Associations of regrets and coping strategies with job satisfaction and turnover intention: international prospective cohort study of novice healthcare professionals
DOI: https://doi.org/10.4414/smw.2019.20074
Boris
Chevalabc, Stéphane
Cullatiabcd, Denis
Monginab, Ralph E.
Schmidtef, Kim
Lauperg, Jesper
Pihl-Thingvadhi, Pierre
Chopardab, Delphine S.
Courvoisierab
aQuality of Care Service, University Hospitals of Geneva, Switzerland
bDepartment of General Internal Medicine, Rehabilitation and Geriatrics, University of Geneva, Switzerland
cSwiss NCCR “LIVES: Overcoming Vulnerability: Life Course Perspectives”, University of Geneva, Switzerland
dInstitute of Sociological Research, University of Geneva, Switzerland
eDepartment of Psychology, University of Geneva, Switzerland
fDepartment of Psychiatry, Psychotherapy and Psychosomatics, Psychiatric University Hospital, University of Zurich, Switzerland
gDivision of Rheumatology, University Hospitals of Geneva, Switzerland
hDepartment of Occupational and Environmental Medicine, Odense University Hospital, Denmark
iNational Centre of Psychotraumatology, University of Southern Denmark, Denmark
Summary
AIMS OF THE STUDY
(1) To assess the associations of care-related regrets with job satisfaction and turnover intention; and (2) to examine whether these associations are partially mediated by coping strategies.
METHODS
Data came from ICARUS, a prospective international cohort study of novice healthcare professionals working in acute care hospitals and clinics from various countries (e.g., Australia, Austria, Botswana, Canada, Denmark, France, Haiti, Ireland, Kenya, the United Kingdom and United States). Care-related regrets (number of regrets and regret intensity), coping strategies, job satisfaction and turnover intention were assessed weekly for 1 year.
RESULTS
229 young healthcare professionals (2387 observations) were included in the analysis. For a given week, experiencing a larger number of care-related regrets was associated with decreased job satisfaction, and experiencing more intense care-related regrets was associated with increased turnover intention. These associations were partially mediated by coping strategies. Maladaptive emotion-focused strategies were associated with decreased job satisfaction and increased turnover intention, whereas adaptive problem-focused strategies showed the opposite pattern.
CONCLUSIONS
Our results revealed that care-related regrets and maladaptive coping strategies are associated with job dissatisfaction and the intention to quit patient care. Helping healthcare professionals to cope with these emotional experiences seems essential to prevent early job quitting.
Introduction
Physical and psychological health problems are common among healthcare professionals. Almost half of American [1] and European physicians [2], as well as residents [3], are estimated to be affected by burnout. In addition, healthcare professionals are particularly at risk of depression (28.8% among medical doctors) [4], poor job satisfaction [5], long spells of sick leave [6], turnover intention [7] and turnover [8]. For instance, research has revealed that a fifth of newly practicing Swedish nurses strongly intended to leave their profession after 5 years of clinical practice [7] and that a fifth of English physicians intended to quit direct patient care within 5 years [9]. In view of the negative impact on healthcare professionals’ own health [10], quality of patient care [11] and the sustainability of the healthcare system [12], a better understanding of the factors that influence the retention of healthcare professionals is warranted. In this context, low job satisfaction and turnover intention are of particular interest because they are early warning signs of job quitting [13].
Current changes in the healthcare professional work environment, including higher workload, complex decision making under increased time pressure, a growing number of patients with chronic diseases and multi-morbidities, and the proliferation of quality measures and control procedures, probably contribute to job dissatisfaction and job quitting [14]. In addition to these context-related risk factors, healthcare-related emotional burden has recently attracted scientific attention [15]. However, most of the relevant studies have focused on exceptional or common emotional reactions to work demands in general [16, 17], but rarely on emotional demands specifically associated with patient care [18], such as regrets. Regret may be defined as the emotion people feel when they think that the outcome would have been better if they had acted or decided differently [19]. In this study, regrets were operationalised as situations with patients that did not work out as the healthcare professionals hoped. The regretted situations can result from decisions or actions, as well as from an absence of decisions or actions. However, crucially, they do not necessarily involve healthcare errors.
A focus on normal emotions related to patient care is important because they are frequent (regret is the second most frequent everyday emotional state) [20] and in healthcare contexts, an “accumulation” of small negative experiences has been observed [21]. Moreover, most previous studies on emotional states have focused on a single healthcare profession [4], namely physicians or nurses, but rarely on several professions at once [22], thereby preventing between-profession comparisons. Yet such comparisons are required because levels of care-related moral distress may differ between professions [23], as may processes leading to job dissatisfaction and turnover intention. Finally, by having access to a multi-measurement longitudinal design, we were able to examine not only the influence of the overall level of regretted experiences (between-person effects), but also change in these regretted experiences at a specific time compared with a given healthcare professional’s overall level (within-person effects).
The main objective of this study was to assess the associations of care-related regrets with job satisfaction and turnover intention. Regrets can hardly be avoided in clinical practice [24, 25], but their consequences depend on the coping strategies healthcare professionals use [26, 27]. Adaptive coping strategies, such as problem solving, can mitigate the negative impact of stressors and even lead to beneficial consequences, for example learning from mistakes and changing procedures [24, 28]. In contrast, maladaptive coping strategies, such as rumination, typically lead to detrimental consequences for healthcare professionals, patient care and institutional life [25, 27]. Therefore, this study examined whether the associations of regrets with job satisfaction and turnover intention were partially mediated by coping strategies. We expected a partial, and not total, mediation because previous studies revealed that coping strategies did not fully explain the adverse influence of care-related regrets on health-related outcomes [16, 22, 27]. We hypothesised a mediation, rather than a moderation, as previous studies showed that emotional burden may directly impact the healthcare professional’s mind-set and favour maladaptive coping strategies [29].
Materials and methods
The study was approved by the Ethics Committee of the University Hospitals of Geneva, Switzerland
Study design and participants
Data came from the Impact of CAre-related Regret Upon Sleep (ICARUS) cohort study [30]. Briefly, ICARUS is an international cohort study (based in Geneva) using intensive longitudinal data collection (weekly assessments for 1 year) to capture real-time associations between care-related regrets and various health-related and psychological variables. ICARUS included newly practicing healthcare professionals working in acute care hospitals and clinics selected from a random sample of French, English, German, or Danish-speaking countries (e.g., Australia, Austria, Botswana, Canada, Denmark, France, Haiti, Ireland, Kenya, Switzerland, the United Kingdom and the United States of America). To ensure that only newly practicing healthcare professionals (individuals starting treating or caring for patients as professionals) were recruited, students in nursing and medical schools were invited to participate in the study during the end of their last year of training. Participants were assessed directly after their first week as healthcare professionals. This study was approved by all the relevant local Ethics Committees, and all participants signed informed consent forms (see Cheval et al. [30] for more details on the ICARUS protocol). Data were collected from May 2017 to July 2018. Participants of two pilot studies with shorter durations conducted in 2014 and 2016 were also added. These pilot studies included all healthcare professionals (not only newly practicing).
