Use of cardiac magnetic resonance imaging and single photon emission computed tomography for the diagnosis of stable coronary artery disease in Switzerland
DOI: https://doi.org/10.4414/smw.2019.20080
Jeanne
du Fay de Lavallaza, Michael J.
Zellwegera, Stefan
Felderbc
aDepartment of Cardiology, University Hospital Basel, Switzerland
bHealth Economics, Faculty of Business and Economics, University of Basel, Switzerland
cSwiss Medical Board, Switzerland
Summary
BACKGROUND
Direct invasive testing in the diagnosis of stable coronary artery disease (CAD) involves high costs and relevant risks. By comparison, single-photon emission computed tomography (SPECT) and cardiac magnetic resonance imaging (CMR) are noninvasive diagnostic tests. SPECT is currently the most widely used diagnostic technique, but new medical and economic evidence favours CMR. Guidelines do not recommend one technique in preference to the other, and their use in Switzerland is poorly documented, as a scoping study by the Swiss Medical Board reported. We aimed at a quantitative and qualitative analysis of the use of these diagnostic techniques in Swiss hospitals.
METHODS
We contacted nine Swiss hospitals to obtain the number of SPECT/CMR investigations used to diagnose stable CAD in 2014–2016 and submitted a questionnaire to investigate the advantages and limitations of the two imaging techniques. In addition, two experts in SPECT and CMR, respectively, at two university hospitals were interviewed, using open questions.
RESULTS
Data were obtained from 8 hospitals, and 22 questionnaires were returned. In Switzerland, both techniques have been implemented very differently in different hospitals, but the overall number of diagnostic procedures has increased. The questionnaires reported lower scores for CMR regarding the availability of the scans, contraindications and the suitability of the technique for the diagnosis of CAD. The experts described potential conflicts of interest in some institutions, depending on how the cardiology and radiology departments collaborated, and highlighted the debated results of studies comparing CMR with SPECT for the diagnosis of CAD. The main conclusion drawn from the interviews was the recommendation of a patient-centred evaluation.
CONCLUSION
The use of SPECT versus CMR in Switzerland for the diagnosis of stable CAD is heterogeneous, but reflects the guidelines, which do not distinguish between the two diagnostic techniques. Expert opinions underlined that discussion should not be so much about the choice of the diagnostic modality but about how a clinical question in a patient can best be answered.
Introduction
Coronary artery disease (CAD) can be diagnosed using various techniques that help to establish the need for therapy. Direct invasive testing by coronary angiography is effective and recommended in patients with a high pre-test probability, but has high costs, lower diagnostic accuracy and unnecessary risks when used in patients with an intermediate pre-test probability [1]. Therefore, current guidelines recommend noninvasive imaging techniques as gatekeeper strategies to select patients with an intermediate pre-test probability for CAD (between 15 and 85%) who will need invasive diagnostic testing [2].
Other, noninvasive diagnostic tests for stable CAD are available: stress echocardiography, coronary computed tomography (CT) or positron emission tomography (PET), single-photon emission computed tomography (SPECT) and cardiac magnetic resonance imaging (CMR). SPECT currently is the most widely used imaging technique for the diagnosis of stable CAD. However, medical and economic data in favour of CMR are accumulating [3–6]. Guidelines [2] mention CMR at the same level as stress echocardiography, SPECT and PET [7]; studies showing a superiority of CMR for the diagnosis of stable CAD have been criticised [8–11]. In addition to the varying sensitivities and specificities reported in the literature, rapid technological improvement and the complexity of patients’ characteristics do not reveal a clear benefit for one technique over the other. Thus, it is generally accepted that the technique chosen in a specific hospital is mainly dictated by local availability, expertise, and patients’ preference and comorbidities.
According to the Organisation for Economic Cooperation and Development (OECD) report published in 2016, Switzerland belongs to the countries with the most CT and MRI scans per inhabitant [12, 13]. Although these scans are used for diagnostic purposes not only in the domain of cardiology, and despite their high availability, little is known regarding the use of CMR or SPECT for the diagnosis of stable CAD in Switzerland.
