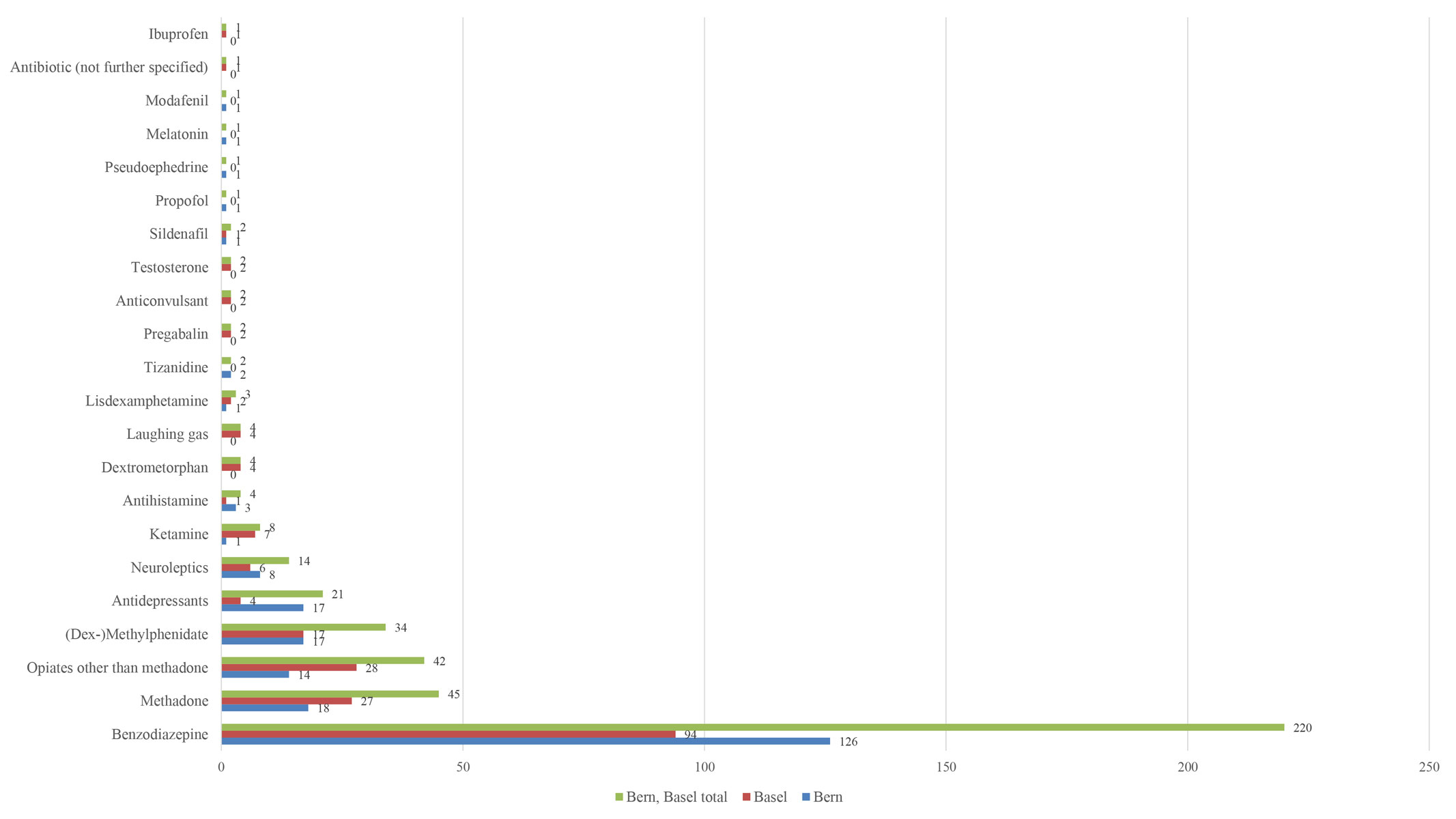
Figure 1 Reported prescription/OTC substances.
DOI: https://doi.org/10.4414/smw.2019.20056
Psychoactive drugs are substances that alter brain functions, consciousness or cognition. They are the substances most often misused for non-medical purposes [1]. Psychoactive substances include not only illicit drugs such as cocaine, cannabis and heroin, but also prescription drugs like benzodiazepines, opioids and over-the-counter (OTC) medications (e.g. dextromethorphan) [1]. The abuse of psychoactive substances is widespread. It is estimated that approximately one in four adults in the European Union have consumed illegal substances at least once in their lifetime [2]. Globally, over 11% of people who abuse illicit substances and/or prescription drugs are estimated to suffer from substance use disorders [3]. In Europe, cannabis and cocaine are the most commonly abused illegal substances [4], while the most widely recreationally used prescription drugs include opioids and benzodiazepines [1].
While the United States has a diverse drug abuse surveillance system, using direct estimates of self-reported drug use and administrative data on drug arrests and drug treatment admissions [5, 6], data collection regarding prescription drug abuse in Europe and Switzerland is sparse. The European Drug Emergencies Network (Euro-DEN) Plus project has been collecting data on acute intoxications with recreational substances (illicit and prescription/OTC drugs) and emergency presentations across Europe since 2013 [7–9]. Two of the 31 European centres currently involved in the project are the University Hospital in Basel (since October 2013) and the Inselspital in Bern (since January 2016). An analysis of data from Bern in the timeframe between May 2012 and April 2016 showed that nearly one-fifth (18%) of emergency department (ED) presentations due to acute intoxications were associated with benzodiazepines or other sedatives [10]. Similar data from Basel showed that benzodiazepines were among the most commonly abused prescription drugs [11, 12].
The aim of the present study was to investigate the prevalence of specific drugs, age- and sex-related consumption patterns and time trends of ED presentations related to acute medical problems after recreational use of prescription/OTC drugs in two major Swiss tertiary care hospitals in order to identify susceptible groups and local differences, which could have major public health implications for primary care givers.
In this retrospective analysis, we included all patients presenting with acute medical problems related to the recreational use of prescription or OTC drugs to the ED of the University Hospital of Bern between 1 May 2012 and 31 August 2017 and the ED of the University Hospital of Basel between 1 October 2013 and 31 July 2017. Both EDs are primary care facilities (walk-in patients) and tertiary referral centres for hospitals in the greater Bern and Basel areas. The study was approved by the local ethics committees.