Measures
Outcomes
Healthcare professionals’ satisfaction with work was assessed with the Global Satisfaction with Work (GSWW) scale [31]. The GSWW includes five items (e.g., “I am satisfied with the type of work I do”; “If I could change anything at work, I would change almost nothing”). Each item is rated on a seven-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree) over the preceding week. In our sample, Cronbach’s alpha was 0.67.
Intention to change profession was assessed with the following validated single item [32]: “If it were possible and you would keep a similar salary, would you like to change profession to take up another one or to keep the same profession but without patient care?” Three answers were possible: “No, I do not want to”, “Perhaps”, and “Yes, I do want to”.
Explanatory variables
To ensure that each participant understand the notion of regret in the same way, the questionnaire began with the following definition of regret: “In clinical practice, we sometimes experience situations with patients that do not work as we would have wished. We can blame ourselves, on way or another, whether we are responsible or not. A choice, an action or a mistake, as well as an absence of decision or action, can be source of a regretted situation.”
Number of recent regrets was assessed with a single item: “During the last week, how many patient care situations were there in which you experienced regret?” with an open (numerical) answer.
Regret intensity was assessed with the following single item: “What would you say is the average level of intensity of your feelings of regret about the situations that happened last week?” with 10 ordinal response options ranging from 0 (null) to 10 (very high). If participants reported no regret over the last 7 days, a mean intensity of 0 was imputed.
Coping strategies were assessed with the Care-related Regret Coping Scale for Health-care Professionals (RCS-HCP) [29]. The RCS-HCP evaluates the use of different coping strategies healthcare professionals may employ to deal with care-related regret. The scale contains 15 items divided in 3 subscales: problem-focused strategies (e.g., “I try to find concrete solutions to the situation”), emotion-focused adaptive strategies (e.g., “I try to put the situation in perspective”), and emotion-focused maladaptive strategies (e.g., “I turn these situations over in my mind all the time”). Answers are given on a four-point Likert scale ranging from 1 (never or almost never) to 4 (always or almost always). In our sample, Cronbach’s alphas were 0.76, 0.78, and 0.86 for problem-focused adaptive, emotion-focused adaptive and emotion-focused maladaptive strategies, respectively.
Statistics
Sample size
This analysis focuses on an ancillary outcome with respect to the main study. Thus, the sample size calculation in the protocol was based on job quitting, and indicated that 400 healthcare professionals should be included. Here we provide an ad-hoc sample size calculation for job satisfaction and turnover intention, using G power [33]. The estimates used are based on a medium effect size (d = 0.5) for a continuous outcome, with α = 0.05 and β = 0.8, using 10 covariates. The calculation yields a sample size of n = 118.
Covariates
The following variables were included as covariates: gender, profession (physicians, nurses, other healthcare professions, e.g., midwife, occupational therapists), number of night shifts, and medical errors (whether the event eliciting the most important regret was related to an error or not).
Data analysis
We performed linear mixed-effect models to examine the associations of regrets (number of regrets and regret intensity) with job satisfaction, and logistic mixed-effect models to examine the associations of regrets with turnover intention (yes and perhaps vs no). Next, we examined whether coping strategies partially mediated these associations. Mixed-effect models provide results with acceptable type I error rates if observations are not independent, as in repeated observations within each participant, and avoid excluding participants with missing observations [34]. Furthermore, these models allow the separation of within-person and between-person effects by introducing both the individual mean value over time of a particular variable (e.g., frequency of maladaptive strategies) and the deviation from this mean at each time-point. The coefficient of the mean value estimates between-person influence. For instance, individuals using problem-focused strategies more frequently may have, on average, higher job satisfaction. In contrast, the coefficient of the deviation estimates the within-person influence. For instance, for a particular individual, using more problem-focused strategies in a given week may be associated with higher than usual job satisfaction.
First, for descriptive purposes, we ran univariable models to separately test the association of each care-related regret variable with job satisfaction and turnover intention (for this analysis, the variables were not separated into within-person and between-person effects). Second, the models that separated within from between-person effects were adjusted for covariates: night shifts, perceived medical error, and consequences for the patient were included as time-varying predictors, whereas gender and profession were included as non-time varying predictors. Third, we added coping strategies as potential mediators. Finally, to explore whether associations differed between healthcare professions, we tested models that added interaction terms between the five care-related regret variables (the two regretted experiences and the three coping strategies at both within- and between-person levels) and the type of profession. Statistical analyses were performed using R, and the lme4 and lmerTest packages, with an alpha threshold fixed at 0.05.
Results
Descriptive results
A total of 229 healthcare professionals (88% females; 27% physicians, 48% nurses, 25% other healthcare professions; mean age 30 years, range 19–56) participated, with a median number of observations by participant of five. Most participants skipped some weekly assessments, leading to a median study duration of 39 weeks (table 1). They contributed to 2387 observations. On the first measurement occasion, job satisfaction, turnover intention, care-related experiences, and coping strategies did not differ between professions. The proportion of men was higher among physicians than in the other professions. Over the course of the study, 18.4% of the healthcare professionals did not report any regret experiences. The mean number of regrets per week was close to 2 (Mnumber regret 1.78 ± 1.11; range 0–10) and the mean regret intensity was moderate (Mregret intensity 4.1 ± 2.36; range 1–10). Job satisfaction was moderate (Mjob satisfaction 4.12 ± 1.90; range 1–7), and turnover intention was high (29.4% of the healthcare professionals considered quitting the profession and 16.7% definitely wanted to quit their profession; that is, about 46% were not sure whether they should continue to work as healthcare professionals and treat patients).
Table 1 Descriptive characteristics of the 229 healthcare professionals on the first occasion of measurement.
