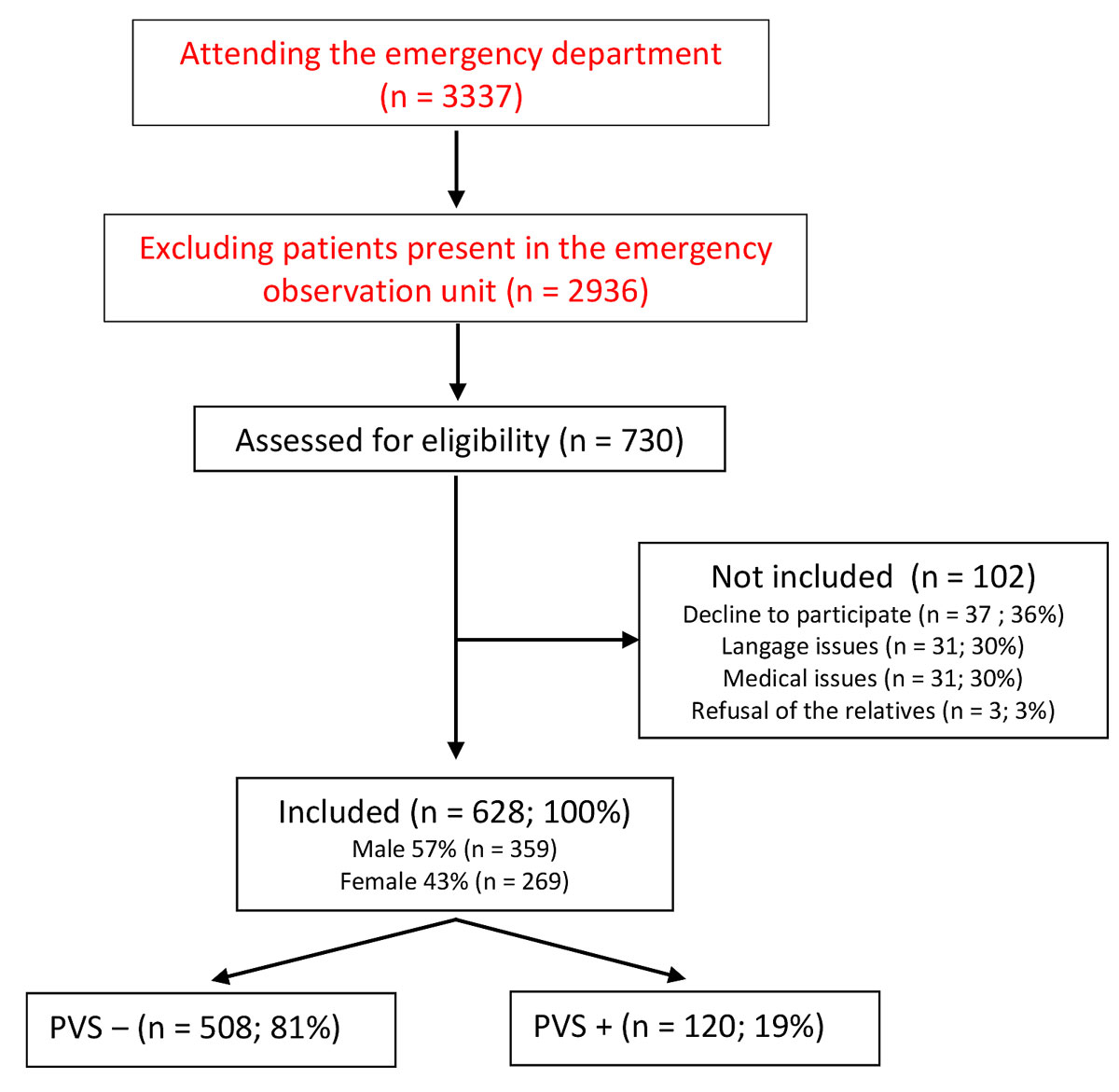
Figure 1 Patient recruitment flowchart.
PVS = Partner Violence Screening questionnaire
DOI: https://doi.org/10.4414/smw.2019.20147
According to a World Health Organization (WHO) report in 2002, violence constituted the fourth commonest cause of death amongst people aged 15 to 44 years [1]. In Switzerland, the incidence and threat of violence has risen overall in recent years, currently reaching levels seen in other European countries [2]. In this study, interpersonal violence was defined according to the WHO definition and for clarity was classified into two main categories: family/domestic violence vs community violence [1].
