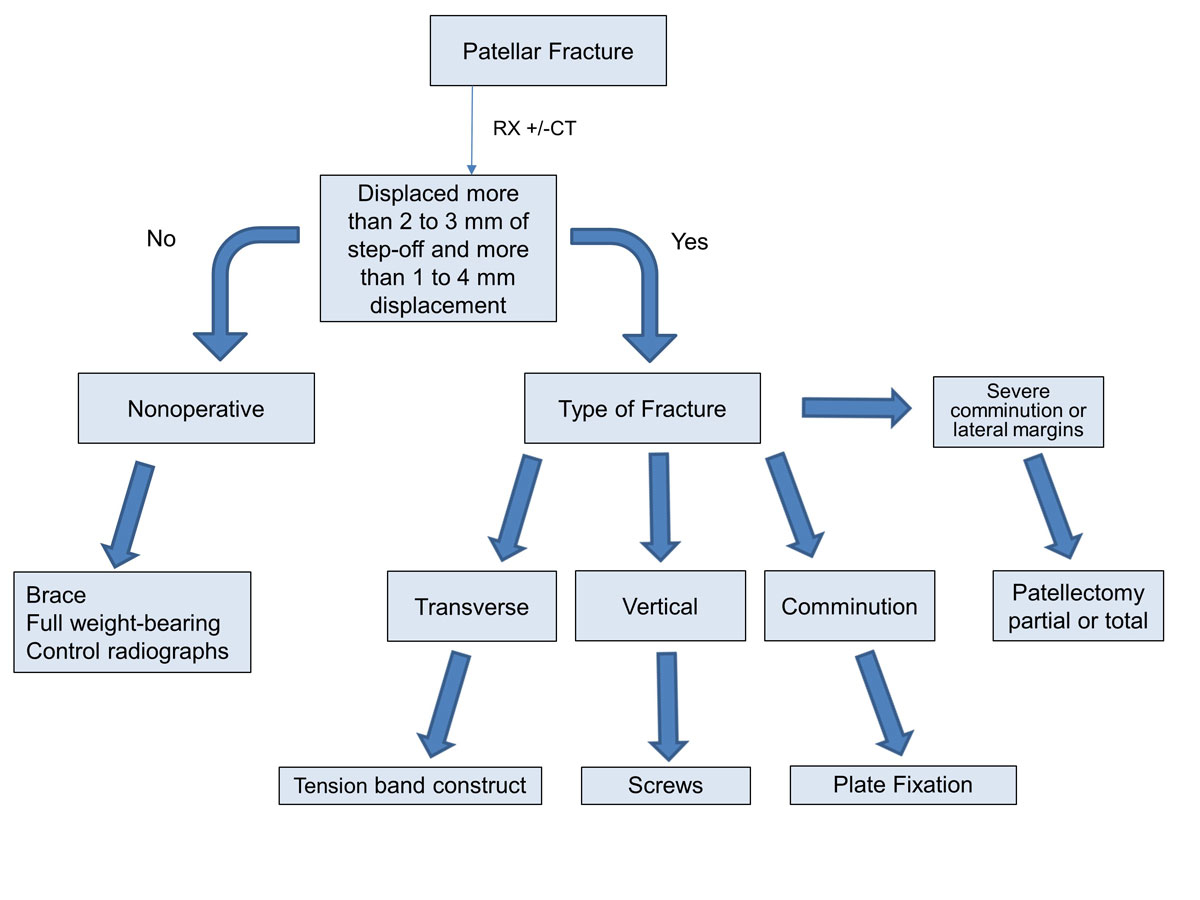
Figure 1 Treatment algorithm for patellar fractures.
DOI: https://doi.org/10.4414/smw.2020.20165
Patellar fractures are infrequent, with an incidence of approximately 1.2 per 100,000 per year [1]. They represent 1% of all fractures [2]. The patella is a part of the knee extensor apparatus. Being a sesamoid bone, it is in continuity with the quadriceps tendon proximally and the patellar ligament distally. Despite the low incidence of patellar fractures, the consequences of inadequate treatment or of very complex fractures are potentially disabling, with possible development of stiffness, loss of extension or patellofemoral osteoarthritis. The patella is integrated into the extensor apparatus of the knee. It has different roles [3] including transmission of forces of the quadriceps muscle, making the junction between the quadricipital tendon and the patellar ligament, and the distribution of the forces on the trochlea, through a thick cartilaginous surface, composed of two facets separated by a ridge and present on the superior three quarters of the articular side. Patellar cartilage thickness can reach up to 5 mm in its central part [2]. The patellofemoral contact area varies according to the degree of flexion of the knee: it is maximum at 90° of flexion (about 4 cm2) and almost zero in full extension of the knee [3]. The constraints on the patella are therefore highly variable too, depending on the amount of knee flexion. Indeed, the position of the patella varies in the sagittal plane depending on the degree of flexion. At 60°, the force reaches 4 times the weight of the body, whereas it is 7.65 times the weight of the body during a complete flexion [4]. Another role of the patella is to increase the lever arm. The patellar tendon has strengths up to 614 kg/cm2 at 5° and 1039 kg/cm2 at 90° of flexion. A decrease in its length causes an increase in the forces due to the decrease of the lever arm. The last role is the centring of the extensor apparatus. The transverse stability is provided by the medial and lateral retinaculae. Medially are the medial patellofemoral ligament, which inserts on the upper two thirds of the inner edge of the patella and the meniscopatellar ligament, which attaches to its lower third. Laterally, the external patellar retinacula attaches to the upper half of the outer edge of the patella and the meniscopatellar ligament to the lower half [2].
