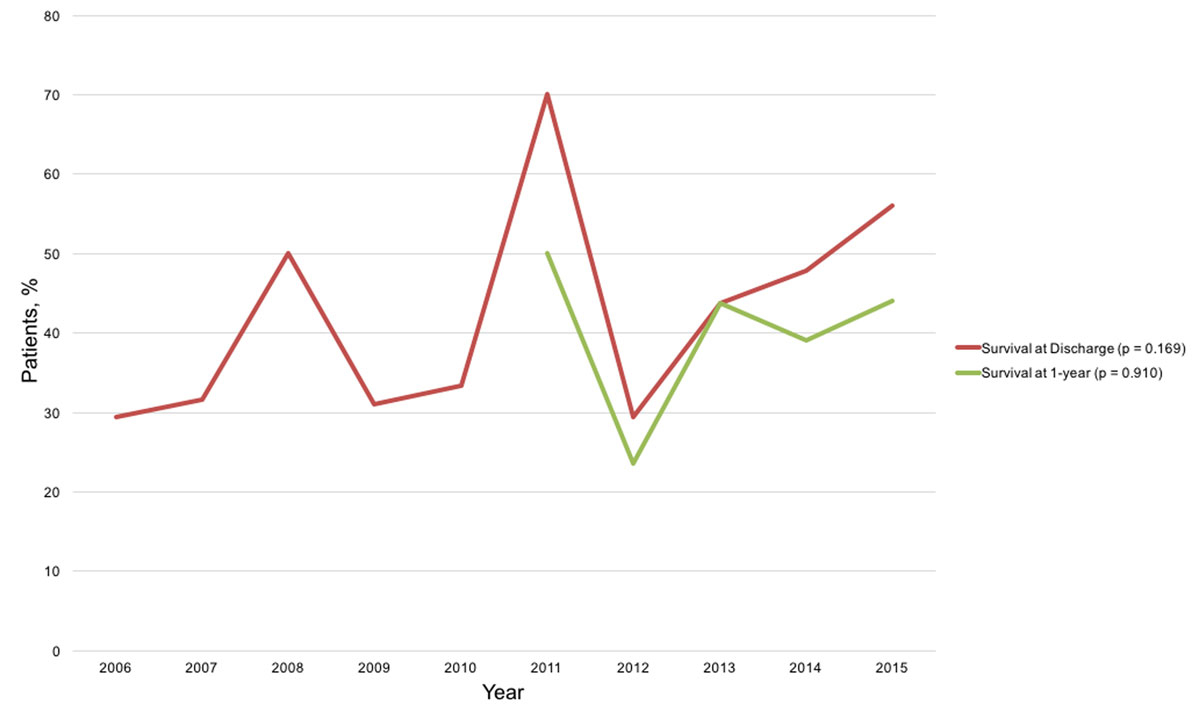
Figure 1 Survival over time.
DOI: https://doi.org/10.4414/smw.2019.20101
The emergency medical services (EMS) of northern St Gallen cover a population of about 200,000 (year: 2015) in eastern Switzerland and carry out around 15,000 responses annually. Paramedics are primarily in charge, but in life-threatening cases an emergency physician is also dispatched (around 2600 missions per year). Emergency physicians at our hospital are residents, the majority in anaesthesiology, with two or more years of clinical experience, who have completed an emergency physician course with the Swiss Society of Emergency and Rescue Medicine (SGNOR) and Advanced Cardiac Life Support (ACLS) training.
Based on population data and our cardiac arrest database, there was a mean incidence of 70 out-of-hospital cardiac arrests (OHCA) per 100,000 people annually in the EMS-covered population in northern St Gallen (2006–2015). The outcome of OHCAs is expected to have improved over the last few decades due to continuously improving cardiopulmonary resuscitation (CPR) training in laypersons, dispatcher-guided resuscitation and automated external defibrillator (AED) availability [1–3]. Furthermore, resuscitation guidelines for professionals have been adapted multiple times over the past few years. The American Heart Association (AHA) and the European Resuscitation Council (ERC) launch resuscitation guidelines, based on the International Liaison Committee on Resuscitation (ILCOR) [4, 5], every five years. The most recent updates were published in 2010 and 2015 [6–9]. The optimisation of the guidelines should allow better outcomes among treated patients. Our EMS staff’s training is based on the AHA guidelines. Accordingly, we hypothesised that the outcomes of the patients treated in our region would improve over time. In particular, the outcomes were expected to be better after the implementation of the 2010 update.
Many studies have analysed outcomes at hospital discharge, but less is known about the long-term survival and neurological outcomes of patients who suffer an OHCA. The primary goals of this study were: (1) to define the short- (hospital discharge) and long-term (1 year post-arrest) ventricular fibrillation (VF) and pulseless ventricular tachycardia (pVT) survival rates and neurological outcomes in the region of northern St Gallen, Switzerland; (2) to estimate the annual changes and the differences between the periods 2006–2010 and 2011–2015; and (3) to compare the results with the international literature based on a systematic review of OHCA studies.
Ethical approval for this study (No. EKSG 15/187) was provided by the Ethics Committee St Gallen, Switzerland. It complies with the principles stated in the Declaration of Helsinki.
For these analyses, prospectively collected data from all patients who suffered an OHCA between January 2006 and December 2015 were retrieved from an electronic database. The data contained information about demographics (age, gender), location (collapse spot), time course (date, time of collapse, alarm at EMS central, arrival of EMS team, start of CPR, first defibrillation, departure of EMS team, ROSC time, abort of resuscitation, arrival at hospital), aetiology and details of cardiac arrest (cardiac, presumed cardiac, non-cardiac with initial rhythm), management (pre-hospital measures such as ventilation, intubation, defibrillation and medication use), survival (until emergency room arrival, intensive care unit and hospital discharge), other factors (bystander witnessed, bystander resuscitation, bystander AED use), and neurological outcomes (CPC score and Glasgow Coma Score) until hospital discharge.
Out-of-hospital cardiac arrest was defined as the stop in effective blood flow due to the heart failing to contract efficiently [10]. In the pre-hospital clinical practice, the emergency physician used clinical signs such as pulselessness, apnoea or agonal breathing. As soon as an electrocardiography was monitored, the four cardiac dysrhythmias of VF, pVT, asystole or pulseless electrical activity were used as confirmation of cardiac arrest.
If return of spontaneous circulation (ROSC) was achieved, the patient was transferred to the Kantonsspital St. Gallen, the largest tertiary care hospital in eastern Switzerland, where percutaneous coronary intervention is immediately available.
Patients were screened and selected according to the Utstein form [11] to allow for a uniform comparison with other studies. The selection criteria were as follows:
At the end of this selection process, only the remaining patients, those with VF and pVT, were analysed for primary and secondary outcomes.
The primary endpoints were survival and a favourable neurological outcome (CPC 1–2) at hospital discharge from 2006 to 2015. CPC 1 is defined as “good cerebral performance”, CPC 2 as “moderate cerebral disability”, CPC 3 as “severe cerebral disability”, CPC 4 as “coma or vegetative state”, and CPC 5 as “brain death”.
The secondary outcomes were survival and a CPC score of 1–2 1 year after OHCA from 2011 to 2015. The secondary outcome data were not registered in the database, but were obtained through individual chart reviews and by a written questionnaire mailed to the patients. We defined the long-term outcome as the outcome at 1 year post-OHCA. The chart and questionnaire reviews were performed by two reviewers (TvH and PI) independently, and any CPC scores that did not match were resolved by consensus with a third reviewer (MF). Patients who did not return the questionnaire were contacted and interviewed by phone. Informed consent was obtained from all surviving patients approached by mail or telephone.
To compare our results with international data, we conducted a systematic literature search. For the full search strategy, review protocol and Prisma flow chart, see appendices 1–3 . Two authors (TvH and CK) individually searched for eligible observational studies using a systematic PubMed search restricted to studies published in English or German and with a search timeframe of January 2000 to April 2018. First, titles and abstracts were screened, then full text reviews were conducted where applicable. The search was restricted to studies reporting on 1000 or more OHCAs treated in or after the year 2000. We followed the PRISMA checklist [12]. The search terms were defined as follows: out-of-hospital cardiac arrest/epidemiology, mortality, therapy, complications, rehabilitation, and cardiopulmonary resuscitation/adverse effects, epidemiology, mortality, therapy and trends.