For victims of violence, the ED is the usual place of care owing to its round-the-clock opening hours with no need for an appointment, and the wide spectrum of medical expertise and technology available [3]. Nonetheless, the prevalence of violence remains underestimated in the ED, especially as patients do not spontaneously mention that they are victims. Often this is considered shameful, even taboo [4].
Moreover, it is complicated for nurses to detect such cases. In fact, unless it is the obvious reason for consultation, any investigation into possible violence might seem intrusive and be difficult to conduct correctly in the bustle of the ED. Doctors, amongst others, have difficulties in recognising victims of violence. They feel insufficiently trained and ill at ease with raising the subject, in particular when it comes to domestic violence [5]. Moreover, few EDs have protocols concerned with screening for violence. Consequently, the problem of interpersonal violence is broached by only a minority of victims during their passage through the ED [6]. A hospital ED is, however, an excellent place for such screening on account of being a first port of call for the general population and in particular for the vulnerable [7].
A previous study carried out in 2002 in the ED of Lausanne University Hospital (CHUV), which included 1602 patients, reported a prevalence of violence among attendees during the previous 12 months of about 11%. Of these, only a quarter consulted specifically for that reason. Men were prone to public violence and women to domestic [8]. In studies performed in EDs, other factors related to interpersonal violence such as the relationship of violence to psychotropic substance abuse, particularly alcohol [9], or the association with maxillofacial fractures were equally evident [10].
The purpose of our study was to assess if the increase in violence in society was reflected in a rise in the current prevalence of violence amongst CHUV ED attendees. Few studies on this subject have been conducted since 2002, even though the problem is critical in terms of public health, as well as the management of victims.
Ours was a cross-sectional study that used a self-administered modified version of the Partner Violence Screen questionnaire. Patients who consulted at the ED of the CHUV during the month of September 2016 were included. Interpersonal violence was defined according to the WHO definition and for clarity classified into two main categories: family/domestic violence vs community violence [1].
Located in the canton the Vaud in the western French-speaking part of Switzerland, the CHUV ED receives >60,000 patients annually of whom 42,000 are directly managed. It functions as a tertiary referral centre for approximately 1 million inhabitants, although the hospital acts as the primary centre of care for the city of Lausanne and its environs. Switzerland is a small, densely populated high-income country of 8.4 million inhabitants. The canton the Vaud has a mix of rural and urban areas, and accounts for 10% of the Swiss population. Lausanne is a festive city, with many clubs and bars and a population of 138,000.
According to the organisation and statutory definitions in our university hospital, patients aged over 16 years are considered as adults and therefore were eligible. Exclusion criteria were: cases requiring immediate attention according to the triage scale, incapacity for decision making, major confusional state, alcoholic intoxication, being affected by psychotropic drugs, psychiatric disturbance, dementia, depressed consciousness, language difficulties rendering understanding of the questionnaire impossible, police custody or legally deprived of liberty.
Patients first received a consent form explaining general and legal details of the study, with guarantees of confidentiality. After giving consent, a paper questionnaire was handed to each patient. Where a patient was physically unable to complete the form, help was provided while the confidentiality of the persons concerned was fully respected and any influencing on responses conscientiously avoiding. Patients who were drunk or agitated were not approached in our study.
The questionnaire used was a modified version of the Partner Violence Screening (PVS, appendix 1), translated into French and used in the 2002 study [8]. Some extra details were added to the questionnaire: the time and place of the act of aggression, the use of a knife, any correlation with alcohol, cannabis, cocaine, etc. A question concerning the role of the general practitioner in screening for violence was also added. The questionnaire was handed out by two authors (TD and AO) once patients had been seen by admission triage nurses and put into a consultation cubicle. Two initial questions intended to screen for violence were posed; two negative responses determined a negative PVS, at which point the enquiry for that particular patient was ended. However, if the response to one of the two initial questions was positive, the patient was asked to complete the questionnaire. Finally, the patient could indicate whether further conversation with an ED doctor was desired, which the authors facilitated.
The ethics committee on human research of the Canton of Vaud, Switzerland, approved this study (CER-VD no. 2016-01087).
Data concerning the age, sex, nationality, marital status and relevant demographic information were extracted directly from the ED administrative database and transferred electronically to the study database. The level of emergency was scored according to the Swiss Triage Scale (EST) from 1 (life-threatening emergency) to 4 (non-urgent) [11].
