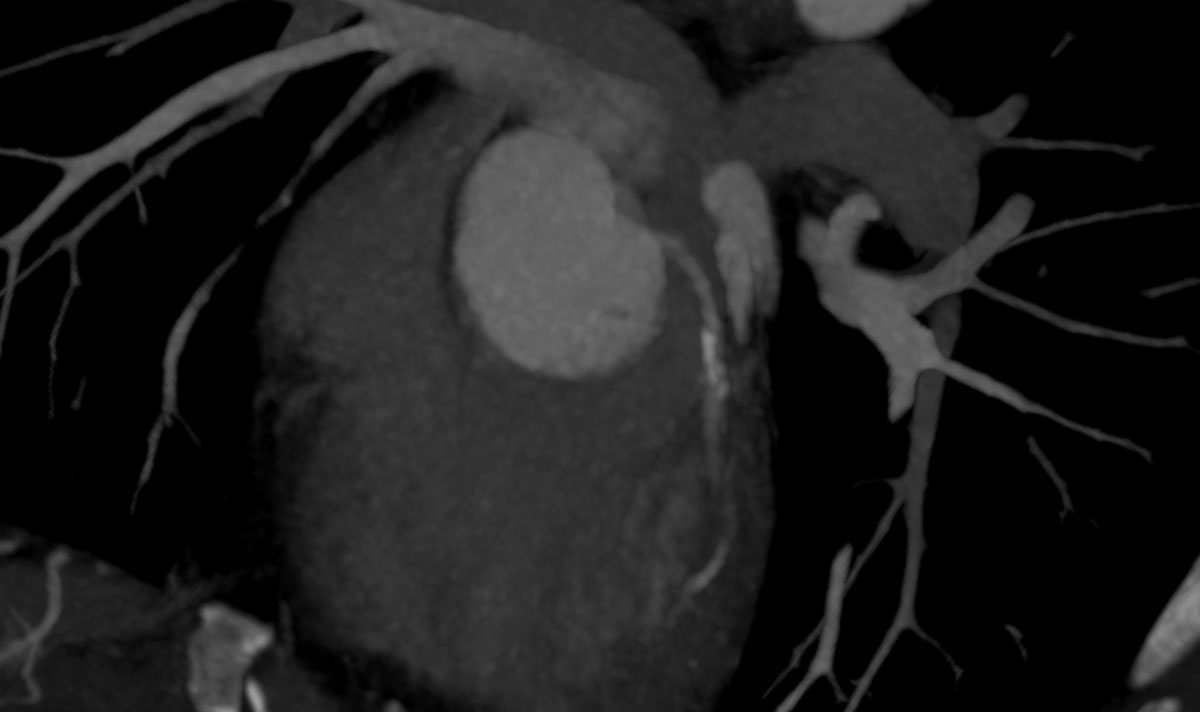
Figure 1 Axial CT scan of the left coronary artery in a 43-year old ED patient showing coronary artery calcification which led to a coronary angiogram.
DOI: https://doi.org/10.4414/smw.2019.20154
coronary artery calcification
computed tomography
computed tomographic angiography
erectile dysfunction
Erectile dysfunction (ED) is defined as “a continuous or repetitive inability to achieve or maintain an erection sufficient for satisfying sexual activity” [1]. Its prevalence is age-related and ranges from 2% in patients younger than twenty years of age and up to over 80% in octogenarians. It is estimated that 322 million males worldwide will suffer from ED in 2025 [2, 3].
In primary care, ED has been shown to be independently associated with cardiovascular diseases such as myocardial infarction, cardiac arrest and coronary heart disease, as well as with increased fasting glucose levels, diabetes mellitus and future coronary events [4]. Thus, ED has recently been identified as a predictor of generalised vascular disease, and besides the functional sexual impairment, symptoms of ED may be indicative of underlying risk factors or cardiovascular comorbidities [5, 6]. In addition, symptoms of ED may lead to a primary medical workup in patients with poor adherence to medical screening opportunities who would otherwise not undergo screening for cardiovascular risk factors. Hence, symptoms of ED may be a window into the entire cardiovascular system and indicative of the patient’s general health state.
Depending on the cause and severity of ED, various treatment options, such as phosphodiesterase-5 inhibitor therapy, testosterone replacement, intracavernous application of alprostradil, penile pumps and implants, are available. More recently, the advent of endovascular therapy of small-calibre arteries has facilitated minimally invasive stent revascularisation in patients with arteriogenic ED [7–11]. Subsequent to penile arterial duplex ultrasound and prior to angioplasty, computed tomography angiographic (CTA) workup of the pelvic arterial circulation is performed to complement haemodynamic findings, confirm suspected arterial obstructions, characterise their anatomical localisation and plan arterial access during angioplasty [9, 12].
Our hypothesis was that, in line with the above-described implications, CTA yields numerous incidental findings in addition to vascular obstructions in ED patients.
This single-centre investigation was approved by the local ethics committee and carried out at a Swiss vascular centre. Between March 2016 and January 2019, 239 patients presented for clinical and duplex-sonographic workup of ED of suspected vascular origin. Patients were referred from urologists, family physicians, internists or other vascular physicians. In this period, a total of 200 patients underwent CTA for suspected arteriogenic ED and provided written informed consent for participation in this investigation.
