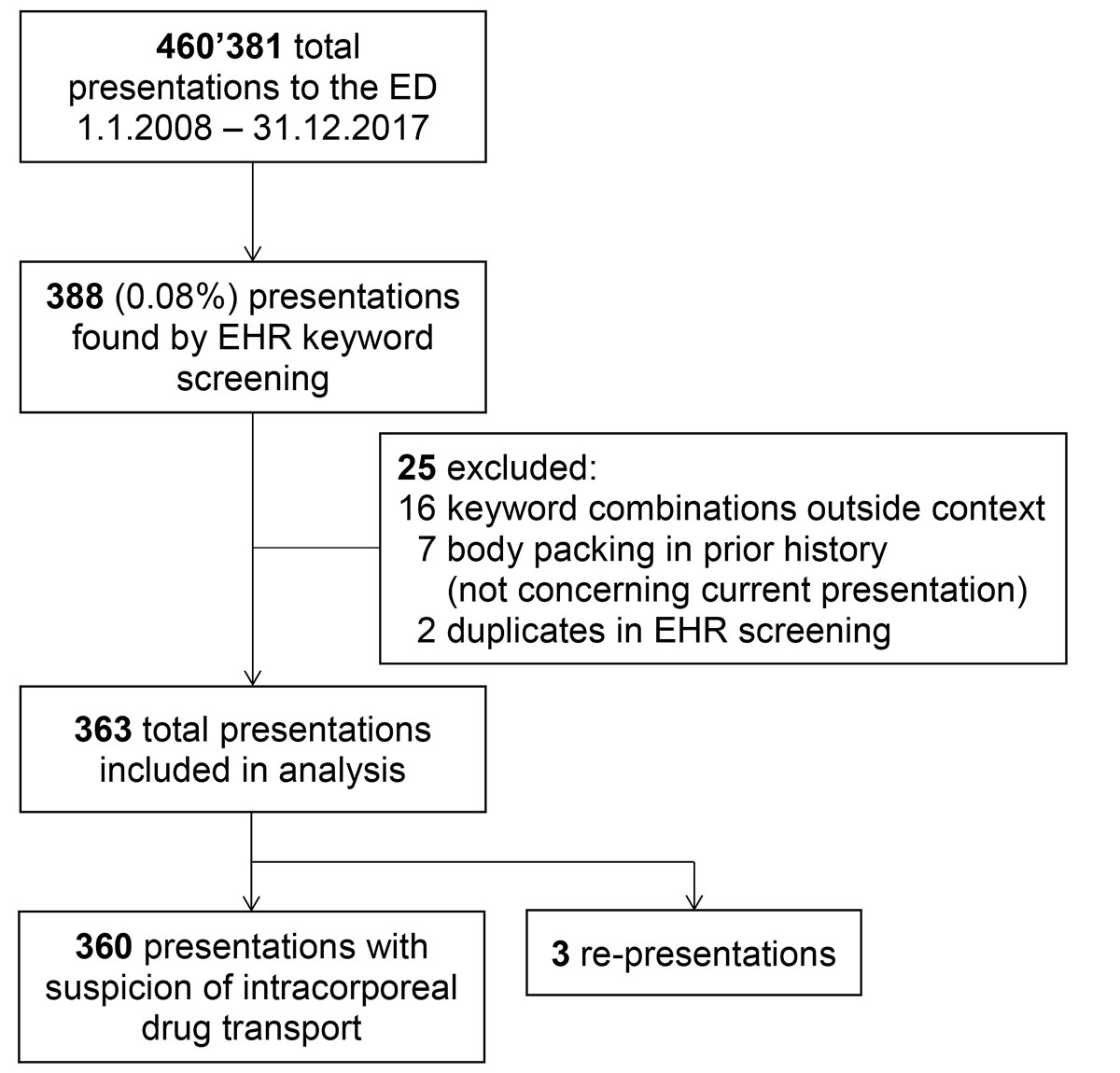
Figure 1 Patient selection with total ED presentations between January 1st 2008 and December 31th 2017, keyword screening of electronic health records (EHRs), exclusions and inclusion in final analysis.
DOI: https://doi.org/10.4414/smw.2019.20113
The transport of illegal substances in intracorporeal containers hidden in the gastrointestinal system or other body cavities is often used for drug trafficking. The first report was in to 1973, when two Canadian physicians first described a bowel obstruction secondary to the swallowing of a drug-filled condom [1].