In this narrative review, we will cover the mechanisms of injury, the clinical facts, useful complementary imaging, as well as the various surgical options available and their complications.
Fractures of the patella can be caused by two different mechanisms, which will determine the type of fracture:
Evaluation of a patient with knee pain begins with a detailed history and physical examination. History of a direct blow to the knee or eccentric loading should raise suspicion for patellar fracture or other extensor mechanism injury. Associated injuries remain rare but must be actively looked for in certain traumas such as the dashboard (dash edge), in which the practitioner also has to rule out a fracture of the femoral neck or the posterior wall of the acetabulum and a hip dislocation.
On inspection, the knee is swollen on its anterior face with peripatellar haematoma, which may be contained in the adjacent soft tissues but may also lead to haemarthrosis. A thorough inspection of the skin is mandatory to rule out an open fracture and identify any skin compromise that could interfere with a surgical approach. Palpation reveals pain. In some cases, the presenting symptom is simply anterior knee pain with moderate oedema and partial loss of function without an active extension deficit. The continuity of the extensor mechanism may be evaluated with a straight leg raise examination. Inability to perform an active extension of the injured leg is critical because it can be sufficient to justify a surgery. Joint aspiration may be necessary in the event of a difficult clinical examination or a pain-induced flexion due to a haemarthrosis.
The main differential diagnosis is rupture of the extensor system, and rupture of the patellar or quadricipital tendon. Bipartite patella, a lack of ossification found in 2–3% of the cases, presents especially on the superolateral edge of the patella. It is bilateral in 50% of cases [5]. Bipartite patella is a congenital disease caused by a lack of fusion of one of the ossification centres and can be classified into three groups based on the position of the accessory centre: type I, at the inferior pole (5% of patients); type II, at the lateral margin (20%); and type III, at the superolateral pole (75%) [5]. Bipartite patella may be a cause of anterior knee pain following overuse, trauma or athletic activity causing an inflammation of the fibrocartilaginous interface separating the accessory bone from the main patella. Another differential diagnosis is osteochondritis of the patella, rare and potentially taken for an osteochondral fracture.
Typically, fracture classification and treatment decisions are based on quality anteroposterior and lateral radiographs of the knee, which help to clarify the type of fracture and exclude associated lesions. Because of the overlay of the patella on the femoral condyles, the anteroposterior view may be difficult to interpret. Lateral radiographs are useful in assessing displacement and articular congruity in transverse fractures.
The axial view of the patella at 30° of flexion is difficult to obtain because of the pain and can cause secondary displacement in cases of transverse or comminuted fracture. It is mostly useful to visualise sagittal fracture patterns, significant osteochondral lesions or retinacular avulsions.
The AO/OTA (AO Foundation / Orthopaedic Trauma Association) patellar fracture classification distinguishes three groups: extra-articular or avulsion fractures, partial articular (sagittal) and complete articular (either coronal or multifragmentary). The patellar bone is coded with the number 34, and a letter describes the type of fracture: A for extra-articular, B for partially articular, and C for completely articular. The next number describes the subtype and the second next one the precise localisation. For example, 34-C1.3 stands for a complete articular, transverse fracture through the distal third of the patella. Due to the complexity of this classification though, its interest remains uncertain in the daily practice.
Computed tomography (CT) with three-dimensional reconstructions can be very useful for quantifying precisely the number of fragments, the articular displacement or to detect small osteochondral fractures.
A recent study by Lazaro et al. demonstrated that it was extremely difficult to classify patellar fractures properly based on standard X-rays. With a CT scan, there was a change in the AO/OTA classification in 66% of the cases and a modification of the surgical strategy for 49% of the patients. In particular, severely comminuted distal pole fractures were missed on nearly half of the standard images [6].
The choice of the treatment is based on the patient’s history, the clinical findings and the configuration and displacement of the fracture. The goal is to restore the articular surface and the extensor mechanism.
It is indicated in fractures that are undisplaced or with a displacement of less than 4 mm and an articular step-off of less than 2 mm, and without interruption of the extensor mechanism (the leg can be actively straightened out) [7].
The treatment involves positioning a brace with approximately 10° of flexion and with a neutral rotation, allowing a slight tension of the extensor apparatus in order to avoid the development of a patella baja.
Early rehabilitation can start around the 10th day with mobilisation in passive flexion without contraction of the quadriceps, followed by a gradual increase without exceeding 90° before consolidation over a minimum of 45 days. This early mobilisation with careful monitoring by a physiotherapist will prevent joint stiffness especially in young subjects. It is also important to wake up the quadriceps and to avoid contractions against resistance. Weight-bearing is complete, with the help of crutches for balance. Delayed weight-bearing, which was previously the rule, has to be used only rarely in the geriatric population, because the patients do not manage to follow the rule or risk a fall while trying [8].
A first check at 10–15 days will exclude secondary displacement and the second at 45 days will look for bone healing or union; these checks being sufficient in a standard follow-up [9]. This well-conducted treatment has proven good results in 90% of cases [2, 9].
The main advantages of nonsurgical treatment are a reduction of the length of hospital stay and absence of a surgical intervention and anaesthesia; its drawbacks are a longer period of immobilisation, a higher rate of secondary displacement and the development of an ankylosis of the joint secondary to fibrous adhesions [10].