Furthermore, the Swiss Medical Board (SMB), a Swiss organisation founded to assess the efficacy, adequacy and cost effectiveness of diagnostic and therapeutic measures, as required for reimbursement by Swiss health insurance providers, recently questioned the value of CMR in comparison with SPECT for the diagnosis of stable CAD [14].
In the light of these uncertainties, we aimed first to evaluate the number of tests and relative use of CMR and SPECT in Swiss hospitals where both techniques are available, and second to investigate the underlying reasons for the preferential use of one or the other technique.
Methods
With the support of SGNM (Schweizerische Gesellschaft für Nuklearmedizin) and through research on hospital-specific websites, the clinic directors of the radiology and cardiology departments of nine main Swiss hospitals were contacted (University Hospitals of Bern, Basel, Lausanne, Geneva and Zurich, the Cantonal Hospitals of Aarau, Lucerne and St Gallen and two centres in Bellinzona-Lugano). The clinic directors were asked about the number of SPECT/CMR examinations conducted to diagnose stable CAD in the years 2014 to 2016. They were also sent a short questionnaire, which they could pass on to their colleagues. An example of this questionnaire is presented in appendix 1.
The questionnaire was designed to take into account the limitations of SPECT and CMR and the presumable impacts they have on the implementation of the two techniques in the clinic. As highlighted in the literature [15, 16], each technique has advantages and disadvantages regarding their suitability for the diagnosis of CAD, their availability and accessibility, the time and effort required for the examination, the contraindications for each technique, their costs, the possibility to have the investigation reimbursed by the insurer and the availability of the corresponding specialists for interpretation of the results.
Each question was asked for CMR and SPECT separately and the possible answers were presented as a five-level Likert-scale (1 being the most negative and 5 the most positive score). The answers to each question were graphically represented and analysed by comparing the median of each question using a Wilcoxon-Mann-Whitney test.
In addition, two experts in SPECT (nuclear medicine specialist) and CMR (cardiologist), respectively, were interviewed at two university hospitals. They were asked open questions about the advantages and disadvantages of both techniques, their availability, the challenges in their everyday implementation, expected future trends of imaging techniques in Switzerland and political or organisational biases that could influence the use of the two diagnostic procedures.
Results
Questionnaires and numbers of procedures were collected over 6 weeks (mid-October 2017 to the end of November 2017). Eight hospitals provided numbers and questionnaires (the total number of questionnaires collected was 22). The precision of the numbers was variable, mainly because the clinic directors did not have direct access to the information or because the data were not recorded in the hospital for some or all of the analysed years. One of the hospitals did not report any numbers (as no statistics were recorded there) and in two further university hospitals, the numbers were only partially available. The numbers of diagnostic procedures are presented in table 1.
Table 1 Number of CMR and SPECT examinations conducted between 2014 and 2016 in the Swiss structures where both technologies are available.
