0–3) | −0.16 | 0.000 | −0.04 | 0.404 | −0.03 | 0.397 | −0.12 | 0.095 | 0.05 | 0.551 | 0.05 | 0.451 | −0.15 | 0.000 | −0.01 | 0.704 | −0.01 | 0.741 | |
| Mediating or intervening variables | General stress (not at all to a very large extent 0–4) | – | −0.38 | 0.000 | −0.34 | 0.000 | – | −0.28 | 0.000 | −0.20 | 0.004 | -0.36 | 0.000 | -0.33 | 0.000 | ||||
| Job autonomy (sum score 0–32) | – | 0.07 | 0.118 | 0.05 | 0.250 | – | 0.16 | 0.048 | 0.14 | 0.059 | 0.09 | 0.006 | 0.07 | 0.019 | |||||
| Work climate (sum score 0–24) | – | 0.09 | 0.017 | 0.06 | 0.085 | – | 0.22 | 0.11 | 0.132 | 0.13 | 0.000 | 0.09 | 0.001 | ||||||
| Control belief (sum score 0–6) | – | – | 0.24 | 0.000 | – | – | 0.39 | 0.000 | – | 0.25 | 0.000 | ||||||||
| Control variables | Gender (male) | −0.03 | 0.439 | −0.04 | 0.315 | −0.03 | 0.338 | 0.11 | 0.139 | 0.06 | 0.419 | 0.08 | 0.230 | 0.03 | 0.319 | 0.01 | 0.643 | 0.02 | 0.431 |
| Age (<25, 25–34, 35–44, 45–54, 55+) | 0.03 | 0.443 | 0.04 | 0.257 | 0.05 | 0.133 | 0.14 | 0.113 | 0.05 | 0.576 | 0.04 | 0.606 | 0.03 | 0.291 | 0.04 | 0.166 | 0.06 | 0.043 | |
| Job status (with supervisory position) | 0.06 | 0.127 | −0.00 | 0.961 | −0.02 | 0.654 | −0.02 | 0.824 | 0.02 | 0.786 | 0.04 | 0.608 | 0.04 | 0.232 | −0.01 | 0.726 | −0.01 | 0.699 | |
| Adjusted R square | 0.031 | 0.191 | 0.242 | 0.026 | 0.193 | 0.319 | 0.025 | 0.191 | 0.250 | ||||||||||
| No. cases in model | 677 | 622 | 617 | 208 | 194 | 193 | 1180 | 1090 | 1082 | ||||||||||
Table 4c Explaining satisfaction with life among health professionals – results of a stepwise multiple linear regression analysis (step 0, step 3 and 4).
| Dependent or outcome variable |
Satisfaction with health
(0–10 rating scale, 10 = completely satisfied) |
Nurses
(n = 705) |
Physicians
(n = 222) |
All health professionals
(n = 1232) |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Step 0 | Step 3 | Step 4 | Step 0 | Step 3 | Step 4 | Step 0 | Step 3 | Step 4 | |||||||||||
| beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | beta coeff. (β) | p-value | ||
| Independent or exposure variables | Overtime hours (0–10+) | 0.01 | 0.811 | 0.04 | 0.288 | 0.03 | 0.393 | 0.05 | 0.497 | 0.05 | 0.564 | 0.04 | 0.649 | 0.05 | 0.142 | 0.09 | 0.007 | 0.08 | 0.011 |
| Time pressure (fully disagree to fully agree 0–3) | −0.15 | 0.000 | −0.05 | 0.294 | −0.04 | 0.307 | −0.20 | 0.005 | 0.03 | 0.716 | 0.03 | 0.676 | −0.16 | 0.000 | −0.04 | 0.277 | −0.03 | 0.346 | |
| Mediating or intervening variables | General stress (not at all to a very large extent 0–4) | – | −0.32 | 0.000 | −0.28 | 0.000 | – | −0.34 | 0.000 | -0.31 | 0.000 | – | −0.35 | 0.000 | −0.33 | 0.000 | |||
| Job autonomy (sum score 0–32) | – | 0.06 | 0.161 | 0.04 | 0.304 | – | 0.13 | 0.120 | 0.12 | 0.141 | – | 0.07 | 0.033 | 0.07 | 0.074 | ||||
| Work climate (sum score 0–24) | – | 0.05 | 0.203 | 0.03 | 0.506 | – | 0.03 | 0.704 | −0.02 | 0.763 | – | 0.05 | 0.090 | 0.02 | 0.453 | ||||
| Control belief (sum score 0–6) | – | – | 0.24 | 0.00 | – | − | 0.17 | 0.019 | – | – | 0.21 | 0.000 | |||||||
| Control variables | Gender (male) | 0.00 | 0.982 | 0.01 | 0.855 | 0.01 | 0.772 | −0.01 | 0.882 | −0.07 | 0.335 | −0.06 | 0.386 | 0.03 | 0.367 | 0.02 | 0.542 | 0.03 | 0.386 |
| Age (<25, 25–34, 35–44, 45–54, 55+) | 0.02 | 0.577 | 0.02 | 0.705 | 0.02 | 0.515 | 0.01 | 0.942 | −0.07 | 0.407 | −0.07 | 0.405 | −0.00 | 0.922 | −0.00 | 0.927 | 0.01 | 0.773 | |
| Job status (with supervisory position) | 0.07 | 0.087 | 0.02 | 0.647 | 0.00 | 0.985 | −0.10 | 0.267 | −0.02 | 0.812 | −0.02 | 0.832 | 0.04 | 0.227 | 0.01 | 0.762 | 0.01 | 0.821 | |
| Adjusted R square | 0.021 | 0.126 | 0.182 | 0.022 | 0.113 | 0.135 | 0.024 | 0.151 | 0.193 | ||||||||||