Personal data (completed questionnaires and sociodemographic parameters) were treated in full confidentiality by being coded and entered into a STATA 14 (StataCorp, College Station, TX, USA) database. In order to guarantee optimal quality of data collection, the data were entered twice in Excel and then fused using KNIME (Konstanz Information Miner). Any discrepancies were checked at source.
Continuous variables having a Gaussian distribution are described as mean and standard deviation (SD); the median and interquartile range (IQR) were reported for variables with a non-Gaussian distribution. Categorical variables are expressed as percentages and 95% confidence intervals (95% CI). Comparisons were made using Student's t-test or Mann–Whitney U test, as appropriate. Categorical data were compared with Pearson’s chi-squared test or Fisher’s exact test, as appropriate. A two-sided p-value <0.05 was considered significant.
During the study period, 730 questionnaires were distributed. Following application of exclusion criteria, 628 patients were included (fig. 1)
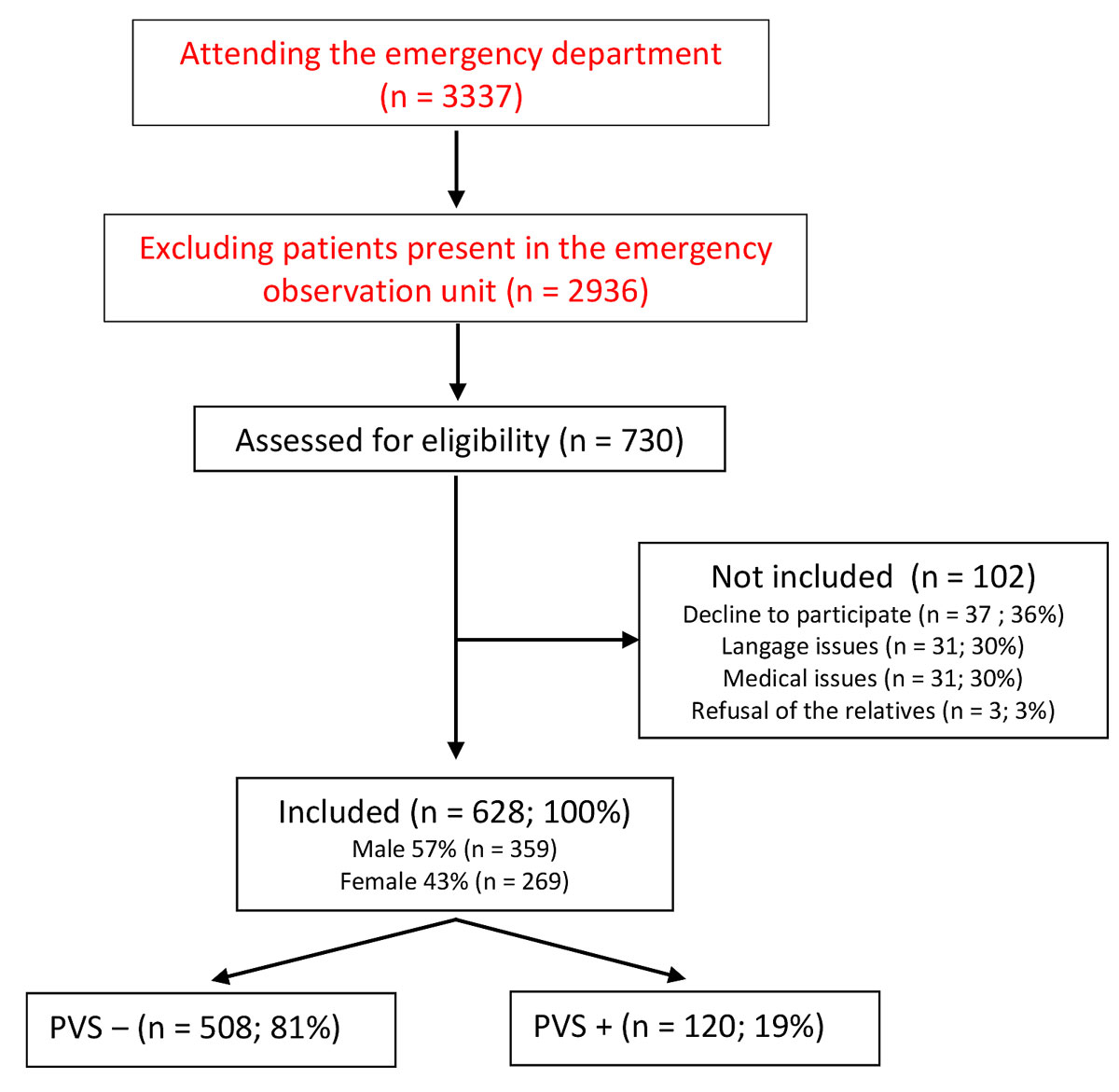
Figure 1 Patient recruitment flowchart.