The following filters were active for the search: clinical study, comparative study, meta-analysis, multicentre study, observational study, research support, non-U.S. Gov't, review and systematic review. These filters were used to deliver the studies most relevant for our comparison. This search gave a total of 1278 results (last search: April 2018). Following our study’s inclusion criteria, we focused our literature search on studies that reported the survival and/or neurological outcome (with CPC score) at both hospital discharge and 1 year of out-of-hospital OHCA patients with a cardiac aetiology that had a shockable heart rhythm, and were bystander witnessed if possible. Studies reporting on OHCAs of non-cardiac origin, in paediatric patients or which occurred in-hospital, were excluded. Overall, 1052 studies could be excluded by considering only the title and/or abstract. In 226 studies, a full text review was performed. Additionally, we manually screened the references of relevant findings in the same way to search for more potentially eligible studies. Thereafter, the independent search results of the two authors were compared, and any disagreements were resolved by consensus. Finally, seven studies were included in the analysis (see appendix 2 for a flow chart) [13–19]. Data were extracted independently by both authors (TvH and CK). We extracted information on the last name of the study’s first author, year of publication, title of the study, study design, country/region, setting, population studied, timescale, and type of outcomes reported (survival, neurological outcomes or both). For certain studies (e.g. our data and Lindner et al.), we present more than one dataset as part of the results (see forest plots figs. 3–6 ) because multiple time periods were analysed independently to get more comparable data. Outcome and selection biases were assessed, see appendix 4. We did not perform any meta- or subgroup analyses.
Continuous variables were shown as means ± standard deviation (SD) or rounded percentages ± 95% confidence interval. Differences in outcomes between the two time periods were assessed by chi-square statistics. Potential annual changes were analysed by logistic regression. A p-value of <0.05 was considered significant. Analyses were performed by SPSS Version 24.0 (IBM, Armonk, USA) for windows (Microsoft, Redmond, USA). The results of the systematic literature review were visualised in figures 3–6 , which were created in Excel (Microsoft, Redmond, USA). The figures show the point estimates (including 95% CIs) of the survival rates and the reported CPC scores, as well as the weight of the corresponding study, at the described timepoint (discharge or 1 year). We did not perform a meta-analysis.
From 1 January 2006 until 31 December 2015, a total of 1423 confirmed OHCAs were recorded and included in the database. Resuscitation was attempted by EMS in 781 patients, 612 of which were of cardiac or presumed cardiac origin. Baseline and analyses characteristics are presented in tables 1–4 . A total of 182 patients (30%) presented a shockable primary rhythm such as VF or pVT at EMS arrival. These were included in the final analysis of survival rates and CPC scores. Seventy-five out of 182 (41%) survived until hospital discharge and 66/75 (88%) had a favourable neurological outcome of a CPC score of 1–2 at discharge. Seven out of 75 patients (11%) had a CPC score of 3–4.
Table 1 Baseline characteristics and collapse spot details.
| Characteristics | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | p-value | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resident population canton of St. Gallen, n* | 461,810 | 465,937 | 471,152 | 474,676 | 478,907 | 483,156 | 487,060 | 491,699 | 495,824 | 499,065 | <0.0001 | |
| Estimated coverage by EMS, n* | 192,038 | 193,954 | 196,004 | 197,511 | 198,875 | 200,280 | 201,635 | 203,050 | 204,182 | 205,324 | <0.0001 | |
| OHCA incidence, n/100,000 | 67.2 | 71.7 | 70.4 | 62.3 | 63.4 | 76.9 | 79.4 | 70.9 | 67.1 | 84.3 | 0.147 | |
| Age, mean (y) ± SD | 63 ± 16 | 67 ± 13 | 76 ± 9 | 63 ± 17 | 74 ± 10 | 70 ± 11 | 65 ± 13 | 66 ± 12 | 66 ± 11 | 64 ± 13 | 0.424 | |
| Male sex, n (%) | 9 (52.9) | 16 (84.2) | 12 (85.7) | 23 (79.3) | 8 (66.7) | 10 (100) | 14 (82.4) | 13 (81.3) | 18 (78.3) | 17 (68) | 0.648 | 140 (76.9)† |
| Collapse spot total, n (%) | 17 (100) | 19 (100) | 14 (100) | 28 (97) | 12 (100) | 10 (100) | 17 (100) | 16 (100) | 23 (100) | 25 (100) | 181 (99.5) | |
| Collapse spot home, n (%) | 7 (41.2) | 11 (57.9) | 4 (28.6) | 17 (60.7) | 7 (58.3) | 3 (30) | 9 (52.9) | 3 (18.8) | 11 (47.8) | 12 (48) | 0.698 | 84 (46.4) |
| Collapse spot public place, n (%) | 6 (35.3) | 6 (31.6) | 8 (57.1) | 7 (25) | 4 (33.3) | 7 (70) | 7 (41.2) | 11 (68.8) | 8 (34.8) | 9 (36) | 0.598 | 73 (40.3) |
| Collapse spot other, n (%) | 4 (2 3.5) |
2 (10.5) | 2 (14.3) | 4 (14.3) | 1 (8.3) | 0 (0) | 1 (5.9) | 2 (12.5) | 4 (17.4) | 4 (16) | 0.632 | 24 (13.3) |
EMS =emergency medical services; OHCA = out-of-hospital cardiac arrest; SD = standard deviation p-values were calculated by logistic regression. * Öffentliche Statistik Kanton St.Gallen [Internet], Online-Statistikdatenbanken STADA-SG, [cited 2018 Feb 21], available on: https://www.statistik.sg.ch/ and http://stada2.sg.ch/† Missing data 7 (3.8%)
Table 2 The Utstein form of our analysed population.
| Characteristics | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | p-value | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OHCA, n | 129 | 139 | 138 | 123 | 126 | 154 | 160 | 144 | 137 | 173 | 0.048 | 1,423 |
| OHCA, resuscitation attempted, n (%) | 69 (53.5) | 78 (56.1) | 78 (56.5) | 79 (64.2) | 61 (48.4) | 67 (43.5) | 88 (55.0) | 87 (60.4) | 79 (57.7) | 95 (54.9) | 0.088 | 781 (54.9) |
| OHCA resuscitation attempted, cardiac aetiology, n (%) | 49 (38.0) | 63 (45.3) | 64 (46.4) | 61 (49.6) | 54 (42.9) | 46 (29.9) | 73 (45.6) | 64 (44.4) | 62 (45.3) | 76 (43.9) | 0.868 | 612 (78.4) |
| Witnessed by bystanders, n (%) | 40 (81.6) | 41 (65.1) | 42 (65.6) | 46 (75.4) | 39 (72.2) | 30 (65.2) | 49 (67.1) | 43 (67.2) | 44 (71.0) | 57 (75.0) | 0.171 | 431 (70.4) |
| Shockable heart rhythm, n (%) | 17 (34.7) | 19 (30.2) | 14 (21.9) | 29 (47.5) | 12 (22.2) | 10 (21.7) | 17 (23.3) | 16 (25.0) | 23 (37.1) | 25 (32.9) | 0.880 | 182 (29.7)* |
| Bystander CPR performed, n (%) | 7 (41.2) | 8 (42.1) | 7 (50) | 14 (48.3) | 2 (16.7) | 5 (50) | 13 (76.5) | 11 (68.8) | 16 (69.6) | 15 (60) | 0.065 | 98 (53.8) |
| Bystander AED use, n (%) | 0 (0) | 1 (5.3) | 1 (7.1) | 2 (6.9) | 0 (0) | 2 (20) | 3 (17.6) | 3 (18.8) | 3 (13) | 3 (12) | 0.03 | 18 (9.9) |
AED = automated external defibrillator; CPR = cardiopulmonary resuscitation; OHCA = out-of-hospital cardiac arrest p-values were calculated by logistic regression. * Missing data = 3 (1.6%)
Table 3 Outcome data from our cardiac arrest database.