From the electronic patient chart databases of both EDs, cases were extracted using a comprehensive full-text search algorithm. This search identified all cases related to abuse, intoxication or related terms, with a large number of substance names including abbreviations and misspellings. Data abstraction was performed in a standardised manner based on the methodology used in the Euro-DEN/Euro-DEN Plus project [8, 10–12]. All cases were reviewed manually and patients with acute toxicity related to recreational use of prescription/OTC drugs were included in our analysis. We identified the drug(s) associated with the presentation based on the patient’s self-reported use, information from bystanders or witnesses and the diagnosis of the physicians assessing the patient at the ED. Abuse of prescription/OTC drugs was defined as use of a drug with a medical indication for recreational rather than for medical purposes. For example, recreational use of the OTC cough medication dextromethorphan was included, but not the recreational use of caffeine pills, as they do not have a medical indication. Furthermore, we excluded drugs with the sole indication of substitution treatment for severe addiction. For example, heroin (available in Switzerland for substitution in severe heroin addiction) was excluded, but cases with recreational use of methadone (labelled for substitution treatment but also for pain management) were included. Further exclusion criteria were: intoxication in the context of a suicidal attempt, isolated ethanol intoxication, symptoms of drug withdrawal, and complications of chronic drug use (e.g. infected injection sites). Cases with positive analytical tests without clinical signs of acute toxicity were not included.
We recorded the patient demographics (age, sex, hour and weekday of ED admission), the substances involved, the clinical symptoms, and the clinical outcome. Clinical features included the Glasgow Coma Scale (GCS) score, heart rate, blood pressure, respiratory rate, body temperature, laboratory tests and electrocardiography (ECG) findings. In cases where the GCS score was not recorded, “alert”, “drowsy” or “coma” was used, based on the notes of the treating clinician. We assessed the severity of poisoning with the Poisoning Severity Score for grading acute poisoning [13]. Minor toxicity refers to mild, transient and spontaneously resolving symptoms, moderate toxicity refers to pronounced or prolonged symptoms, severe toxicity indicates severe or life-threatening symptoms and fatal indicates that the intoxication resulted in death.
In Bern, analytical results are based on urine drug screening using an immunoassay (Triage® TOX Drug Screen, Alere, Cologne, Germany) for amphetamines, barbiturates, benzodiazepines, cocaine, methadone, methamphetamines (including MDMA), opiates, phencyclidine (PCP), tricyclic antidepressants and tetrahydrocannabinol (cannabis) [14]. Ethanol levels were estimated from osmolar gap. Analytical findings in Basel are based on CEDIA immunoassays (Thermo Fisher Scientific, Passau, Germany) for barbiturates, amphetamines (including MDMA), benzodiazepines, cocaine, cannabis, methadone and heroin, and DRI immunoassays (Thermo Fisher Scientific, Passau, Germany) for tricyclic antidepressants and opiates. Ethanol blood levels and γ-hydroxybutyrate (GHB) levels were determined by an enzymatic assay. An additional liquid chromatography-tandem mass spectrometry (LC-MS/MS) analysis with a method covering over 770 substances [15] was also available in some cases.
Data from Bern and Basel were also analysed separately to identify local differences. The data were arranged by consecutive month/year of presentation, type of prescribed/OTC substance(s) abused, co-abuse of other psychoactive substances, age, sex, and severity of intoxication. We investigated time trends, sex differences and consumption patterns within three age groups (young: ≥16 to <36 years; middle-aged: ≥36 to <56 years; elderly ≥56 years). To investigate time trends, we fitted a linear regression with a Poisson distribution, with time as the independent variable and number of ED presentations due to prescription/OTC drugs as the dependent variable. To further investigate sex differences, two separate regressions were performed for men and women. To find which age group has the greatest potential for abusive behaviour, we analysed the frequency of ED presentations in the three age groups. We further examined the severity of intoxication with prescription/OTC drugs over time to see whether an increase or decrease in intoxication severity could be found. The individual presentations at the ED were considered independent of each other. Statistical significance was defined on the basis of a two-sided nominal p-value of 0.05. Statistical analyses were conducted using the statistical software R using a generalised linear model (glm) with a Poisson distribution (family = ‘Poisson’) to analyse count data on the number of cases presented per month to identify time trends [16]. Differences were tested using the chi-square test for categorical variables where levels were recorded exclusively, i.e. sex, age groups, ethanol co-ingestion.
During the study period there were 1715 cases of acute recreational drug toxicity (818 in Bern and 897 in Basel) among a total of 412,557 ED presentations (218,166 in Bern and 194,391 in Basel). After applying the inclusion and exclusion criteria, 344 cases related to acute toxicity of prescription/OTC drugs were extracted and included in the present analysis, of which 190 cases were retrieved in Bern and 154 Basel, corresponding to 23% and 17% of acute recreational drug toxicity ED attendances in Bern and Basel, respectively. The mean patient age was 36 years (SD 11.4, range 16–73). In total, 73% (n = 250) of patients were brought to the ED by ambulance. The patient characteristics are shown in table 1. No statistically significant differences in sex, age groups and ethanol co-ingestion were found between the two sites (table 1).
Table 1 Patient characteristics Bern and Basel.
|
Bern + Basel
(n = 344) Number of cases (%) |
Bern
(n = 190) Number of cases (%) |
Basel
(n = 154) Number of cases (%) |
||
|---|---|---|---|---|
| Sex | Female | 126 (37) | 73 (38) | 53 (34) |
| Male | 218 (63) | 117 (62) | 101 (66) | |
| Age group (years) | ≥16 to <36 | 166 (48) | 95 (50) | 71 (46) |
| ≥36 to <56 | 147 (43) | 82 (43) | 65 (42) | |
| ≥56 | 30 (9) | 13 (7) | 17 (11) | |
| Unknown | 1 (<1) | 0 (0) | 1 (<1) | |
| Time of presentation | Night arrival (20:00–8:00) | 163 (47) | 82 (43) | 81 (53) |
| Weekend arrival (Friday 17:00 to Monday 8:00) | 131 (38) | 73 (38) | 58 (38) | |
| Ethanol co-ingestion (self-reported) | Yes | 174 (51) | 98 (52) | 76 (49) |
| No | 54 (16) | 24 (13) | 30 (19) | |
| Not known | 116 (34) | 68 (36) | 48 (31) | |
| Drug use reported | 1 substance | 134 (39) | 83 (44) | 51 (33) |
| >1 substance | 210 (61) | 107 (56) | 103 (67) | |
| >1 prescription/OTC | 85 (25) | 34 (18) | 51 (27) | |
| Co-use with an illicit drug | 168 (49) | 90 (47) | 78 (51) | |
In both hospitals, the most frequently reported recreationally used prescription drugs were benzodiazepines (64%, n = 220 in both centres collectively; 66%, n = 126 in Bern; 61%, n = 94 in Basel) (fig. 1). In Bern, benzodiazepines were followed by methadone (10%, n = 18), (dex)methylphenidate and antidepressants (both 9%, n = 17) (fig. 1). In Basel, benzodiazepines were followed by opiates other than methadone (18%, see below), methadone (18%) and (dex)methylphenidate (11%) (fig. 1).