Good to excellent functional results can be expected with a nonsurgical treatment for minimally displaced fractures with no disruption of the extensor apparatus. We typically recommend immediate weight bearing in a hinged knee brace locked in extension followed by early range of motion (ROM) exercises with radiographic checks.
If the patient has significant medical comorbidities, nonsurgical management (brace and early full weight bearing) should be considered with a fracture >1 cm of displacement without severe pain. Nevertheless, at a 2-year follow-up there was a mean extensor lag of ≥20° and 25% patients considered their outcome to be poor [11].
Indications for surgical treatment are transverse, stellar or comminuted fractures with a displacement greater than 4 mm and/or with an articular step-off greater than 2 mm, as well as interruptions of the extensor apparatus (fig. 1) [7]. The goal of surgical treatment is to obtain an anatomical reduction of the joint surface, and to provide stable fixation to allow for early range of motion and thus restore the knee‐extensor mechanism.
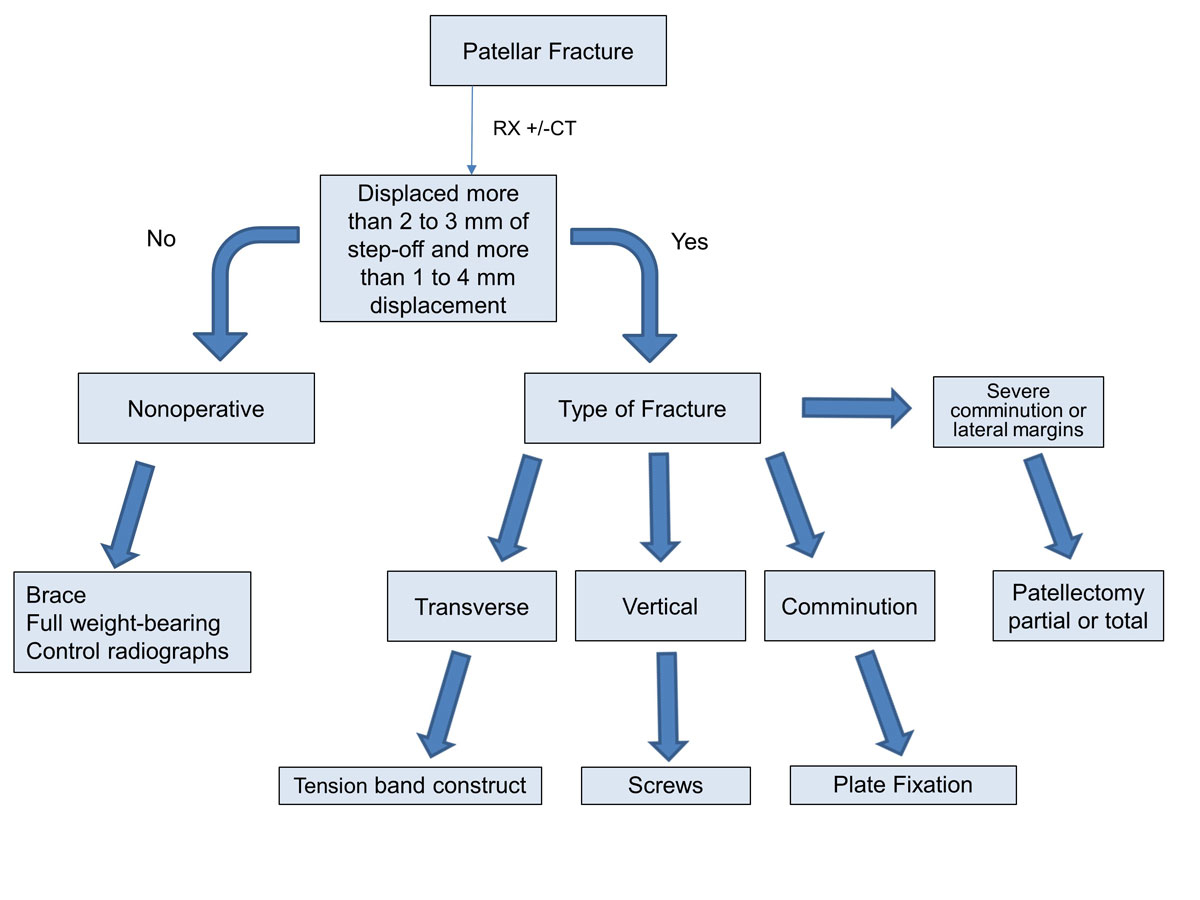
Figure 1 Treatment algorithm for patellar fractures.
The procedure can be performed under general or locoregional anaesthesia, preferably without a tourniquet in order to keep the quadriceps free. The incision is most often median or adapted to the cutaneous lesions and associated with a small external arthrotomy to assess the quality of the reduction, except if a passage through a traumatic capsuloligamentous lesion allows finger palpation of the articular surface from the medial side [12].
The technique developed in the 1950s by the Arbeitsgemeinschaft für Osteosynthesefragen / Association for the Study of Internal Fixation (AO/ASIF) for transverse fractures is ideal because it uses the compression of the braces during bending movements, which allows early mobilisation [13]. This technique converts the anterior tension forces produced by the extensor mechanism and knee flexion into compression forces at the articular surface (fig. 2). For maximum efficiency, there should be no loss of substance on the articular surface of the patella. Two parallel pins are inserted, then the brace is made of a metal wire that passes in front of the patella and then behind each pin by making a “figure of 8” (fig. 3). The pins are bent and depressed so as not to interfere with the soft tissues [14]. This technique gives good results in more than 80% of cases [15].