The inclusion criterion for this retrospective analysis was arteriogenic ED diagnosed based on findings from duplex ultrasound. ED was considered to be caused by arterial obstructions if arterial peak-systolic velocity in one or both cavernosal arteries was ≤0.3 m/s 10 minutes after an intracavernosal injection of 10 μg alprostadil at the proximal edge of the shaft of the penis [13].
In the case of pathological arterial flow on penile duplex ultrasound, patients were referred for CTA to further assess the anatomical level of arterial obstructions and for planning of endovascular intervention.
CT investigations were carried out on an Aquilion Prime of Toshiba. A 120-ml dose of Omniscan 350 mg/ml (GE Healthcare) contrast material was administered at a body weight of 80 kg with a flow of 4 ml/s. Two spirals were then dedicated: the first spiral from the level of the aortic bifurcation to the lower margin of scrotum and the second spiral from the lower margin of the scrotum to the jugulum. The rotation time was 0.45 seconds with a corresponding helical pitch of 65. The slice thickness was calibrated at 0.5 mm or rather 0.3 mm. The default was 2D depictions of planes in sagittal and coronal, and multiplanar representations in coronal and oblique-sagittal planes of the internal pudenda artery. An absolute exclusion criterion for CTA was insufficient renal function defined as glomerular filtration rate (GFR) lower than 40 ml/min and a relative exclusion criterion was allergy to contrast medium.
CT images were analysed independently by two experienced radiologists. In unclear cases, consensus was sought by both readers.
The following pre-existing risk factors were documented and defined as follows. Cigarette smokers were distinguished from non-smokers with smoking of 1 pack-year or more based on date of admission or chart documentation. Elevated lipoprotein(a) was assumed at levels ≥100 mg/l. The presence of arterial hypertension was defined as systolic blood pressure >140 mm Hg and/or diastolic blood pressure >80 mm Hg, or if the patient on any antihypertensive drug. The presence of diabetes mellitus was defined by fasting blood sugar >120 mg/dl or glycosylated haemoglobin >6% or if the patient was on hypoglycaemic drugs. The presence of hyperlipidaemia was defined by total cholesterol levels >5 mmol/l, or high-density lipoprotein cholesterol <1 mmol/l, or triglycerides > 2 mmol/l, or if the patient was taking any lipid-lowering drug. An ankle brachial pressure measurement with ratio <0.9 was considered to be indicative of peripheral arterial disease.
The following comorbidities were retrieved from patient chart diagnoses: coronary heart disease, previous surgery, relevant associated and/or currently treated illnesses such as prostatitis, hormonal imbalances, neurological anomalies, cerebrovascular diseases and history of dialysis, as well as previously diagnosed venous leak, alcohol consumption and drug abuse.
Incidental findings were classified based on a system used by Hoppe et al., 2006 [14]. After evaluating the total number of patients with incidental findings, these findings were then classified into those requiring immediate treatment, requiring deferred treatment or having relative or no clinical importance. Moreover, incidental findings were each classified into sub-categories cardiovascular, urogenital, visceral, musculoskeletal or other.
Findings requiring immediate further medical workup and/or treatment were coronary artery calcification (CAC), tumour findings, aortic aneurysm, pulmonary embolism, enlarged lymph nodes (larger than 1 cm) and stenosis with acute malperfusion of organs (kidney). Aortic aneurysms were assumed if the transverse arterial diameter was more than 1.5 times the size of the normal aorta. Accordingly, cases where the aortic diameter was enlarged below the above-mentioned threshold, arterial ectasia was assumed.
Vascular ectasia, enlarged truncus pulmonalis, complicated renal cysts, nephrolithiasis, prostate sclerosis, liver steatosis, colon diverticulosis, cholecystolithiasis, liver haemangioma, hernia, granuloma, nodules or marked organ enlargement (cardiomegaly, hepatomegaly, benign prostate hyperplasia, splenomegaly), lung abnormalities such as bronchiectasis and emphysema were defined as findings requiring deferred medical workup and/or treatment.
Findings with relative or no clinical importance were defined as those being unlikely to require treatment or further examination at a later time. These were anatomical variants of diseases such as non-irritant renal vascular disorders, aberrant subclavian artery, uncomplicated and non-irritant cysts (liver, kidney, pericardium), horseshoe kidney, skeletal degenerative diseases and arthritic joint abnormalities, lipoma, benign calcifications and other congenital anomalies.
Of the 200 male patients, with a mean age of 59.6 (±11.7) years, undergoing CTA for arterial ED, 181 patients (90.5%) were reported to have arterial obstructions of erection-related arteries plus incidental findings. A total of 168/200 (84.0%) patients exhibited multiple incidental CT findings. Table 1 illustrates risk factors and comorbidities of patients in the study.