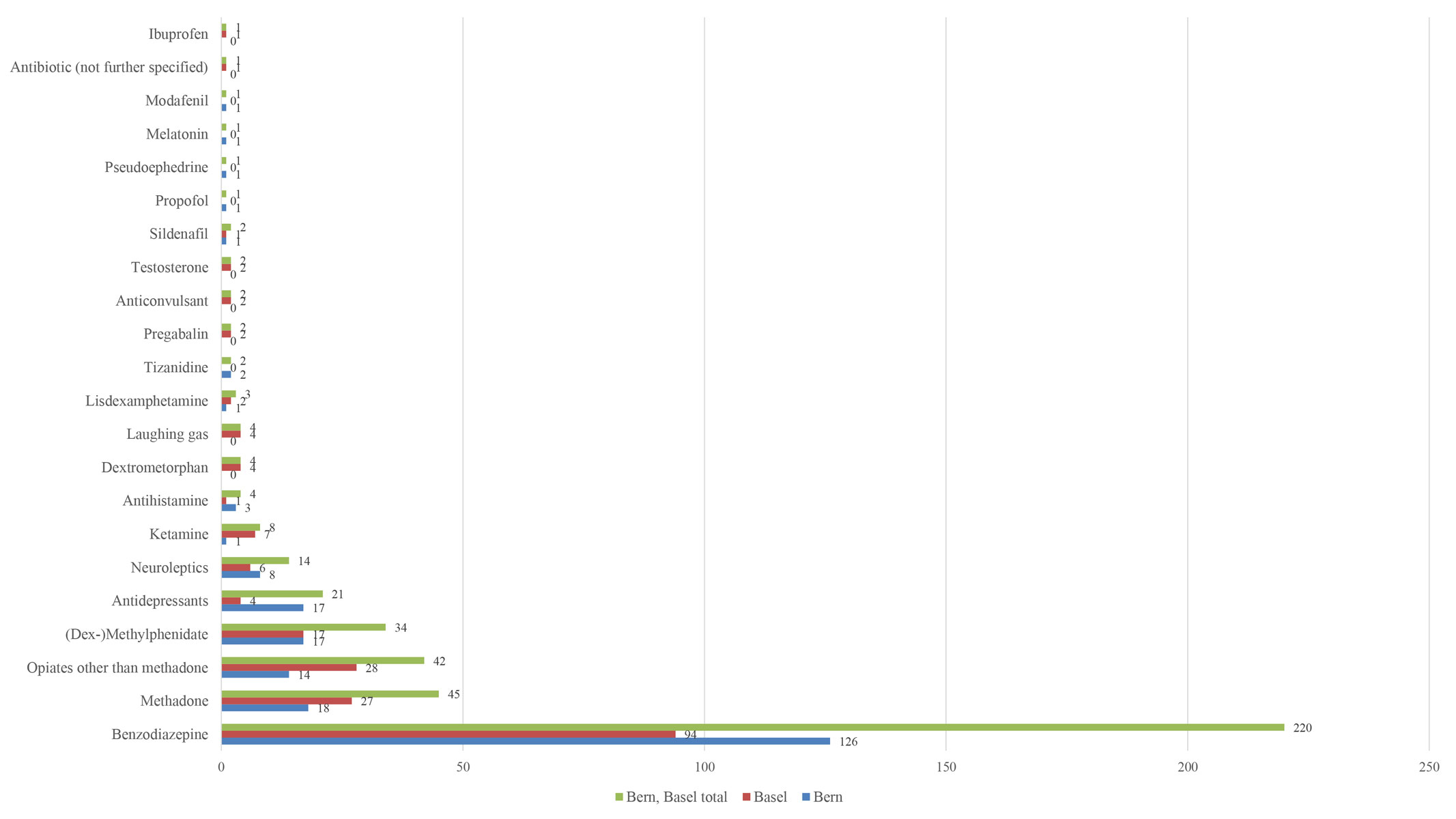
Figure 1 Reported prescription/OTC substances.
In both centres, the most commonly reported benzodiazepines were diazepam, lorazepam and midazolam. While in Bern the most commonly used benzodiazepine was midazolam (33%, n = 41), followed by diazepam (22%, n = 28) and lorazepam (15%, n = 19), in Basel diazepam (29%, n = 27) was most frequently used, followed by lorazepam (21%, n = 20) and midazolam (16%, n = 15). In 14 (11%) and 29 (31%) cases, a further specification of the benzodiazepine used was not available in Bern and Basel, respectively. Following methadone (13%, n = 45), morphine (50%, n = 21) and tramadol (14%, n = 6) were the most commonly used opioids in both centres collectively. In Bern, the most commonly used opioids (other than methadone) were morphine (35%, n = 5), tramadol (21%, n = 3) and codeine or codeine-containing agents (21%, n = 3) (e.g. the cough syrup Resyl Plus®). In Basel, the most commonly used opioids (other than methadone) were morphine (61%, n = 17), tramadol (14%, n = 4), codeine (7%, n = 2) and oxycodone (4%, n = 1). A further specification of the consumed opioids was not reported in 3 (21%) and 4 (14%) cases in Bern and Basel, respectively.
The youngest age group had the most ED presentations in both hospitals (table 1). In Basel, the analysis of time trends showed a significant increase in presentations in the youngest age group (p = 0.013; estimated increase in cases per month = 0.02, 95% CI 0.006–0.043) and the oldest group (p = 0.02; estimated increase in cases per month = 0.05, 95% CI 0.011–0.093), while in Bern the trend remained stable over time for all age groups (fig. 2). While in Bern the number of presentations remained constant over time for men (increase in cases of 0.0003 per month, p = 0.96) and women (decrease in cases of 0.002 per month, p = 0.71) in Bern, a significant increase was found for the female cohort in Basel (p = 0.032; estimated increase in cases per month = 0.04, 95% CI 0.019–0.065) (fig. 3). The male cohort in Basel showed a non-significant increase in cases per month of 0.01 (p = 0.15).