|
Hospital
|
Year
|
CMR
(only for diagnosis of ischaemia)
(number and % of total)
|
SPECT
(number and % of total)
|
| Basel |
2014 |
124 (10.5%) |
1057 (89.5%) |
| 2015 |
152 (9.2%) |
1507 (90.8%) |
| 2016 |
160 (9.8%) |
1470 (90.2%) |
| Lucerne |
2014–2016 |
500† (47.9%) |
544 (52.1%) |
| St Gallen |
2014 |
173 (31.6%) |
374 (68.4%) |
| 2015 |
164 (23.5%) |
533 (76.5%) |
| 2016 |
230 (23.3%) |
758 (76.7%) |
| Lausanne |
2014–2016*
|
1800–2200† (98.5%‡) |
30 (1.5%) |
| Bellinzona/Lugano |
2014 |
91 (8.4%) |
986 (91.6%) |
| 2015 |
111 (10.3%) |
966 (89.7%) |
| 2016 |
106 (10.4%) |
917 (89.6%) |
| Bern |
2014 |
520 (71.2%) |
210 (28.8%) |
| 2015 |
650 (77.4%) |
190 (22.6%) |
| 2016 |
650 (82.3%) |
140 (17.7%) |
| Zurich |
2014 |
NA |
1351 |
| 2015 |
NA |
1424 |
| 2016 |
787 (34.8%) |
1474 (65.2%) |
| Geneva |
2014 |
NA |
NA |
| 2015 |
95 (8.1%) |
1082 (91.9%) |
| 2016 |
155 (10.2%) |
1369 (89.8%) |
| 2017§
|
161 (10.5%) |
1371 (89.5%) |
There was notable heterogeneity across years and hospitals. The hospitals in Lausanne and Bern used CMR to a much larger extent, whereas most of the other hospitals rather used SPECT to diagnose stable CAD. Over the years, there was a tendency to more examinations overall, but the numbers of the each procedure differed depending on the hospital: there was a growing use of CMR in all hospitals, but the number of SPECT examinations both increased (in St Gallen, Geneva, Basel and Zurich) and decreased (in Bellinzona/Lugano and Bern).
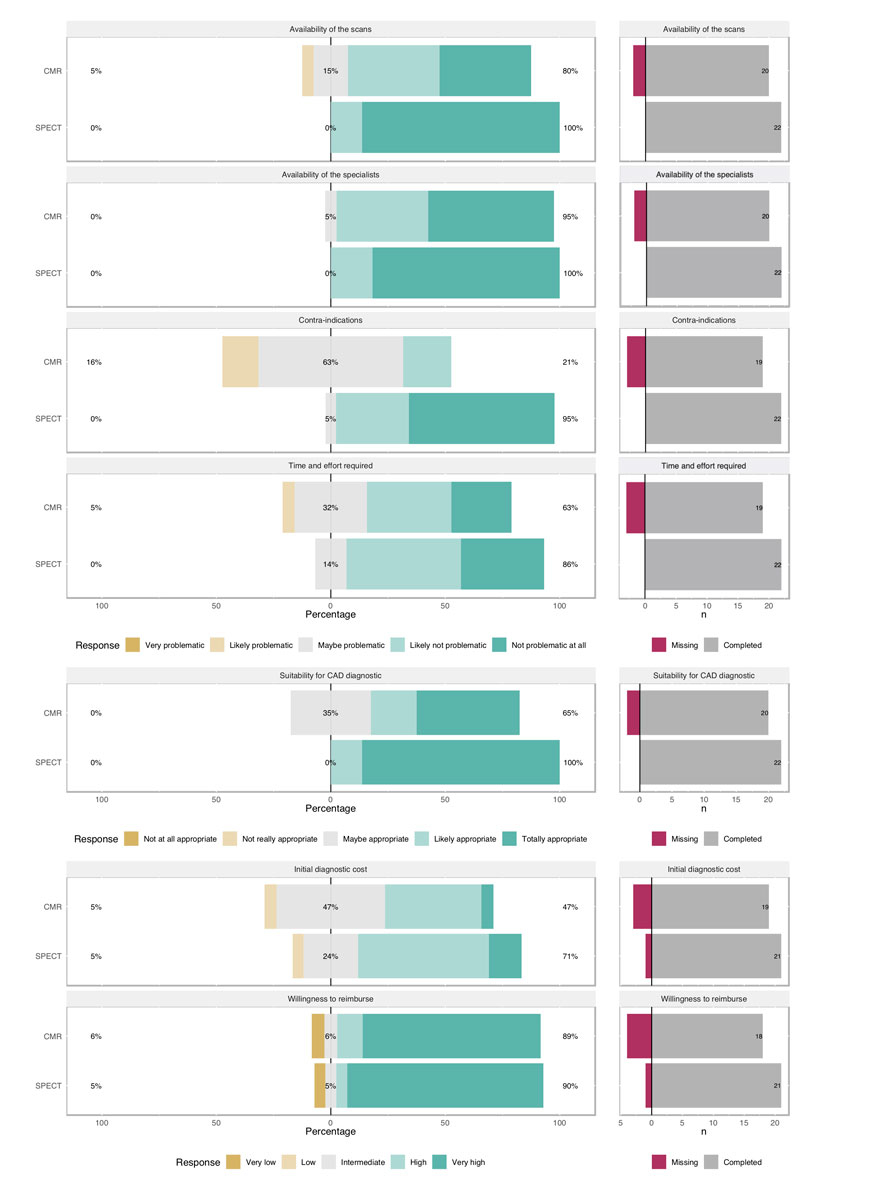
The answers to the questionnaires are presented in figure 1. The median score and the p-value for the comparison between SPECT and CMR for each question are shown in table 2. Of the 22 questionnaires, 4 (18%) were filled in by clinic directors, 3 (14%) by chief physicians, 11 (50%) by attending physicians and 4 (18%) by residents. Nine respondents were cardiologists, 4 radiologists and 14 nuclear medicine specialists (respondents could record more than one speciality). Missing data (a skipped question or part of a question) was allowed for and happened more often with questions regarding CMR than SPECT (mainly because some of the nuclear medicine specialists did not take a position on some of the CMR-related questions).