| Characteristics | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | p-value | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ROSC, n (%) | 9 (52.9) | 10 (52.6) | 9 (64.3) | 16 (55.2) | 8 (66.7) | 9 (90.0) | 10 (58.8) | 12 (75.0) | 15 (65.2) | 20 (80.0) | 0.054 | 118 (15.1) |
| Survival to discharge, n (%) | 5 (29.4) | 6 (31.6) | 7 (50.0) | 9 (31.0) | 4 (33.3) | 7 (70.0) | 5 (29.4) | 7 (43.8) | 11 (47.8) | 14 (56.0) | 0.169 | 75 (41.2) |
| Survival to discharge per time period, n (%) | 31 (34%) | 44 (48%) | 0.071 | 75 (41.2) | ||||||||
| CPC 1–2 at discharge, n (%) | 4 (80.0) | 6 (100.0) | 4 (57.1) | 8 (88.9) | 4 (100.0) | 5 (71.4) | 5 (100.0) | 7 (100.0) | 10 (90.9) | 13 (92.9) | 0.332 | 66 (36.3) |
| CPC 3–4 at discharge, n (%) | 1 (20.0) | 0 (0.0) | 2 (28.6) | 1 (11.1) | 0 (0.0) | 2 (28.6) | 0 (0.0) | 0 (0.0) | 1 (9.1) | 0 (0.0) | 0.247 | 7 (3.8)* |
| Survival at 1 year, n (%) | NA | NA | NA | NA | NA | 5 (50.0) | 4 (23.5) | 7 (43.8) | 9 (39.1) | 11 (44.0) | 0.910 | 36 (19.8)† |
| CPC 1–2 at 1 year, n (%) | NA | NA | NA | NA | NA | 5 (71.4) | 4 (80.0) | 7 (100.0) | 9 (81.8) | 11 (78.6) | 0.969 | 36 (19.8) |
| CPC 3–4 at 1 year, n (%) | NA | NA | NA | NA | NA | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
CPC = cerebral performance category; ROSC = return of spontaneous circulation p-values of trends over years were calculated by logistic regression, p-value of the two time periods by chi-square test. * Missing data = 2 (1.1%) † Missing data = 3 (1.6%)
Table 4 Management details after EMS arrival at the scene.
| Characteristics | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | p-value | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Shockable heart rhythm, n (%) | 17 (34.7) | 19 (30.2) | 14 (21.9) | 29 (47.5) | 12 (22.2) | 10 (21.7) | 17 (23.3) | 16 (25.0) | 23 (37.1) | 25 (32.9) | 0.880 | 182 (29.7)* |
| Defibrillation, n (%) | 16 (94.1) | 17 (89.5) | 14 (100.0) | 26 (89.7) | 12 (100.0) | 10 (100.0) | 15 (88.2) | 14 (87.5) | 19 (82.6) | 24 (96.0) | 0.412 | 167 (91.8) |
| Mean shocks admitted, n ± SD | 3.3 ± 2 | 4.3 ± 2 | 3.2 ± 2 | 4.3 ± 3 | 4.4 ± 4 | 2.6 ± 2 | 3.9 ± 3 | 4.6 ± 2 | 3.8 ± 2 | 4.2 ± 4 | ||
| Intubation, n (%) | 10 (58.8) | 12 (63.2) | 5 (35.7) | 16 (55.2) | 3 (25.0) | 1 (10.0) | 9 (52.9) | 8 (50.0) | 10 (43.5) | 12 (48.0) | 0.566 | 86 (47.3) |
| Adrenaline use, n (%) | 12 (70.6) | 17 (89.5) | 11 (78.6) | 23 (79.3) | 8 (66.7) | 6 (60.0) | 15 (88.2) | 13 (81.3) | 15 (65.2) | 14 (56.0) | 0.221 | 134 (73.6) |
| Mean adrenaline dose, mg, ± SD | 4.2 ± 2.8 | 4.5 ± 4.4 | 4.6 ± 2.8 | 4.6 ± 3.2 | 5.1 ± 3.4 | 3.8 ± 1.3 | 4.9 ± 2.9 | 3.6 ± 1.9 | 2.9 ± 1.1 | 3.5 ± 2.1 | ||
| Amiodarone use, n (%) | 6 (35.3) | 12 (63.2) | 8 (57.1) | 16 (55.2) | 6 (50.0) | 2 (20.0) | 8 (47.1) | 9 (56.3) | 13 (56.5) | 9 (36.0) | 0.708 | 89 (48.9) |
| Mean amiodarone dose admitted, mg, ± SD | 300.0 ± 0.0 | 290.0 ± 88.6 | 300.0 ± 75.0 | 328.1 ± 58.5 | 425.0 ± 103.1 | 300.0 ± 0.0 | 356.3 ± 72.6 | 250.0 ± 100.0 | 334.6 ± 86.3 | 316.7 ± 85.0 | 0.853 | |
| Atropine use, n (%) | 6 (35.3) | 11 (57.9) | 5 (35.7) | 18 (62.1) | 4 (33.3) | 2 (20.0) | 2 (11.8) | 1 (6.3) | 1 (4.3) | 1 (4.0) | 0.003 | 51 (28.0) |
| Mean atropine dose, mg, ± SD | 1.9 ± 1.1 | 1.5 ± 0.9 | 2.6 ± 0.8 | 2.6 ± 0.9 | 2.8 ± 0.4 | 1.8 ± 1.3 | 1.5 ± 0.5 | 0.5 ± 0.0 | 0.5 ± 0.0 | 0.5 ± 0.0 | 0.023 | |
| Mean time to EMS arrival, min | 16 | 13 | 16 | 18 | 13 | 12 | 13 | 10 | 11 | 13 | 0.042 | |
| Mean time to ROSC, min | 20 | 10 | 14 | 8 | 15 | 17 | 24 | 20 | 16 | 16 | 0.347 |
EMS = emergency medical services; ROSC = return of spontaneous circulation; SD = standard deviation p-values were calculated by logistic regression. * Missing data = 3 (1.6%)
Of the analysed population, 91 were treated between 2006 and 2010 and 91 between 2011 and 2015. 31 (34%) survived until hospital discharge in the first time period, 44 (48%) in the second time period (p = 0.071 for a comparison between the two time periods). 26/31 (83%) and 40/44 (91%) respectively had CPC scores of 1–2. Between 2011 and 2015, the 1-year survival rate was 36/44 (82%), and these 36 patients all had a favourable neurological outcome (CPC 1–2).
Neither the hospital survival rate (time period 2006–2015) nor the 1-year survival rate (time period 2011–2015) or CPC score improved significantly (figs 1 and 2 ). However, the mean time until EMS arrival decreased from 16 to 13 minutes (p = 0.042). The ROSC rate did not change in the observed period (p = 0.054), but AED use by bystanders increased (p = 0.03). The use of intubation, adrenaline (epinephrine) and amiodarone (Cordarone) remained stable, and the use of atropine decreased (p = 0.003). An EMS defibrillator was used for shockable rhythms in 92% of cases, with a median of 3.1 (2.4–3.8) shocks. Most cardiac arrests happened at home (46%), while 40% occurred in a public place (street, workplace, public building, retirement home). See tables 1–4 for details.