Table 1 Pre-existing risk factors, comorbidities and medication in 200 patients with erectile dysfunction.
| Risk factors | n (%) | |
|---|---|---|
| Arterial hypertension | 92 (46.0) | |
| Elevated lipoprotein(a) | 85 (42.5) | |
| Hypercholesterolaemia | 85 (42.5) | |
| Cigarette smoking | 52 (26.0) | |
| Diabetes mellitus | 31 (15.5) | |
| Coronary artery disease / coronary heart disease | 30 (15.0) | |
| Peripheral artery disease | 16 (8.0) | |
| Chronic prostatitis | 10 (5.0) | |
| Post-prostate interventions / surgery | 6 (3.0) | |
| Alcohol abuse | 5 (2.5) | |
| Hormonal imbalances | 3 (1.5) | |
| Cerebrovascular diseases | 3 (1.5) | |
| Venous leak | 2 (1.0) | |
| Neurological diseases | 1 (0.5) | |
| Dialysis | 0 (0) | |
| Drug abuse | 0 (0) | |
| Medication | Aspirin | 121 (60.5) |
| Clopidogrel | 34 (17.0) | |
| Oral anticoagulants | 20 (10.0) | |
| Antihypertensives | 87 (43.5) | |
| Antidepressants | 10 (5.0) | |
| Antihistamines | 3 (1.5) | |
| Antipsychotic | 1 (0.5) | |
| Androgen antagonists | 0 (0) | |
A total of 85/200 patients (42.5%) exhibited incidental findings requiring immediate further medical workup and/or treatment. Of note, most incidental findings here were newly diagnosed cardiovascular conditions, with coronary artery calcification being the most prevalent finding followed by arterial aneurysms and incidentally detected embolism (table 2, figs 1, 2a and 2b ). Pancreatic and liver tumours were less frequent, but significant. Examples of incidentally diagnosed tumours are shown in figures 3 and 4 .
Table 2 Findings requiring immediate treatment in 85/200 patients with erectile dysfunction.
| Findings | n (%) | |
|---|---|---|
| Cardiovascular | Coronary artery calcification | 75 (37.5%) |
| Abdominal aortic aneurysm | 4 (2.0%) | |
| Thoracic aortic aneurysm | 3 (1.5%) | |
| Iliac artery aneurysm | 1 (0.5%) | |
| Pulmonary embolism | 1 (0.5%) | |
| Renal artery stenosis | 1 (0.5%) | |
| Urogenital | Urinary bladder tumour | 1 (0.5%) |
| Gastrointestinal | Pancreatic tumour | 3 (1.5%) |
| Liver tumour | 2 (1.0%) | |
| Other | Adrenal incidentaloma | 1 (0.5%) |
| Enlarged lymph nodes | 1 (0.5%) | |
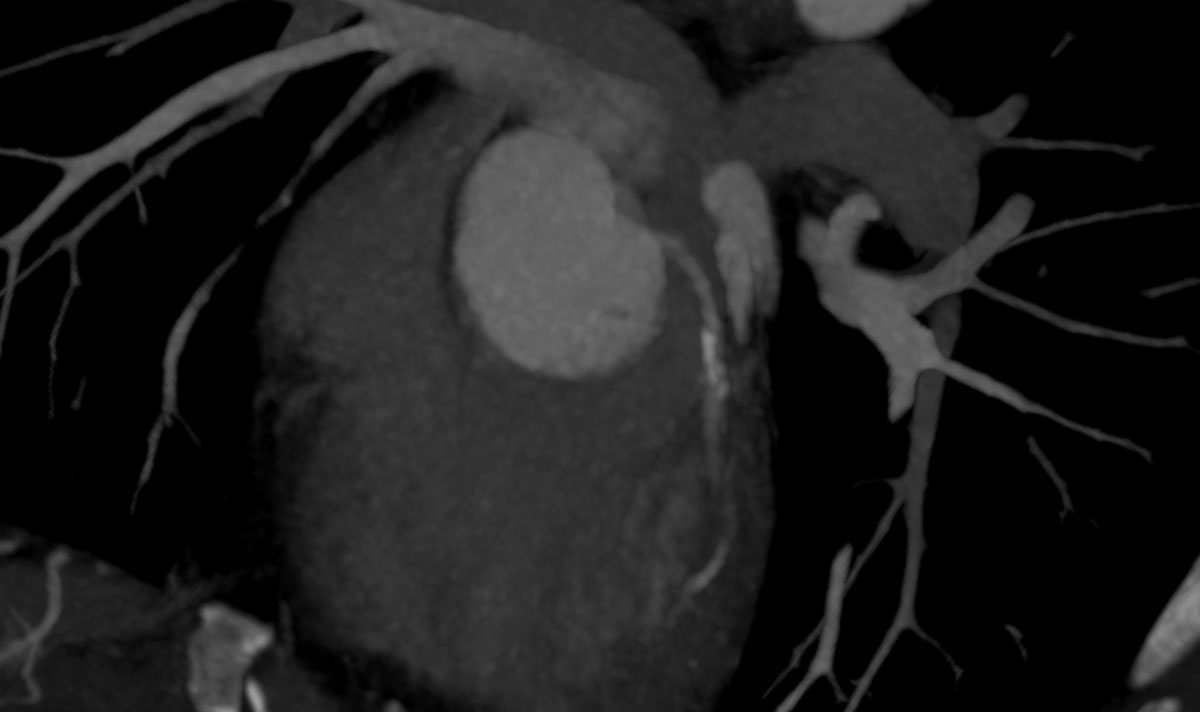
Figure 1 Axial CT scan of the left coronary artery in a 43-year old ED patient showing coronary artery calcification which led to a coronary angiogram.