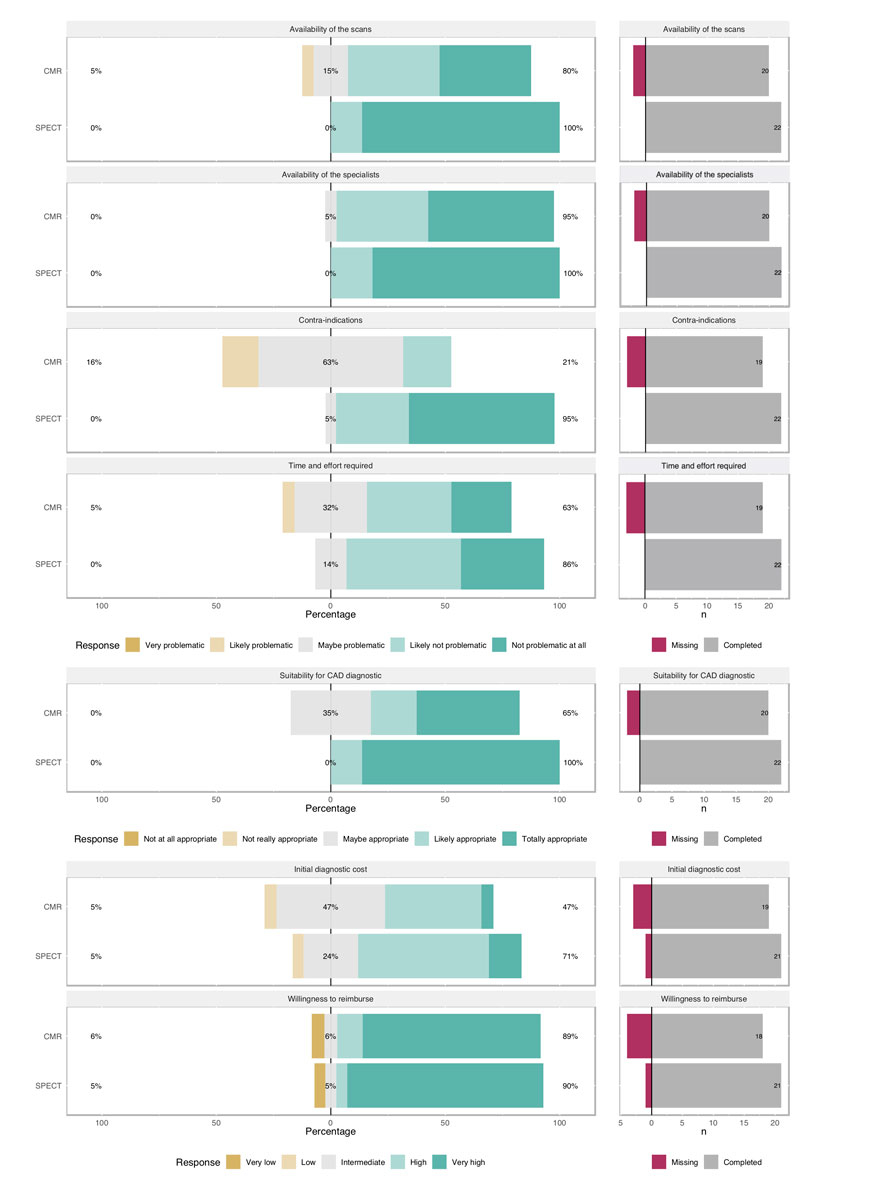
Figure 1 Answers of the 22 physicians to the questionnaire. The percentages of answers given for each level of the Likert scale (from the most negative to the most positive answers) are represented on the left. The numbers of missing answers per question and technology are represented on the right.