|
Characteristics
|
Physicians
(n = 61, 27%)
|
Nurses
(n = 111, 48%)
|
Other professions
(n = 57, 25%)
|
p-value*
|
| Follow-up duration in weeks (median, SD) |
36 (18) |
37(17) |
42 (18) |
0.895 |
| Gender |
Male |
20 (67%) |
4 (4%) |
3 (5%) |
<0.001 |
| Female |
41 (33%) |
107 (96%) |
54 (95%) |
| Job satisfaction (1–7) |
4.34 (1.04) |
4.52 (1.14) |
4.34 (1.43) |
0.337 |
| Turnover intention |
No |
42 (69%) |
81 (73%) |
42 (74%) |
0.895 |
| Perhaps |
17 (28%) |
24 (22%) |
13 (23%) |
| Yes |
2 (3%) |
6 (5%) |
2 (3%) |
| Regret |
Yes (at least one) |
37 (61%) |
52 (47%) |
26 (46%) |
0.175 |
| No |
24 (39%) |
59 (53%) |
31 (54%) |
| Number of regrets (past week) |
1.97 (1.32) |
1.56 (0.94) |
1.92 (1.06) |
0.430 |
| Regret intensity (1–10) |
4.20 (1.41) |
4.18 (2.13) |
3.92 (1.79) |
0.266 |
| Coping strategies (1–5) |
Problem-focused |
2.53 (0.65) |
2.41 (0.62) |
2.54 (0.61) |
0.504 |
| Maladaptive |
2.05 (0.66) |
1.97 (0.67) |
1.91 (0.71) |
0.096 |
| Adaptive |
2.74 (0.54) |
2.49 (0.61) |
2.66 (0.54) |
0.298 |
| Night shifts |
Yes (at least one) |
18 (30%) |
25 (23%) |
8 (14%) |
0.130 |
| No |
43 (70%) |
86 (77%) |
49 (86%) |
| Perceived errors |
Yes |
12 (20%) |
17 (15%) |
4 (7%) |
0.137 |
| No |
49 (80%) |
94 (85%) |
53 (93%) |
Job satisfaction
Univariable models
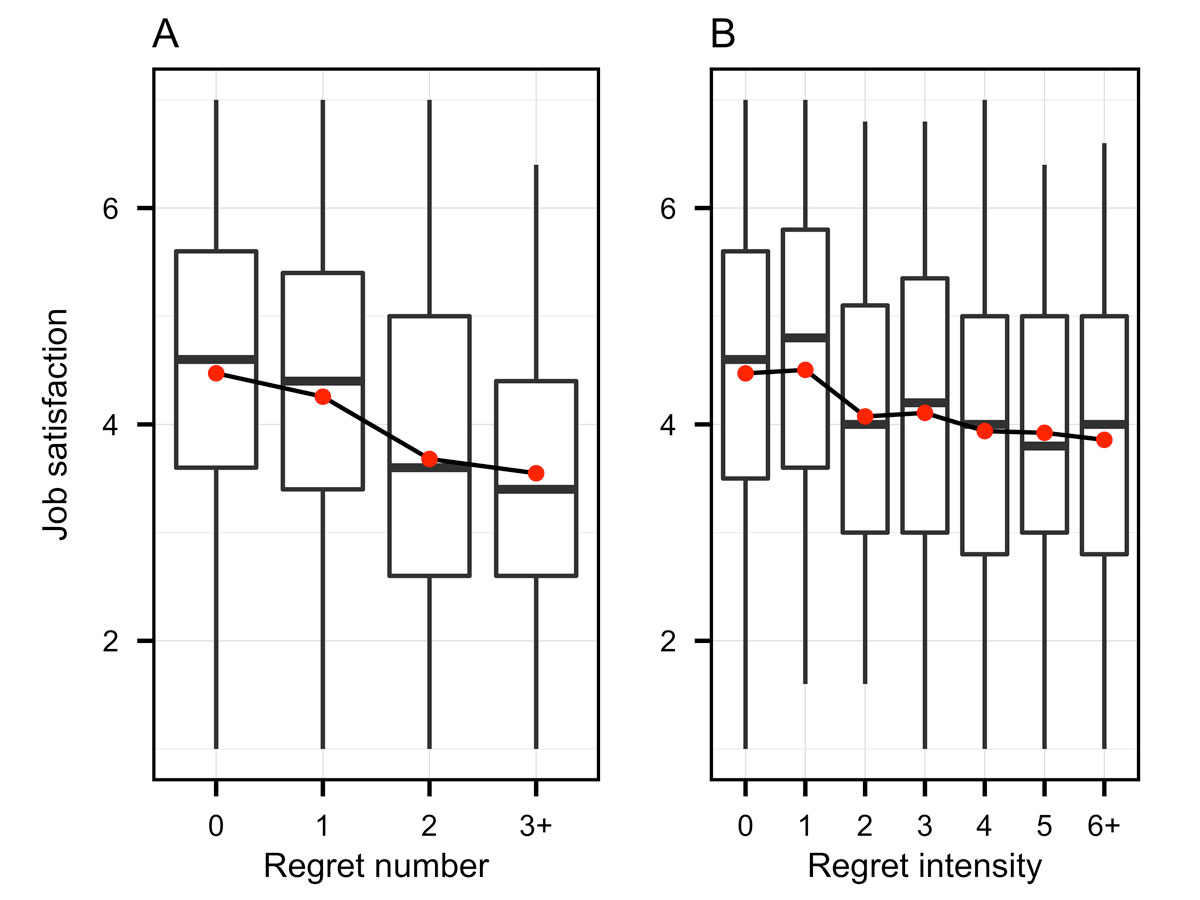
Job satisfaction was significantly associated with number of regrets (p <0.001) and regret intensity (p <0.001) (fig. 1).
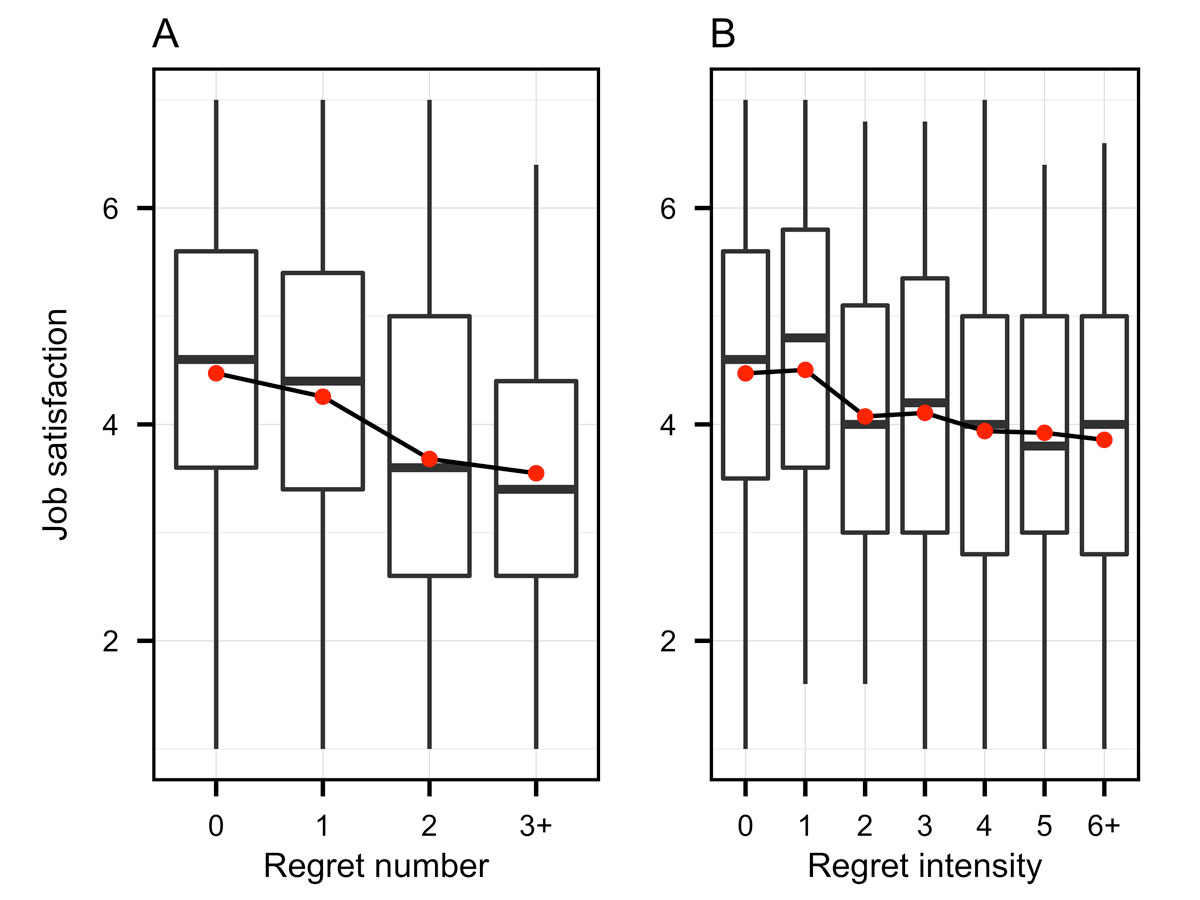
Figure 1 Descriptive results showing the association between regret intensity (A) and number of regrets (B) and job satisfaction (on a 7-point Likert scale ranging from 1 to 7 with higher levels indicating higher job satisfaction). Note: mean levels of job satisfaction as a function of regret intensity (A) and number of regrets (B) are shown in red. Boxplots of observed data are shown in grey.