Use of the human body for illegal drug transport has become increasingly common in recent years [2]. The fastest growing market for cocaine and heroin transported via this method is Europe. Therefore, Switzerland is among the main drug gateways to Europe due to its strategic position in the heart of Europe [3]. Being close to an international airport and to German and French borders, emergency physicians in Basel encounter an increasing demand to examine suspects.
Three ways of intracorporeal drug transport are commonly used: Body packing is the planned intra-abdominal transport by swallowing large amounts of drug containers. In body stuffing, small amounts of drugs are orally ingested, usually at short notice, when there is a risk of being searched or arrested. Body pushing is the insertion of containers into body cavities such as the rectum or vagina.
The first report evaluating all three ways of transport recently documented a Swiss University Hospital’s experience with body packing and body stuffing and showed very low complication rates [4].
Some Swiss emergency departments (EDs) prefer in-hospital observation, whereas others discharge the majority of positively tested subjects, assuming relative safety for this procedure. Furthermore, the topic of intracorporeal drug transport is under discussion in media and politics, and recent recommendations about the handling of suspected body packers endorsed in-hospital observation [5] owing to lack of evidence for the safety of outpatient observation.
Therefore, we conducted this retrospective study in order to analyse outcomes in all patients presenting to the Basel University Hospital ED with suspicion of intracorporeal drug transport over the last decade.
We conducted a single-centre retrospective study using electronic health records (EHRs) from the Emergency Department of the University Hospital of Basel, an academic tertiary-care hospital in north-western Switzerland with 700 beds and an annual census of more than 50,000 ED visits. The local ethics committee approved the study protocol and waived informed consent (EKNZ 2018-02113, www.eknz.ch).
To find every suspect referred to our ED over a period of 10 years, diagnosis and history of presenting complaints of EHRs were screened for combinations of keywords “body”, “pack”, “stuff” and “push”, between 1 January 2008 and 31 December 2017. Subsequently, duplicates in EHR screening, keyword combinations outside of the context of drug transport, and cases with intracorporeal drug transport in the prior history not concerning the current presentations were excluded (fig. 1). Suspects were mostly referred by police of the Canton of Basel-City or Swiss border guards, including suspects arriving at the international airport EuroAirport Basel-Mulhouse-Freiburg.
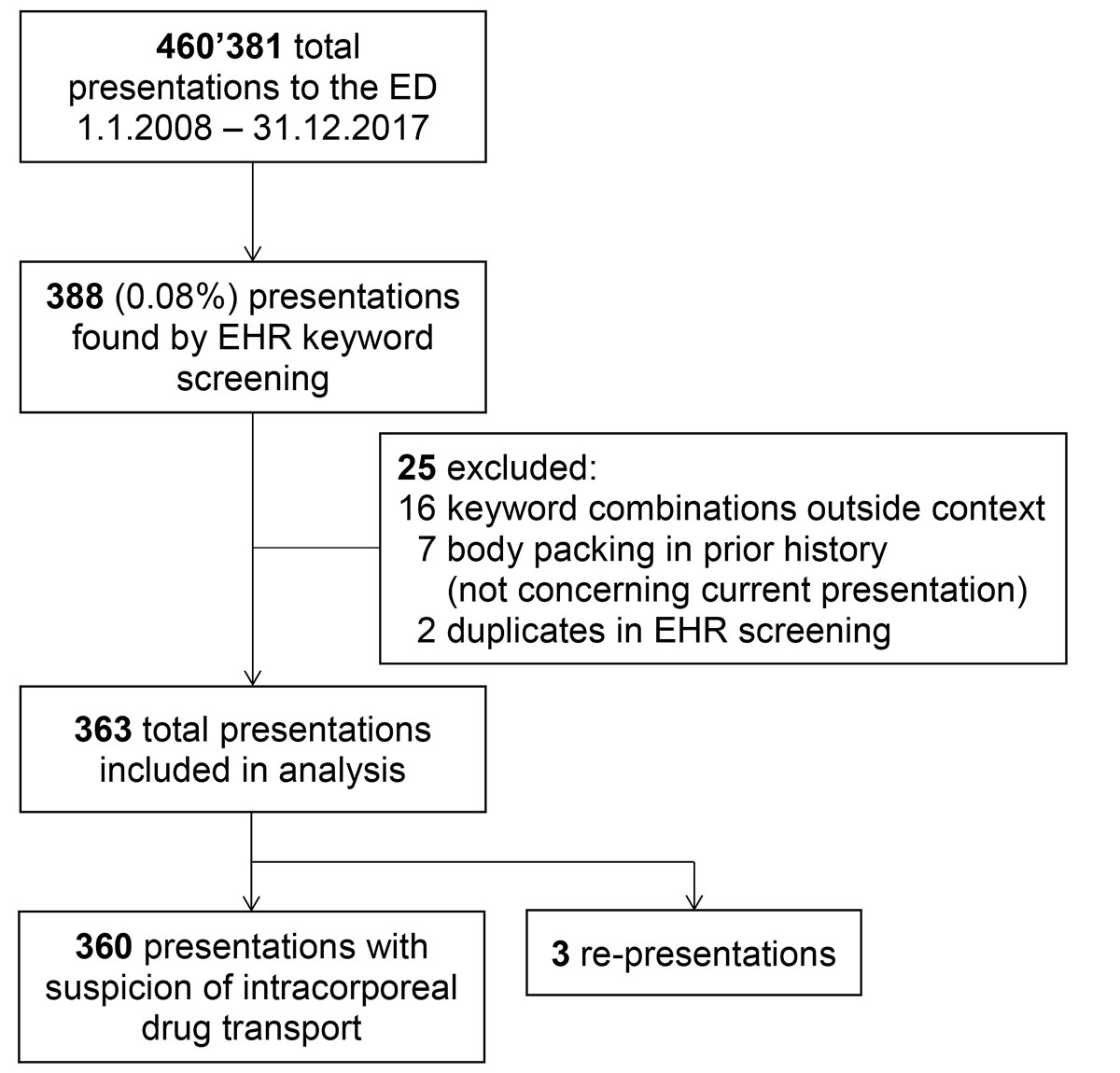
Figure 1 Patient selection with total ED presentations between January 1st 2008 and December 31th 2017, keyword screening of electronic health records (EHRs), exclusions and inclusion in final analysis.