Table 2 Median score of each question with interquartile range.
|
Question
|
Technique
|
Median (IQR)
|
p-value of the comparison (Wilcoxon rank sign test)
|
| Availability of the scans |
CMR |
4 (3–4) |
0.01 |
| SPECT |
4 (4–4) |
| Availability of the specialists |
CMR |
4 (3–4) |
0.058 |
| SPECT |
4 (4–4) |
| Contra-indications |
CMR |
2 (2–2( |
<0.001 |
| SPECT |
4 (3–4) |
| Time and effort required |
CMR |
3 (2–3) |
0.17 |
| SPECT |
3 (3–4) |
| Suitability for CAD diagnosis |
CMR |
3 (2–4) |
0.002 |
| SPECT |
4 (4–4) |
| Initial diagnostic cost |
CMR |
2 (2–3) |
0.11 |
| SPECT |
3 (2–3) |
| Willingness of the insurance to reimburse |
CMR |
3 (2–4) |
0.57 |
| SPECT |
3 (2–4) |
The greatest discrepancy in the answers concerned contraindications to the procedures: Physicians perceived CMR to be have more contraindications, hindering its implementation for the diagnosis of stable CAD. The availability of the SPECT scans and the suitability of SPECT for the diagnosis of CAD were considered better than the equivalent for CMR. The other parameters did not show any significant differences.
The interviews with the two experts are available in appendix 1. The experts emphasised that selecting a single imaging technique suitable for diagnosing all patients with an intermediate pre-test probability of CAD is not realistic in Swiss hospitals, where both nuclear medicine and CMR techniques are available. On the basis of the advantages and disadvantages of the techniques, a “patient-centred” evaluation of each case should address patient-specific questions, namely what information is valuable for which patients and which technique will probably deliver the most relevant answers. For the expert in cardiology, SPECT and CMR are not equivalent: CMR is extremely sensitive to previous myocardial infarctions, myocardial diseases and scars, whereas a SPECT or a PET-CT scan was stated by both experts to be the current most accurate technique to diagnose ischaemia. The techniques were perceived as similarly specific for excluding stable CAD. In addition, both experts emphasised that an analysis limited to the comparison of SPECT and CMR, without including other techniques (such as stress echocardiography or PET-CT), would not be representative of the complexity of the current diagnostic process for stable CAD. They would prefer an evaluation of all noninvasive and invasive techniques available.
Discussion
The present study evaluated the current use of two of imaging techniques for the diagnosis of stable CAD (namely SPECT and CMR), physicians’ perceptions of these procedures and the opinion of two experts, and led us to four main conclusions. First, not all Swiss hospitals implement both techniques to the same extent and one of them shows a very strong preference for CMR. In fact, except for this one hospital (Lausanne), the results in table 2 are consistent and show that both techniques are used in daily practice. Second, in the last few years there has been a tendency to more diagnostic procedures, with growing use of CMR. Third, according to our questionnaires, physicians believe that the contraindications associated with CMR are more problematic than those associated with SPECT for the diagnosis of stable CAD, and that SPECT remains a more appropriate and more easily available diagnostic option. Fourth, some topics were repeatedly highlighted as challenging by both experts interviewed, namely inconsistent medical evidence, differences in collaboration or conflicts of interest between hospital departments, local availability of scans and expertise, hospital-specific decision makers and competition with the private sector. The need for a comprehensive evaluation of the diagnostic process, not limited to SPECT or CMR, was highlighted. Especially in private practice, stress testing without imaging or stress echocardiography are widely used even though such a practice is no longer recommended by the relevant guidelines [2].