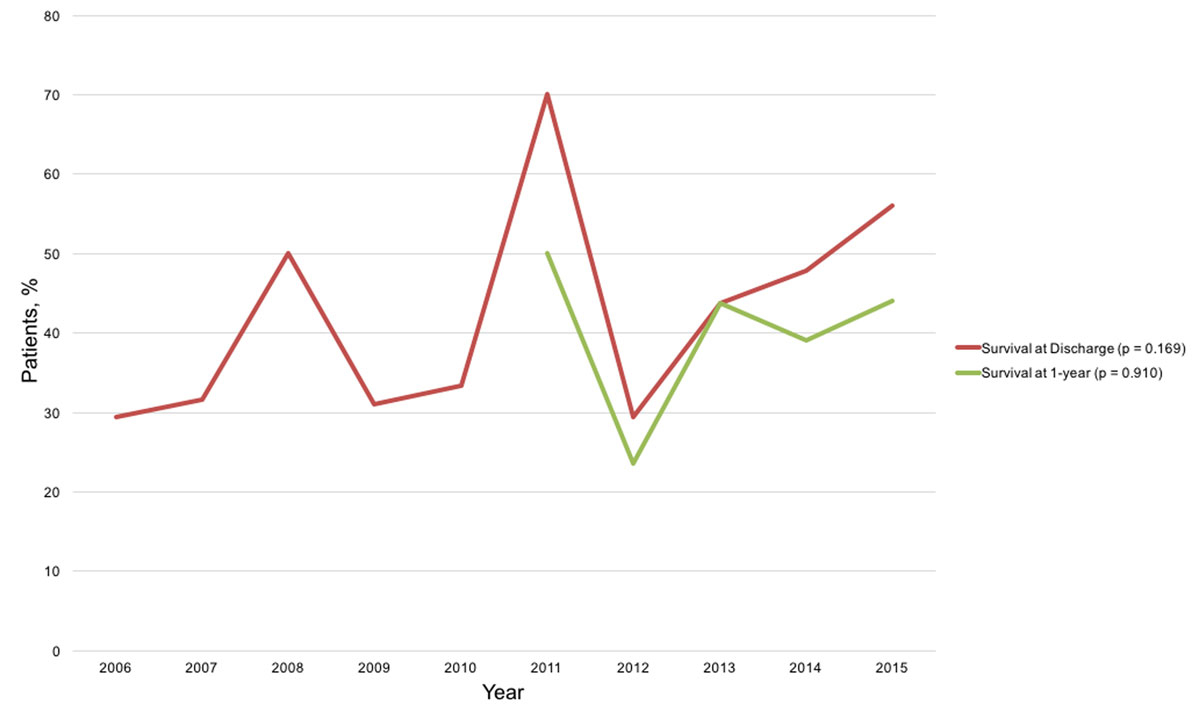
Figure 1 Survival over time.
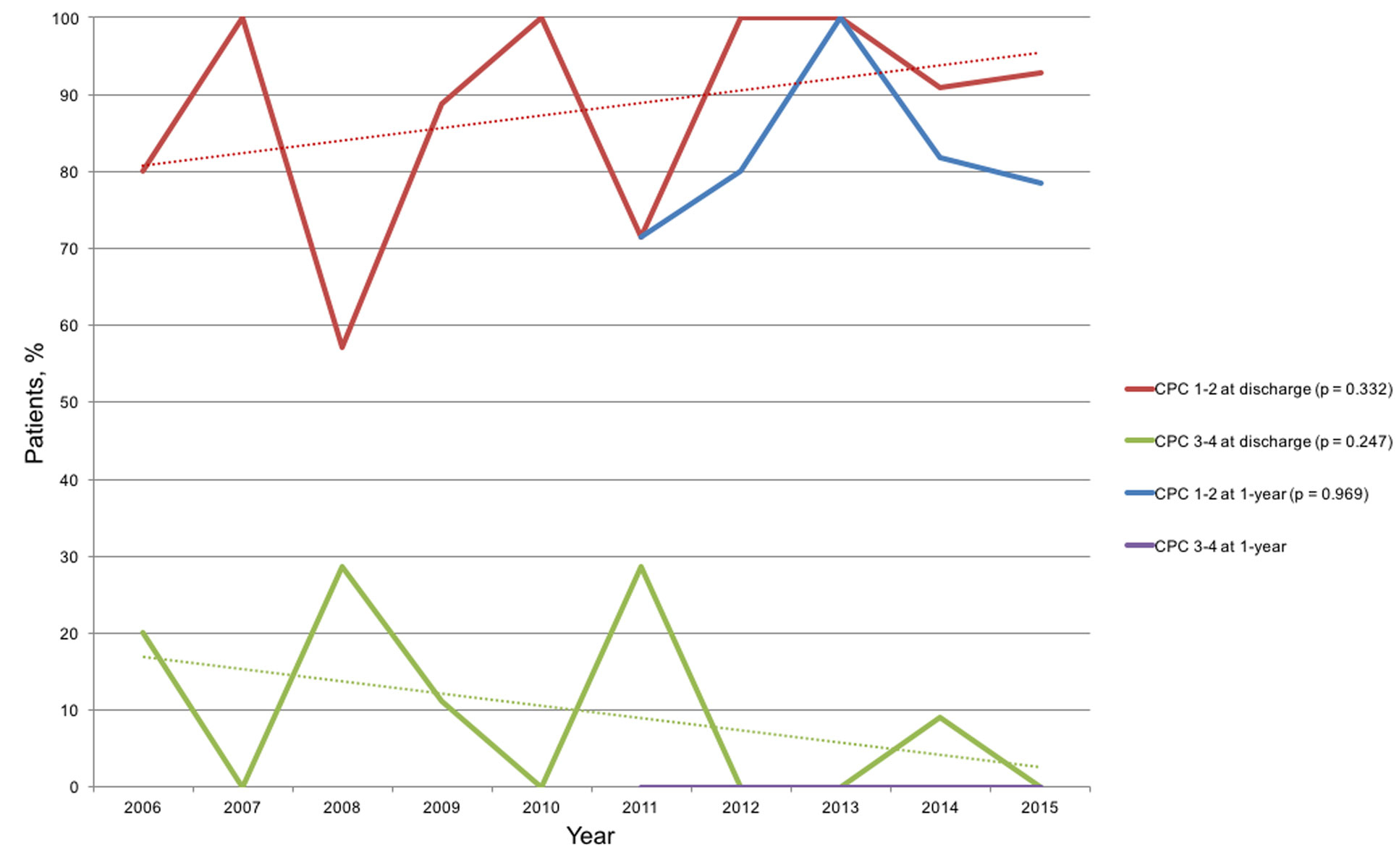
Figure 2 Cerebral Performance Category over time.
Seven studies were included in the analysis. The hospital and 1-year survival rates varied substantially, from 11 to 52% and from 6 to 47% respectively (figs 3 and 4 ). At discharge and after 1 year, 66–87% and 83–96% of patients respectively had a CPC score of 1–2 (figs 5 and 6 ).
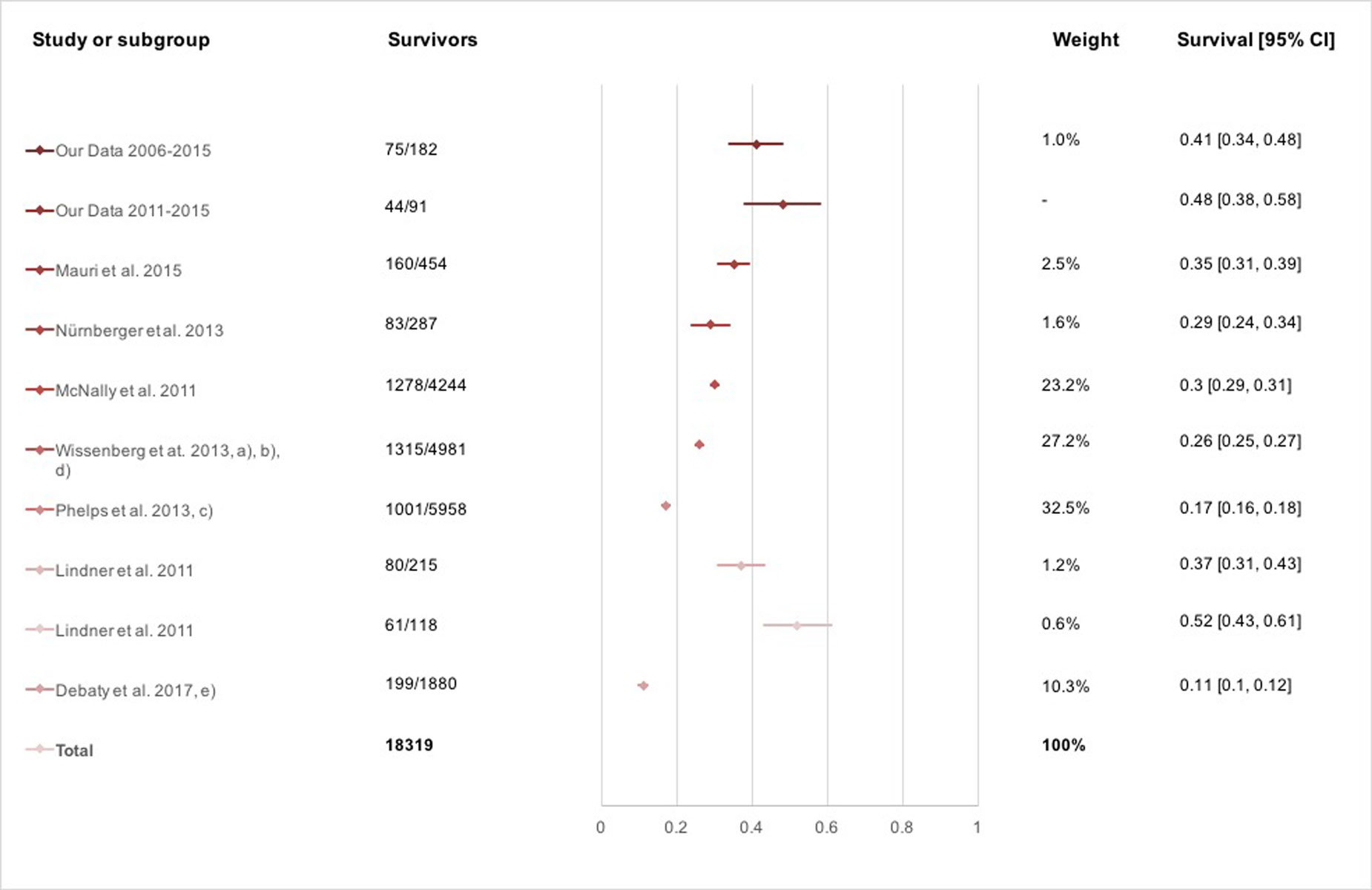
Figure 3 Survival at hospital discharge.