| No. cases in model | 677 | 622 | 617 | 208 | 194 | 193 | 1180 | 1090 | 1082 | ||||||||||
General stress emerged as the strongest predictor of dissatisfaction by far in all health professionals and the two subsamples of physicians and nurses. The association was strongest for satisfaction with health as the outcome. As a predictor, only general stress was significant and decisive in this context.
In this study, more than one third of hospital physicians reported working six and more extra hours per week. More than half of all health professionals worked overtime. The majority, over 80%, of the respondents reported feeling that they were under time pressure (heavy workload), but were still more or less satisfied with their work and life. The strengths of the associations were depended on the profession of the study participants: physicians vs nurses vs other health professionals.
As to the first research question, temporal work stressors turned out to be inversely associated with satisfaction outcomes and mediated by general stress. Accordingly, general stress emerged as the strongest predictor of dissatisfaction in health professionals. Depending on the outcome and the subgroup studied, up to 45% of the variance was thus explainable. Data showed to different extents the significant influence of temporal work stressors on the outcomes under study. As expected, the association was strongest for job satisfaction. Overtime often adds to the general stress of an already demanding job [43]. Similarly, stress and satisfaction in physicians were inversely correlated in a Canadian study; associations of other stressors and resources were not investigated [44]. In this study, overtime hours had no significant effect on physicians’ general stress, as opposed to time pressure, even though extra hours of at least 3 and more per week on average were reported. This suggests that working extra hours is just one aspect of the temporal workload [45–48]. In Switzerland a maximum of 50 hours per week is stipulated by law, but on average the working time was still 56 hours per week in 2016, as a recent online survey revealed [49]. This highlights the problem that health professionals have limited time resources [15] and at the same time are under consistent time pressure [16]. In fact, limiting working hours may inadvertently have led to more time pressure. Studies in that realm may be little comparable between countries. Healthcare systems and health professionals’ tasks may differ substantially between countries. For example, countries may allow fewer or a great deal more working hours than Switzerland does. This may substantially affect any outcome.
With regard to the second research question, general stress was observed to (most) strongly predict domain-specific satisfaction, sometimes only surpassed by resources such as work climate or internal control belief. These findings confirm the importance of a good working atmosphere. In this study, the vast majority of all health professionals considered their work in the team as positive. According to these data, a good work climate was associated with less general stress and better job satisfaction. This result is in line with other studies [50]. However, our results suggest that the effect of general stress, as a mediator in the relationship between temporal work stressors and satisfaction with work, differs between physicians and nurses. The stratified analyses revealed that among physicians the association of temporal work stressors (exposure variables) and job satisfaction (outcome variable) was fully mediated by general stress, whereas among nurses mediation by general stress was only partial and incomplete.