Patient characteristics, Emergency Severity Index (ESI) levels at triage, imaging modalities and the results of imaging were assessed, the main outcome being surgical intervention during hospital and prison observation. The ESI is an ED triage algorithm that stratifies patients into five groups from 1 (most urgent) to 5 (least urgent) on the basis of acuity and resource needs. On the basis of diagnosis, history of presenting complaints and radiology reports, all suspects were categorised according to the three ways of intracorporeal drug transport. The study outcomes were ED and hospital length of stay (LOS), hospitalisation, admission to intensive care unit (ICU), surgical intervention and mortality (in-hospital and in-prison). A rate of surgical intervention (due to serious complications) of less than 5% was defined as safe in terms of management. This was determined by clinical experts in the field. LOS in the ED was calculated for in- and outpatients separately, the total LOS in hospital for inpatients, and the total LOS for all patients (in the ED for outpatients and in hospital for inpatients). The average costs per presentation were calculated using a standardised unit cost accounting.
Data were processed using Microsoft Excel, version 2016. The statistical analysis was performed using R version 3.4.1 (www.R-project.org). Results are presented as descriptive statistics, with categorical variables as absolute numbers and percent values, as well as continuous variables as medians and ranges or interquartile ranges (IQRs: 25th and 75th percentile). To illustrate the results, bar plots showing imaging modality and results and a Kaplan-Meier graph showing LOS were created.
It is stated in the Swiss Criminal Procedure Code and customs law that examinations of persons and interventions involving their physical integrity shall be carried out by a physician or other medical specialist [6, 7]. Medical imaging modalities are defined as part of the physical examination and also can only be ordered by physicians. Therefore, it is the task of physicians to verify if imaging can be done in a patient considering his or her health condition, especially when a suspect is underage or pregnant. Further, the Federal Customs Administration, namely border guards, may search a person or have a person physically examined on the basis of a suspicion that the person poses a risk or carries objects to be secured [7].
A statement of the Federal Customs Administration emphasises that physical examinations can be ordered only if they are proportionate and expedient, meaning if there is a compelling suspicion of body packing, the person is in a life-threatening condition, or no less drastic measure is available. Additionally, a written order must be provided by the commanding officer [8].
Furthermore, the Swiss Academy of Medical Sciences states in its recent guideline that detained persons have the same health-related rights as any other patient. As in any other medical situation, physicians acting in the capacity of an expert or therapist may carry out a diagnostic or therapeutic measure only after obtaining consent of the detained person. Only in-hospital observation is recommended for all presentations of body packing, and a second computed tomography (CT) scan after expulsion of packs is endorsed [5].