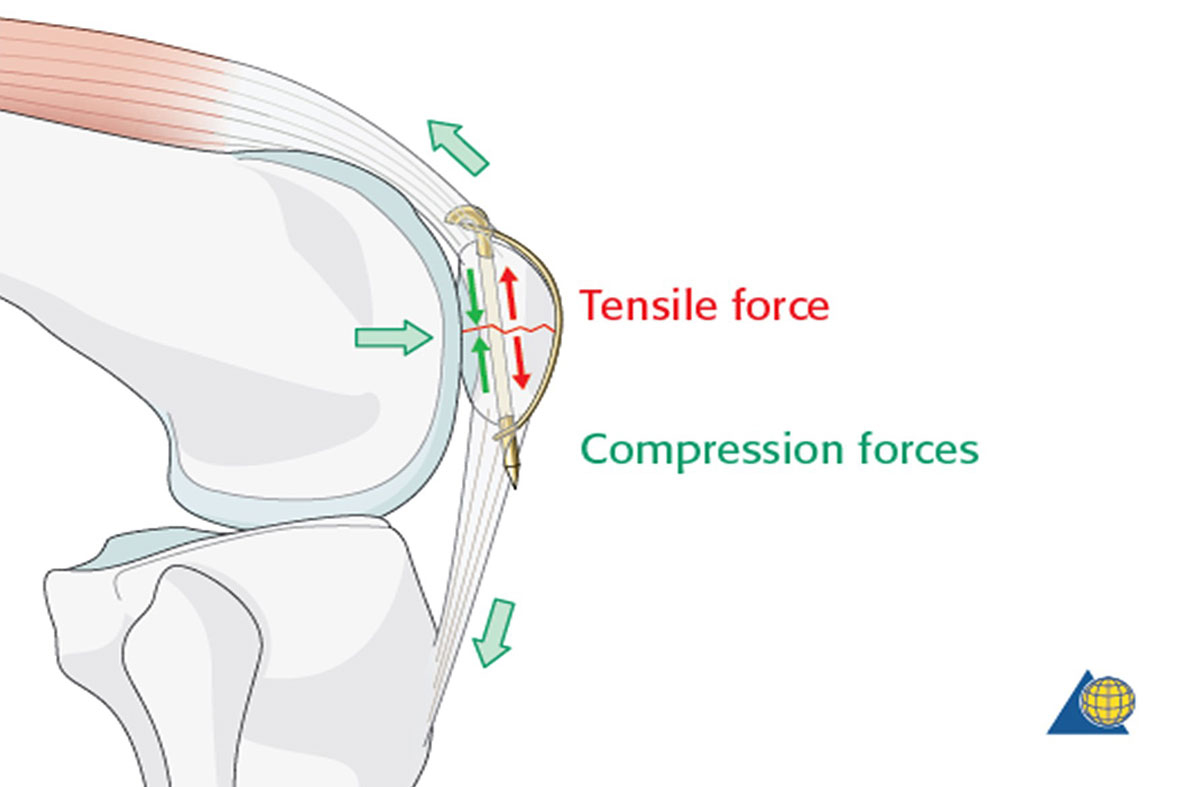
Figure 2 The tensile band principle (©AO Foundation, Switzerland; Source: AO Surgery Reference, www.aosurgery.org).
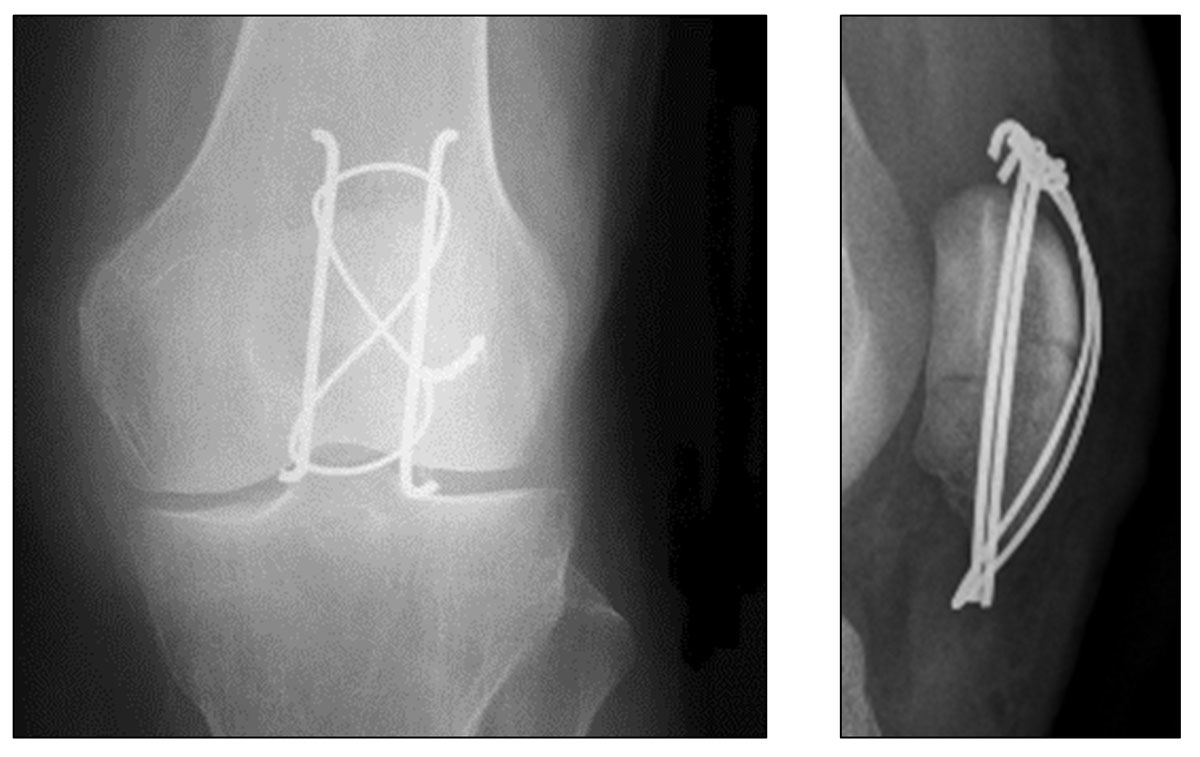
Figure 3 X-ray of a patella with tension band construct (CHUV).