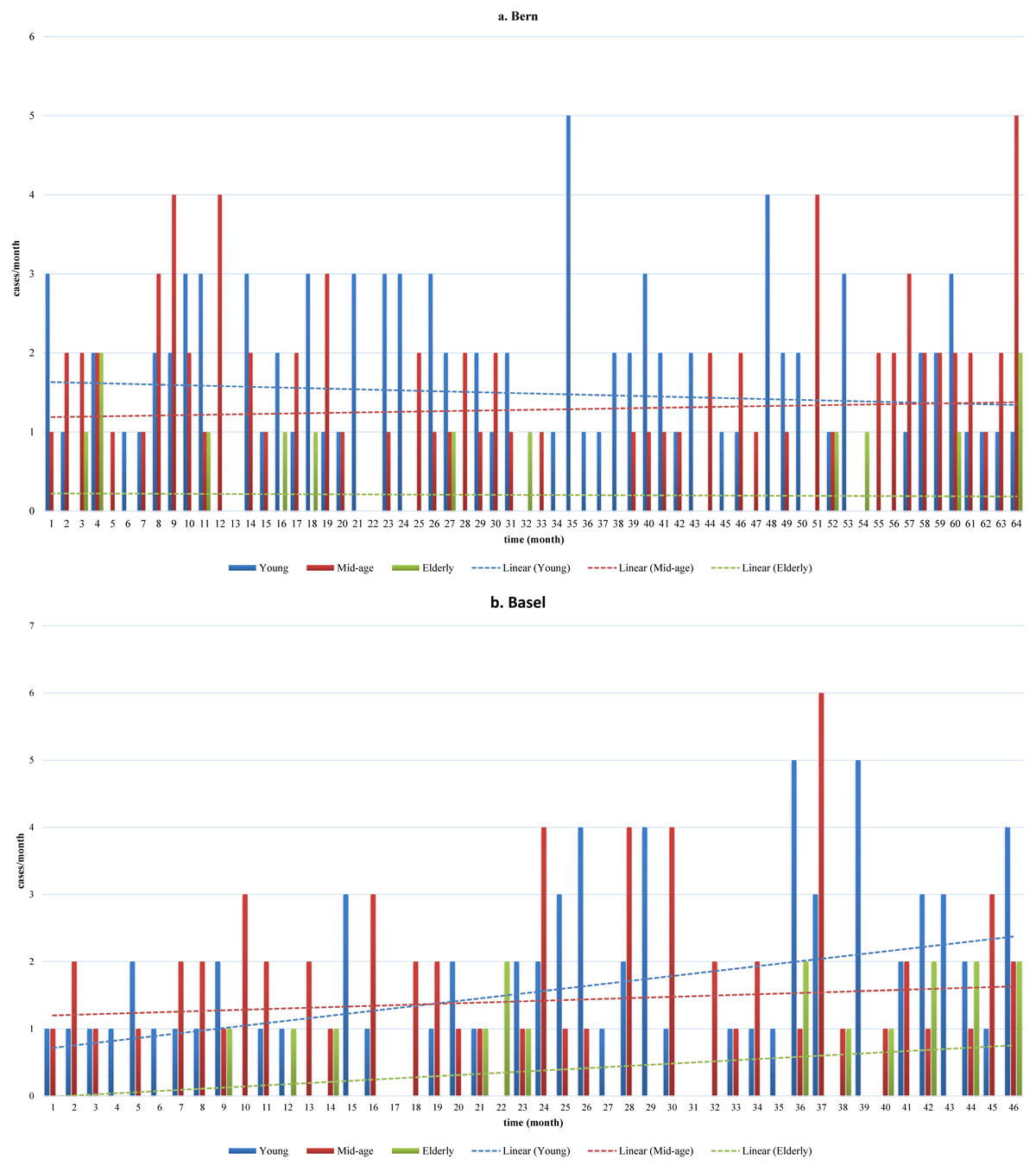
Figure 2 Time trends in the number of presentations by age group in (a) Bern, (b) Basel.
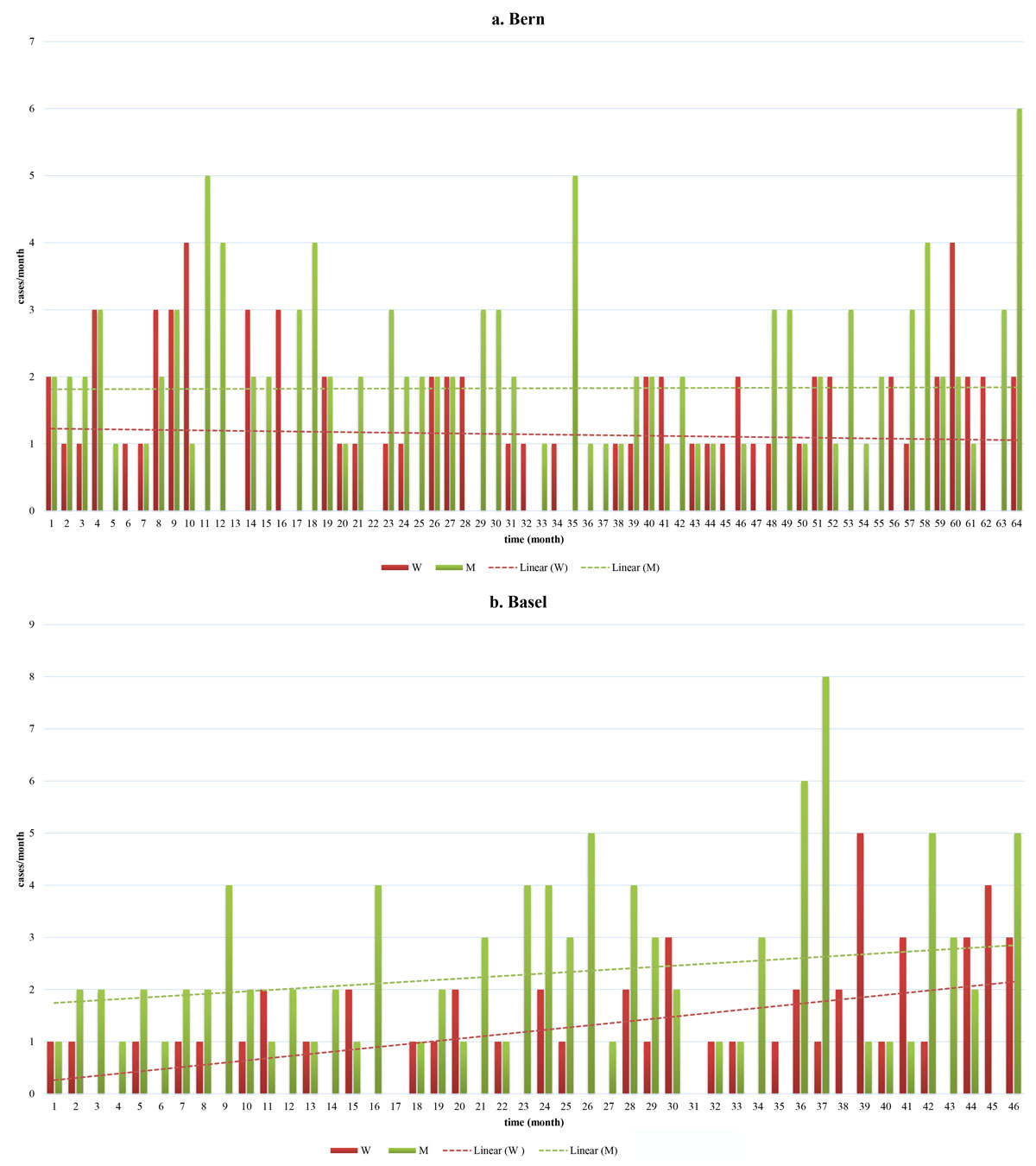
Figure 3 Time trends in the number of presentations by sex in (a) Bern, (b) Basel.
Patients in all age groups in both cohorts presented with toxicities of predominantly minor severity (fig. 4). One fatal case occurred, in the mid-aged group in Bern: a 39-year-old female patient died due to a generalised brain oedema, most likely as a consequence of hypoxia after oral intake of an estimated dose of 180 mg methadone. While the number of cases with minor severity increased significantly over time in Basel (p <0.001), with an increase of 0.032 cases per month, the number of minor severity cases in Bern decreased (p = 0.042). We checked for correlations between the time trends of all types of severity and found no statistical significance (fig. S1 in appendix 1).