To support all medical professionals in the legally, ethically, and medically correct handling of suspects, our ED has introduced IT-based decision support, accessible under emergencystandards.com. Patients with a positive imaging result, but no high-risk factors, normal vital signs and no signs of a toxidrome can be handed over to the authorities for expulsion in prison [9]. High-risk patients undergo blood tests and are subsequently monitored for at least 6 hours. If symptoms, such as abdominal pain, occur during observation, suspects are admitted as patients; all other cases are transferred to prison. Factors indicating a high risk are based on literature data summarising factors indicating complications of concealed drugs and include symptoms such as abdominal pain, vomiting, poisoning and abnormal vital signs, as well as improvised packaging, high number of containers (>50), delayed passage of drug packets (>48 h), use of constipating agents and previous abdominal surgery [9].
To uphold confidentiality and protect the identity of suspects, our ED is equipped with specific facilities, namely a segregated path from entrance to the hospital, starting from separate medical triage facilities, segregated from waiting room patients and leading straight to the CT scanner. The responsible emergency physician has to inform each individual about the required procedure, and CT scans are not performed if the subject does not agree, or if scanning poses a risk (e.g., pregnancy).
After the responsible ED physician has decided to hand over a patient to the police for expulsion of the packs in prison, he or she is taken to the detention centre. The prison physician in charge examines the detainee transporting drugs intracorporeally. The detainee is subsequently monitored in a room with video surveillance and a portable body packer toilet for expulsion of the drug containers. Whenever the detainee reports symptoms – or if any complications are visible on video surveillance – the patient is immediately taken back to the ED of the University Hospital of Basel, which is nearby (1.3 km). After expulsion of the containers/packs or two normal bowel movements without packs while eating normally, the detainee is taken to a normal room in prison. The further stay in prison is decided by the court in charge.
We found 388 patient presentations with suspected intracorporeal drug transport by screening the diagnosis and history of presenting complaints in EHRs for combinations of keywords “body”, “pack”, “stuff” and “push”, between 1 January 2008 and 31 December 2017. All results with keyword combinations outside the context of drug transport (n = 16), presentations with intracorporeal drug transport in the prior history and not concerning the current presentations (n = 7), and duplicates in EHR screening (n = 2) were then excluded (fig. 1). Finally, we included 363 presentations of 347 patients for final analysis. Table 1 shows the baseline characteristics in detail. The median age was 35 years (range 19–64) and 46 (12.7%) were female. The median ESI level at triage was 4 of 5 possible levels (one external resource such as an imaging study needed), with 246 (76.9%) at level 4 out of 320 presentations with available ESI levels. In total, the rate of positive results of imaging was 81 (22.9%). We observed 36 instances of body packing, 10 of body stuffing and 15 of body pushing. Twenty presentations were combinations of the three methods, or indeterminate because they could not be classified owing to inconclusive radiology reports.
Table 1 Baseline characteristics.
| Total | Imaging positive | Imaging negative | ||
|---|---|---|---|---|
| Results of imaging, n (%) | 363* | 81 (22.9) | 268 (75.9) | |
| Female sex, n (%)† | 46 (12.7) | 6 (7.4) | 36 (13.4) | |