Adjusted models
Within-person effects
An increase in the number of regrets was associated with lower job satisfaction (b = −0.09, p <0.001), whereas change in regret intensity was not (p = 0.241). That is, for a given healthcare professional, having one more regret than the mean number of regrets usually experienced was associated with a 0.09-point decrease in job satisfaction (range of job satisfaction 1–7). The association between within-person change in number of regrets and job satisfaction remained unchanged after adjusting for coping strategies (b = −0.09, p <0.001). A more frequent use of problem-focused strategies was associated with higher job satisfaction (b = 0.19, p <0.001). Conversely, more frequent use of emotion-focused maladaptive strategies was associated with lower job satisfaction (b = −0.23, p <0.001) (table 2). These associations did not significantly differ between healthcare professions, except for the adverse effect of emotion-focused maladaptive strategies, which was more pronounced in physicians than in nurses (p for interaction = 0.013).
Table 2 Linear mixed models testing the association of within- and between-person variability in care-related regrets as predictors of job satisfaction and the mediation of coping strategies.
Outcome: job satisfaction
Fixed effects
|
Without coping strategies
|
With coping strategies
|
|
b (95% CI)
|
p-value
|
b (95% CI)
|
p-value
|
|
Within-person effects
|
| Weekly regret experiences |
Regret intensity |
−0.01 (−0.03;0.01) |
0.241 |
−0.01 (−0.03;0.05) |
0.632 |
| Number of regrets |
−0.09 (−0.14;−0.04) |
<0.001 |
−0.09 (−0.16;−0.01) |
<0.001 |
| Weekly regret coping strategies |
Problem-focused |
|
|
0.19 (0.08;0.45) |
<0.001 |
| Emotion-focused adaptive |
|
|
0.08 (−0.21;0.154 |
0.124 |
| Emotion-focused maladaptive |
|
|
−0.23 (−0.31;−0.02) |
<0.001 |
|
Between-person effects
|
| Regret experiences |
Regret intensity |
−0.02 (−0.14;0.10) |
0.765 |
−0.01 (−0.18;0.11) |
0.875 |
| Number of regrets |
−0.41 (−0.68;−0.14) |
0.003 |
−0.37 (−0.65;0.06) |
0.007 |
| Regret coping strategies |
Problem-focused |
|
|
0.36 (0.09;0.79) |
0.012 |
| Emotion-focused adaptive |
|
|
0.04 (−0.47;0.24) |
0.802 |
| Emotion-focused maladaptive |
|
|
−0.30 (−0.46;0.17) |
0.028 |
|
Covariates
|
| Not time varying |
Gender (ref. male) |
0.04 (−0.46;0.56) |
0.860 |
0.09 (−0.52;0.65) |
0.700 |
|
Profession:
|
|
| Nurses |
Ref. |
|
Ref. |
|
| Physicians |
−0.21 (−0.60;0.18) |
0.293 |
−0.23 (−0.76;0.19) |
0.256 |
| Other professions |
−0.06 (−0.44;0.32) |
0.746 |
−0.12 (−0.49;0.41) |
0.524 |
| Time varying |
Week |
−0.01 (−0.02;−0.01) |
0.018 |
−0.01 (−0.03;−0.01) |
0.012 |
| Night shifts (ref. no) |
−0.08 (−0.17;0.01) |
0.069 |
−0.08 (−0.14;0.19) |
0.058 |
| Perceived medical error (ref. no) |
0.11 (−0.01;0.23) |
0.071 |
0.10 (−0.20;0.18) |
0.083 |
Between-person effects
Consistent with within-person effects, healthcare professionals’ average number of regrets was associated with job satisfaction (b = -0.41, p = 0.003), whereas average regret intensity was not (p = 0.765). Put differently, healthcare professionals who reported on average one regret fewer than their colleagues showed a 0.41-point increase in job satisfaction. This association was slightly attenuated, but remained significant, after adjusting for coping strategies (b = −0.37, p = 0.007). Healthcare professionals’ average use of problem-focused strategies was associated with higher job satisfaction (b = 0.36, p = 0.012), whereas emotion-focused maladaptive strategies were associated with lower job satisfaction (b = −0.30, p = 0.028). These associations did not significantly differ between healthcare professions.