In line with the diverging evidence supporting or refuting the superiority of CMR over SPECT in the literature [3–6, 8–11], the use of these techniques in Switzerland is heterogeneous. The factors explaining why some hospitals in Switzerland favour one technique over the other include the availability of CMR scans, the suitability of this modality for the diagnosis of stable CAD and its contraindications, as all these factors were revealed as limiting factors when CMR was compared with SPECT in our questionnaire. Moreover, both our experts confirmed local availability and expertise as key players in the implementation of both techniques. Acknowledging the important differentiation between efficacy (how well does the technique perform when implemented in an optimal setting?) and effectiveness (how well does the technique perform when implemented in a real-life setting?), guidelines from the UK National Institute for Health and Care Excellence (NICE) [17] recommend that the technique used should be chosen depending on “local availability, expertise and patients preference.” [17]
However, further factors, such as conflicts of interest between radiologists, nuclear medicine specialists and cardiologists who strongly favour one technique over the other, or personal interpretation of the heterogeneous available literature [3–6, 8–11] could possibly overrule important patient- or expertise-related considerations and therefore negatively impact on the medical and cost effectiveness of the choice of diagnostic technique. As confirmed by the interviews with our experts, clear separation of the nuclear medicine department and the cardiology department in the various hospitals, conflicts of interest and physicians’ preferences seem to play a large role in the choice of technique. Such biases have already been highlighted by Thom et al. [11], who showed that personal beliefs, preferences and domain of professional expertise could influence referral for the diagnosis of stable CAD (with interventional cardiologists referring more patients for coronary angiography as compared with non-interventional cardiologists, despite negative imaging results ). However, these biases must be considered in the context of various departments competing for funding and profit, not only within the same hospital but also with external private institutes, which are spreading in Switzerland.
The cost effectiveness of procedures and the question of scarce resource allocation is of increasing importance in the modern medical world. We observed that a rising number of imaging diagnostic examinations are conducted by the hospitals in Switzerland; this is not limited to cardiology and seems to be justified in the context of an aging population with a growing disease burden, and the high expectations of the Swiss population regarding quality of care. Cost-effectiveness data applicable to Switzerland were highlighted in a study by Pletscher et al., which assessed the comparative costs of both techniques in Switzerland [18], and formally showed a statistically significant cost reduction when using CMR rather than SPECT for the diagnosis of stable CAD. However, the relevance of these data needs to be put into perspective: a previous study comparing direct invasive coronary angiography with SPECT and selective coronary angiography for the diagnosis of table CAD showed a cost reduction of 30 to 40% in intermediate risk patients [19], whereas the study by Pletscher et al. showed a cost reduction of 1.3% per quality-adjusted life-year (QALY) with use of CMR instead of SPECT. Moreover, a change in technique would require enormous investment in hardware, software and competencies for the hospitals, which would in the end outweigh the benefit of a few gained percentages of sensitivity or specificity and the small amount of money spared in the diagnostic process. Therefore, assessing the limitations in the practical use of these techniques, as well as the overall structural adaptations that would be needed for their implementation, will be a central point to ensure effective diagnosis of stable CAD in the future.
The diagnostic process for stable CAD is complex and not restricted to the choice of CMR or SPECT. We limited our analysis to these two techniques, as the SMB mainly questioned their comparative efficacy and effectiveness [14], but wider assessments, including other rapidly evolving and promising techniques, would allow a broader perspective (PET-CT, CT angiography, stress echocardiography).