| Age, median (range)† | 35 (19–64) | 35 (20–59) | 35 (19–64) | |
| ESI levels, median (IQR)‡ | 4 (4–4) | 4 (3–4) | 4 (4–4) | |
| Imaging modalities, n (%)§ | X–ray (plain abdominal radiography) | 115 (31.9) | 20 (24.7) | 93 (34.7) |
| CT scan | 225 (62.3) | 57 (70.4) | 167 (62.3) | |
| X–ray and CT scan | 13 (3.6) | 4 (4.9) | 8 (3.0) | |
| Hospital admission, n (%) | 15 (4.1)¶ | 10 (12.3) | 4 (1.5) | |
| ED | 9 (60.0)¶ | 7 (70.0) | 1 (25.0) | |
| Ward | 1 (6.7) | 1 (10.0) | 0 (0.0) | |
| Intensive care unit | 5 (33.3) | 2 (20.0) | 3 (75.0) | |
| Total LOS, median (IQR) in hours‖,** | 1.8 (1.2–3.4) | 3.6 (2.3–7.1) | 1.5 (1.1–2.2) | |
| ED LOS outpatients, median (IQR) in hours** | 1.7 (1.2–2.8) | 3.4 (2.1–5.8) | 1.5 (1.1–2.2) | |
| ED LOS inpatients, median (IQR) in hours | 6.9 (3.2–13.5) | 7.1 (3.7–10.6) | 10.0 (3.6–17.0) | |
| Hospital LOS inpatients, median (IQR) in hours | 29.8 (17.5–47.6) | 29.8 (20.6–47.9) | 23.6 (8.9–40.3) | |
| Surgical intervention, n (%) | 0 (0) | 0 (0) | 0 (0) | |
| Mortality, n (%) | 0 (0) | 0 (0) | 0 (0) | |
CT = computed tomography; ED = emergency department; ESI = Emergency Severity Index; IQR = interquartile range; LOS = length of stay * Including 10 (2.8%) presentations without imaging and 4 (1.1%) indeterminate results on imaging † Calculated including 13 patients that presented twice with a second suspicion and 3 re-presentations ‡ Available for 320 (88.2%) presentations: level 1 (n = 1), level 2 (n = 15), level 3 (n = 52), level 4 (n = 246), level 5 (n = 6) § For 353 presentations with imaging (10 presentations without imaging) ¶ Including 1 presentation without imaging ‖ Total LOS calculated with ED LOS for outpatients and hospital LOS for inpatients ** ED LOS available for 269 (77.3%) of 348 outpatients
Of the 363 presentations, 334 patients presented once to our ED and 13 patients twice as a result of a second suspicion by police or border guards. The rate of positive results in these patients was 15.4% (2 out of 13) and median time to second suspicion was 8.6 months (range 1 day to 42 months). Three patients presented a second time to our ED one day after the initial presentation because of abdominal symptoms and a suspicion of intoxication, which could be ruled out in all three cases.
The number of suspects referred by border guards and police rose during the study decade, whereas the relative number of positive imaging results has remained almost stable over the 6 years from 2012 to 2017 (fig. 2).
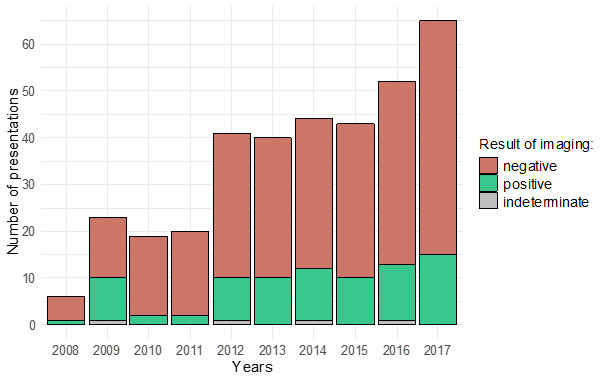
Figure 2 Results of imaging in presentations with suspicion of intracorporeal drug transport for the years 2008 to 2017.
We observed no severe or life-threatening complications or deaths in our cohort over the 10-year period. Additionally, no patient needed a surgical intervention.
Most of the patients with a positive result on imaging, 71 out of 81 (87.7%), were discharged and handed over to the police or border guards for expulsion of the packages in prison. Their median ED LOS was 3.4 hours (IQR 2.1–5.8). Within the study period of 10 years, 10 patients with positive results (12.3%) were observed in hospital (7 in a separate room in the ED, 2 in the intensive care unit, 1 on the ward) with a median hospital LOS of 29.8 hours (IQR 20.6–47.9). The maximum hospital LOS was 68.7 hours. The Kaplan-Meier graph (fig. 3) illustrates the total LOS – ED LOS for outpatients and hospital LOS for inpatients – stratified by result of imaging. ED LOS was available for 269 (77.3%) of 348 outpatients in total.
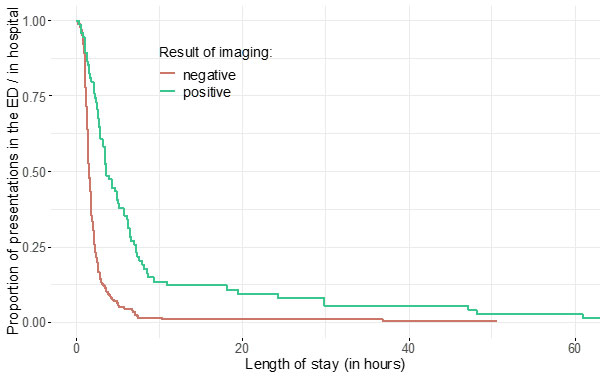
Figure 3 Kaplan-Meier plot of total length of stay (LOS) in hours, stratified by result of imaging, calculated with emergency department (ED) LOS for outpatients and hospital LOS for inpatients.