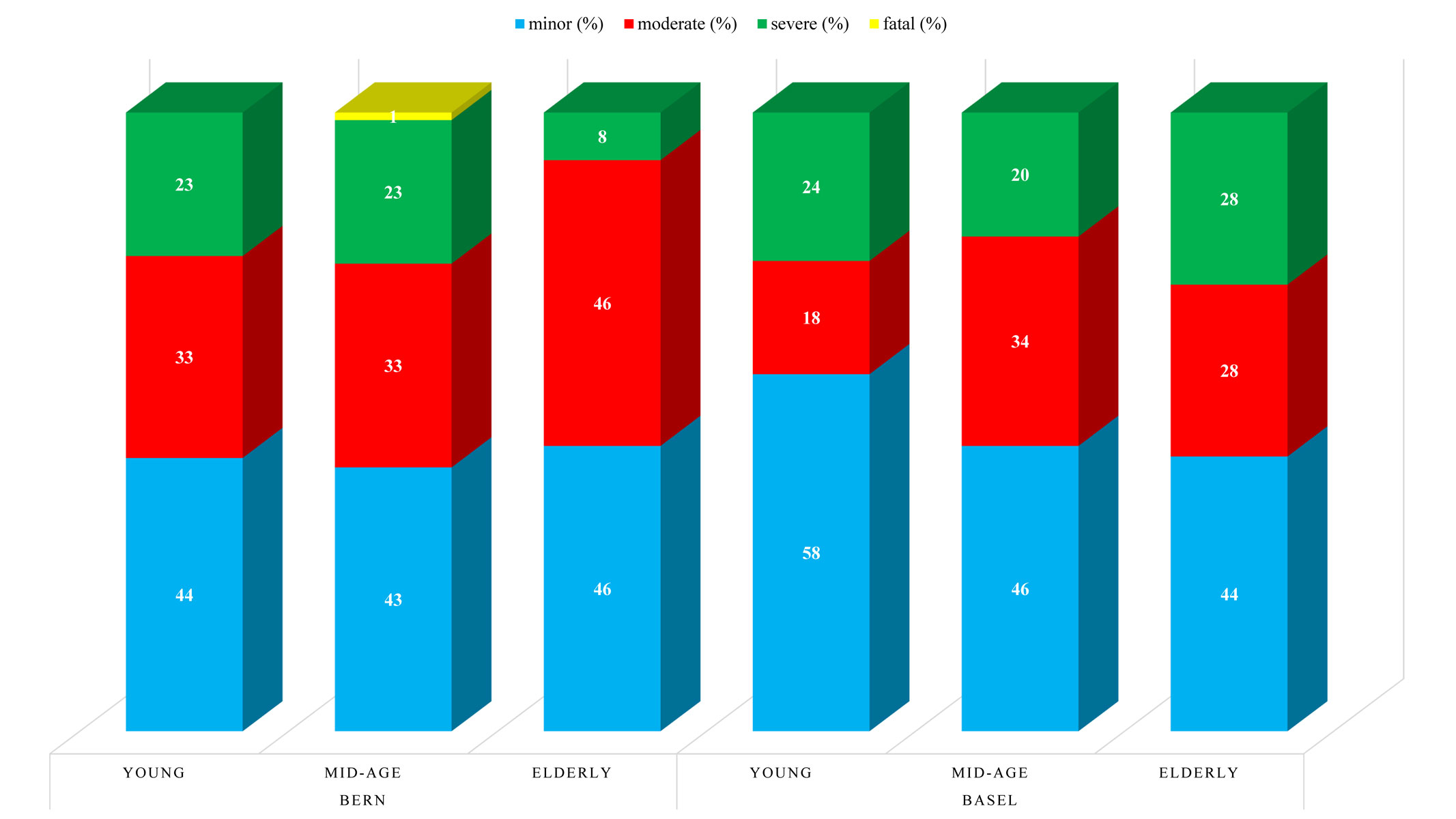
Figure 4 Severity of intoxication by age group in Bern and Basel.
Among all cases from both centres, co-use of ethanol was reported in 49% (n = 37) of severe cases, 48% (n = 49) of moderate severity cases and 54% (n = 88) of minor severity cases. The use of more than one substance (either prescription/OTC or illicit drug(s)) was reported in 72% (n = 55) of severe cases, 69% (n = 71) of moderate severity cases and 51% (n = 84) of minor severity cases in both centres collectively. The co-use of illicit substances was reported in 55% (n = 42) of all severe cases, 56% (n = 58) of all moderate severity cases and 41% (n = 68) of all minor severity cases collectively. A detailed summary of the co-used substances reported at each centre by severity of intoxication is shown in table 2. Three cases reported having taken an unknown substance in addition to a prescription/OTC drug in Basel. In Bern, no such cases occurred.
Table 2 Reported co-use patterns in Bern and Basel by severity of intoxication.
| Ethanol co-use | >1 substance (more than one prescription/OTC or additional illicit drug) | Co-use of illicit substance(s) | ||
|---|---|---|---|---|
| Both centres combined n (%) |
Minor (n = 164) | 88 (54) | 84 (51) | 68 (41) |
| Moderate (n = 103) | 49 (48) | 71 (69) | 58 (56) | |
| Severe (n = 76) | 37 (49) | 55 (72) | 42 (55) | |
| Fatal (n = 1) | na | na | na | |
| Total (n = 344) | 174 (51) | 210 (61) | 168 (49) | |
| Bern n (%) |
Minor (n = 83) | 44 (53) | 39 (47) | 31 (37) |
| Moderate (n = 64) | 29 (45) | 39 (61) | 34 (53) | |
| Severe (n = 42) | 25 (60) | 29 (69) | 25 (60) | |
| Fatal (n = 1) | na | 0 (0) | 0 (0) | |
| Total (n = 190) | 98 (52) | 107 (56) | 90 (47) | |
| Basel n (%) |
Minor (n = 81) | 44 (54) | 45 (56) | 37 (46) |
| Moderate (n = 39) | 20 (51) | 32 (82) | 24 (62) | |
| Severe (n = 34) | 12 (35) | 26 (76) | 17 (50) | |
| Fatal (n = 0) | na | na | na | |
| Total (n = 154) | 76 (49) | 103 (67) | 78 (51) | |
na = not applicable or information not available
The patient symptoms are shown in table 3. Medical treatment including e.g. intravenous fluid administration was provided in 277 cases (81%) collectively, with 157 (83%) cases in Bern and 120 (78%) cases in Basel. Tracheal intubation was performed in 11 (3%) cases overall (6 (3%) cases in Bern and 5 (3%) in Basel). Benzodiazepines and/or antipsychotics were administered in 57 (17%) cases overall (32 (17%) in Bern and 25 (16%) in Basel). The data regarding discharge from the ED are summarised in table 4.