PVS = Partner Violence Screening questionnaire
The total prevalence of self-reported interpersonal violence was 19.1% (n = 120/628, 95% CI 0.16–0.22): The majority of victims (with positive PVS charts) were young single Swiss men aged 16–34 years (tables 1 and 2 ). Half of these victims consulted at the ED during the period between Friday and Sunday. More than 30% of patients questioned admitted to the ED during the night (midnight to 8 a.m.) described episodes of violence.
Table 1 Characteristics of patients who were and were not screened as victim of violence.
| Variable | All patients (n = 628) | PVS+ (n = 120) | PVS− (n = 508) | p-values* | |
|---|---|---|---|---|---|
| Sex, n (%†) | Male | 359 (57) | 73 (61) | 286 (56) | 0.367 |
| Female | 269 (43) | 47 (39) | 222 (44) | ||
| Age, years, n (%†) | 16–34 | 242 (39) | 75 (63) | 167 (33) | <0.001 |
| 35–54 | 168 (27) | 29 (24) | 139 (27) | ||
| >55 | 218 (35) | 16 (13) | 202 (40) | ||
| Marital status, n (%†) | Single | 269 (43) | 85 (71) | 184 (36) | <0.001 |
| Married | 224 (36) | 14 (12) | 210 (41) | ||
| Divorced | 72 (11) | 13 (11) | 59 (12) | ||
| Separated | 21 (3) | 6 (5) | 15 (3) | ||
| Widowed | 42 (7) | 2 (2) | 40 (8) | ||
| Nationality, n (%†) | Swiss | 374 (60) | 75 (63) | 299 (59) | 0.528 |
| Border‡ | 76 (12) | 16 (13) | 60 (12) | ||
| Non-border§ | 177 (28) | 29 (24) | 148 (29) | ||
| Days of admission, n (%†) | Monday–Thursday | 367 (58) | 61 (51) | 306 (60) | 0.060 |
| Friday–Sunday | 261 (42) | 59 (49) | 202 (40) | ||
| Triage category¶, n (%†) | Absolute emergency (1–2) | 136 (22) | 23 (19) | 113 (22) | 0.49 |
| Relative emergency (3–4) | 491 (78) | 96 (81) | 395 (78) | ||
| Trauma as reason for consultation, n (%†) | 199 (32) | 67 (56) | 132 (26) | <0.001 | |
| Consultation outcome, n (%†) | Return home | 491 (78) | 104 (87) | 387(76) | 0.012 |
| Hospitalisation | 137 (22) | 16 (13) | 121 (24) | ||
PVS = Partner Violence Screening questionnaire * χ2 and Fischer exact test used; † percentage of sociodemographic category; ‡ countries bordering Switzerland (France, Germany, Italy, Lichtenstein, Austria); § countries not bordering Switzerland; ¶ Swiss Emergency Triage Scale (SETS) [11]. Due to rounding, total percentages may not equal 100% exactly.
Table 2 Odds ratio tests of surveyed patients’ sociodemographic characteristics
| Variable | Odds ratio | 95% CI | p-values* | |
|---|---|---|---|---|
| Sex | Male | Reference | – | – |
| Female | 0.83 | 0.55–1.24 | 0.367 | |
| Age, years | 16–34 | 5.67 | 3.18–10.10 | <0.001 |
| 35–54 | 2.63 | 1.38–5.03 | 0.003 | |
| >55 | Reference | – | – | |
| Marital status | Single | 9.24 | 2.18–39.12 | 0.003 |
| Married | 1.33 | 0.29–6.10 | 0.71 | |
| Divorced | 4.41 | 0.94–20.59 | 0.06 | |
| Separated | 8.0 | 1.45–44.1 | 0.017 | |
| Widowed | Reference | – | – | |
| Nationality | Swiss | Reference | – | – |
| Border† | 1.06 | 0.58–1.95 | 0.84 | |
| Non-border‡ | 0.78 | 0.49–1.25 | 0.31 | |
| Day of admission | Monday–Thursday | Reference | – | – |
| Friday–Sunday | 1.47 | 0.98–2.18 | 0.06 | |
| Hour of admission | 8 a.m. to 4 p.m. | Reference | – | – |
| 4 p.m. to midnight | 1.54 | 0.97–2.43 | 0.07 | |
| Midnight to 8 a.m. | 2.66 | 1.57–4.53 | <0.001 | |
CI = confidence interval * χ2 test used; † countries bordering Switzerland (France, Germany, Italy, Lichtenstein, Austria); ‡ countries not bordering Switzerland
The subgroups of age 16–34 years or being single were the most frequently affected. Patients consulting during the weekend were more likely to be victims of violence, but this was not statistically significant. The detailed characteristics of violence are described in table 3.