Of all patients with negative results on imaging (n = 268), 264 (98.5%) could be discharged after a median ED LOS of 1.5 hours (IQR 1.1-2.2), whereas 4 patients (1.5%) were admitted for reasons not associated with the suspicion of intracorporeal drug transport.
A cost analysis of 295 presentations with available data from the hospital’s administration database, based on a standardised unit cost accounting, resulted in an average of 650 Swiss francs per presentation.
We found ten presentations without imaging, including three men who refused imaging and were therefore handed over for observation in prison as they were asymptomatic and not at high risk. In the remaining presentations, there were no imaging studies because three women were pregnant, two patients removed or regurgitated the hidden container, and two were re-presentations who had imaging the day before. No rehospitalisation occurred in these presentations.
Plain abdominal radiography was used for all cases until April 2013, when our guideline on emergencystandards.com was changed because of the availability of new low-dose CT. Immediately after publication of the new guideline, all presentations underwent low-dose CT without contrast [10, 11] (fig. 4).
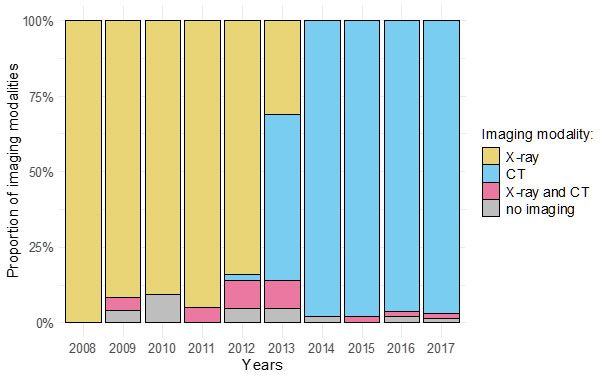
Figure 4 Imaging modalities in presentations with suspicion of intracorporeal drug transport for the years 2008 to 2017.
The number of suspects brought forward by police and border guards increased over the last decade, whereas the relative number of positive results remained stable over the last 6 years. We suspect the following reasons for the higher number of work-ups. On one hand, police and border guards might have information on an increase in local drug trafficking, or they might have a decreased threshold of suspicion. The Federal Customs Administration reported 105 body packers in 2012, which is an increase of 40% compared with previous years [12]. In 2018, intracorporeal drug transport was suspected in 237 persons across Switzerland [13].
On the other hand, body packers might use new wrapping techniques with lower radio-density, ultimately resulting in more false negative results [14]. Additionally, better training of radiologists in recognising intracorporeal containers could have led to an increase in positive findings. However, the change in radiological procedure from plain abdominal radiography to low-dose CT did not influence the number of positive results.
No severe or life-threatening complications were observed in our cohort, which meets our definition of less than 5% to be a safe management. This is comparable to the Lausanne cohort, as well as to bigger cohorts in Europe showing very low complication rates (1.2–2.3%) and no rupture of drug packages [4, 9, 15]. New wrapping techniques might reduce package rupture [14]. Only patients with proven body packs and high-risk features were recommended for further diagnostic work-up and observation, according to the largest published case series [9, 15]. Our findings question the traditional risk factors [9] and the necessity to observe all patients in hospital until expulsion of all drug packages [4, 16, 17]. Whereas some authors have claimed that in Europe patients are generally observed in hospital until complete expulsion of all packs, in some countries observation in prison is preferred if patients are asymptomatic and have no high-risk features [4, 9]. In Switzerland, the recently published guidelines of the Swiss Academy of Medical Sciences suggest in-hospital observation of all patients until complete expulsion, followed by a second CT scan [5]. Based on the very low rates of complications, interventions and revisits, this approach may be questioned. Considering waning resources in hospitals without prison department or high security ward, the outpatient procedure could safely be practiced.
At the same time, medical professionals, as well as police, border guards, and judicial authorities, always have to uphold the patient’s rights according to judicial and ethical guidelines, particularly in the vulnerable group involved in drug trafficking. On one hand, police and border guards have the duty to identify drug traffickers and therefore ask medical professionals to provide support for examining people when there is a compelling suspicion of intracorporeal drug transport. On the other hand, the suspects may be in a potentially life-threatening condition due to possible rupture of drug containers. Thus, a referral to a medical institution for initial evaluation seems of utmost importance. However, there is an ongoing debate whether prolonged monitoring in hospital is indeed necessary [5], our own data in 81 patients showing no evidence for rupture of packs, intoxication, or any life-threatening complications.