* Outcomes are reported according to Utstein (cardiac aetiology, witnessed [layperson or EMS] and shockable initial rhythm), if not mentioned otherwise: (a) at 30 days post-discharge; (b) excludes EMS-witnessed; (c) includes non-witnessed, non-shockable; d) includes non-witnessed; (e) includes non-cardiac, non-witnessed, non-shockable, excludes EMS-witnessed.
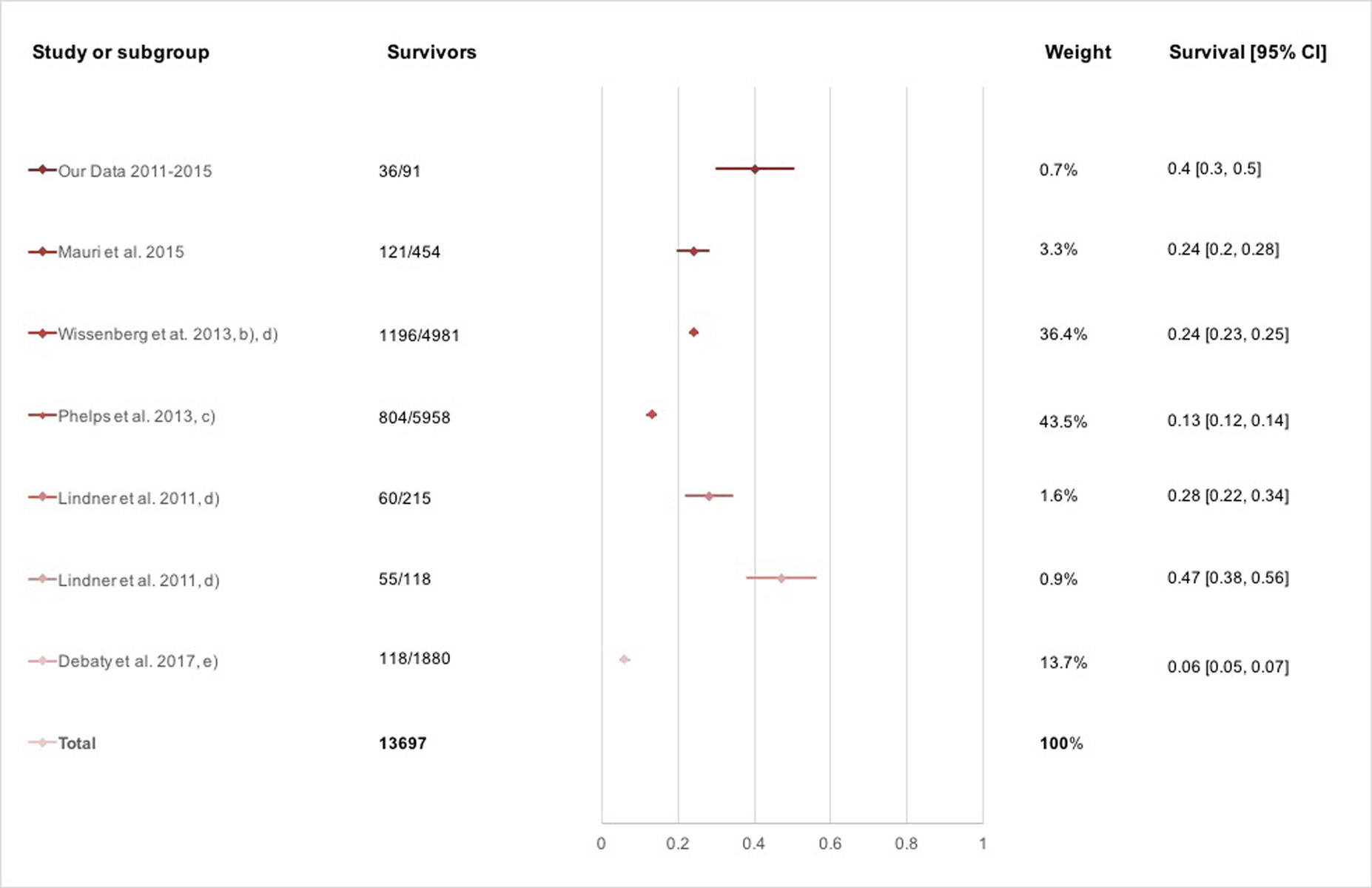
Figure 4 Survival at 1 year post-arrest.
* Outcomes are reported according to Utstein (cardiac aetiology, witnessed [layperson or EMS] and shockable initial rhythm), if not mentioned otherwise: (a) at 30 days post-discharge; (b) excludes EMS-witnessed; (c) includes non-witnessed, non-shockable; d) includes non-witnessed; (e) includes non-cardiac, non-witnessed, non-shockable, excludes EMS-witnessed.