Table 3 Assault characteristics described by patients, differentiated by sex.
| Variable |
All PVS+
(n = 120) |
Male
(n = 73) |
Female
(n = 47) |
p-values* | |
|---|---|---|---|---|---|
| Physical assault, n (%†) | 68 (57) | 46 (63) | 22 (47) | 0.08 | |
| Verbal assault, n (%†) | 101 (84) | 59 (81) | 42 (89) | 0.211 | |
| Type of violence, n (%†) | Community | 66 (55) | 46 (64) | 20 (43) | <0.001 |
| Domestic | 26 (22) | 5 (7) | 21 (45) | ||
| Other‡ | 27 (23) | 21 (29) | 6 (13) | ||
| Place of aggression, n (%†) | Public place | 16 (13) | 13 (18) | 3 (7) | 0.051 |
| Home | 22 (18) | 9 (13) | 13 (29) | ||
| Café/bar/restaurant | 29 (24) | 21 (30) | 8 (18) | ||
| Public transport | 8 (7) | 4 (6) | 4 (9) | ||
| Multiple | 16 (13) | 7 (10) | 9 (20) | ||
| Other§ | 25 (21) | 17 (24) | 8 (18) | ||
| Timing of the assault, n (%†) | <24 hours | 24 (20) | 18 (25) | 6 (13) | 0.24 |
| <30 days | 21 (18) | 10 (14) | 11 (24) | ||
| <12 months | 56 (48) | 33 (45) | 23 (51) | ||
| Multiple | 17 (14) | 12 (16) | 5 (11) | ||
| Substance used, n (%†) | None | 70 (60) | 41 (59) | 29 (62) | 0.96 |
| Alcohol | 34 (29) | 21 (30) | 13 (28) | ||
| Drugs ± alcohol | 12 (10) | 7 (10) | 5 (11) | ||
| Weapon used, n (%†) | None | 94 (79) | 54 (74) | 40 (87) | 0.20 |
| Non-firearm weapon | 23 (19) | 17 (23) | 6 (13) | ||
| Firearm ± other | 2 (2) | 2 (3) | - | ||
| Violence as reason for consultation, n (%†) | 33 (28) | 22 (31) | 11 (23) | 0.37 | |
| Unsafe feeling, n (%†) | 35 (30) | 11 (15) | 24 (51) | <0.001 | |
| Willing to speak with the ED physician about it, n (%†) | 25 (21) | 15 (21) | 10 (21) | 0.95 | |
| Situation discussed with the referring/family physician, n (%†) | No | 88 (74) | 58 (79) | 30 (65) | 0.15 |
| Yes | 17 (14) | 7 (10) | 10 (22) | ||
| No doctor | 14 (12) | 8 (11) | 6 (13) | ||
PVS = Partner Violence Screening questionnaire * χ2 and Fischer exact test used; † percentage of sociodemographic category; ‡ workplace related, during activities, etc.; § workplace-related, on the phone, during activities, etc.; due to rounding, total percentages may not equal 100% exactly.
In 84% of cases, patients reported being menaced or psychologically pressured, and more than one person in two (57%) were victims of physical aggression (table 3). Public violence was most frequent, accounting for nearly three cases in five and occurring principally in cafés, bars and restaurants. In 19% of cases assaults involved knives. Alcohol had been consumed by the victims in 30% of cases.
A sensation of insecurity towards a person in the vicinity was mentioned by 30% of victims, this being rarely taken into account by a general practitioner or ED doctor during their consultation.
Amongst the PVS-positive cases, violence was the main reason for consultation in nearly one patient in three (28%, table 3). In this group, men were more numerous, but this difference was not significant. Victims of violence needed moderately urgent attention in four cases out of five (table 1). Most (87%) were discharged home from the ED.