Table 3 Clinical presentations in Bern and Basel.
|
Bern + Basel
n = 344 |
Bern
n = 190 |
Basel
n = 154 |
||
|---|---|---|---|---|
| Cardiovascular n (%) |
Chest pain | 10 (3) | 4 (2) | 6 (4) |
| Palpitations | 9 (3) | 5 (3) | 4 (3) | |
| Dyspnoea | 12 (3) | 6 (3) | 6 (4) | |
| Hypertension (systolic blood pressure ≥180 mm Hg) | 9 (3) | 8 (4) | 1 (1) | |
| Hypotension (systolic blood pressure ≤90 mm Hg) | 16 (5) | 13 (7) | 3 (2) | |
| Tachycardia (> 100 beats per minute) | 70 (20) | 40 (21) | 30 (19) | |
| Myocardial infarction | 2 (1) | 1 (1) | 1 (1) | |
| Arrhythmias | 5 (1) | 2 (1) | 3 (2) | |
| Psychiatric n (%) |
Anxiety, nervousness and/or fear | 69 (20) | 47 (25) | 22 (14) |
| Psychosis | 16 (5) | 13 (7) | 3 (2) | |
| Hallucinations | 18 (5) | 13 (7) | 5 (3) | |
| Agitation and/or aggression | 80 (23) | 55 (29) | 25 (16) | |
| Panic attack | 2 (1) | 2 (1) | 0 (0) | |
| Insomnia | 10 (3) | 5 (3) | 5 (3) | |
| Suicidal ideation | 3 (1) | 3 (2) | 0 (0) | |
| Neurological n (%) |
Loss of consciousness (GCS <8) on presentation or pre-hospital | 12 (3) | 3 (2) | 9 (6) |
| Impaired consciousness (GCS <15) on presentation or pre-hospital | 115 (33) | 90 (47) | 25 (16) | |
| Vertigo and/or dizziness | 15 (4) | 10 (6) | 5 (3) | |
| Headache | 10 (3) | 7 (4) | 3 (2) | |
| Paraesthesia | 5 (1) | 2 (1) | 3 (2) | |
| Seizure | 10 (3) | 4 (2) | 6 (4) | |
| Tremor | 9 (3) | 6 (3) | 3 (2) | |
| Amnesia | 13 (4) | 9 (5) | 4 (3) | |
| Other neurological symptoms n (%) |
Miosis | 55 16) | 34 (18) | 21 (14) |
| Mydriasis | 25 (7) | 15 (8) | 10 (6) | |
| Respiratory depression | 56 (16) | 35 (18) | 21 (14) | |
| Miscellaneous n (%) |
Hyperventilation | 6 (2) | 4 (2) | 2 (1) |
| Nausea and/or vomiting | 28 (8) | 14 (7) | 14 (9) | |
| Sweating | 10 (3) | 9 (5) | 1 (1) | |
| Malaise | 5 (1) | 4 (2) | 1 (1) | |
| Abdominal pain | 7 (2) | 4 (2) | 3 (2) | |
| Hyperthermia (≥39.0°C) | 2 (1) | 1 (1) | 1 (1) | |
| Muscle cramps | 7 (2) | 5 (3) | 2 (1) | |
| Injuries (e.g., fracture, wound) | 10 (3) | 2 (1) | 8 (5) | |
GCS = Glasgow Coma Scale
Table 4 Discharge data in Bern and Basel, n (%).
|
Bern + Basel
n = 344 |
Bern
n = 190 |
Basel
n = 154 |
|
|---|---|---|---|
| Medically discharged home | 182 (53) | 100 (53) | 82 (53) |
| Self-discharged | 41 (12) | 14 (7) | 27 (18) |
| Admission to critical care unit | 37 (11) | 18 (9) | 19 (12) |
| Admission to ward other than critical care unit | 28 (8) | 14 (6) | 14 (9) |
| Admission to psychiatric clinic | 56 (16) | 44 (23) | 12 (8) |
This study describes presentations related to acute toxicity after recreational prescription/OTC drug use at the EDs of two urban hospitals in Switzerland during a time period of five (Bern) and four (Basel) years. In both hospitals, approximately one-fifth of presentations due to acute recreational drug use were related to prescription/OTC drugs. The typical patient was male and belonged to the youngest age group. Benzodiazepines were the most commonly reported prescription drugs used. Use of more than one substance was common, with use of more than one prescription/OTC drug or co-use of illicit drug(s) in more than half the cases in Bern and in two-thirds of the patients in Basel. Ethanol co-use occurred in approximately half the cases in both hospitals. There was one fatality, and further severe complications included two cases of myocardial infarction. Our time trend analysis showed an increase in presentations related to recreational use of prescription/OTC drugs in the youngest and oldest group, and in the female cohort in Basel.
The prescription/OTC drugs most frequently leading to ED presentations after acute recreational intoxication were benzodiazepines. In both hospitals, midazolam, diazepam and lorazepam were the most commonly recreationally used benzodiazepines, possibly reflecting the local availability on the black market or, more likely, prescription trends of local physicians. However, the type of benzodiazepine was not always reported. The pattern seen in our analysis is similar to that of prescription drug abuse seen in Europe, where sedatives and hypnotics are among the most commonly abused prescription drugs [17]. To improve sleep, to cope with stress and to get high are the main reasons reported for the abuse of sedatives and hypnotics [18].
After benzodiazepines, methadone and other opioids were the most commonly used prescription/OTC drugs in both our cohorts. The only patient with a fatal outcome in our analysis had used methadone belonging to her partner, who was under maintenance therapy. This highlights the importance of avoiding high permissible dosage dispensations. Almost two-thirds (63%) of patients under substitution receive methadone in Europe [1]. In the last twenty years, the use of prescription opioids has increased [19]. The leading motive for non-medical use in about 40% of cases was pain relief. However, about every other user of non-medical prescription opioids reported non-pain relief motives only, e.g. to get drugged or to relax [20].
After benzodiazepines and opioids, the third most commonly abused prescription drug in our cohorts was methylphenidate. An analysis in the US showed an increase in the abuse of prescription stimulants in recent years, especially among high school and college students [21]. Reasons for using stimulants reported by US university students were to increase their alertness and energy [22]. Another study among Swiss secondary school students showed that methylphenidate was the drug most frequently used to enhance cognition [23].
Most ED presentations occurred in the youngest age group in both hospitals. Teenagers and young adults especially seem to believe that prescribed medications are safer than illicit drugs, even when used illicitly [24, 25]. The motivations associated with the abuse of prescription drugs by teenagers are, among others, self-medication of e.g. anxiety or insomnia, to enhance performance and to get high or experiment, often in combination with alcohol [20, 24, 25]. Our analysis of time trends showed a significant increase in presentations not only in the youngest, but also in the oldest group in Basel. According to reviews of psychoactive drug abuse in elderly patients, the leading factors for drug abuse are social isolation, history of substance-use or mental health disorders and exposure to prescription drugs with abuse potential [26]. Different approaches compared to those for younger patients might be necessary when treating abuse disorders in this patient population [26]. The different spectrum of motivations in different age groups requires intervention strategies that address the diversity of motivations.