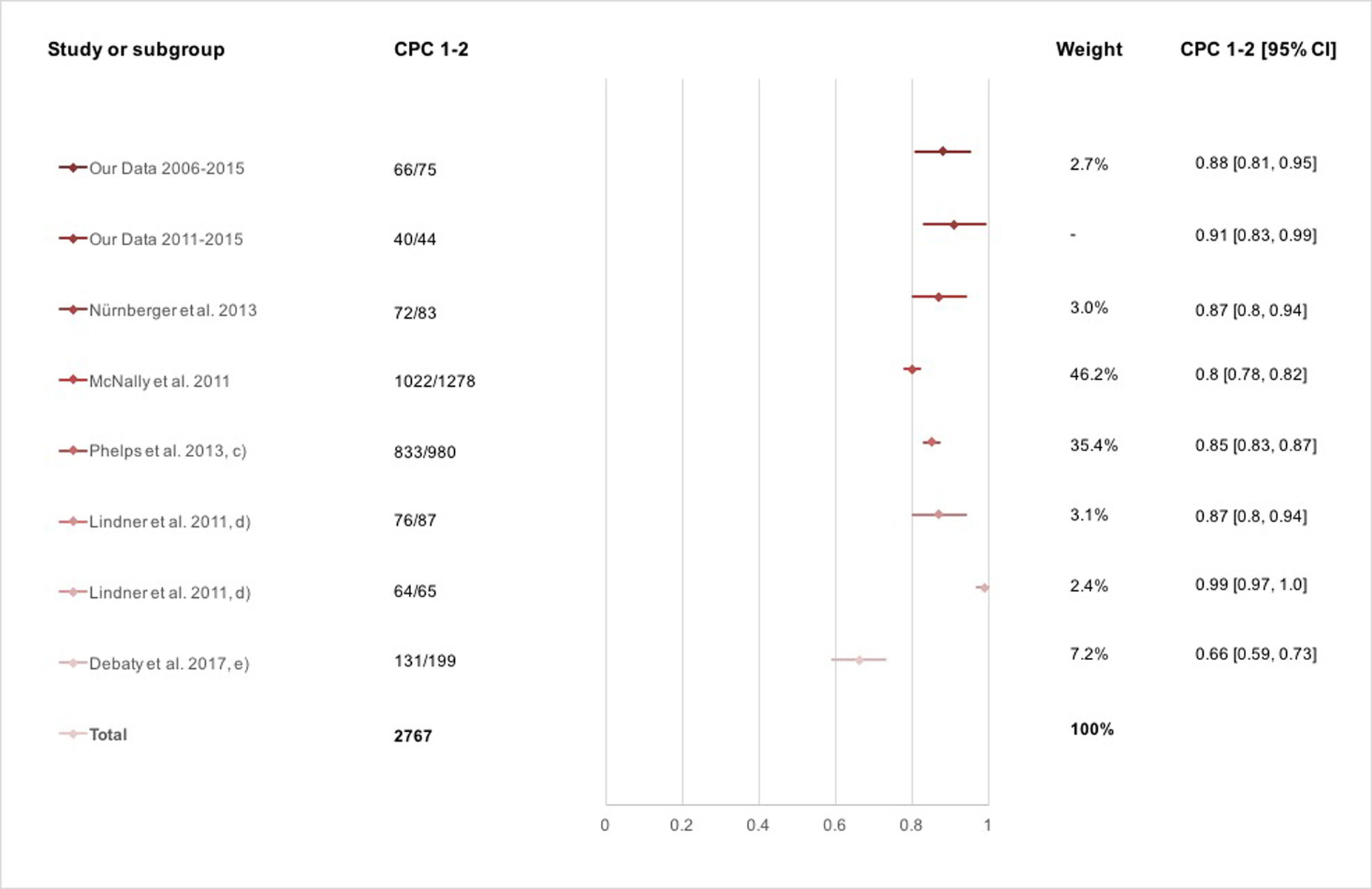
Figure 5 CPC score at hospital discharge.
* Outcomes are reported according to Utstein (cardiac aetiology, witnessed [layperson or EMS] and shockable initial rhythm), if not mentioned otherwise: (c) includes non-witnessed, non-shockable; (d) includes non-witnessed; (e) includes non-cardiac, non-witnessed, non-shockable, excludes EMS-witnessed.
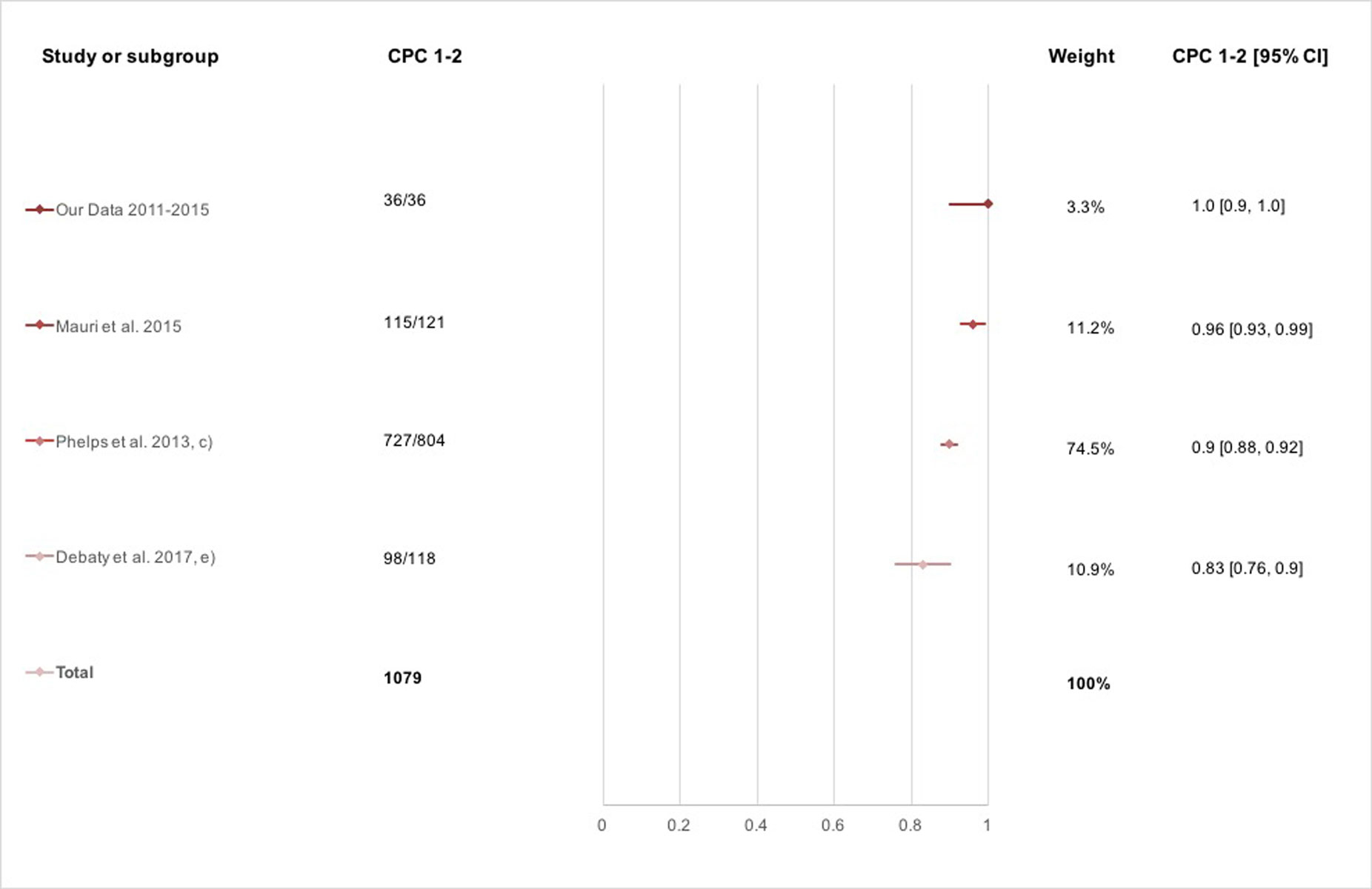
Figure 6 CPC score at 1 year post-arrest.
* Outcomes are reported according to Utstein (cardiac aetiology, witnessed [layperson or EMS] and shockable initial rhythm), if not mentioned otherwise: (c) includes non-witnessed, non-shockable; (e) includes non-cardiac, non-witnessed, non-shockable, excludes EMS-witnessed.
Lindner et al., Mauri et al. and Wissenberg et al. found a statistically significant improvement in the survival to discharge in the observed time periods: Lindner compared two periods (2001–2005 and 2006–2008) and found a significant improvement in the survival at discharge (37 to 52%, p for comparison = 0.0105) and at 1 year (28 to 47%, p = 0.0005). Mauri found an improved survival to discharge over the 10 years observed (15 to 55%, p for trend = 0.00), as did Wissenberg (3.5 to 10.8%, p for the trend <0.001 at discharge, and 2.9 to 10.2%, p <0.001 at 1 year) [13, 15, 19].
Similar results were found for neurological outcomes (see figs. 3–6 ).
In our study of 182 patients with a shockable primary rhythm, 75/182 survived until hospital discharge, most of them (88%) with a good neurological outcome. The introduction of the 2010 AHA guidelines had no beneficial effect on survival.