Men were victims of public violence in almost two cases out of three (table 3), which corresponded more frequently to consultations concerning physical injury, with the use of knives in 25% of cases. These accounted for two thirds of assaults in public, which occurred in a public place such as a bar, nightclub or restaurant in 24% of all cases, but for men in 70% of cases. Men consulted more often during the weekend (53.4 vs 42.6%), particularly during the night, whereas women consulted principally during the week towards early evening.
Men were more likely than women to be admitted to hospital, which was related to a higher rate of being attacked even though the figures are not significant. Overall, victims, regardless of gender, were significantly more inclined to consult as a result of physical than verbal aggression.
Women were more frequently victims of domestic violence (p <0.001), which occurred in 65% of cases. They suffered less physical violence than men, but reported a greater sense of insecurity (p <0.001). Such violence was more likely to be discussed with their general practitioner.
The percentage of patients consulting at the ED as a result of violence has risen significantly from 11.4% to 19.1%, a relative increase of 68%, compared with the previous study in 2002 [8], with violence affecting one patient in five (19%) in 2016. This increase in violence reported matches a similar trend observed in society at large over the past few years. An enquiry conducted by the Institute of Criminology of the University of Zurich identified a five-fold rise in the amount of physical or threatened violence between 1984 and 2011 [10]. Such a trend has likewise been observed in accident insurance figures, which show that the incidence of violence amongst men aged 15–24 years rose from 4 to 12 per 1000 individuals between 1991 and 2006, whereas domestic violence seems to have remained stable in incidence [12]. Our results confirm that violence disproportionally affects young patients. Particular types of violence have changed in these years. According to the Swiss Government statistics (LAVI), the number of injuries has tripled since 2000, notably physical, but also acts of extortion, blackmail, intimidation or coercion [13]. This greater burden related to injuries from interpersonal violence was reflected in a study conducted at the ED of another tertiary Swiss urban hospital, where both the absolute number of patients and the severity of their injuries significantly increased between 2001 and 2006 [14]. Victims of violence accounted for 14% of admissions, a lower figure than our study conducted 10 years later, which demonstrates an ongoing upward trend.
Women and men were equally affected by violence, but of a different kind: predominantly domestic for the former and community for the latter. In 2018 in Switzerland, 18,522 domestic offences were registered by the police, a 9% increase from 2017 [15]. It is estimated than one in five Swiss women [16] will become a victim of psychological or physical violence during her life-time. As women represent more than half of all ED visits in the 19–45 year age group [17], screening for domestic violence is pertinent in this setting. Furthermore, according to a Canadian study, nearly 90% of women approved universal violence screening for women presenting to the ED [18], thus shattering the myth of a taboo surrounding violence.
Our results also underline the strong correlation between violence and the consumption of psychotropic substances, in particular alcohol, which was involved in 29% of events. This figure probably underestimates the true involvement of psychotropic substances, as patients who were drunk or agitated at presentation were not approached in our study. But most of the included patients reported previous violent incidents associated with alcohol or psychotropic substances, well-known contributing factors amongst victims as well as aggressors [19].
Notably, only 21% of victims voluntarily expressed a wish to speak about their experience of violence to an ED doctor, even though violence was the motive for consultation in 28% of cases. This low number is all the more surprising as one person in three felt insecure (51% of women, which was three times more than amongst men; p <0.001). This statistic is unchanged since 2002, and is the more disconcerting since enquiries about security had been broached with only one in seven victims by the treating physician. Several factors may explain this low figure. Patients mostly speak of their experience of violence during the acute phase (24 h after injury) rather than later. Violence can be very personal, especially when it involves words and psychological violence. Our results reflect this subjectivity, particularly in the feeling of insecurity and verbal abuse.
Interestingly, a significant number of patients were reticent about giving their consent, particularly those aged 55 years and over: 3.3% compared with 0.6% amongst those 16–34 years old. Numbers participating in our study were very high (86%) and the majority of patients were pleased to complete the questionnaire while they waited to be attended to in the ED. This high participation rate may be explained by the fact that both investigators took time to discuss matters with patients and to explain the purpose of the study.
According to these results, the problem of violence should deserve more consideration in primary medical consultations. There are currently no clear guidelines for general practitioners in Switzerland on violence screening. Given the participation rate, patients appear willing to talk about it without hesitation; thus earlier screening could prevent the health and economic consequences among this patient group.