Figure 2a Intra-arterial coronary angiogram showing a high-grade stenosis of the circumflex branch of the left coronary artery prior to drug eluting stent placement.
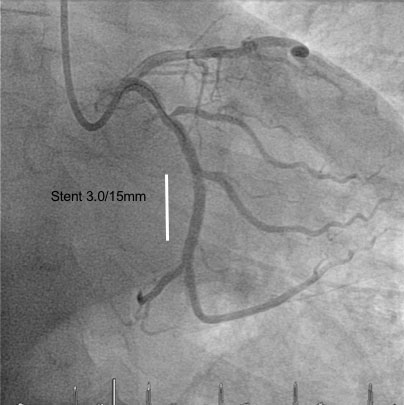
Figure 2b Intra-arterial coronary angiogram after drug eluting stent placement.

Figure 3 Axial CT scan of a neuroendocrine pancreatic tumour incidentally diagnosed in a 67-year old ED patient.
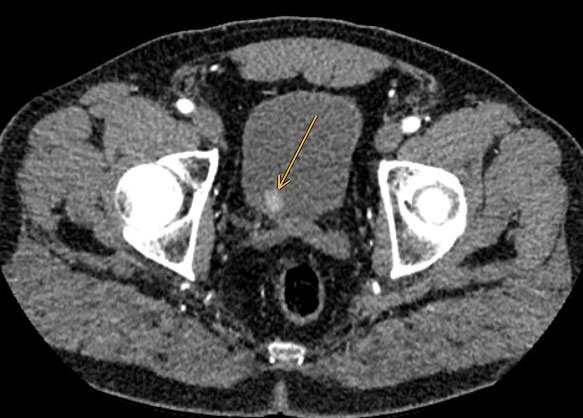
Figure 4 Axial CT scan of a bladder tumour incidentally diagnosed in a 62-year old ED patient with a history of cigarette smoking and cerebrovascular disease.
Incidental findings requiring deferred medical workup and/or treatment were detected in 175/200 patients (87.5%) (table 3). The findings with the highest prevalence were liver steatosis followed by colon diverticulosis and prostate hyperplasia.
Table 3 Findings requiring deferred treatment in 175/200 patients with erectile dysfunction.
| Findings | n (%) | |
|---|---|---|
| Cardiovascular | Arterial ectasia | 15 (7.5%) |
| Enlarged truncus pulmonalis | 1 (0.5%) | |
| Urogenital | Prostate hyperplasia | 77 (38.5%) |
| Prostate sclerosis | 11 (5.5%) | |
| Nephrolithiasis | 6 (3.0%) | |
| Complicated renal cyst | 5 (2.5%) | |
| Other urogenital findings | 6 (3.0%) | |
| Gastrointestinal | Liver steatosis | 112 (56.0%) |
| Colon diverticulosis | 95 (47.5%) | |
| Liver haemangioma | 11 (5.5%) | |
| Cholecystolithiasis | 8 (4.0%) | |
| Hepatomegaly | 3 (1.5%) | |
| Other gastrointestinal findings | 10 (5.0%) | |
| Musculoskeletal | Umbilical hernia | 22 (11.0%) |
| Hiatal hernia | 21 (10.5%) | |
| Inguinal hernia | 7 (3.5%) | |
| Other | Lung granuloma | 34 (17.0%) |
| Lung emphysema | 15 (7.5%) | |
| Lung nodules | 14 (7.0%) | |
| Bronchiectasis | 13 (6.5%) | |
| Cardiomegaly | 10 (5.0%) | |
| Other | 41 (20.5%) | |
Finally, findings with little to no clinical importance were reported in 117 (58.5%) patients (table 4). These include uncomplicated renal cysts, spinal degeneration and renal vascular anomalies.
Table 4 Findings with little clinical importance in 117/200 patients with erectile dysfunction.
| Findings | n (% | |
|---|---|---|
| Cardiovascular | Renal artery anomaly | 25 (12.5%) |
| Lusorian artery | 2 (1.0%) | |
| Right descending aorta | 1 (0.5%) | |
| Urogenital | Uncomplicated renal cysts | 54 (27.0%) |
| Horseshoe kidney | 1 (0.5%) | |
| Gastrointestinal | Liver cysts | 24 (12.0%) |
| Other gastrointestinal findings | 2 (1.0%) | |
| Musculoskeletal | Spine degeneration | 38 (19.0%) |
| Hyperostosis thoracic spine | 6 (3.0%) | |
| Coxarthrosis | 6 (3.0%) | |
| Other musculoskeletal findings | 11 (5.5%) | |
| Other | Thyroid cysts | 6 (3.0%) |
| Lipoma | 4 (2.0%) | |
| Spleen cysts | 2 (1.0%) | |
| Other findings | 2 (1.0%) | |
Erectile dysfunction is a highly prevalent disorder in the western world. Although frequently misinterpreted as a mainly lifestyle-limiting condition, ED is a medically highly relevant problem in middle-aged men that frequently carries relevant comorbidities and may serve as a very important marker symptom for atherosclerosis [15].
A previous study by Mulhall and coworkers has shown that men with a diagnosis of ED had a doubled prevalence of any comorbidity (including arterial hypertension, other cardiovascular disease, diabetes mellitus, depression and benign prostatic hyperplasia) when compared with men without ED [16].