Regarding the third research question, a high control belief was strongly and positively associated with being more satisfied with life, health and work. According to the concept or construct of locus of control, individuals who have strong internal control feelings believe that they can largely determine their environment or their lives on their own. Conversely, individuals who have an external locus of control believe that their lives are determined by chance, luck or fate. Some authors view control belief as personality traits of importance for stress and conflict management [29, 51]. A recent study investigated the interactive relationship between the two control beliefs and job autonomy [52], and found that a combination of high job control, high stressors and a strong internal control belief was a beneficial match. In the present study, we could also prove that the variable (internal) control belief was a strong predictor for being more satisfied with life, in particular for physicians. However, we investigated only internal control belief in our analyses. Still, our results support the findings that internal control belief as a personal resource also decides whether or not and to what extent a person is stressed and satisfied. Nevertheless, our data do not suggest that job autonomy is significantly correlated with physicians’ general stress. A possible explanation might be that high levels of job autonomy in general were rarely reported by hospital employees. Limited job autonomy is recognised to be a common problem for both physicians and nurses in hospitals [1, 31, 53]. However, it is certainly of influence that nurses experience less or different levels of job autonomy than physicians. This is also reflected in the lower number of nurses in higher job positions who participated in this survey. Yet, hypothetically, a personality trait such as a feeling of being in control of one’s life may overcome the general lack of autonomy of health professionals.
High workloads and resulting negative consequences, such as presenteeism, depression, burnout [54, 55] or leaving the profession may be counteracted by improved working conditions [1]. However, the precise relations between these factors have not been known so far. The results of this study suggest that temporal work overload generates general stress. However, this has not resulted in reducing the maximum permitted working time per week to satisfactory levels, as this may worsen physicians’ education, training and experience [56]. Furthermore, the number of working hours may be less relevant than other aspects of job satisfaction. Thus, changes in measures of autonomy for physicians, including being allowed to increase working hours (rather than reduce them) and physicians’ ability to obtain services for their patients, were identified as the strongest predictors of job satisfaction [57]. Therefore, the debate on work hours should ideally focus on the balance between protecting residents’ health and caring for the patients [58] with the corresponding moral pressure. To prevent a future shortage of qualified health professionals, attractive working conditions would have to be somewhat adapted to employees’ current needs and expectations, such as regarding work-life balance (e.g., work, leisure time, family, return). More than two thirds of the persons interviewed in this survey were women. This reflects the generally high proportion of women employed in health care. At present, 60% of students at medical faculties in Switzerland are women, with an increasing trend [59]. In the nursing profession, this relationship is traditionally even more prominent (more than 80% being female) [60]. In a recent survey of residents in internal medicine in Switzerland, women were more interested in part-time work and thus a different work-life balance [61]. Certainly, hospitals should become more family friendly, for example by establishing a comprehensive childcare infrastructure at or in proximity to the workplace [62] with opening hours in line with working hours of married or single health care professionals or perhaps by making leisure opportunities available [63]. Also, innovative flexible work time arrangements (e.g., attractive options for compensation of shift work, overtime) would possibly enable health professionals – both men and women – to have more time for family and rest [64].
However, the key question remains difficult to answer: Which influence is the most decisive in view of general stress and/or overall satisfaction in the workplace? In general, overtime by itself does not seem to be the main problem. However, there was evidence for overtime hours increasing risk of general stress in nurses. In a 2018 study, Hämmig showed that one out of six health professionals in this survey thought frequently of leaving the profession [33]. This supports our finding that these health professionals were a burdened group of employees. We assume that it is the meaningful aspect of working with patients, above all, that contributes to high overall satisfaction despite stress and limited job autonomy.
Our study is limited in several ways. First, because of the cross-sectional and nonrandomised design of the study, no causal assumptions can be made. We analysed secondary data. Therefore, sample size calculation was not an issue. The survey data are not representative for healthcare professionals in general or for hospital employees in particular, and the findings are therefore limited in their generalisability. A systematic selection bias is possible, as the hospitals and employees involved may not have participated randomly (sample selection bias). In general, reasons for hospitals or institutions not participating could be to protect employees from substantial work overload, other existing employee surveys, or the operational need for action that would result from the survey. At the individual level, the reasons for participation or nonparticipation in the survey are also not verifiable. It might be that heavily overloaded and more dissatisfied employees did not participate. Therefore, an underestimation of general stress and dissatisfaction is possible (self-selection bias). Furthermore, employee satisfaction is not the same as engagement. We measured only overall satisfaction with work, life and health. Overall satisfaction can still be very high, but individual aspects can already be rated as unfavourable. No information on the clinical specialty of the participating physicians was available. Moreover, the number of years in clinical training cannot be specified. With regard to the measurement of resources, we did not capture other dimensions of personality (e.g., externality, conscientiousness, openness to experience), as the focus was not primarily on personality and job performance. Finally, the Cronbach’s alpha for the work climate and locus of control scale was rather low. However, the Cronbach’s alpha for internal locus of control was expected to be lower by using just two items.