In our study, a significant increase in presentations over time was found for the female cohort in Basel. In previous studies with chronic pain patients, women were found to keep unused medications as well as using additional drugs (e.g. sedatives) to enhance the effect of analgesics more frequently than men [27]. Our results might also suggest differences regarding the drug prescribing practices of physicians towards men and women.
Although cases of minor severity increased over time in Basel and decreased in Bern, the contrast with cases of moderate and severe severity was not significant, thus indicating that the increase in minor severity in Basel is not related to a decrease of moderate and severe severity cases. Moreover, the results reflect local trends over a limited period of four (Basel) and five years (Bern).
Our study has limitations. The study was retrospective, and the study duration was too short to reliably determine time trends, for which longer studies would be more appropriate. Due to the limited dataset, some significant results could be spurious findings, and further studies with an independent set of data would be necessary to replicate and validate these findings, rendering them more robust. We used self-reports as references, which carries the risk of reporting biases and may vary in accuracy. Moreover, data from the two ED may reflect a regional trend and may not be representative of the whole country. Some symptoms could have been due to withdrawal and not due to acute substance toxicity (e.g. seizures in case of benzodiazepine withdrawal). Severe intoxications may have been overrepresented because of the co-use of alcohol or other psychoactive substances in many cases. Some patients were transferred directly from the ED to the psychiatric ward without a full check-up. In these cases the data retrieved were limited. Furthermore, the source of abused prescription/OTC drugs (e.g. black market, prescription, internet) is often not reported and thus important information for combatting the abuse remains unaccounted for.
We regard the search algorithm, which provides us with a detailed and sensitive search result, and the manual review of all cases as a strength of this study. Our study is not based solely on coded diagnoses or laboratory results, which carry the risk of including patients with e.g. regular or iatrogenic benzodiazepine intake. Furthermore, our systematic data abstraction and analysis makes comparison with similar data easier.
This retrospective study at two urban EDs in Switzerland showed that most presentations due to acute recreational prescription/OTC drug toxicity were associated with benzodiazepines, methadone and other opioids. In contrast to other countries, benzodiazepines seem to be more widely recreationally used than opioids and/or lead to more ED attendances. This potentially indicates a national trend or the greater local availability of benzodiazepines. Furthermore, a significant increase in presentations was seen not only within the youngest, but also in the oldest age group and in females in one of the study cohorts. Health care providers should be alert to current demographic trends of prescription/OTC abuse. This information can be used to adapt the prevention and treatment strategies in their communities without compromising drug access to patients who use them correctly.
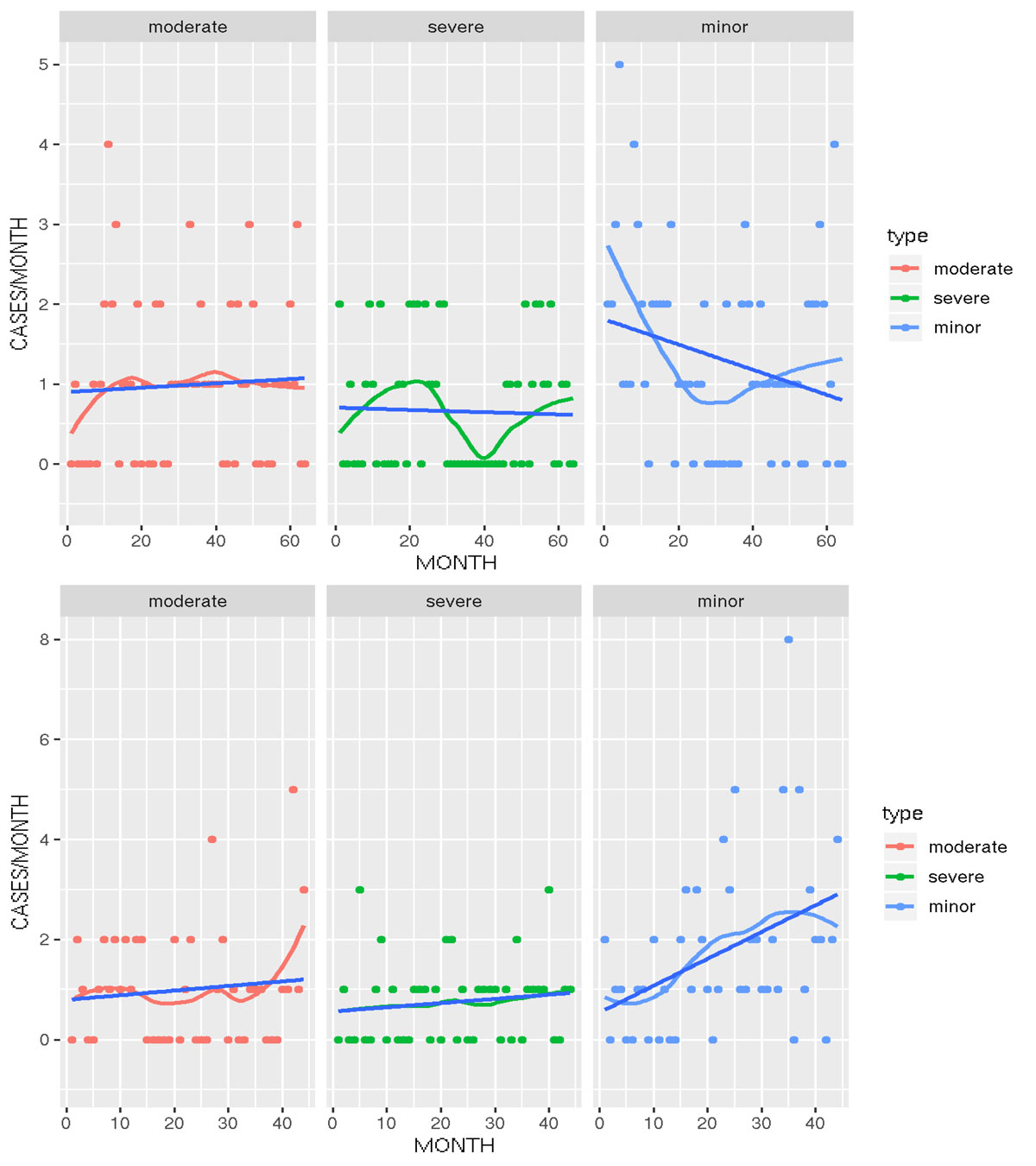
Figure S1 Trends in severity of toxicity in (a) Bern, (b) Basel. Red, green and light blue = lowess (locally weighted scatterplot smoothing) curve fit.
We thank Sabine Müller and Adrian Stoller for their assistance with the data abstraction.
MEL, YS and EL received funding from the Swiss Centre for Applied Human Toxicology.
The authors have no conflict of interest to report.
1European Drug Report 2018. Trends and Developments 2018; Available from: http://www.emcdda.europa.eu/edr2018_en.
2European Monitoring Centre for Drugs and Drug Abuse. Data Tables. 2015. http://www.emcdda.europa.eu/stats13#display:/stats13/gpstab1c, in emcdda.