In the present study of patients undergoing contrast-enhanced CTA for workup of ED of arterial origin, a remarkable percentage exhibited incidental findings unrelated to ED that required immediate or deferred treatment. These incidental findings influenced the medical management of patients’ individual clinical situations and treatment pathways, and provided important information with regards to additional therapeutic consequences.
Most of the findings considered to require immediate treatment were related to CAC. CAC was seen on CT scans in over 37.5% of ED patients. Thus, coronary atherosclerosis was incidentally diagnosed in more than 20% of patients in our study. According to the American College of Radiology, assessing the presence of CAC on CT scans may be valuable to the patient and referring physician, either for reassurance that no CAC is present or to increase patient awareness of coronary heart disease risk, and to stimulate discussion and further workup of cardiac risk factors [17]. Thus, based on these findings, a significant number of previously asymptomatic patients may have had an additional benefit from the CT scan performed for workup of ED.
It is known that ED and coronary heart disease share most modifiable risk factors leading to atherosclerosis [18, 19]. Since erection-related arteries have a smaller diameter than coronary arteries, the earliest manifestation of cardiovascular disease may be ED [5]. A recent meta-analysis by Dong et al. supports an increased risk of cardiovascular disease, stroke and all-cause mortality in men with ED [20]. Additionally, in a multi-ethnic study of atherosclerosis, ED was an independent predictor of myocardial infarction, cardiac arrest, fatal acute coronary syndrome und fatal stroke [18].
Aorto-iliac aneurysms were incidentally diagnosed in a total of 4% of ED patients in our present study. It remains unclear whether ED is an independent predictor of arterial aneurysm or whether the co-prevalence with cardiovascular risk factors influenced this finding. To our knowledge, the incidence of arterial aneurysms has not been studied in an ED population so far. However, several studies have addressed the prevalence of ED in men with abdominal aortic aneurysm prior to surgical intervention and revealed pre-operative ED rates to range from 10.3% to 74% [21–27].
Tumour findings deemed to require immediate attention were observed in 3% in our sample population. Thus, the CT scan changed treatment pathways in a considerable number of patients in the present series, based on suspicion of neoplasm [28]. This finding is not entirely new since it was previously shown that the incidence of cancer 5 years after an ED diagnosis is significantly higher when compared with that of the general population [29]. This finding further supports the medical burden associated with ED.
Liver steatosis led the findings of diseases that were deemed to require deferred treatment. Since the rate of reported alcohol abuse was comparatively low in our study, we suspect that this phenomenon may be attributed to nonalcoholic fatty liver disease. A recent study conducted by Hasanain et al. proved that ED is a common disorder in male patients with nonalcoholic fatty liver disease, with insulin resistance and low serum testosterone as contributing factors to its development. It was suggested that treatment of insulin resistance may improve erectile function and decrease the grade of hepatic steatosis [30].
Diverticular disease of the colon is among the most prevalent conditions in western society and is among the leading reasons for outpatient visits and causes of hospitalisation [31]. Accordingly, more than 50% of patients deemed to require deferred treatment exhibited colonic diverticulosis.
Finally, prostate hyperplasia was found in every third ED patient undergoing CTA. The connection between prostate hyperplasia and ED is quite complex and it was previously reported that 70% of men with prostate hyperplasia have an associated ED [32–34]. Thus, our imaging study confirms a close interrelation of prostate hyperplasia and ED.
Various other studies have investigated the incidence of incidental findings depicted in CT scans for various conditions such as aortic dissection [35], medical check-up [36], aortic valve stenosis [37], coronary artery disease [38], acute flank pain [14] and upper limb vascular disease [39], and on cardiac CT [40]. Prabhakar assessed incidental findings during evaluation for aortic dissection in the emergency department in 370 patients with a mean age of 63 years [35]. Similarly to our series, almost 90% of patients had at least one incidental finding, with aspiration pneumonia, pleural effusion and pericardial effusion being the most prevalent findings. In that study, severe arterial stenosis (in femoral, renal and subclavian arteries) was found in less than 7.0% of the cohort, which is more than found in our cohort.
In a study by Millor and colleagues of 6516 patients with mean age of 58.4 years undergoing whole body CT scans for medical check-up, incidental findings were found in 93% of patients. Of these, 1.47% were primary tumours (96 in total with 35 cases kidney related and 15 lung related), whereas 3% of our cohort had incidental findings that were tumour related. Abnormal results in men were significantly higher than in women in this study [36].
Hinton and coworkers investigated 652 patients with mean age of 82 undergoing CT prior to transcatheter aortic valve intervention [37]. Clinically significant incidental findings were detected in 95.6% of patients. In summary, 14% of patients had at least one significant incidental finding, with possible malignancy in 74% of that subgroup. Of note, patients were significantly older than the present cohort and, given that they were investigated for minimal-invasive aortic valve stenosis, they were often burdened with multiple comorbidities.
Karius and colleagues investigated a cohort of 3898 patients (mean age not specified) without significant coronary artery disease over 14 years [38]. Incidental findings were seen in a total of 30.2% patients, with lung cancer being most frequently detected. Moreover, vascular incidental findings were seen in 0.5% of patients. In comparison, incidental vascular findings were seen in 52% in our cohort owing to the design of our study, which focused only on males and contrast-enhanced CTA for workup of ED of arterial origin.