Turnover intention (yes or perhaps vs no)
Univariable models
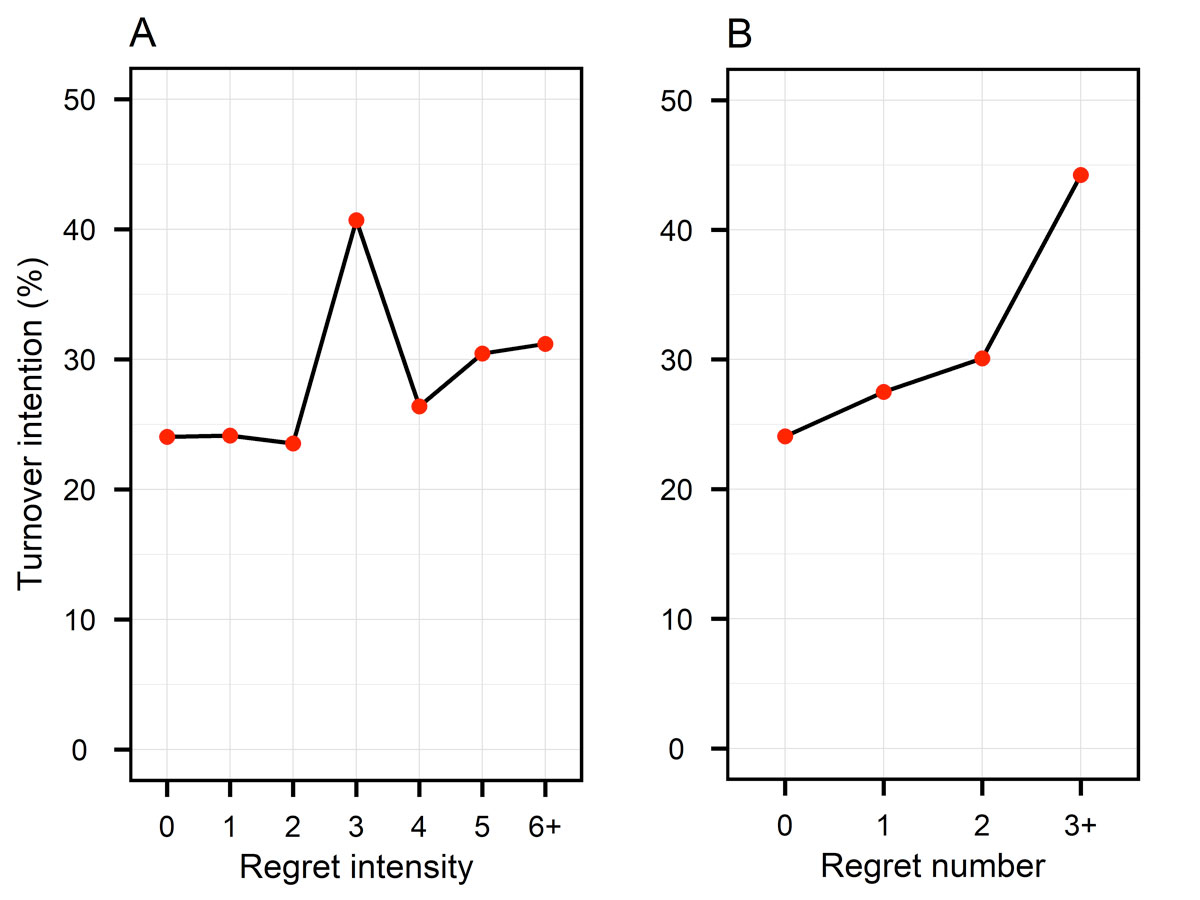
Results revealed significant univariate associations of turnover intention with number of regrets (p <0.001) and regret intensity (p <0.001) (fig. 2).
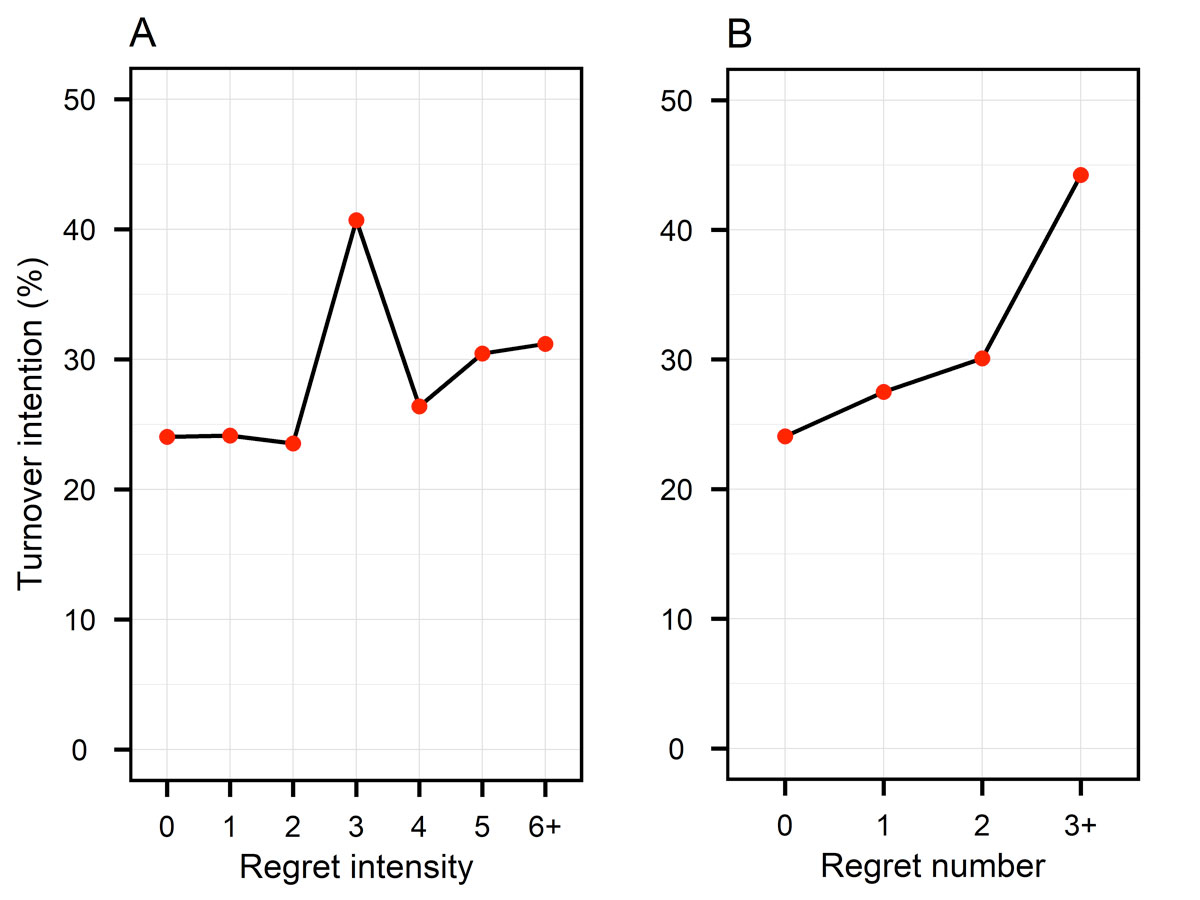
Figure 2 Descriptive results showing the association between regret intensity (A) and number of regrets (B) and intention turnover. Note: percentages of turnover intention as a function of regret intensity (A) and number of regrets (B) are shown in red.
Adjusted models
Within-person effects
An increase in regret intensity was associated with a higher risk of turnover intention (odds ratio [OR] 1.13, p = 0.049), whereas change in number of regrets was not (p = 0.163). That is, for a particular healthcare professional, an increase of regret intensity by one unit multiplied the odds of turnover intention by 1.13. The association was attenuated and became nonsignificant after adjusting for coping strategies (OR 1.08, p = 0.278). A more frequent use of emotion-focused maladaptive strategies was associated with a higher risk of turnover intention (OR 2.16, p = 0.006), whereas this was not the case for the two other types of coping strategies (p >0.155) (table 3). These associations did not significantly differ between healthcare professions.
Table 3 Linear mixed models testing the association of within- and between-person variability in care-related regrets as predictors of job satisfaction and the mediation of coping strategies.