Nevertheless, a major strength of this study is that the size of the entire study sample as well as of the subgroups was large enough to allow for stratified analyses and to mostly obtain statistically significant measures of association (beta coefficients), except for rather weak associations (beta coefficients of ±0.14 and below) in the numerically smallest subgroup of physicians. This study is innovative because it investigated the emerging topic of temporal work stressors in health professionals – and whether organisational or personal resources such as specific personality traits play an important role in this regard.
Work overload in the form of frequent or excessive overtime work or permanent time pressure at work is an important job stressor that can strongly affect the satisfaction and well-being of those concerned. This applies not only but particularly to health professionals. Organisational and personal resources, such as a high level of job autonomy, a good work climate, or a strong internal control belief, partly compensate for the negative consequences of temporal work stressors.
No financial support and no other potential conflicts of interest relevant to this article were reported.
1 Wallace JE , Lemaire JB , Ghali WA . Physician wellness: a missing quality indicator. Lancet. 2009;374(9702):1714–21. doi:.https://doi.org/10.1016/S0140-6736(09)61424-0
2 Smith R . Why are doctors so unhappy? There are probably many causes, some of them deep. BMJ. 2001;322(7294):1073–4. doi:.https://doi.org/10.1136/bmj.322.7294.1073
3 Frenk J , Chen L , Bhutta ZA , Cohen J , Crisp N , Evans T , et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–58. doi:.https://doi.org/10.1016/S0140-6736(10)61854-5
4 Morse T , Fekieta R , Rubenstein H , Warren N , Alexander D , Wawzyniecki P . “Doing the heavy lifting: health care workers take back their backs”. New Solut. 2008;18(2):207–19. doi:.https://doi.org/10.2190/NS.18.2.j
5 Shan Z , Li Y , Zong G , Guo Y , Li J , Manson JE , et al. Rotating night shift work and adherence to unhealthy lifestyle in predicting risk of type 2 diabetes: results from two large US cohorts of female nurses. BMJ. 2018;363:k4641. doi:.https://doi.org/10.1136/bmj.k4641
6 Jackson EJ , Moreton A . Safety during night shifts: a cross-sectional survey of junior doctors’ preparation and practice. BMJ Open. 2013;3(9):e003567. doi:.https://doi.org/10.1136/bmjopen-2013-003567
7 Hansen J . Night Shift Work and Risk of Breast Cancer. Curr Environ Health Rep. 2017;4(3):325–39. doi:.https://doi.org/10.1007/s40572-017-0155-y
8 Weigl M , Müller A , Vincent C , Angerer P , Sevdalis N . The association of workflow interruptions and hospital doctors’ workload: a prospective observational study. BMJ Qual Saf. 2012;21(5):399–407. doi:.https://doi.org/10.1136/bmjqs-2011-000188
9 Bellandi T , Cerri A , Carreras G , Walter S , Mengozzi C , Albolino S , et al. Interruptions and multitasking in surgery: a multicentre observational study of the daily work patterns of doctors and nurses. Ergonomics. 2018;61(1):40–7. doi:.https://doi.org/10.1080/00140139.2017.1349934
10 Bochatay N , Muller-Juge V , Scherer F , Cottin G , Cullati S , Blondon KS , et al. Are role perceptions of residents and nurses translated into action? BMC Med Educ. 2017;17(1):138. doi:.https://doi.org/10.1186/s12909-017-0976-2
11 Cockburn J , Pit S . Prescribing behaviour in clinical practice: patients’ expectations and doctors’ perceptions of patients’ expectations--a questionnaire study. BMJ. 1997;315(7107):520–3. doi:.https://doi.org/10.1136/bmj.315.7107.520
12 Matthys J , Elwyn G , Van Nuland M , Van Maele G , De Sutter A , De Meyere M , et al. Patients’ ideas, concerns, and expectations (ICE) in general practice: impact on prescribing. Br J Gen Pract. 2009;59(558):29–36. doi:.https://doi.org/10.3399/bjgp09X394833
13 Cannavò M , La Torre F , Sestili C , La Torre G , Fioravanti M . Work Related Violence As A Predictor Of Stress And Correlated Disorders In Emergency Department Healthcare Professionals. Clin Ter. 2019;170(2):e110–23.