In conclusion, the use of SPECT versus CMR in Switzerland for the diagnosis of stable CAD depends on physician and hospital preferences, organisational structure, availability, and patients’ comorbidities. The large heterogeneity observed, however, reflects the situation in the guidelines, which leave the choice of diagnostic technique up to the discretion of the treating physicians. The discussion should not be so much about technique, but about how a clinical question in a patient can best be answered.
Limitations
Several limitations need to be considered when interpreting our results. First, owing to the ongoing debate within the SMB about the usefulness of both techniques for the diagnosis of stable CAD, our analysis was focussed on two noninvasive imaging techniques. Therefore, we cannot draw any conclusion on the use of, for instance, stress echocardiography or PET, nor on their possibly important role in the diagnosis of stable CAD. Second, the number of SPECT and CMR examinations could be obtained for only eight hospitals and some data were missing for two of the hospitals. The reason for these missing data was the absence of systematic data collection in the respective hospitals. Also, no information on smaller hospitals and doctors’ offices were used. This limits the conclusion we can draw regarding the increase in CMR over the years in Switzerland. Moreover, 22 physicians answered our questionnaires, which is a relatively small sample. Further studies need to include a much larger number of physicians, record their exact specialisation (nuclear radiologist or cardiologist) and assess in more detail the real reasons underlying the preferential implementation of one or the other diagnostic technique. Finally, we interviewed two experts from two hospitals, whose opinion might not be representative for the cause of the differences in the hospitals studies in the current analysis.
Appendix 1 Questionnaire submitted to the nine Swiss hospitals and interviews with the two experts
The appendix is available as a separate file for downloading at https://smw.ch/en/article/doi/smw.2019.20080/
References
1
Patel
MR
,
Peterson
ED
,
Dai
D
,
Brennan
JM
,
Redberg
RF
,
Anderson
HV
, et al.
Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362(10):886–95. doi:.https://doi.org/10.1056/NEJMoa0907272
2
Montalescot
G
,
Sechtem
U
,
Achenbach
S
,
Andreotti
F
,
Arden
C
,
Budaj
A
, et al., the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. 2013 ESC guidelines on the management of stable coronary artery disease. Eur Heart J. 2013;34(38):2949–3003. doi:.https://doi.org/10.1093/eurheartj/eht296
3
Greenwood
JP
,
Maredia
N
,
Younger
JF
,
Brown
JM
,
Nixon
J
,
Everett
CC
, et al.
Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet. 2012;379(9814):453–60. doi:.https://doi.org/10.1016/S0140-6736(11)61335-4
4
Schwitter
J
,
Wacker
CM
,
van Rossum
AC
,
Lombardi
M
,
Al-Saadi
N
,
Ahlstrom
H
, et al.
MR-IMPACT: comparison of perfusion-cardiac magnetic resonance with single-photon emission computed tomography for the detection of coronary artery disease in a multicentre, multivendor, randomized trial. Eur Heart J. 2008;29(4):480–9. doi:.https://doi.org/10.1093/eurheartj/ehm617
5
Schwitter
J
,
Wacker
CM
,
Wilke
N
,
Al-Saadi
N
,
Sauer
E
,
Huettle
K
, et al.; MR-IMPACT Investigators. MR-IMPACT II: Magnetic Resonance Imaging for Myocardial Perfusion Assessment in Coronary artery disease Trial: perfusion-cardiac magnetic resonance vs. single-photon emission computed tomography for the detection of coronary artery disease: a comparative multicentre, multivendor trial. Eur Heart J. 2013;34(10):775–81. doi:.https://doi.org/10.1093/eurheartj/ehs022
6
Greenwood
JP
,
Herzog
BA
,
Brown
JM
,
Everett
CC
,
Nixon
J
,
Bijsterveld
P
, et al.