Our systematic literature review included seven studies and revealed broad variability in hospital and 1-year survival rates (11 to 52% and 6 to 47%, respectively). The outcomes of the patients treated in our region lie within this range reported in the literature. However, some studies used broader inclusion criteria, not strictly following the Utstein-based definitions we used (see table 5 for details). Another meta-analysis of OHCA outcomes in 67 studies on four different continents (Europe, North America, Asia and Australia) also showed high variability in the reported outcomes (VF survival to discharge rates of 3 to 43%) [20]. Reasons for this are differences in methodology, population characteristics, geographical factors and – potentially – quality of care [20]. Data from Europe and the United States show more similar results to our own: in a large study from Vienna, Austria, 110/446 (25%) patients with a shockable rhythm survived until hospital discharge, while 91/110 (83%) had a CPC score of 1–2 [17]. The authors identified early bystander resuscitation, onsite AED use and first responder dispatching as contributing factors for favourable outcomes. Data from the Centre of Disease Control in the United States show a survival to discharge rate of 1278 out of 4244 (30%) patients with initial shockable rhythms over five years (2005–2010), with 1022/1278 (80%) having a CPC score of 1–2 [14]. The results of this study are very much comparable with our data, which shows a similar in-hospital survival rate (30 vs 34%) and a similar proportion of patients with CPC scores of 1–2 (80 vs 83%).
Table 5 Studies included in the systematic literature review.
| First author and year of publication [ref. no.] | Location | Study period | Participants | Main outcomes | Study design | Setting | Comments |
|---|---|---|---|---|---|---|---|
| Mauri et al. 2015 [13] | Ticino, Switzerland | 01/2005–12/2014 | 3367 OHCA, of which 454 fulfil all Utstein comparator* criteria |
Survival to hospital admission, survival to discharge and 1 year; CPC at discharge and 1 year | Cohort study | Web-based registry of all OHCA in the Swiss Canton of Ticino, multicentre | |
| Nürnberger et al. 2013 [17] | Vienna, Austria | 01/2009–12/2010 | 7030 OHCA, of which 283 fulfil all Utstein comparator criteria | Any ROSC, event survival, survival and CPC at discharge | Cohort study | Vienna Ambulance Service, multicentre | |
| McNally et al. 2011 [14] | United States | 10/2005–12/2010 | 40,274 OHCA, of which 4244 fulfil all Utstein comparator criteria | Survival to hospital admission, survival to discharge, CPC at discharge | Cohort study | Nationwide Cardiac Arrest Registry, multicentre | Excluded EMS-witnessed arrests (analysed in a separate cohort) |
| Wissenberg et al. 2013 [15] | Denmark | 06/2001–12/2010 | 32,577 OHCA, 19,468 were analysed, of which 4981 shockable rhythms | Survival to 30 days, survival to 1 year | Cohort study | Nationwide Danish Cardiac Arrest Registry, multicentre | Included non-witnessed and excluded EMS-witnessed arrests; No analysis of CPC but analysis of “anoxic brain damage” between discharge and 30 days |
| Phelps et al. 2013 [18] | King County, Washington, United States | 01/2001–12/2009 | 6560 OHCA, 5958 EMS-treated, non-traumatic OHCA | Survival to discharge, CPC at discharge, survival at 1 year, survival at five years | Cohort study | EMS registry, multicentre | Included non-cardiac, non-witnessed and non-shockable patients |
| Lindner et al. 2011 [19] | Stavanger, Norway | 01/2001–12/2008 | 1628 OHCA, of which 215 and 118 (time periods 2001–2005 and 2006–2008 respectively) fulfil all Utstein comparator criteria | Any ROSC, survival to discharge, CPC at discharge, survival to 1 year | Cohort study | Single centre | We included both time periods in the study as separate analyses; 1-year survivors include non-witnessed arrests |
| Debaty et al. 2017 [16] | United States | 08/2007– 07/2009 |
1880 OHCA, stratified for “gasping” vs “no gasping” | Survival to discharge, CPC at discharge, survival to 1 year, CPC at 1 year | Observational study with data from randomised controlled trial | 46 EMS registries, multi-centre | Numbers include non-cardiac, non-witnessed and non-shockable patients; EMS-witnessed arrests were excluded |
CPC = cerebral performance category; EMS = emergency medical services; OHCA = out-of-hospital cardiac arrest; ROSC = return of spontaneous circulation * We defined Utstein comparator criteria as cardiac aetiology, witnessed by bystanders and with shockable rhythm (ventricular fibrillation, pulseless ventricular tachycardia).
Public health measures such as CPR training in laypersons (in driving schools and even elementary schools) and AED availability are important steps for improving outcomes [21, 22]. These efforts are associated with an improved hospital survival rate [23]. In Switzerland, first aid training in driving schools has been mandatory since 1977, and Samaritan societies have provided voluntary training in basic CPR since 1993. Still, basic CPR training is absent among the general population in many cantons, although there have been more initiatives towards building first responder networks [13]. In the canton of St Gallen, first responder networks (e.g. Samaritans, firefighters) are being built up, and these were called out 110 times in 2015 [24]. AED use increased in the observed time period, potentially caused by the greater availability of AED devices in the covered area.
In our study, 36/44 (82%) patients who survived to discharge were still alive after 1 year, all of them with a good neurological outcome. In the study by Mauri et al., a 1-year survival rate of 121/160 (76%), with a neurologically intact status in 115/121 (96%) was reported [13]. Data on long-term neurological outcomes after OHCA are surprisingly sparse. Reasons for this are the supposed difficulties of following up patients over a long period of time and a lack of national databases. Also, a national resuscitation outcome register for comparison was absent in Switzerland for a long time, but one is currently being built up, having been begun in 2016 (“Swiss ReCa”, Swiss Registry of Cardiac Arrest). Nevertheless, even if all EMS in Switzerland participate, the numbers obtained from this registry might be too small to draw reliable conclusions. Accordingly, a study covering many European countries or participation in European Resuscitation Registries (e.g. “EuReCa”, European Registry of Cardiac Arrest), is needed.
In our data, there was no significant change in outcomes over time. However, there were differences in clinical practice between the two time periods investigated, giving evidence of the successful implementation of the 2010 AHA resuscitation guidelines. Reasons for the lack of improvement are presumably multifactorial. Firstly, the number of patients in the final analyses is quite small, possibly precluding a statistically significant result. Secondly, the outcome at the beginning of the observed time period was quite favourable (see comparison with the literature), which does not leave much room for substantial improvement. An alternative explanation, however, is that the improvements implemented through the guideline updates are not fundamental enough to allow for a substantial improvement in outcomes. In contrast to our study, Mauri et al., demonstrated an increase in the hospital survival rate from 15% in 2005 to 55% in 2014 (p = 0.0) [13]. In the area covered in that study, in the south of Switzerland, a large effort was made to build up an effective first responder network through a mobile phone alarm system, shortening the hands-on time significantly and thereby improving the “chain of survival”. Furthermore, CPR training in laypersons and AED availability in that area have been vastly ameliorated over the past decade. In addition, patients were transferred to a tertiary care hospital after 2010. The effort was successful and resulted in an impressive improvement in outcomes. The survival rate at the end of the study period was comparable with ours. The training of laypersons is not as strict in our region as in that described in Mauri’s study.
Lindner et al. compared two periods (2001–2005 and 2006–2008) in a Norwegian study and showed a relevant rise in the 1-year survival rate for shockable rhythms of 29% to 43% (p = 0.005) [19]. Here again, the different parts of the “survival chain” all play a certain role. Although there was an increase in the EMS response time from 8 to 9 minutes and a decline in shockable rhythms, the layperson CPR rate was significantly higher. But most importantly, they successfully implemented therapeutic hypothermia, emergency percutaneous coronary intervention (PCI) and the 2005 ERC (European Resuscitation Council) CPR guidelines. These reasons are a possible (but not proven) explanation for the better outcomes in the second period.
A nationwide study conducted in Denmark from 2001–2010 showed an increase in 1-year survival: 1.3/100,000 in 2001 to 3.5/100,000 people in 2010. There are no data from the study on CPC scores, although it reported the presence of anoxic brain damage in 10% of the 1-year survivors [15]. In Denmark between 2001 and 2010, CPR training in elementary and driving schools was mandatory, and CPR training kits and first aid certificates were distributed. Furthermore, AED availability was increased, although these devices were only used occasionally (1.1% in 2001 and 2.2% in 2010, p = 0.003). In summary, efforts to give laypersons CPR training and the distribution of AEDs seem to have the potential to improve survival after out-of-hospital cardiac arrest. The optimisation of guidelines for health care professionals might be a less important effect. However, the outcome after CPR does not only depend on the initial management, but is very much modified by the in-hospital treatment and the availability of PCI and intensive care facilities.