The most commonly used method is a tension band technique; however, this is only possible after a more complex fracture has been converted into a two‐part fracture and if there is no discontinuity on the articular side. Additional fracture fragments can be fixed using supplementary circular wire (fig. 4) [16] or mini‐fragment screws (fig. 5) [17]. The repair of the retinacular defect contributes also to the overall stability of the construct.

Figure 4 Tension band construct reinforced with an equatorial wire (CHUV).

Figure 5 Tension band construct reinforced with an equatorial wire (CHUV).
The option to replace the metal wire with nonabsorbable suture wire (FiberWire / Ethibond) shows similar results, with a lower rate of ablation for hardware discomfort or complications such as infection [18, 19]. Removal of troublesome material is needed in up to 60% of patients [3, 20, 21].
Based on the AO principle of anatomical reduction and compression, the screws must hold firmly in the bone, but the cancellous bone of the patella is not always a favourable site in cases of comminution and/or osteoporosis. Nonetheless, this technique has the advantage of reducing by 50% the rate of hardware removal (fig. 6) [22].
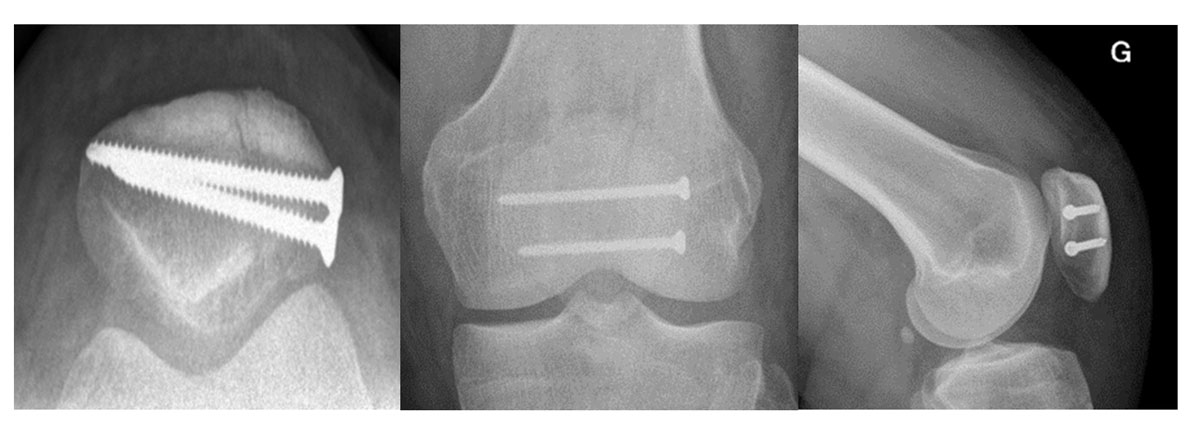
Figure 6 X-ray of knees with two screws for a longitudinal (vertical) fracture (CHUV.
This technique, initially described by Appel, consists of a parallel screwing using two cannulated screws on which a metal stay is supported [23].
The advantage of arthroscopy is that it allows the surgeon to make a precise assessment of the cartilage and ligaments in the knee and to accurately check the reduction from inside the joint, before screwing the fracture percutaneously. This technique has shown good results on transverse fractures without comminution and mild displacement [24].
This technique also has advantages in the presence of skin compromise, as it decreases the rate of skin complications compared with open surgery [25].
This technique consists of replacing the pins with screws in which the bracing passes. The metal strapping can be placed in a frame or in a figure of 8. This technique ensures compression of the fracture site if the screws are cannulated and protrude from the fracture site. The problem of this type of assembly is possible rupture of the strapping at the exit of the screws. It showed better stability (732 Newtons) than that with screws alone (554 Newtons) or that of the AO (tension band) technique [26].
Small plates can be applied to the anterior surface of the patella in the setting of comminution to provide additional stability.
A recent study by Taylor et al. reported the outcomes for eight patients with acute patellar fractures or nonunions treated with a combination of plates and interfragmentary screw fixation. All the patients went on to consolidation, with a mean range of motion of 129°. They reported no hardware removal for symptomatic implants. A second study by Thelen et al., published in 2012, compared three techniques of fixation for transverse fractures in the cadaver laboratory. This work showed that after 100 cycles of full extension to 90° flexion, the displacement of the fracture was less than 1 mm in the fixed-angle plating group, versus 3.7 mm in the cannulated screw tension-band group and 7.1 mm in the K-wire tension-band group [27].