Prognostic value of cardiovascular magnetic resonance and single-photon emission computed tomography in suspected coronary heart disease: Long-term follow-up of a prospective, diagnostic accuracy cohort study. Ann Intern Med. 2016;165(1):1–9. doi:.https://doi.org/10.7326/M15-1801
7
von Knobelsdorff-Brenkenhoff
F
,
Schulz-Menger
J
. Role of cardiovascular magnetic resonance in the guidelines of the European Society of Cardiology. J Cardiovasc Magn Reson. 2016;18(1):6. doi:.https://doi.org/10.1186/s12968-016-0225-6
8
Bonow
RO
. What’s past is prologue: advances in cardiovascular imaging. Lancet. 2012;379(9814):393–5. doi:.https://doi.org/10.1016/S0140-6736(11)61671-1
9
Einstein
AJ
. Letter by Einstein regarding article "comparison of cardiovascular magnetic resonance and single-photon emission computed tomography in women with suspected coronary artery disease from the Clinical Evaluation of Magnetic Resonance Imaging in Coronary Heart Disease (CE-MARC) trial". Circulation. 2014;130(24):e339. doi:. https://doi.org/10.1161/CIRCULATIONAHA.114.008737
10
Greenwood
JP
,
Brown
JM
,
Berry
C
; CE-MARC 2 Investigators. Alternatives in the Evaluation of Suspected Coronary Heart Disease-Reply. JAMA. 2017;317(2):212–3. doi:.https://doi.org/10.1001/jama.2016.18335
11
Thom
H
,
West
NEJ
,
Hughes
V
,
Dyer
M
,
Buxton
M
,
Sharples
LD
, et al.; CECaT study group. Cost-effectiveness of initial stress cardiovascular MR, stress SPECT or stress echocardiography as a gate-keeper test, compared with upfront invasive coronary angiography in the investigation and management of patients with stable chest pain: mid-term outcomes from the CECaT randomised controlled trial. BMJ Open. 2014;4(2):e003419. doi:.https://doi.org/10.1136/bmjopen-2013-003419
12OECD. Computed tomography (CT) exams (indicator). 2018. doi:https://doi.org/10.1787/3c994537-en (Accessed on 01 October 2018).
13OCDE. Magnetic resonance imaging (MRI) exams (indicator). 2018. doi:https://doi.org/10.1787/1d89353f-en (Accessed on 01 October 2018).
14SMB. “Swiss Medical Board.” Themenliste Stand Januar 2016. 2016. http://www.medical-board.ch/fileadmin/docs/public/mb/themenumfrage/themenliste_januar_2016.pdf.
15
Dweck
MR
,
Williams
MC
,
Moss
AJ
,
Newby
DE
,
Fayad
ZA
. Computed Tomography and Cardiac Magnetic Resonance in Ischemic Heart Disease. J Am Coll Cardiol. 2016;68(20):2201–16. doi:.https://doi.org/10.1016/j.jacc.2016.08.047
16
Foley
JR
,
Plein
S
,
Greenwood
JP
. Assessment of stable coronary artery disease by cardiovascular magnetic resonance imaging: Current and emerging techniques. World J Cardiol. 2017;9(2):92–108. doi:.https://doi.org/10.4330/wjc.v9.i2.92
17National Institute for Health and Care Excellence (NICE). NICE guideline CG95. Chest pain of recent onset: Assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin (update). 2016;73(March):4–27.
18
Pletscher
M
,
Walker
S
,
Moschetti
K
,
Pinget
C
,
Wasserfallen
JB
,
Greenwood
JP
, et al.
Cost-effectiveness of functional cardiac imaging in the diagnostic work-up of coronary heart disease. Eur Heart J Qual Care Clin Outcomes. 2016;2(3):201–7. doi:.https://doi.org/10.1093/ehjqcco/qcw008
19
Shaw
LJ
,
Hachamovitch
R
,
Berman
DS
,
Marwick
TH
,
Lauer
MS
,
Heller
GV
, et al.; Economics of Noninvasive Diagnosis (END) Multicenter Study Group. The economic consequences of available diagnostic and prognostic strategies for the evaluation of stable angina patients: an observational assessment of the value of precatheterization ischemia. J Am Coll Cardiol. 1999;33(3):661–9. doi:.https://doi.org/10.1016/S0735-1097(98)00606-8