The most important limitation is the small number of patients analysed, despite the long data acquisition period of 10 years. This fact is caused by the large number of hospitals and ambulance services all covering relatively small areas in Switzerland. The small sample size limits the statistical power and generalisability of the results and makes the results prone to biases. A second important limitation is the lack of details about post-resuscitation care (e.g. PCI, therapeutic hypothermia) and certain baseline information such as the Charlson Comorbidity Score and/or ASA status. In addition, no statement could be made about the impact of external resuscitation devices such as AutoPulse® or LUCAS, as these devices are not routinely used in our region. Furthermore, there might have been some recall bias by the attending physicians. The decision as to whether an OHCA is of cardiac cause or not is often a clinical one, and may therefore lead to inaccurate data. The assessment of the neurological status by CPC score might be an oversimplification, and important limitations in daily activities could remain undetected.
Survival rates and neurological outcomes to hospital discharge and 1 year are favourable in our hospital, although there was no improvement in either the primary (survival and CPC score at hospital discharge) or secondary (survival and CPC score after 1 year) outcomes. We found our survival rates to be on a stable, high level in comparison to international studies from Europe and the United States. To compare our findings, further studies are needed, covering larger areas of Switzerland or, preferably, Europe. Further public health measures should be undertaken, and a national register for the analysis of OHCA outcomes is of high importance.
The appendices are available as a separate file for downloading at: https://smw.ch/en/article/doi/smw.2019.20101/
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Chan PS , McNally B , Tang F , Kellermann A ; CARES Surveillance Group. Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation. 2014;130(21):1876–82. doi:.https://doi.org/10.1161/CIRCULATIONAHA.114.009711
2 Hollenberg J , Herlitz J , Lindqvist J , Riva G , Bohm K , Rosenqvist M , et al. Improved survival after out-of-hospital cardiac arrest is associated with an increase in proportion of emergency crew--witnessed cases and bystander cardiopulmonary resuscitation. Circulation. 2008;118(4):389–96. doi:.https://doi.org/10.1161/CIRCULATIONAHA.107.734137
3 Blom MT , Beesems SG , Homma PCM , Zijlstra JA , Hulleman M , van Hoeijen DA , et al. Improved survival after out-of-hospital cardiac arrest and use of automated external defibrillators. Circulation. 2014;130(21):1868–75. doi:.https://doi.org/10.1161/CIRCULATIONAHA.114.010905
4 Hazinski MF , Nolan JP , Billi JE , Böttiger BW , Bossaert L , de Caen AR , et al. Part 1: Executive summary: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2010;122(16, Suppl 2):S250–75. doi:.https://doi.org/10.1161/CIRCULATIONAHA.110.970897
5 Hazinski MF , Nolan JP , Aickin R , Bhanji F , Billi JE , Callaway CW , et al. Part 1: Executive Summary: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2015;132(16, Suppl 1):S2–39. doi:.https://doi.org/10.1161/CIR.0000000000000270
6 Link MS , Berkow LC , Kudenchuk PJ , Halperin HR , Hess EP , Moitra VK , et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18, Suppl 2):S444–64. doi:.https://doi.org/10.1161/CIR.0000000000000261
7 Neumar RW , Otto CW , Link MS , Kronick SL , Shuster M , Callaway CW , et al. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18, Suppl 3):S729–67. doi:.https://doi.org/10.1161/CIRCULATIONAHA.110.970988
8 Nolan JP , Soar J , Zideman DA , Biarent D , Bossaert LL , Deakin C , et al.; ERC Guidelines Writing Group. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation. 2010;81(10):1219–76. doi:.https://doi.org/10.1016/j.resuscitation.2010.08.021
9 Monsieurs KG , Nolan JP , Bossaert LL , Greif R , Maconochie IK , Nikolaou NI , et al.; ERC Guidelines 2015 Writing Group. European Resuscitation Council Guidelines for Resuscitation 2015: Section 1. Executive summary. Resuscitation. 2015;95:1–80. doi:.https://doi.org/10.1016/j.resuscitation.2015.07.038
10National Heart. Lung and Blood Institute [Internet]. Sudden Cardiac Arrest [cited 2018 Aug 25]. Available from: https://www.nhlbi.nih.gov/health/health-topics/topics/scda
11 Jacobs I , Nadkarni V , Bahr J , Berg RA , Billi JE , Bossaert L , et al.; International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa; ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation. Circulation. 2004;110(21):3385–97. doi:.https://doi.org/10.1161/01.CIR.0000147236.85306.15
12 Moher D , Liberati A , Tetzlaff J , Altman DG ; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi:.https://doi.org/10.1371/journal.pmed.1000097
13 Mauri R , Burkart R , Benvenuti C , Caputo ML , Moccetti T , Del Bufalo A , et al. Better management of out-of-hospital cardiac arrest increases survival rate and improves neurological outcome in the Swiss Canton Ticino. Europace. 2016;18(3):398–404. doi:.https://doi.org/10.1093/europace/euv218
14 McNally B , Robb R , Mehta M , Vellano K , Valderrama AL , Yoon PW , et al.; Centers for Disease Control and Prevention. Out-of-hospital cardiac arrest surveillance --- Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005--December 31, 2010. MMWR Surveill Summ. 2011;60(8):1–19.
15 Wissenberg M , Lippert FK , Folke F , Weeke P , Hansen CM , Christensen EF , et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310(13):1377–84. doi:.https://doi.org/10.1001/jama.2013.278483
16 Debaty G , Labarere J , Frascone RJ , Wayne MA , Swor RA , Mahoney BD , et al. Long-Term Prognostic Value of Gasping During Out-of-Hospital Cardiac Arrest. J Am Coll Cardiol. 2017;70(12):1467–76. doi:.https://doi.org/10.1016/j.jacc.2017.07.782
17 Nürnberger A , Sterz F , Malzer R , Warenits A , Girsa M , Stöckl M , et al. Out of hospital cardiac arrest in Vienna: incidence and outcome. Resuscitation. 2013;84(1):42–7. doi:.https://doi.org/10.1016/j.resuscitation.2012.07.002
18 Phelps R , Dumas F , Maynard C , Silver J , Rea T . Cerebral Performance Category and long-term prognosis following out-of-hospital cardiac arrest. Crit Care Med. 2013;41(5):1252–7. doi:.https://doi.org/10.1097/CCM.0b013e31827ca975
19 Lindner TW , Søreide E , Nilsen OB , Torunn MW , Lossius HM . Good outcome in every fourth resuscitation attempt is achievable--an Utstein template report from the Stavanger region. Resuscitation. 2011;82(12):1508–13. doi:.https://doi.org/10.1016/j.resuscitation.2011.06.016
20 Berdowski J , Berg RA , Tijssen JGP , Koster RW . Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–87. doi:.https://doi.org/10.1016/j.resuscitation.2010.08.006
21 Capucci A , Aschieri D , Guerra F , Pelizzoni V , Nani S , Villani GQ , et al. Community-based automated external defibrillator only resuscitation for out-of-hospital cardiac arrest patients. Am Heart J. 2016;172:192–200. doi:.https://doi.org/10.1016/j.ahj.2015.10.018
22 Nordberg P , Hollenberg J , Rosenqvist M , Herlitz J , Jonsson M , Järnbert-Petterson H , et al. The implementation of a dual dispatch system in out-of-hospital cardiac arrest is associated with improved short and long term survival. Eur Heart J Acute Cardiovasc Care. 2014;3(4):293–303. doi:.https://doi.org/10.1177/2048872614532415
23 Lick CJ , Aufderheide TP , Niskanen RA , Steinkamp JE , Davis SP , Nygaard SD , et al. Take Heart America: A comprehensive, community-wide, systems-based approach to the treatment of cardiac arrest. Crit Care Med. 2011;39(1):26–33. doi:.https://doi.org/10.1097/CCM.0b013e3181fa7ce4
24Rettung St. Gallen [Internet]. First Responder [cited 2018 Aug 25]. Teil der Notfallversorgung [about 1 screen]. Available from: http://www.rettung-sg.ch/index.php?id=22
No financial support and no other potential conflict of interest relevant to this article was reported.