14Sattler A. [Multimorbidität in der stationären Versorgung – Sichtweise internistischer Ärztinnen und Ärzte: Behandungsziele, Schwierigkeiten und Optimierungspotential]. Dissertation an der Medizinischen Fakultät der Universität Zürich. 2017.
15 Wenger N , Méan M , Castioni J , Marques-Vidal P , Waeber G , Garnier A . Allocation of Internal Medicine Resident Time in a Swiss Hospital: A Time and Motion Study of Day and Evening Shifts. Ann Intern Med. 2017;166(8):579–86. doi:.https://doi.org/10.7326/M16-2238
16 Meyer B , Rohner B , Golder L , Longchamp C . Administrativer Aufwand für Ärzte steigt weiter an. Begleitstudie im Auftrag der FMH: Auswirkungen der neuen Spitalfinanzierung. Schweiz Arzteztg. 2016;97(1):6–8.
17 Mansukhani MP , Kolla BP , Surani S , Varon J , Ramar K . Sleep deprivation in resident physicians, work hour limitations, and related outcomes: a systematic review of the literature. Postgrad Med. 2012;124(4):241–9. doi:.https://doi.org/10.3810/pgm.2012.07.2583
18 Papp KK , Stoller EP , Sage P , Aikens JE , Owens J , Avidan A , et al. The effects of sleep loss and fatigue on resident-physicians: a multi-institutional, mixed-method study. Acad Med. 2004;79(5):394–406. doi:.https://doi.org/10.1097/00001888-200405000-00007
19 Gander P , Purnell H , Garden A , Woodward A . Work patterns and fatigue-related risk among junior doctors. Occup Environ Med. 2007;64(11):733–8. doi:.https://doi.org/10.1136/oem.2006.030916
20 Hasselhorn HM , Tackenberg P , Kuemmerling A , Wittenberg J , Simon M , Conway PM , et al. Nurses’ health, age and the wish to leave the profession--findings from the European NEXT-Study. Med Lav. 2006;97(2):207–14.
21Bolliger C, Golder L. [Der Ausstieg aus der kurativen ärztlichen Tätigkeit. Eine Umfrage im Auftrag des Verbands der Schweizerischen Assistenz- und Oberärztinnen und -ärzte (VSAO) und der Verbindung der Schweizer Ärztinnen und Ärzte (FMH)]. Bern: Büro Vatter & gfs; 2016.
22 Kivimäki M , Jokela M , Nyberg ST , Singh-Manoux A , Fransson EI , Alfredsson L , et al.; IPD-Work Consortium. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet. 2015;386(10005):1739–46. doi:.https://doi.org/10.1016/S0140-6736(15)60295-1
23 Mayor S . Working long hours is associated with higher risk of stroke, study shows. BMJ. 2015;351:h4523. doi:.https://doi.org/10.1136/bmj.h4523
24 Edwards N , Kornacki MJ , Silversin J . Unhappy doctors: what are the causes and what can be done? BMJ. 2002;324(7341):835–8. doi:.https://doi.org/10.1136/bmj.324.7341.835
25 Karasek R . Job Demands, Job Decision Latitude, and Mental Strain: Implications for Job Redesign. Adm Sci Q. 1979;24(2):285–308. doi:.https://doi.org/10.2307/2392498
26 Demerouti E , Bakker AB , Nachreiner F , Schaufeli WB . The job demands-resources model of burnout. J Appl Psychol. 2001;86(3):499–512. doi:.https://doi.org/10.1037/0021-9010.86.3.499
27 Mayerl H , Stolz E , Großschädl F , Rásky É , Freidl W . The moderating role of personal resources in the relationship between psychosocial job demands and health: a cross-sectional study. BMJ Open. 2017;7(8):e015710. doi:.https://doi.org/10.1136/bmjopen-2016-015710
28 Jimenez P , Dunkl A . The Buffering Effect of Workplace Resources on the Relationship between the Areas of Worklife and Burnout. Front Psychol. 2017;8:12. doi:.https://doi.org/10.3389/fpsyg.2017.00012
29 Darshani R . A Review of Personality Types and Locus of Control as Moderators of Stress and Conflict Management. Internal Journal of Scientific Research Publications. 2014;4(2):??.