Hoppe and colleagues evaluated CT findings in 1500 patients examined for flank pain only with mean age of 50. However, patients analysed in the Hoppe paper were significantly younger than those in the present series. Tumour findings that needed immediate attention accounted for 3% of our sample population. These included liver, pancreas and urinary bladder tumours. In comparison with Hoppe’s study, which revealed multiple tumours of various origins, with an incidence of only 5.8% only after application of contrast medium. Without contrast medium, there was a much higher percentage of patients with tumour findings. Besides, all tumour patients included in our study were categorised as needing immediate treatment, whereas Hoppe linked them with deferred treatment. In the Hoppe study there were initially 10 patients thought to have prostate cancer, but upon application of contrast there were 4, of whom only 3 were surgically treated. We found that 70% of men in our cohort with benign prostatic hypertrophy have ED, but in Hoppe’s research, the number of benign prostatic hypertrophy cases seemed significantly lower at 57/1500 patients [14].
Nourzaie and associates investigated frequency of incidental findings in upper limb CT scans, focusing on undiagnosed malignancies [39]. A total of 70.3% out of 1383 patients with a mean age of 59 had incidental findings. In that series, 8.4% of incidental findings, which included newly diagnosed malignancies or cancer progression, were deemed to be of immediate clinical significance and were lower in frequency when compared with our series.
In a systematic review of papers published between 2006 and 2018, Fernando and colleagues found incidental findings in 45% of cardiac CTs in a cohort of over 40,000 patients with mean age of 60 years. The five most commonly reported incidental findings were lung nodules or masses, lung parenchymal changes, lymphadenopathy, emphysema and liver nodules or cysts. Of note, CAC was seen in 42% of these patients, which is similar to the 37.5% witnessed in our cohort [40].
Our paper has several limitations. Since some patients came from long distances and to respect existing collaborations of their family physicians, they were not systematically seen by the same specialists. Therefore, we cannot provide complete follow-up with regards to incidental findings. Moreover, we did not quantify the extent of CAC. Thus, it may be that the clinical impact of coronary calcification may be overestimated in these imaging findings. However, since many patients presenting to our ED centre are naïve in terms of cardiovascular diagnostic workup and may not even have a family physician, we still feel that further scrutiny of imaging findings may lead to an early detection of medical conditions associated with morbidity and mortality that would otherwise go undiagnosed.
In summary, incidental findings were common among ED patients undergoing CTA for arterial workup. It is important not to limit examinations only to the detection of ED of arterial origin because other findings, mainly related to cardiovascular, gastrointestinal musculoskeletal and urogenital systems are rather common among ED patients. Thus, the benefit of CTA investigations in patients with ED of suspected arterial origin may extend beyond the anatomic description of arterial obstructions of erection-related arteries. Further studies assessing clinical endpoints are required to fully define the clinical yield of CT imaging aimed at detecting incidental findings besides arterial workup in ED patients.
We kindly acknowledge Lisa Sammarchi and Simon Weber for their help in data handling within the present study.
No financial support and no other potential conflict of interest relevant to this article were reported.
1 Castro RP , Hernández PC , Casilda RR , García JR , Tapia MJR . Epidemiología de la disfunción eréctil. Factores de riesgo [Epidemiology of erectile dysfunction. Risk factors]. Arch Esp Urol. 2010;63(8):637–9. Article in Spanish.
2 Feldman HA , Goldstein I , Hatzichristou DG , Krane RJ , McKinlay JB . Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151(1):54–61. doi:.https://doi.org/10.1016/S0022-5347(17)34871-1
3 Aytaç IA , McKinlay JB , Krane RJ . The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int. 1999;84(1):50–6. doi:.https://doi.org/10.1046/j.1464-410x.1999.00142.x
4 Grover SA , Lowensteyn I , Kaouache M , Marchand S , Coupal L , DeCarolis E , et al. The prevalence of erectile dysfunction in the primary care setting: importance of risk factors for diabetes and vascular disease. Arch Intern Med. 2006;166(2):213–9. doi:.https://doi.org/10.1001/archinte.166.2.213