Taylor et al. recently reported techniques and outcomes of plate fixation for patella fractures. They described eight patients with patella fractures or nonunions treated with a combination of plate and interfragmentary screw fixation. All of their patients went on to union at a mean of 3.2 months with an average total knee range of motion of 129°. There were no cases of hardware removal for symptomatic implants.
Thelen et al. [27] evaluated in cadavers the fixation of transverse fractures and compared Kirschner wire tension band fixation, cannulated screw tension band fixation and fixed-angle plates. After 100 cycles of bending from full extension to 90° of flexion, the fixed-angle plating group averaged less than 1 mm of displacement, compared with 7.1 and 3.7 mm in the Kirschner wire and cannulated screw tension band groups, respectively.
The patellar fractures fixed with tension band fixation construct had a 33% lower load to failure and 5 times larger fracture gap displacement than the locking plate construct in a simulated walk [28].
Two other surgical techniques used since the 1960s are partial and complete patellectomy.
This technique should be reserved for cases with significant cartilage loss, severe comminution or fracture of the internal or of the external lateral margins. A minimum of 60% of the patella should remain to avoid horizontal rocking [21]. The technique gives 78% good and excellent results with a quadriceps strength at 85% compared with the contralateral side [22].
Reserved for failures including cases of uncontrolled sepsis, it should be avoided because of the consequences of total patellectomy on the extensor mechanism: a loss of strength of up to 50% [23].
Knee stiffness is one of the main functional complications because of a prolonged immobilization following conservative or surgical treatment. Early physiotherapy is critical to minimize it and often avoids the need for revision surgery.
Failure of the material is most often due to a technical error or non-compliance of the patient [24]. Its rate is variable, up to 22% [22, 29].
Anterior knee pain is also a common symptom encountered after patellar fractures, whether they were treated surgically or not. The pain is often maximum when the extensor mechanism is activated while the knee is under load in flexion. After a patellar fracture, a vicious circle may develop that limits rehabilitation of the quadriceps muscle: an atrophic and weak quadriceps leads to a maltracking patella and increased articular stress, resulting in anterior knee pain that inhibits muscle activity. The vastus medialis obliquus, critical for the stabilisation of the patellar movement, is the first part of the quadriceps muscle that atrophies following disuse. A likely contributing factor to this maltracking and anterior knee pain is scarring and tightness of the structures surrounding the knee, which may result from the initial fracture or subsequent surgical treatment. During surgical repair, a lateral arthrotomy is often performed to allow direct visual reduction of the articular surface. This approach may contribute to a tight lateral retinaculum, associated with patellar tilt and excessive lateral patellar pressures.
Early rehabilitation is of critical importance to strengthen and balance the quadriceps forces, as is a cautious closure of all the structures responsible for patellar stability such as the lateral and medial retinaculae.
High prevalence of thigh muscle atrophy (41%) and limited quadriceps performance following patellar fractures may cause pathological patellar tracking, which increases stress on the patellofemoral joint and, thus, anterior knee pain.
Nonunion is rare, estimated at between 1 to 5% for closed fractures, but can be up to 7% for open fractures [7, 29]. The tolerance of these nonunions is variable. The main clinical symptom is pain associated with walking difficulties, mostly occurring on stairs. The clinical examination shows an active extension deficit. Imaging confirms the diagnosis. Treatment consists of solid osteosynthesis associated with bone grafting after exclusion of a septic problem. Total patellectomy should be discussed in cases of septic pseudarthrosis.
Deep infection is also rare (0–5%), although substantially higher in cases of open fracture (11%) [22, 29, 30]. If an early infection is diagnosed in the first 2 weeks, debridement with implant retention can be performed, followed by organism-specific antibiotic treatment until bony union (approximately 12 weeks). In cases of secondary displacement, inadequate reduction or poor skin condition, the hardware should be removed during the first 6 weeks of the antibiotic treatment, before a revision osteosynthesis is planned.
If infection occurs between 2 weeks and 3 months after the surgery, and if the local skin condition is good, a one-step exchange of the hardware with 12 weeks antibiotic treatment should be considered.
The treatment of late infections, diagnosed more than 3 months postoperatively, depends on fracture healing. An imaging evaluation with plain radiographs and a computed tomography is used to confirm proper healing of the fracture. If so, the hardware should be promptly removed and the patient should be treated for 6 weeks with antibiotics adapted to the organism found in cultures [31]
Posttraumatic patellofemoral osteoarthritis, resulting either from trauma-related cartilage damage or from a nonanatomical reduction of the fracture, is common. After 8.4 years, radiological osteoarthritis is diagnosed in more than 50% of cases [32].
Soft-tissue procedures for patellofemoral osteoarthritis include release of the lateral patellar retinaculum, reattachment or reconstruction of the medial patellofemoral ligament, and advancement of the vastus medialis obliquus. The results of soft-tissue realignment procedures for patellofemoral osteoarthritis in the absence of patellar instability have not yet been sufficiently investigated. The medial patellofemoral ligament is known to be a crucial component in patellofemoral joint stability for the prevention of lateral patellofemoral dislocation. This underlines the importance of an anatomical reconstruction of the vastus medialis obliquus and the patellofemoral ligaments during the surgery.