3World Drug Report Global overview of drug demand and supply. 2017; Available from: https://www.unodc.org/wdr2017/field/Booklet_2_HEALTH.pdf.
4 Mena G , Giraudon I , Álvarez E , Corkery JM , Matias J , Grasaasen K , et al. Cocaine-related health emergencies in Europe: a review of sources of information, trends and implications for service development. Eur Addict Res. 2013;19(2):74–81. doi:.https://doi.org/10.1159/000341719
5Monitoring the future national results on drug use: key findings on adolescent drug use. 2013; Available from: https://deepblue.lib.umich.edu/bitstream/handle/2027.42/142406/Overview%202017%20FINAL.pdf?sequence=1&isAllowed=y.
6 Paulozzi LJ , Strickler GK , Kreiner PW , Koris CM ; Centers for Disease Control and Prevention (CDC). Controlled Substance Prescribing Patterns--Prescription Behavior Surveillance System, Eight States, 2013. MMWR Surveill Summ. 2015;64(SS09):1–14. doi:.https://doi.org/10.15585/mmwr.ss6409a1
7 Heyerdahl F , Hovda KE , Giraudon I , Yates C , Dines AM , Sedefov R , et al. Current European data collection on emergency department presentations with acute recreational drug toxicity: gaps and national variations. Clin Toxicol (Phila). 2014;52(10):1005–12. doi:.https://doi.org/10.3109/15563650.2014.976792
8 Wood DM , Heyerdahl F , Yates CB , Dines AM , Giraudon I , Hovda KE , et al. The European Drug Emergencies Network (Euro-DEN). Clin Toxicol (Phila). 2014;52(4):239–41. doi:.https://doi.org/10.3109/15563650.2014.898771
9 Dines AM , Wood DM , Yates C , Heyerdahl F , Hovda KE , Giraudon I , et al.; Euro-DEN Research Group. Acute recreational drug and new psychoactive substance toxicity in Europe: 12 months data collection from the European Drug Emergencies Network (Euro-DEN). Clin Toxicol (Phila). 2015;53(9):893–900. doi:.https://doi.org/10.3109/15563650.2015.1088157
10 Liakoni E , Müller S , Stoller A , Ricklin M , Liechti ME , Exadaktylos AK . Presentations to an urban emergency department in Bern, Switzerland associated with acute recreational drug toxicity. Scand J Trauma Resusc Emerg Med. 2017;25(1):26. doi:.https://doi.org/10.1186/s13049-017-0369-x
11 Liakoni E , Dolder PC , Rentsch K , Liechti ME . Acute health problems due to recreational drug use in patients presenting to an urban emergency department in Switzerland. Swiss Med Wkly. 2015;145:w14166. doi:.https://doi.org/10.4414/smw.2015.14166
12 Liakoni E , Dolder PC , Rentsch KM , Liechti ME . Presentations due to acute toxicity of psychoactive substances in an urban emergency department in Switzerland: a case series. BMC Pharmacol Toxicol. 2016;17(1):25. doi:.https://doi.org/10.1186/s40360-016-0068-7
13 Persson HE , Sjöberg GK , Haines JA , Pronczuk de Garbino J . Poisoning severity score. Grading of acute poisoning. J Toxicol Clin Toxicol. 1998;36(3):205–13. doi:.https://doi.org/10.3109/15563659809028940
14Alere TM Triage® TOX Drug Screen Product Insert. Rapid Qualitative simultaneous detection of drug and/or the major urinary metabolites of 10 different drug classes (11 unique assays). 2013; Available from: http://www.alere.com/en/home/product-details/triage-tox-drug-screen-au.html.
15 Mueller DM , Rentsch KM . Online extraction toxicological MS(n) screening system for serum and heparinized plasma and comparison of screening results between plasma and urine in the context of clinical data. J Chromatogr B Analyt Technol Biomed Life Sci. 2012;883-884:189–97. doi:.https://doi.org/10.1016/j.jchromb.2011.08.022
16R Core Team (2013). R Foundation for Statistical Computing, Vienna, Austria; Available from: http://www.R-project.org/.
17 Casati A , Sedefov R , Pfeiffer-Gerschel T . Misuse of medicines in the European Union: a systematic review of the literature. Eur Addict Res. 2012;18(5):228–45. doi:.https://doi.org/10.1159/000337028
18 Kapil V , Green JL , Le Lait C , Wood DM , Dargan PI . Misuse of benzodiazepines and Z-drugs in the UK. Br J Psychiatry. 2014;205(5):407–8. doi:.https://doi.org/10.1192/bjp.bp.114.149252
19 Kolodny A , Courtwright DT , Hwang CS , Kreiner P , Eadie JL , Clark TW , et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36(1):559–74. doi:.https://doi.org/10.1146/annurev-publhealth-031914-122957
20 McCabe SE , Cranford JA , Boyd CJ , Teter CJ . Motives, diversion and routes of administration associated with nonmedical use of prescription opioids. Addict Behav. 2007;32(3):562–75. doi:.https://doi.org/10.1016/j.addbeh.2006.05.022
21 Lakhan SE , Kirchgessner A . Prescription stimulants in individuals with and without attention deficit hyperactivity disorder: misuse, cognitive impact, and adverse effects. Brain Behav. 2012;2(5):661–77. doi:.https://doi.org/10.1002/brb3.78
22 Hall KM , Irwin MM , Bowman KA , Frankenberger W , Jewett DC . Illicit use of prescribed stimulant medication among college students. J Am Coll Health. 2005;53(4):167–74. doi:.https://doi.org/10.3200/JACH.53.4.167-174
23 Liakoni E , Schaub MP , Maier LJ , Glauser GV , Liechti ME . The Use of Prescription Drugs, Recreational Drugs, and “Soft Enhancers” for Cognitive Enhancement among Swiss Secondary School Students. PLoS One. 2015;10(10):e0141289. doi:.https://doi.org/10.1371/journal.pone.0141289
24Substance Abuse and Mental Health Services Administration. Results from the 2007 National Survey on Drug Use and Health: National Findings, in Rockville, MD: 2008. Office of Applied Studies, NSDUH Series H-34, DHHS Publication No. SMA 08-4343(Table B-8).
25 Volkow ND . Teen prescription drug abuse a major health concern. Tenn Med. 2009;102(4):28–9.
26 Simoni-Wastila L , Yang HK . Psychoactive drug abuse in older adults. Am J Geriatr Pharmacother. 2006;4(4):380–94. doi:.https://doi.org/10.1016/j.amjopharm.2006.10.002
27 Back SE , Payne RA , Waldrop AE , Smith A , Reeves S , Brady KT . Prescription opioid aberrant behaviors: a pilot study of sex differences. Clin J Pain. 2009;25(6):477–84. doi:.https://doi.org/10.1097/AJP.0b013e31819c2c2f
MEL, YS and EL received funding from the Swiss Centre for Applied Human Toxicology.
The authors have no conflict of interest to report.