30 Rotter JB . Generalized expectancies for internal versus external control of reinforcement. Psychol Monogr. 1966;80(1):1–28. doi:.https://doi.org/10.1037/h0092976
31 Aiken LH , Sloane DM , Bruyneel L , Van den Heede K , Sermeus W ; RN4CAST Consortium. Nurses’ reports of working conditions and hospital quality of care in 12 countries in Europe. Int J Nurs Stud. 2013;50(2):143–53. doi:.https://doi.org/10.1016/j.ijnurstu.2012.11.009
32 Williams ES , Skinner AC . Outcomes of physician job satisfaction: a narrative review, implications, and directions for future research. Health Care Manage Rev. 2003;28(2):119–39. doi:.https://doi.org/10.1097/00004010-200304000-00004
33 Hämmig O . Explaining burnout and the intention to leave the profession among health professionals - a cross-sectional study in a hospital setting in Switzerland. BMC Health Serv Res. 2018;18(1):785. doi:.https://doi.org/10.1186/s12913-018-3556-1
34 Häusler N , Bopp M , Hämmig O . Effort-Reward Imbalance, Work-Privacy Conflict, and Burnout Among Hospital Employees. J Occup Environ Med. 2018;60(4):e183–7. doi:.https://doi.org/10.1097/JOM.0000000000001287
35 Häusler N , Bopp M , Hämmig O . Informal caregiving, work-privacy conflict and burnout among health professionals in Switzerland - a cross-sectional study. Swiss Med Wkly. 2017;147:w14552.
36 Kristensen TS , Hannerz H , Høgh A , Borg V . The Copenhagen Psychosocial Questionnaire--a tool for the assessment and improvement of the psychosocial work environment. Scand J Work Environ Health. 2005;31(6):438–49. doi:.https://doi.org/10.5271/sjweh.948
37Kovaleva A. The IE-4: Construction and Validation of a Short Scale for the Assessment of Locus of Control. GESIS - Leibnitz-Institut für Sozialwissenschaften. 2012:https://nbn-resolving.org/urn:nbn:de:0168-ssoar-371199.
38 Elo AL , Leppänen A , Jahkola A . Validity of a single-item measure of stress symptoms. Scand J Work Environ Health. 2003;29(6):444–51. doi:.https://doi.org/10.5271/sjweh.752
39SHS. Swiss Health Survey 2012. Overview. Available at: https://www.bfs.admin.ch.
40SILC. Statistics on Income and Living Conditions (SILC). Available at: https://www.bfs.admin.ch/bfs.
41SHP. Swiss Household Panel (SHP). Available at: https://forsbase.unil.ch/project/study-public-overview/15632/0/.
42 Baron RM , Kenny DA . The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82. doi:.https://doi.org/10.1037/0022-3514.51.6.1173
43 McCall TB . The impact of long working hours on resident physicians. N Engl J Med. 1988;318(12):775–8. doi:.https://doi.org/10.1056/NEJM198803243181210
44 Williams ES , Rondeau KV , Xiao Q , Francescutti LH . Heavy physician workloads: impact on physician attitudes and outcomes. Health Serv Manage Res. 2007;20(4):261–9. doi:.https://doi.org/10.1258/095148407782219067
45 Bae SH , Fabry D . Assessing the relationships between nurse work hours/overtime and nurse and patient outcomes: systematic literature review. Nurs Outlook. 2014;62(2):138–56. doi:.https://doi.org/10.1016/j.outlook.2013.10.009
46 Lobo V , Fisher A , Peachey G , Ploeg J , Akhtar-Danesh N . Integrative review: an evaluation of the methods used to explore the relationship between overtime and patient outcomes. J Adv Nurs. 2015;71(5):961–74. doi:.https://doi.org/10.1111/jan.12560
47 Tomioka K , Morita N , Saeki K , Okamoto N , Kurumatani N . Working hours, occupational stress and depression among physicians. Occup Med (Lond). 2011;61(3):163–70. doi:.https://doi.org/10.1093/occmed/kqr004
48 Rosta J , Gerber A . Excessive working hours and health complaints among hospital physicians: a study based on a national sample of hospital physicians in Germany. Ger Med Sci. 2007;5:Doc09.