Outcome: turnover intention
Fixed effects
|
Without coping strategies
|
With coping strategies
|
|
Odds ratio (95% CI)
|
p-value
|
Odds ratio (95% CI)
|
p-value
|
|
Within-person effects
|
| Weekly regret experiences |
Regret intensity |
1.13 (1.01;1.29) |
0.049 |
1.08 (0.94;1.23) |
0.278 |
| Number of regrets |
1.22 (0.92;1.62) |
0.163 |
1.20 (0.90;1.59) |
0.209 |
| Weekly regret coping strategies |
Problem-focused |
|
|
0.63 (0.32;1.23) |
0.173 |
| Emotion-focused adaptive |
|
|
0.60 (0.30;1.21) |
0.155 |
| Emotion-focused maladaptive |
|
|
2.16 (1.25;3.74) |
0.006 |
|
Between-person effects
|
| Regret experiences |
Regret intensity |
0.78 (0.24;2.56) |
0.688 |
0.82 (0.36;1.87) |
0.642 |
| Number of regrets |
6.09 (0.56;66.19) |
0.138 |
4.11 (0.76;22.15) |
0.100 |
| Regret coping strategies |
Problem-focused |
|
|
0.05 (0.006;0.42) |
0.006 |
| Emotion-focused adaptive |
|
|
1.95 (0.22;17.16) |
0.546 |
| Emotion-focused maladaptive |
|
|
8.66 (1.19;63.06) |
0.033 |
|
Covariates
|
| Not time varying |
Gender (ref. male) |
0.26 (0.002;40.31) |
0.599 |
0.06 (0.001;1.89) |
0.109 |
|
Profession:
|
|
| Nurses |
Ref. |
|
Ref. |
|
| Physicians |
0.60 (0.02;6.90) |
0.802 |
0.70 (0.04;11.54) |
0.802 |
| Other professions |
0.29 (0.001;32.38) |
0.612 |
0.31 (0.013;7.49) |
0.475 |
| Time varying |
Week |
0.85 (0.69;1.03) |
0.053 |
0.88 (0.76;1.03) |
0.117 |
| Night shifts (ref. no) |
1.46 (0.76;2.82) |
0.260 |
1.35 (0.71;2.55) |
0.359 |
| Perceived medical error (re. no) |
0.76 (0.35;1.62) |
0.472 |
0.82 (0.39;1.75) |
0.615 |
Between-person effects
There was no significant association between the average number of regrets and turnover intention. However, consistent with within-person effects, healthcare professionals’ average use of emotion-focused maladaptive strategies was associated with much higher turnover intention (OR 8.66, p = 0.033). In contrast, problem-focused strategies were associated with lower turnover intention (OR 0.05, p = 0.006). These associations did not significantly differ between healthcare professions.
Discussion
Main findings
In this international cohort study of novice healthcare professionals working in acute care hospitals and clinics, emotional burden was found to predict job dissatisfaction and turnover intention. At the within-subject level (individual variations over time), we found that experiencing more regrets than usual in a given week was associated with decreased job satisfaction. Furthermore, experiencing higher than usual regret intensity was associated with increased turnover intention. In other words, when healthcare professionals experience an increase in their routine levels of care-related regrets (more regrets than usual, higher regret intensity than usual), this change is likely to influence their retention in the hospitals’ workforce. Previous qualitative studies showed that healthcare-related regrets refer to a wide range of clinical situations including diagnosis, treatment, outcome evaluation, patient management and inter-personal relations between the patient and the healthcare professional. These qualitative studies also revealed that regret intensity is on average not higher when a medical error was involved [24, 35]. At the between-subject level, results showed that healthcare professionals who experienced more regrets had a decreased job satisfaction. These associations were slightly attenuated after adjusting for coping strategies. Maladaptive emotion-focused strategies had a strong and consistent detrimental impact on job satisfaction and turnover intention, whereas problem-focused strategies had, to a lesser extent, a positive influence on these outcomes.
Overall, our findings suggest that the emotional burden of common care-related regrets, in terms of both intensity and number, was associated with job satisfaction and turnover intention. Individual coping strategies were partially useful to reduce the impact of the emotional burden. These findings may suggest that other strategies, perhaps at the team or institutional levels, are needed, for instance a change in safety culture [36].
Comparison with other studies
Healthcare professionals had high levels of turnover intention, which could result from their moderate level of job satisfaction. Approximately half the healthcare professionals were thinking about quitting their profession. These figures are especially high given that the sample was comprised of novice healthcare professionals. Our findings are consistent with previous studies suggesting that healthcare professionals are particularly at risk of turnover intention [9] and actual turnover [8]. A possible interpretation is that confrontation with the reality of the clinical work may very quickly make healthcare professionals doubt whether they are on the right professional track. Additionally, the general requirement of adaption due to a new work environment, including many specific demands, new clinical practices and “socialisation pressure,” can have a negative emotional impact that threatens job retention not only in newly practicing but also in experienced healthcare professionals [37].
Results revealed that a higher number or regrets (when compared with colleagues or to one’s average number of regrets) was associated with job dissatisfaction, whereas more intense regrets (when compared to one’s average intensity level) were associated with increased turnover intention. These findings are consistent with previous studies examining the association of emotional burden with job dissatisfaction and turnover intention [38–40], two key variables underlying early job quitting. However, to the best of our knowledge, our study was the first to assess these associations with a specific focus on the common experience of regrets rather than exceptional emotional states [41]. A potential explanation for the differential effects of regret number and regret intensity is that healthcare professionals may consider regret experiences as an inevitable part of their job. An accumulation of small regrets may therefore produce a certain level of discomfort and decrease job satisfaction [24], but is unlikely to represent an overwhelming experience that calls the whole career into question. In contrast, intensely regretted experiences may be perceived as too difficult to cope with, exceeding what individuals are willing to endure during their clinical practice. These hard-to-bear experiences may raise doubts in healthcare professionals’ minds regarding their intention to pursue their career.
The associations of care-related regret experiences with job satisfaction and turnover intention were only slightly attenuated after adjusting for coping strategies. These findings are consistent with previous studies revealing that coping strategies partially explained how emotional experiences, including regrets, influence health-related outcomes [16, 22, 27]. Coping strategies were also associated with job satisfaction and turnover intention, independently of regret intensity and frequency. Problem-focused strategies were associated with higher job satisfaction and lower turnover intention. Conversely, maladaptive emotion-focused coping strategies were associated with lower job satisfaction and higher turnover intention. For both outcomes, our findings revealed –at both the intra- and inter-individual levels – the key role that coping strategies play. Specifically, maladaptive emotion-focused strategies produce adverse effects not only on healthcare professionals’ perception of their job satisfaction but also on their willingness to pursue their career. In sum, our results suggest that the ability to manage the build-up of emotional strain associated with providing healthcare may represent an important factor for the retention of healthcare professionals.
The comparisons between healthcare professions revealed only one significant difference: The adverse effect of emotion-focused maladaptive strategies was more pronounced in physicians than nurses. Taken together, our findings might suggest that the mechanisms underlying job quitting could be similar across different healthcare professions. However, further research involving larger samples is clearly needed to explore potential differences between healthcare professions.