5 Gandaglia G , Briganti A , Montorsi P , Mottrie A , Salonia A , Montorsi F . Diagnostic and Therapeutic Implications of Erectile Dysfunction in Patients with Cardiovascular Disease. Eur Urol. 2016;70(2):219–22. doi:.https://doi.org/10.1016/j.eururo.2016.01.054
6 Caretta N , De Rocco Ponce M , Minicuci N , Palego P , Valente U , Garolla A , et al. Penile doppler ultrasound predicts cardiovascular events in men with erectile dysfunction. Andrology. 2019;7(1):82–7. doi:.https://doi.org/10.1111/andr.12561
7 Diehm N , Borm AK , Keo HH , Wyler S . Interdisciplinary options for diagnosis and treatment of organic erectile dysfunction. Swiss Med Wkly. 2015;145:w14268. doi:.https://doi.org/10.4414/smw.2015.14268
8 Diehm N , Marggi S , Ueki Y , Schumacher D , Keo HH , Regli C , et al. Endovascular Therapy for Erectile Dysfunction-Who Benefits Most? Insights From a Single-Center Experience. J Endovasc Ther. 2019;26(2):181–90. doi:.https://doi.org/10.1177/1526602819829903
9 Rogers JH , Goldstein I , Kandzari DE , Köhler TS , Stinis CT , Wagner PJ , et al. Zotarolimus-eluting peripheral stents for the treatment of erectile dysfunction in subjects with suboptimal response to phosphodiesterase-5 inhibitors. J Am Coll Cardiol. 2012;60(25):2618–27. doi:.https://doi.org/10.1016/j.jacc.2012.08.1016
10 Doppalapudi S , Shukla P , Kolber M , Singh M , Fischman A , Rastinehad A . Endovascular therapy for vasculogenic erectile dysfunction: a systematic review of arterial and venous therapies. J Vasc Interv Radiol. 2019;30(8):1251–1258.e2. doi:. https://doi.org/10.1016/j.jvir.2019.01.024
11 Baumann F , Hehli D , Makaloski V , Schumacher M , Schönhofen H , Diehm N . Erectile dysfunction - overview from a cardiovascular perspective. Vasa. 2017;46(5):347–53. doi:.https://doi.org/10.1024/0301-1526/a000627
12 Wang TD , Lee WJ , Yang SC , Lin PC , Tai HC , Hsieh JT , et al. Safety and six-month durability of angioplasty for isolated penile artery stenoses in patients with erectile dysfunction: a first-in-man study. EuroIntervention. 2014;10(1):147–56. doi:.https://doi.org/10.4244/EIJV10I1A23
13 Altinkilic B , Hauck EW , Weidner W . Evaluation of penile perfusion by color-coded duplex sonography in the management of erectile dysfunction. World J Urol. 2004;22(5):361–4. doi:.https://doi.org/10.1007/s00345-004-0423-y
14 Hoppe H , Studer R , Kessler TM , Vock P , Studer UE , Thoeny HC . Alternate or additional findings to stone disease on unenhanced computerized tomography for acute flank pain can impact management. J Urol. 2006;175(5):1725–30, discussion 1730. doi:.https://doi.org/10.1016/S0022-5347(05)00987-0
15 Feldman HA , Johannes CB , Derby CA , Kleinman KP , Mohr BA , Araujo AB , et al. Erectile dysfunction and coronary risk factors: prospective results from the Massachusetts male aging study. Prev Med. 2000;30(4):328–38. doi:.https://doi.org/10.1006/pmed.2000.0643
16 Mulhall JP , Luo X , Zou KH , Stecher V , Galaznik A . Relationship between age and erectile dysfunction diagnosis or treatment using real-world observational data in the USA. Int J Clin Pract. 2016;70(12):1012–8. doi:.https://doi.org/10.1111/ijcp.12908
17 Munden RF , Carter BW , Chiles C , MacMahon H , Black WC , Ko JP , et al. Managing Incidental Findings on Thoracic CT: Mediastinal and Cardiovascular Findings. A White Paper of the ACR Incidental Findings Committee. J Am Coll Radiol. 2018;15(8):1087–96. doi:.https://doi.org/10.1016/j.jacr.2018.04.029
18 Uddin SMI , Mirbolouk M , Dardari Z , Feldman DI , Cainzos-Achirica M , DeFilippis AP , et al. Erectile dysfunction as an independent predictor of future cardiovascular events: The multi-ethnic study of atherosclerosis. Circulation. 2018;138(5):540–2. doi:. https://doi.org/10.1161/CIRCULATIONAHA.118.033990
19 Allen MS , Walter EE . Erectile Dysfunction: An Umbrella Review of Meta-Analyses of Risk-Factors, Treatment, and Prevalence Outcomes. J Sex Med. 2019;16(4):531–41. doi:.https://doi.org/10.1016/j.jsxm.2019.01.314
20 Dong JY , Zhang YH , Qin LQ . Erectile dysfunction and risk of cardiovascular disease: meta-analysis of prospective cohort studies. J Am Coll Cardiol. 2011;58(13):1378–85. doi:.https://doi.org/10.1016/j.jacc.2011.06.024
21 Regnier P , Lareyre F , Hassen-Khodja R , Durand M , Touma J , Raffort J . Sexual Dysfunction After Abdominal Aortic Aneurysm Surgical Repair: Current Knowledge and Future Directions. Eur J Vasc Endovasc Surg. 2018;55(2):267–80. doi:.https://doi.org/10.1016/j.ejvs.2017.11.028
22 Majd P , Ahmad W , Luebke T , Gawenda M , Brunkwall J . Impairment of erectile function after elective repair of abdominal aortic aneurysm. Vascular. 2016;24(1):37–43. doi:.https://doi.org/10.1177/1708538115577290