Moreover, we observed an immediate change of procedure after introduction of the new low-dose CT algorithm, most likely due to IT-based decision support. Obviously, this sort of decision support may have immediate impact on procedures effectively performed. Indeterminate results have therefore only been observed once in the last 200 presentations. Newer studies have confirmed that low-dose CT without contrast is the most powerful imaging modality for intracorporeal drug transport, providing definite diagnosis with roughly similar radiation as compared to plain radiographs [2, 14, 18].
The major limitations of this study are the retrospective design, which leads to the risk of different types of bias, most importantly inclusion bias, the single-centre design and the relatively small sample size. This reduces the power of the study and, possibly, the occurrence of serious complications. Since this study was based on electronic health records, there is a risk of documentation bias. Furthermore, there is a risk of both false positive and false negative results on imaging. In studies, sensitivity levels of plain abdominal radiography and in body packing ranged between 40 and 100% [2, 9, 18, 19], related to variations in drug type, degree of purity, packaging material used, location in gastrointestinal system and expertise of the radiologist [19]. The specificity of plain abdominal radiography is higher, at 90%, with hardened faeces, calcifications and gas possibly leading to false positive results [19]. Sensitivity of CT for the diagnosis of body packing, however, ranges between 96.5 and 100% and its specificity between 94.1 and 100% [2, 20, 21].
In the future, because of rising case numbers, efficient guidelines presenting a national consensus must be established to facilitate the diagnostic procedure in persons suspected of intracorporeal drug transport. Traditional risk factors, such as the number of body packs, need to be evaluated prospectively. Furthermore, as a result of the consistently low complication rates and waning resources in emergency departments, in-hospital observation may be questioned. The outpatient procedure commenced a decade ago can be recommended, on the basis of the data presented here and previous reports. Considering the ongoing discussion in the media and politics, we suggest prospectively validating medical, legal, and ethical guidelines across centres in Switzerland, with medical professionals, police and border guards. While reducing overtreatment by in-hospital observation in all patients, the rights of this vulnerable group of suspects of drug trafficking must be guaranteed.
We acknowledge the support of Klaus Baumgartl for the assistance with the electronic health records.
The University Hospital Basel funded this study.
RB is publisher of emergencystandards.com (medstandards.com), a symptom-based medical decision-support tool licensed to 150 European hospitals, owned by the University Hospital Basel. The authors declare no further conflict of interest.
1 Deitel M , Syed AK . Intestinal obstruction by an unusual foreign body. Can Med Assoc J. 1973;109(3):211–2.
2 Bulakci M , Cengel F . The role of radiology in diagnosis and management of drug mules: an update with new challenges and new diagnostic tools. Br J Radiol. 2016;89(1060):20150888. doi:.https://doi.org/10.1259/bjr.20150888
3 Cappelletti S . Medico-legal issues of body packing: what do clinicians need to know? Swiss Med Wkly. 2017;147:w14494. doi:.https://doi.org/10.4414/smw.2017.14494
4 Heymann-Maier L , Trueb L , Schmidt S , Carron PN , Hugli O , Heymann E , et al. Emergency department management of body packers and body stuffers. Swiss Med Wkly. 2017;147:w14499.
5Schweizerische Akademie der Medizinischen Wissenschaften (SAMW). Medizinisch-ethische Richtlinien zur Ausübung der ärztlichen Tätigkeit bei inhaftierten Personen. Incl. Anhang H: Medizinische Betreuung von Personen mit mutmasslichem Bodypacking. 2002, aktualisiert 2012, Anhang Lit. H ergänzt 2018. Available at: https://www.samw.ch/dam/jcr:1ad584ee-ad5f-4aa1-9f8b-96335d329a3e/richtlinien_samw_inhaftierte.pdf
6Art. 252, Schweizerische Strafprozessordnung (StPO) vom 5. Oktober 2007, SR 312.0.
7Art. 102, Zollgesetz vom 18. März 2005, SR 631.0.