Strengths and weaknesses of the study
Strengths of this study include the comprehensive sample and the longitudinal design. The use of a multicentre sample from various countries provided more generalisable results. The selection of novice healthcare professionals allowed us to study all professionals instead of only those who remain in the profession after a few years, thus limiting survivor bias. The inclusion of different healthcare professions allowed us to investigate profession-specific problems and processes within the same general context. The intensive longitudinal data collection (once per week during 1 year) allowed us to assess real-time associations of regrets with job satisfaction and turnover intention. A longer measurement interval could have missed the complex interplay between work-related emotions and healthcare professionals’ attitudes toward their job. Another strength of this study was that it focused on a normal and common emotion specifically associated with patient care, that is, regret, instead of focusing on abnormal and less common emotional states, such as burnout, or to emotional demands to work in general [16, 17]. This focus allowed us to draw conclusions that apply to a large proportion of healthcare professionals. Finally, the use of advanced statistical models allowed us to disentangle inter-individual differences in emotional burden and coping strategies from intra-individual differences over time.
However, several limitations should also be mentioned. First, although measures were gathered once per week, they were nevertheless retrospective and, thus, subject to recall bias. Second, our study included a limited number of participants (229). This limitation was partially compensated by the high number of measurements for each participant (up to 52, yielding a total of 2387 observations), which increased statistical power. Third, selection bias due to attrition cannot be excluded. However, the statistical procedure allowed us to include participants who had at least one measurement, that is, we could take all healthcare professionals into account instead of only those with full participation. Furthermore, given that this study focused on change within individuals, the selection bias is unlikely to explain the pattern of results we obtained. Fourth, the reliability of GSWW scale was relatively low (Cronbach’s alpha was 0.67), probably due to a more homogeneous population (only novice healthcare professionals instead of professionals with different levels of experience). Low reliability decreases the ability to detect significant associations and, as such, nonsignificant associations should be interpreted with caution. Fifth, this study did not include the individuals’ characteristics, such as personality traits, which may influence both the emergence of regrets and how healthcare professional deal with these regretted experiences. Thus, causal interpretation may not be correct. Future research should take into account how individuals’ characteristics may independently influence or interact with regretted experiences to predict job-related outcomes.
Conclusions and implications
Accumulation of care-related regrets was mainly associated with lower job satisfaction, whereas regret intensity was associated with turnover intention. Coping strategies played a role in reducing (problem-focused strategies) or strengthening (maladaptive strategies) these associations. Efforts to increase job satisfaction and to prevent job turnover should consider the emotional burden of providing healthcare, especially the accumulation of regrets, and the strategies used to cope with these normal and common emotional experiences.
Acknowledgments
We would like to thank all the healthcare professionals for their contributions.
Author contributions
Study design: BC, SC, DSC. Data collection: BC, DSC. Data analysis: BC, DM, DSC. Draft preparation: BC, SC, DSC. Figures preparation: BC, DSC, DM. Manuscript edition: BC, SC, DM, RES, KL, JP, PC, DSC.
References
1
Shanafelt
TD
,
Boone
S
,
Tan
L
,
Dyrbye
LN
,
Sotile
W
,
Satele
D
, et al.
Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–85. doi:.https://doi.org/10.1001/archinternmed.2012.3199
2
Arigoni
F
,
Bovier
PA
,
Sappino
AP
. Trend of burnout among Swiss doctors. Swiss Med Wkly. 2010;140:w13070. doi:.https://doi.org/10.4414/smw.2010.13070
3
Dyrbye
L
,
Shanafelt
T
. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50(1):132–49. doi:.https://doi.org/10.1111/medu.12927
4
Mata
DA
,
Ramos
MA
,
Bansal
N
,
Khan
R
,
Guille
C
,
Di Angelantonio
E
, et al.
Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 2015;314(22):2373–83. doi:.https://doi.org/10.1001/jama.2015.15845
5
Domagała
A
,
Bała
MM
,
Peña-Sánchez
JN
,
Storman
D
,
Świerz
MJ
,
Kaczmarczyk
M
, et al.
Satisfaction of physicians working in hospitals within the European Union: state of the evidence based on systematic review. Eur J Public Health. 2019;29(2):232–41. doi:.https://doi.org/10.1093/eurpub/cky117
6
Dewa
CS
,
Loong
D
,
Bonato
S
,
Thanh
NX
,
Jacobs
P
. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res. 2014;14(1):325. doi:.https://doi.org/10.1186/1472-6963-14-325
7
Rudman
A
,
Gustavsson
P
,
Hultell
D
. A prospective study of nurses’ intentions to leave the profession during their first five years of practice in Sweden. Int J Nurs Stud. 2014;51(4):612–24. doi:.https://doi.org/10.1016/j.ijnurstu.2013.09.012
8
Hayes
LJ
,
O’Brien-Pallas
L
,
Duffield
C
,
Shamian
J
,
Buchan
J
,
Hughes
F
, et al.
Nurse turnover: a literature review - an update. Int J Nurs Stud. 2012;49(7):887–905. doi:.https://doi.org/10.1016/j.ijnurstu.2011.10.001
9
Sibbald
B
,
Bojke
C
,
Gravelle
H
. National survey of job satisfaction and retirement intentions among general practitioners in England. BMJ. 2003;326(7379):22. doi:.https://doi.org/10.1136/bmj.326.7379.22
10
Dyrbye
LN
,
Thomas
MR
,
Massie
FS
,
Power
DV
,
Eacker
A
,
Harper
W
, et al.
Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334–41. doi:.https://doi.org/10.7326/0003-4819-149-5-200809020-00008
11
Panagioti
M
,
Geraghty
K
,
Johnson
J
,
Zhou
A
,
Panagopoulou
E
,
Chew-Graham
C
, et al.
Association between physician burnout and patient safety, professionalism, and patient satisfaction: A systematic review and meta-analysis. JAMA Intern Med. 2018;178(10):1317–30. doi:.https://doi.org/10.1001/jamainternmed.2018.3713
12
Dyrbye
LN
,
Shanafelt
TD
. Physician burnout: a potential threat to successful health care reform. JAMA. 2011;305(19):2009–10. doi:.https://doi.org/10.1001/jama.2011.652
13
Hann
M
,
Reeves
D
,
Sibbald
B
. Relationships between job satisfaction, intentions to leave family practice and actually leaving among family physicians in England. Eur J Public Health. 2011;21(4):499–503. doi:.https://doi.org/10.1093/eurpub/ckq005
14
Nei
D
,
Snyder
LA
,
Litwiller
BJ
. Promoting retention of nurses: A meta-analytic examination of causes of nurse turnover. Health Care Manage Rev. 2015;40(3):237–53. doi:.https://doi.org/10.1097/HMR.0000000000000025
15
Oh
Y
,
Gastmans
C
. Moral distress experienced by nurses: a quantitative literature review. Nurs Ethics. 2015;22(1):15–31. doi:.https://doi.org/10.1177/0969733013502803
16
Sirriyeh
R
,
Lawton
R
,
Gardner
P
,
Armitage
G
. Coping with medical error: a systematic review of papers to assess the effects of involvement in medical errors on healthcare professionals’ psychological well-being. Qual Saf Health Care. 2010;19(6):e43. doi:.https://doi.org/10.1136/qshc.2009.035253
17
Borritz
M
,
Bültmann
U
,
Rugulies
R
,
Christensen
KB
,
Villadsen
E
,
Kristensen
TS
. Psychosocial work characteristics as predictors for burnout: findings from 3-year follow up of the PUMA Study. J Occup Environ Med. 2005;47(10):1015–25. doi:.https://doi.org/10.1097/01.jom.0000175155.50789.98
18
Jakimowicz
S
,
Perry
L
,
Lewis
J
. An integrative review of supports, facilitators and barriers to patient-centred nursing in the intensive care unit. J Clin Nurs. 2017;26(23-24):4153–71. doi:.https://doi.org/10.1111/jocn.13957
19
Zeelenberg
M
,
Pieters
R
. A theory of regret regulation 1.0. J Consum Psychol. 2007;17(1):3–18. doi:.https://doi.org/10.1207/s15327663jcp1701_3
20Frijda NH. Varieties of affect: Emotions and episodes, moods, and sentiments; in Ekman P, Davidson R (eds): The nature emotion: Fundamental questions. Oxford: Oxford University Press; 1994 pp 59–67.