23 Ballard JL , Abou-Zamzam AM, Jr , Teruya TH , Harward TRS , Flanigan DP . Retroperitoneal aortic aneurysm repair: long-term follow-up regarding wound complications and erectile dysfunction. Ann Vasc Surg. 2006;20(2):195–9. doi:.https://doi.org/10.1007/s10016-006-9014-2
24 Lederle FA , Johnson GR , Wilson SE , Acher CW , Ballard DJ , Littooy FN , et al.; Aneurysm Detection and Management Veterans Affairs Cooperative Study. Quality of life, impotence, and activity level in a randomized trial of immediate repair versus surveillance of small abdominal aortic aneurysm. J Vasc Surg. 2003;38(4):745–52. doi:.https://doi.org/10.1016/S0741-5214(03)00423-3
25 Unno N , Inuzuka K , Yamamoto N , Sagara D , Suzuki M , Konno H . Preservation of pelvic circulation with hypogastric artery bypass in endovascular repair of abdominal aortic aneurysm with bilateral iliac artery aneurysms. J Vasc Surg. 2006;44(6):1170–5. doi:.https://doi.org/10.1016/j.jvs.2006.08.011
26 Koo V , Lau L , McKinley A , Blair P , Hood J . Pilot study of sexual dysfunction following abdominal aortic aneurysm surgery. J Sex Med. 2007;4(4 Pt 2):1147–52. doi:.https://doi.org/10.1111/j.1743-6109.2006.00343.x
27 Lee ES , Kor DJ , Kuskowski MA , Santilli SM . Incidence of erectile dysfunction after open abdominal aortic aneurysm repair. Ann Vasc Surg. 2000;14(1):13–9. doi:.https://doi.org/10.1007/s100169910003
28 Resorlu M , Arslan M , Karatag O , Adam G . Thorax Computed Tomography Findings in Patients with Erectile Dysfunction. J Clin Imaging Sci. 2017;7:25. doi:.https://doi.org/10.4103/jcis.JCIS_32_17
29 Chung SD , Kang JH , Liao CH , Chiu KM , Lin HC . Increased risk for cancer following erectile dysfunction: a nationwide population-based follow-up study. J Sex Med. 2011;8(5):1513–20. doi:.https://doi.org/10.1111/j.1743-6109.2010.02076.x
30 Hasanain AFA , Mahdy RE , Mahran AMA , Safwat ASM , Mohamed AO , Abdel-Aal SM . Erectile dysfunction in patients with nonalcoholic fatty liver disease. Arab J Gastroenterol. 2017;18(1):21–4. doi:.https://doi.org/10.1016/j.ajg.2017.02.002
31 Weizman AV , Nguyen GC . Diverticular disease: epidemiology and management. Can J Gastroenterol. 2011;25(7):385–9. doi:.https://doi.org/10.1155/2011/795241
32 Calogero AE , Burgio G , Condorelli RA , Cannarella R , La Vignera S . Epidemiology and risk factors of lower urinary tract symptoms/benign prostatic hyperplasia and erectile dysfunction. Aging Male. 2019;22(1):12–9. doi:.https://doi.org/10.1080/13685538.2018.1434772
33 Kardasevic A , Milicevic S . The Correlation Between Prostate Volume in Patients with Benign Prostatic Hyperplasia in Relation to Erectile Dysfunction. Med Arch. 2016;70(6):449–52. doi:.https://doi.org/10.5455/medarh.2016.70.449-452
34 Kardasevic A , Milicevic S . Correlation of Subjective Symptoms in Patients with Benign Prostatic Hyperplasia and Erectile Dysfunction. Med Arch. 2017;71(1):32–6. doi:.https://doi.org/10.5455/medarh.2017.71.32-36
35 Prabhakar AM , Le TQ , Abujudeh HH , Raja AS . Incidental findings and recommendations are common on ED CT angiography to evaluate for aortic dissection. Am J Emerg Med. 2015;33(11):1639–41. doi:.https://doi.org/10.1016/j.ajem.2015.07.078
36 Millor M , Bartolomé P , Pons MJ , Bastarrika G , Beloqui Ó , Cano D , et al. Whole-body computed tomography: a new point of view in a hospital check-up unit? Our experience in 6516 patients. Radiol Med (Torino). 2019; Epub ahead of print. doi:.https://doi.org/10.1007/s11547-019-01068-y
37 Hinton J , Gough S , Ahmed H , Gabara L , Rawlins J , Calver A , et al. Frequency and impact of incidental findings on computed tomography during work-up for transcatheter aortic valve implantation: single centre experience and review of the literature. Br J Radiol. 2019;92(1102):20190344. doi:.https://doi.org/10.1259/bjr.20190344
38 Karius P , Lembcke A , Sokolowski FC , Gandara IDP , Rodríguez A , Hamm B , et al. Extracardiac findings on coronary computed tomography angiography in patients without significant coronary artery disease. Eur Radiol. 2019;29(4):1714–23. doi:.https://doi.org/10.1007/s00330-018-5688-4
39 Nourzaie R , Das J , Abbas H , Thulasidasan N , Gkoutzios P , Ilyas S , et al. Extravascular findings during upper limb computed tomographic angiography focusing on undiagnosed malignancy. World J Radiol. 2019;11(1):10–8. doi:.https://doi.org/10.4329/wjr.v11.i1.10
40 Kay FU , Canan A , Abbara S . Common Incidental Findings on Cardiac CT: a Systematic Review. Curr Cardiovasc Imaging Rep. 2019;12(6):21. doi:.https://doi.org/10.1007/s12410-019-9494-4
No financial support and no other potential conflict of interest relevant to this article were reported.