49vsao.ch. Bern: Verband Schweizerischer Assistenz- und Oberärztinnen und ärzte, [cited 2019 May 14]. Arbeitsbelastung der Assistenz- und Oberärztinnen und ärzte. Mitgliederbefragung 2017. Available from: https://www2.vsao.ch/fileupload/20174119517_pdf.pdf.
50 Aalto AM , Heponiemi T , Josefsson K , Arffman M , Elovainio M . Social relationships in physicians’ work moderate relationship between workload and wellbeing-9-year follow-up study. Eur J Public Health. 2018;28(5):798–804. doi:.https://doi.org/10.1093/eurpub/ckx232
51 Erbin-Roesemann MA , Simms LM . Work locus of control: the intrinsic factor behind empowerment and work excitement. Nurs Econ. 1997;15(4):183–90.
52 Meier LL , Semmer NK , Elfering A , Jacobshagen N . The double meaning of control: three-way interactions between internal resources, job control, and stressors at work. J Occup Health Psychol. 2008;13(3):244–58. doi:.https://doi.org/10.1037/1076-8998.13.3.244
53 Arnetz BB . Physicians’ view of their work environment and organisation. Psychother Psychosom. 1997;66(3):155–62. doi:.https://doi.org/10.1159/000289127
54 Shanafelt TD , Bradley KA , Wipf JE , Back AL . Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(5):358–67. doi:.https://doi.org/10.7326/0003-4819-136-5-200203050-00008
55 Aiken LH , Clarke SP , Sloane DM , Sochalski J , Silber JH . Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–93. doi:.https://doi.org/10.1001/jama.288.16.1987
56 Goitein L , Shanafelt TD , Wipf JE , Slatore CG , Back AL . The effects of work-hour limitations on resident well-being, patient care, and education in an internal medicine residency program. Arch Intern Med. 2005;165(22):2601–6. doi:.https://doi.org/10.1001/archinte.165.22.2601
57 Landon BE , Reschovsky J , Blumenthal D . Changes in career satisfaction among primary care and specialist physicians, 1997-2001. JAMA. 2003;289(4):442–9. doi:.https://doi.org/10.1001/jama.289.4.442
58 Fletcher KE , Underwood W, 3rd , Davis SQ , Mangrulkar RS , McMahon LF, Jr , Saint S . Effects of work hour reduction on residents’ lives: a systematic review. JAMA. 2005;294(9):1088–100. doi:.https://doi.org/10.1001/jama.294.9.1088
59 Clair C . Geschlecht in der Medizin: ein Thema mit vielen Facetten. Schweiz Arzteztg. 2017;98(50):1680–1. doi:.https://doi.org/10.4414/saez.2017.06269
60Merçay C, Burla L, Widmer M. [Gesundheitspersonal in der Schweiz. Bestandesaufnahme und Prognosen bis 2030 (Obsan Bericht 71)]. Neuchâtel: Schweizerisches Gesundheitsobservatorium; 2016.
61 Cribari M , Holzer BM , Battegay E , Minder CE , Zimmerli LU . What makes internal medicine attractive for the millennial generation? A survey of residents in internal medicine in Switzerland. Swiss Med Wkly. 2018;148:w14696. doi:.https://doi.org/10.4414/smw.2018.14696
62 Treister-Goltzman Y , Peleg R . Female Physicians and the Work-Family Conflict. Isr Med Assoc J. 2016;18(5):261–6.
63 Dieser RB , Edginton CR , Ziemer R . Decreasing Patient Stress and Physician/Medical Workforce Burnout Through Health Care Environments: Uncovering the Serious Leisure Perspective at Mayo Clinic’s Campus in Rochester, Minnesota. Mayo Clin Proc. 2017;92(7):1080–7. doi:.https://doi.org/10.1016/j.mayocp.2017.03.017
64 Aaron M , Levenberg P . The millennials in medicine: tips for teaching the next generation of physicians. Journal of Academic Ophthalmology. 2014;7:e17–20.
No financial support and no other potential conflicts of interest relevant to this article were reported.