Patellofemoral prosthetic implants are available but their indications are limited owing to their high rates of failure [33–37]. However, prosthesis design has since evolved to produce improved outcomes [6, 38]. The femoral flange is shallow and broad to promote stable fixation of the patella to the femoral trochlea. The medial side of the patellar component is uniquely concave to avoid impingement on the femoral component in flexion. This design improvement has contributed to ruling out the potential risk of early polyethylene wear and malalignment, which in turn causes a low complication rate and improved ROM (fig. 5). Patellofemoral replacement is primarily indicated in patients who are too young for total knee arthroplasty or have isolated patellofemoral arthritis. In general, patellectomy produces unsatisfactory results in young patients, and in 47% of all patients, compared with total knee arthroplasty, patellofemoral replacement is advantageous for maintaining the biomechanics of the knee joint while preserving the menisci and cruciate ligaments.
The prognosis after patellar fractures depends on the type of fracture, the force of the trauma and the number of fragments. The management will influence the prognosis. The clinical examination must always be methodical and thorough in order to look for associated lesions. The radiological assessment allows the type of fracture to be accurately determined. The management can be conservative or surgical, depending on fracture displacement and extensor apparatus integrity. As for all articular fractures, anatomical reduction, if possible, is essential for a satisfactory long-term outcome. Full weight-bearing should be allowed in all cases, and early mobilisation should be favoured, with both conservative and surgical treatment, to avoid stiffness. Classical osteosynthesis (tension band construct) is the most frequently performed technique, but alternatives using screws and/or plates or even combinations exist and have shown similar outcomes. Complications after patella fracture are not rare and potentially debilitating, and can be avoided by well-conducted treatment.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 van Staa TP , Dennison EM , Leufkens HG , Cooper C . Epidemiology of fractures in England and Wales. Bone. 2001;29(6):517–22. doi:.https://doi.org/10.1016/S8756-3282(01)00614-7
2 Boström A . Fracture of the patella. A study of 422 patellar fractures. Acta Orthop Scand Suppl. 1972;43(sup143):1–80. doi:.https://doi.org/10.3109/ort.1972.43.suppl-143.01
3 Melvin JS , Mehta S . Patellar fractures in adults. J Am Acad Orthop Surg. 2011;19(4):198–207. doi:.https://doi.org/10.5435/00124635-201104000-00004
4 Teitz CC , Harrington RM . Patellar stress fracture. Am J Sports Med. 1992;20(6):761–5. doi:.https://doi.org/10.1177/036354659202000621
5 Atesok K , Doral MN , Lowe J , Finsterbush A . Symptomatic bipartite patella: treatment alternatives. J Am Acad Orthop Surg. 2008;16(8):455–61. doi:.https://doi.org/10.5435/00124635-200808000-00004
6 Lazaro LE , Wellman DS , Pardee NC , Gardner MJ , Toro JB , Macintyre NR, 3rd , et al. Effect of computerized tomography on classification and treatment plan for patellar fractures. J Orthop Trauma. 2013;27(6):336–44. doi:.https://doi.org/10.1097/BOT.0b013e318270dfe7
7 Carpenter JE , Kasman R , Matthews LS . Fractures of the patella. J Bone Joint Surg Am. 1993;75(10):1550–61. doi:.https://doi.org/10.2106/00004623-199310000-00016
8 Sayum Filho J , Lenza M , Teixeira de Carvalho R , Pires OG , Cohen M , Belloti JC . Interventions for treating fractures of the patella in adults. Cochrane Database Syst Rev. 2015;2(2):CD009651. doi:.https://doi.org/10.1002/14651858.CD009651.pub2
9 Braun W , Wiedemann M , Rüter A , Kundel K , Kolbinger S . Indications and results of nonoperative treatment of patellar fractures. Clin Orthop Relat Res. 1993;&NA;(289):197–201. doi:.https://doi.org/10.1097/00003086-199304000-00028
10Muller M, Allgower M, Schneider R, Willenegger H. Manual of Internal Fixation: Techniques Recommended by the AO‐ASIF Group. 3rd Edition. Berlin: Springer‐Verlag, 1991.
11 Pritchett JW . Nonoperative treatment of widely displaced patella fractures. Am J Knee Surg. 1997;10(3):145–7, discussion 147–8.
12 Gardner MJ , Griffith MH , Lawrence BD , Lorich DG . Complete exposure of the articular surface for fixation of patellar fractures. J Orthop Trauma. 2005;19(2):118–23. doi:.https://doi.org/10.1097/00005131-200502000-00008
13 Helfet DL , Haas NP , Schatzker J , Matter P , Moser R , Hanson B . AO philosophy and principles of fracture management-its evolution and evaluation. J Bone Joint Surg Am. 2003;85(6):1156–60. doi:.https://doi.org/10.2106/00004623-200306000-00029
14Muller ME, Algöwer M, Schneider R, et al. Manual of internal fixation, 3rd edn. Springer, Berlin Heidelberg New York 1990.