Our figures must be interpreted with care because of several factors; patients aged 16–34 years were overrepresented in the total number of persons consulting the ED in the month of September 2016, rising from 30% to 38% (table 2), whereas the numbers of persons 55 years and over dropped from 43% to 35%, and the proportion of those of intermediate age (35–54 years) stayed the same. There is a possible sampling bias to take into account. Compared with the study of 2002, the sampled contained more young, male and single patients. They were therefore more likely to experience violence. Compared with the Vaud canton population, people of 20–39 years were overrepresented in our 2016 sample at 39% versus 28% [20]. It is also likely that this number was underestimated because of a detection bias, especially as some patients were accompanied by their partner. The questionnaire was completed alone and confidentially, but they may have still been reluctant to report violence objectively.
Nevertheless, the methodology of our study excluded those without a decision-making capacity, and the majority of these were aged with polymorbidity. An overrepresentation of the prevalence of violence is thus expected because of our exclusion criteria. The high rate of participation is representative of the number of patients who met our inclusion criteria, and one of the limitations of the study is that many agitated patients who could not be approached were not ultimately identified. There was a logistical limit to our study, with only two principal investigators, which was optimised with 3 × 8 hour survey schedules, equally distributed over weekends, to cover all time slots over the month of September 2016. During the time period a total of 3337 patients came to the ED. Patients in the emergency observation unit were not included (n = 402), and a total of 730 (24.9%) could be approached (fig. 1).
Conversely, certain patients consulting because of violence were not included for several reasons, notably because of agitation or diminished mental capacity, thus contributing to an underestimation of the prevalence of violence.
The Partner Violence Screening questionnaire was initially developed as a questionnaire for domestic violence screening. It may not be ideal for the evaluation of other types of violence, but was previously used in the princeps study, allowing for a comparison of the change in violence prevalence over time in our ED [8]. The questionnaire was filled out manually on paper rather than on an electronic tablet, which would have been probably a better method as it might have facilitated announcing violence and enabled interaction [21].
Our socio-historical context has also changed, and the definition of and reaction to violence has likewise changed during the last few years. Violence was previously understood as being physical, but now the comprehension of violence includes verbal assault, including attacks on human dignity. The level of tolerance to violence has also diminished, and as a result people are possibly more likely to report it [22].
The current prevalence of violence self-reported by patients attending our ED is now one in five. Single Swiss men consulting because of injury were the largest group. Women remained prone to domestic violence, which is too little taken into consideration by ED doctors, despite one in three affected women feeling personally insecure.
Our results underline the importance of a more systematic approach to questions of violence as presenting in the ED, essential to the identification and management of victims.
The appendix is available as a separate file at: https://smw.ch/article/doi/smw.2019.20147.
No financial support and no other potential conflict interest relevant to this article was reported.
1World Health Organization (WHO). WHO Global Consultation on Violence and Health. Violence: a public health. Geneva. document WHO/EHA/SPI. POA. 2). Available from: http://www. who. int/violenceprevention/approach/definition/en; 1996.
2Killias M, Staubli S, Biberstein L, Bänziger M, Iadanza S. Sondage au sujet des expériences et opinions sur la criminalité à Neuchâtel. Institut de Criminologie de l’Université de Zürich; 2011. Available from: https://www.fr.ch/sites/default/files/2018-07/icvs_2011_canton_fribourg.pdf.