21
Epstein
EG
,
Hamric
AB
. Moral distress, moral residue, and the crescendo effect. J Clin Ethics. 2009;20(4):330–42.
22
Cheval
B
,
Mongin
D
,
Cullati
S
,
Winz
C
,
von Arx
M
,
Schmidt
RE
, et al.
Reciprocal relations between care-related emotional burden and sleep problems in healthcare professionals: a multicentre international cohort study. Occup Environ Med. 2018;75(9):647–53. doi:.https://doi.org/10.1136/oemed-2018-105096
23
Whitehead
PB
,
Herbertson
RK
,
Hamric
AB
,
Epstein
EG
,
Fisher
JM
. Moral distress among healthcare professionals: report of an institution-wide survey. J Nurs Scholarsh. 2015;47(2):117–25. doi:.https://doi.org/10.1111/jnu.12115
24
Courvoisier
DS
,
Agoritsas
T
,
Perneger
TV
,
Schmidt
RE
,
Cullati
S
. Regrets associated with providing healthcare: qualitative study of experiences of hospital-based physicians and nurses. PLoS One. 2011;6(8):e23138. doi:.https://doi.org/10.1371/journal.pone.0023138
25
Courvoisier
D
,
Merglen
A
,
Agoritsas
T
. Experiencing regrets in clinical practice. Lancet. 2013;382(9904):1553–4. doi:.https://doi.org/10.1016/S0140-6736(13)62325-9
26
Carver
CS
,
Connor-Smith
J
. Personality and coping. Annu Rev Psychol. 2010;61(1):679–704. doi:.https://doi.org/10.1146/annurev.psych.093008.100352
27
Cullati
S
,
Cheval
B
,
Schmidt
RE
,
Agoritsas
T
,
Chopard
P
,
Courvoisier
DS
. Self-rated health and sick leave among nurses and physicians: the role of regret and coping strategies in difficult care-related situations. Front Psychol. 2017;8:623. doi:.https://doi.org/10.3389/fpsyg.2017.00623
28
Marchiori
D
,
Warglien
M
. Predicting human interactive learning by regret-driven neural networks. Science. 2008;319(5866):1111–3. doi:.https://doi.org/10.1126/science.1151185
29
Courvoisier
DS
,
Cullati
S
,
Ouchi
R
,
Schmidt
RE
,
Haller
G
,
Chopard
P
, et al.
Validation of a 15-item care-related regret coping scale for health-care professionals (RCS-HCP). J Occup Health. 2014;56(6):430–43. doi:.https://doi.org/10.1539/joh.14-0060-OA
30
Cheval
B
,
Cullati
S
,
Pihl-Thingvad
J
,
Mongin
D
,
Von Arx
M
,
Chopard
P
, et al.
Impact of CAre-related Regret Upon Sleep (ICARUS) cohort study: protocol of a 3-year multicentre, international, prospective cohort study of novice healthcare professionals. BMJ Open. 2018;8(3):e022172. doi:.https://doi.org/10.1136/bmjopen-2018-022172
31
Blais
MR
,
Brière
NM
,
Riddle
AS
,
Vallerand
RJ
. L’inventaire des motivations au travail de Blais. Rev Que Psychol. 1993;14:185–215.
32
Heponiemi
T
,
Kouvonen
A
,
Vänskä
J
,
Halila
H
,
Sinervo
T
,
Kivimäki
M
, et al.
The association of distress and sleeping problems with physicians’ intentions to change profession: the moderating effect of job control. J Occup Health Psychol. 2009;14(4):365–73. doi:.https://doi.org/10.1037/a0015853
33
Faul
F
,
Erdfelder
E
,
Lang
A-G
,
Buchner
A
. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91. doi:.https://doi.org/10.3758/BF03193146
34
Boisgontier
MP
,
Cheval
B
. The anova to mixed model transition. Neurosci Biobehav Rev. 2016;68:1004–5. doi:.https://doi.org/10.1016/j.neubiorev.2016.05.034
35
von Arx
M
,
Cullati
S
,
Schmidt
RE
,
Richner
S
,
Kraehenmann
R
,
Cheval
B
, et al.
“We Won’t Retire Without Skeletons in the Closet”: Healthcare-Related Regrets Among Physicians and Nurses in German-Speaking Swiss Hospitals. Qual Health Res. 2018;28(11):1746–58. doi:.https://doi.org/10.1177/1049732318782434
36Donaldson MS, Corrigan JM, Kohn LT. To err is human: building a safer health system. Washington DC: National Academies Press; 2000.
37
Kinghorn
GR
,
Halcomb
EJ
,
Froggatt
T
,
Thomas
SD
. Transitioning into new clinical areas of practice: An integrative review of the literature. J Clin Nurs. 2017;26(23-24):4223–33. doi:.https://doi.org/10.1111/jocn.14008
38
Gan
Y
,
Gong
Y
,
Chen
Y
,
Cao
S
,
Li
L
,
Zhou
Y
, et al.
Turnover intention and related factors among general practitioners in Hubei, China: a cross-sectional study. BMC Fam Pract. 2018;19(1):74. doi:.https://doi.org/10.1186/s12875-018-0752-3
39
Aggarwal-Gupta
M
,
Vatharkar
P
. Impact of stress and work-family conflict on the mental well-being of physicians: mediation by job and career satisfaction. Br J Health Care Manage. 2017;23(9):409–16. doi:.https://doi.org/10.12968/bjhc.2017.23.9.409
40
Josephson
M
,
Lindberg
P
,
Voss
M
,
Alfredsson
L
,
Vingård
E
. The same factors influence job turnover and long spells of sick leave--a 3-year follow-up of Swedish nurses. Eur J Public Health. 2008;18(4):380–5. doi:.https://doi.org/10.1093/eurpub/ckn009
41
Waterman
AD
,
Garbutt
J
,
Hazel
E
,
Dunagan
WC
,
Levinson
W
,
Fraser
VJ
, et al.
The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33(8):467–76. doi:.https://doi.org/10.1016/S1553-7250(07)33050-X