15 Hung LK , Chan KM , Chow YN , Leung PC . Fractured patella: operative treatment using the tension band principle. Injury. 1985;16(5):343–7. doi:.https://doi.org/10.1016/0020-1383(85)90144-5
16 Fortis AP , Milis Z , Kostopoulos V , Tsantzalis S , Kormas P , Tzinieris N , et al. Experimental investigation of the tension band in fractures of the patella. Injury. 2002;33(6):489–93. doi:.https://doi.org/10.1016/S0020-1383(01)00173-5
17 Baran O , Manisali M , Cecen B . Anatomical and biomechanical evaluation of the tension band technique in patellar fractures. Int Orthop. 2009;33(4):1113–7. doi:.https://doi.org/10.1007/s00264-008-0602-3
18 Camarda L , La Gattuta A , Butera M , Siragusa F , D’Arienzo M . FiberWire tension band for patellar fractures. J Orthop Traumatol. 2016;17(1):75–80. doi:.https://doi.org/10.1007/s10195-015-0359-6
19 Gosal HS , Singh P , Field RE . Clinical experience of patellar fracture fixation using metal wire or non-absorbable polyester--a study of 37 cases. Injury. 2001;32(2):129–35. doi:.https://doi.org/10.1016/S0020-1383(00)00170-4
20 Kumar G , Mereddy PK , Hakkalamani S , Donnachie NJ . Implant removal following surgical stabilization of patella fracture. Orthopedics. 2010;33(5). doi:.https://doi.org/10.3928/01477447-20100329-14
21 LeBrun CT , Langford JR , Sagi HC . Functional outcomes after operatively treated patella fractures. J Orthop Trauma. 2012;26(7):422–6. doi:.https://doi.org/10.1097/BOT.0b013e318228c1a1
22 Hoshino CM , Tran W , Tiberi JV, III , Black MH , Li BH , Gold SM , et al. Complications following tension-band fixation of patellar fractures with cannulated screws compared with Kirschner wires. J Bone Joint Surg Am. 2013;95(7):653–9. doi:.https://doi.org/10.2106/JBJS.K.01549
23 Appel MH , Seigel H . Treatment of transverse fractures of the patella by arthroscopic percutaneous pinning. Arthroscopy. 1993;9(1):119–21. doi:.https://doi.org/10.1016/S0749-8063(05)80357-3
24 El-Sayed AM , Ragab RK . Arthroscopic-assisted reduction and stabilization of transverse fractures of the patella. Knee. 2009;16(1):54–7. doi:.https://doi.org/10.1016/j.knee.2008.07.010
25 Turgut A , Günal I , Acar S , Seber S , Göktürk E . Arthroscopic-assisted percutaneous stabilization of patellar fractures. Clin Orthop Relat Res. 2001;(389):57–61. doi:.https://doi.org/10.1097/00003086-200108000-00010
26 Carpenter JE , Kasman RA , Patel N , Lee ML , Goldstein SA . Biomechanical evaluation of current patella fracture fixation techniques. J Orthop Trauma. 1997;11(5):351–6. doi:.https://doi.org/10.1097/00005131-199707000-00009
27 Thelen S , Schneppendahl J , Jopen E , Eichler C , Koebke J , Schönau E , et al. Biomechanical cadaver testing of a fixed-angle plate in comparison to tension wiring and screw fixation in transverse patella fractures. Injury. 2012;43(8):1290–5. doi:.https://doi.org/10.1016/j.injury.2012.04.020
28 Sutton FS, Jr , Thompson CH , Lipke J , Kettelkamp DB . The effect of patellectomy on knee function. J Bone Joint Surg Am. 1976;58(4):537–40. doi:.https://doi.org/10.2106/00004623-197658040-00017
29 Smith ST , Cramer KE , Karges DE , Watson JT , Moed BR . Early complications in the operative treatment of patella fractures. J Orthop Trauma. 1997;11(3):183–7. doi:.https://doi.org/10.1097/00005131-199704000-00008
30 Catalano JB , Iannacone WM , Marczyk S , Dalsey RM , Deutsch LS , Born CT , et al. Open fractures of the patella: long-term functional outcome. J Trauma. 1995;39(3):439–44. doi:.https://doi.org/10.1097/00005373-199509000-00007
31 Steinmetz S , Wernly D , Moerenhout K , Trampuz A , Borens O . Infection after fracture fixation. EFORT Open Rev. 2019;4(7):468–75. doi:.https://doi.org/10.1302/2058-5241.4.180093
32 Saltzman CL , Goulet JA , McClellan RT , Schneider LA , Matthews LS . Results of treatment of displaced patellar fractures by partial patellectomy. J Bone Joint Surg Am. 1990;72(9):1279–85. doi:.https://doi.org/10.2106/00004623-199072090-00001
33 McKeever DC . Patellar prosthesis. J Bone Joint Surg Am. 1955;37(5):1074–84. doi:.https://doi.org/10.2106/00004623-195537050-00015
34 Lubinus HH . Patella glide bearing total replacement. Orthopedics. 1979;2(2):119–27.
35 Tauro B , Ackroyd CE , Newman JH , Shah NA . The Lubinus patellofemoral arthroplasty. A five- to ten-year prospective study. J Bone Joint Surg Br. 2001;83-B(5):696–701. doi:.https://doi.org/10.1302/0301-620X.83B5.0830696
36 Kooijman HJ , Driessen AP , van Horn JR . Long-term results of patellofemoral arthroplasty. A report of 56 arthroplasties with 17 years of follow-up. J Bone Joint Surg Br. 2003;85-B(6):836–40. doi:.https://doi.org/10.1302/0301-620X.85B6.13741
37 Krajca-Radcliffe JB , Coker TP . Patellofemoral arthroplasty. A 2- to 18-year followup study. Clin Orthop Relat Res. 1996;330:143–51. doi:.https://doi.org/10.1097/00003086-199609000-00017
38 Marsh JL , Slongo TF , Agel J , Broderick JS , Creevey W , DeCoster TA , et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(10, Suppl):S1–6. doi:.https://doi.org/10.1097/00005131-200711101-00001
No financial support and no other potential conflict of interest relevant to this article was reported.