3Vilpert S. Consultations dans un service d’urgence en Suisse. Neuchâtel: Obsan: Observatoire suisse de la santé; 2013. Available from: https://www.obsan.admin.ch/sites/default/files/publications/2015/obsan_bulletin_2013-03_f.pdf
4 Waalen J , Goodwin MM , Spitz AM , Petersen R , Saltzman LE . Screening for intimate partner violence by health care providers. Barriers and interventions. Am J Prev Med. 2000;19(4):230–7. doi:.https://doi.org/10.1016/S0749-3797(00)00229-4
5 Della Rocca GJ , Sprague S , Dosanjh S , Schemitsch EH , Bhandari M . Orthopaedic surgeons’ knowledge and misconceptions in the identification of intimate partner violence against women. Clin Orthop Relat Res. 2013;471(4):1074–80. doi:.https://doi.org/10.1007/s11999-012-2749-x
6 Abbott J , Johnson R , Koziol-McLain J , Lowenstein SR . Domestic violence against women. Incidence and prevalence in an emergency department population. JAMA. 1995;273(22):1763–7. doi:.https://doi.org/10.1001/jama.1995.03520460045033
7 From the Centers for Disease Control and Prevention. Emergency department response to domestic violence--California, 1992. JAMA. 1993;270(10):1174–6. doi:.https://doi.org/10.1001/jama.1993.03510100024008
8 Hofner M-C , Python NV , Martin E , Gervasoni JP , Graz B , Yersin B . Prevalence of victims of violence admitted to an emergency department. Emerg Med J. 2005;22(7):481–5. doi:.https://doi.org/10.1136/emj.2003.013979
9 Kyriacou DN , Anglin D , Taliaferro E , Stone S , Tubb T , Linden JA , et al. Risk factors for injury to women from domestic violence. N Engl J Med. 1999;341(25):1892–8. doi:.https://doi.org/10.1056/NEJM199912163412505
10 Arslan ED , Solakoglu AG , Komut E , Kavalci C , Yilmaz F , Karakilic E , et al. Assessment of maxillofacial trauma in emergency department. World J Emerg Surg. 2014;9(1):13. doi:.https://doi.org/10.1186/1749-7922-9-13
11 Rutschmann OT , Hugli OW , Marti C , Grosgurin O , Geissbuhler A , Kossovsky M , et al. Reliability of the revised Swiss Emergency Triage Scale: a computer simulation study. Eur J Emerg Med. 2018;25(4):264–9. doi:.https://doi.org/10.1097/MEJ.0000000000000449
12Lanfranconi B. Nouvelle montée de la violence chez les jeunes: résultats des statistiques de l’assurance-accidents selon la LAA. Lucerne; 2011. Available from: http://www.lips-org.ch/documents/SuvaStudieGewaltFrz-UpdateGewalt_20072011_F.pdf
13Statistiques sur l’aide aux victimes 2018, Criminalité et droit pénal. Office Fédérale de la Statistique; 2019. Available from: https://www.bfs.admin.ch/bfs/fr/home/statistiques/catalogues-banques-donnees/tableaux.assetdetail.8166964.html
14 Exadaktylos AK , Häuselmann S , Zimmermann H . Are times getting tougher? A six year survey of urban violence related injuries in a Swiss university hospital. Swiss Med Wkly. 2007;137(37-38):525–30.
15Domestic violence. Police Crime Statistics (PCS) 2018 [Internet]. Federal Statistical Office - Switzerland; 2019. Available from: https://www.bfs.admin.ch/bfs/en/home/statistics/crime-criminal-justice/police/domestic-violence.html
16Gillioz L, De Puy J, Ducret V. Domination et violence envers la femme dans le couple. Lausanne: Payot; 1997.
17Merçay C. Le recours aux services d’urgence en Suisse. Description des différences cantonales (Obsan Dossier 64) [Internet]. Neuchâtel: Observatoire suisse de la santé; 2018 p. 44. Available from: https://www.obsan.admin.ch/sites/default/files/publications/2018/obsan_dossier_64_0.pdf
18 Hurley KF , Brown-Maher T , Campbell SG , Wallace T , Venugopal R , Baggs D . Emergency department patients’ opinions of screening for intimate partner violence among women. Emerg Med J. 2005;22(2):97–8. doi:.https://doi.org/10.1136/emj.2002.002626
19 Kuendig H , Hasselberg M , Laflamme L , Daeppen J-B , Gmel G . Acute alcohol consumption and injury: risk associations and attributable fractions for different injury mechanisms. J Stud Alcohol Drugs. 2008;69(2):218–26. doi:.https://doi.org/10.15288/jsad.2008.69.218
20Canton de Vaud SCRIS. Chiffres-clés annuels de la population, 1981-2016 [Internet]. 2017. Available from: http://www.scris.vd.ch/Default.aspx?DocID=6808&DomId=2605
21 Rhodes KV , Lauderdale DS , He T , Howes DS , Levinson W . “Between me and the computer”: increased detection of intimate partner violence using a computer questionnaire. Ann Emerg Med. 2002;40(5):476–84. doi:.https://doi.org/10.1067/mem.2002.127181
22Mucchielli L. Une société plus violente?: Une analyse socio-historique des violences interpersonnelles en france, des années 1970 à nos jours. Déviance et Société [Internet]. 2008 [cited 2017 Nov 29];32(2):115. Available from: http://www.cairn.info/revue-deviance-et-societe-2008-2-page-115.htm
Joint first authors
TD, AO, OH, NRG, PC developed the protocol for this study. PC obtained ethics committee approval. TD and AO collected all the data and were assisted by OH and PC in the analysis and interpretation. All authors contributed to drafting and critical revision of the manuscript.
No financial support and no other potential conflict interest relevant to this article was reported.