8Stellungnahme der Eidgenoessischen Zollverwaltung (EZV) vom 09. Juli 2018 auf den Bericht der Nationalen Kommission zur Verhuetung von Folter (NKVF). Available at: https://www.nkvf.admin.ch/dam/data/nkvf/Berichte/2017/rancate/stellungnahme-rancate.pdf.
9 Booker RJ , Smith JE , Rodger MP . Packers, pushers and stuffers--managing patients with concealed drugs in UK emergency departments: a clinical and medicolegal review. Emerg Med J. 2009;26(5):316–20. doi:.https://doi.org/10.1136/emj.2008.057695
10 Poletti PA , Canel L , Becker CD , Wolff H , Elger B , Lock E , et al. Screening of illegal intracorporeal containers (“body packing”): is abdominal radiography sufficiently accurate? A comparative study with low-dose CT. Radiology. 2012;265(3):772–9. doi:.https://doi.org/10.1148/radiol.12112767
11 Shahnazi M , Hassanian-Moghaddam H , Gachkar L , Ahmadi N , Zamani N , Bahrami-Motlagh H , et al. Comparison of abdominal computed tomography with and without oral contrast in diagnosis of body packers and body stuffers. Clin Toxicol (Phila). 2015;53(7):596–603. doi:.https://doi.org/10.3109/15563650.2015.1054501
12Eidgenoessischen Zollverwaltung (EZV). Medienmitteilung; Zoll 2012: gegen organisierten Schmuggel grenzüberschreitende Kriminalität und illegale Migration. 2013. Available at: https://www.admin.ch/gov/de/start/dokumentation/medienmitteilungen.msg-id-47656.html
13Antwort der Eidgenoessischen Zollverwaltung (EZV) auf eigene Anfrage, 04 Dezember 2018.
14 Reginelli A , Russo A , Urraro F , Maresca D , Martiniello C , D’Andrea A , et al. Imaging of body packing: errors and medico-legal issues. Abdom Imaging. 2015;40(7):2127–42. doi:.https://doi.org/10.1007/s00261-015-0469-x
15 Moreira M , Buchanan J , Heard K . Validation of a 6-hour observation period for cocaine body stuffers. Am J Emerg Med. 2011;29(3):299–303. doi:.https://doi.org/10.1016/j.ajem.2009.11.022
16 de Prost N , Lefebvre A , Questel F , Roche N , Pourriat JL , Huchon G , et al. Prognosis of cocaine body-packers. Intensive Care Med. 2005;31(7):955–8. doi:.https://doi.org/10.1007/s00134-005-2660-y
17 Glovinski PV , Lauritsen ML , Bay-Nielsen M , Brandstrup B , Bisgaard T . Asymptomatic body packers should be treated conservatively. Dan Med J. 2013;60(11):A4723.
18 Pinto A , Reginelli A , Pinto F , Sica G , Scaglione M , Berger FH , et al. Radiological and practical aspects of body packing. Br J Radiol. 2014;87(1036):20130500. doi:.https://doi.org/10.1259/bjr.20130500
19 Berger FH , Nieboer KH , Goh GS , Pinto A , Scaglione M . Body packing: a review of general background, clinical and imaging aspects. Radiol Med (Torino). 2015;120(1):118–32. doi:.https://doi.org/10.1007/s11547-014-0458-0
20 Bulakci M , Kalelioglu T , Bulakci BB , Kiris A . Comparison of diagnostic value of multidetector computed tomography and X-ray in the detection of body packing. Eur J Radiol. 2013;82(8):1248–54. doi:.https://doi.org/10.1016/j.ejrad.2012.12.022
21 Flach PM , Ross SG , Ampanozi G , Ebert L , Germerott T , Hatch GM , et al. “Drug mules” as a radiological challenge: sensitivity and specificity in identifying internal cocaine in body packers, body pushers and body stuffers by computed tomography, plain radiography and Lodox. Eur J Radiol. 2012;81(10):2518–26. doi:.https://doi.org/10.1016/j.ejrad.2011.11.025
CW – data acquisition and analysis, statistical analysis and drafting of manuscript; CHN – critical revision of the manuscript; AS – data acquisition and analysis about use of resources; JM – responsible for statements on legislation; SF – responsible for standard operating procedure in prison and outcomes in prison; RB – principal investigator and study supervisor, study design, critical revision of the manuscript
The University Hospital Basel funded this study.
RB is publisher of emergencystandards.com (medstandards.com), a symptom-based medical decision-support tool licensed to 150 European hospitals, owned by the University Hospital Basel. The authors declare no further conflict of interest.