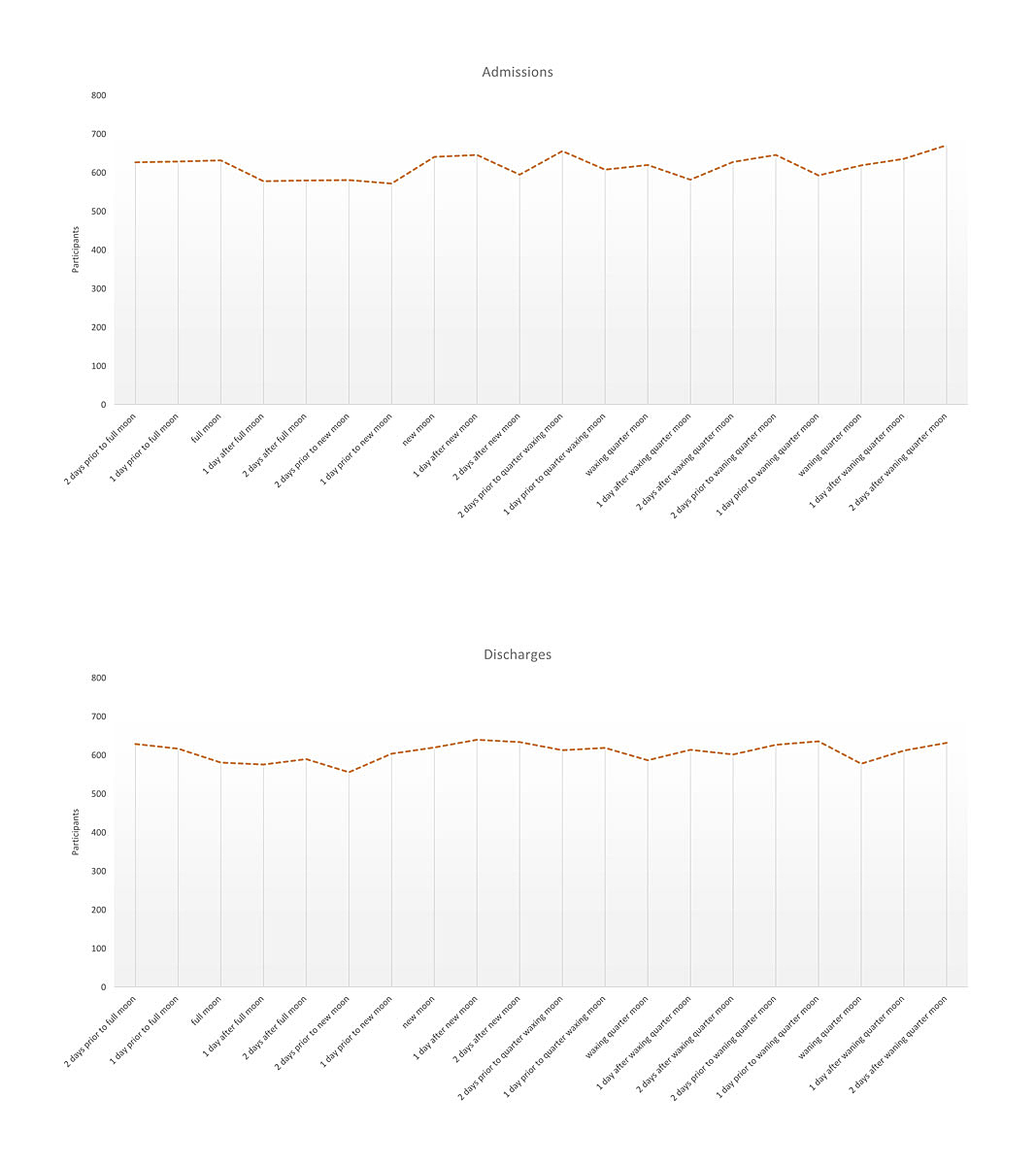
Figure 1 Number of admissions and discharges stratified by lunar phases.
DOI: https://doi.org/10.4414/smw.2019.20070
The belief that the moon influences human lives, emotions, and welfare is deeply anchored in human history, dating back to the ancient cultures of Assyria, Babylonia and Egypt [1, 2]. Medieval European mythology and superstition held that humans were transformed into werewolves or vampires under the influence of a full moon [3]. The antiquated and potentially offensive colloquial word “lunatic” derives from the Latin lunaticus (originally derived from Luna – moon), a term that originally referred mainly to epilepsy and madness, because those diseases were at one time thought to be caused by the moon [1].
To date, there is an ongoing debate concerning the connection between lunar cycle and psychiatric illness [4, 5]. The literature presents conflicting results, with the majority of studies showing no relationship between lunar cycle and either psychiatric admissions or emergency evaluations [6–9], psychiatric inpatient admissions [10], use of community psychiatry services [11, 12], violent behaviour [13–17], suicide [18, 19], or sleep disturbances [20, 21]. However, some studies do show relationships between the lunar cycle various psychiatric phenomena. For example, in a study of 17 healthy individuals Cajochen et al. [22] demonstrated under laboratory conditions that around the full moon, electroencephalogram (EEG) delta activity during non-REM sleep (an indicator of deep sleep) decreased by 30%, time to fall asleep increased by 5 minutes, and EEG-assessed total sleep duration was reduced by 20 minutes. These results presented a possible explanation for morning fatigue associated with a full moon [23]. In a prospective study involving 91 psychiatric inpatients, Calver et al. [4] observed an increase of violent and acute behavioural disturbances during the full moon among patients with severe forms of behavioural disturbance at admission. Another study, focused on gender differences regarding distress phone calls, showed that distress calls by women were more strongly linked to the lunar month than were those by men [24]. Family practitioners have also found a correlation between general practice consultation and the lunar cycle [25]. A large prospective case series of 2281 patients similarly showed an increase in frequency of outpatient psychiatric visits for non-affective psychosis during the full moon [26].
Parmar et al. [5] highlighted the importance of a clear operationalisation of the stages of the lunar cycle for scientific study; in their work, they observed significantly different outcomes regarding psychiatric emergency department presentations during different phases of the moon. Other authors have postulated associations, not only with the full moon, but also different lunar phases, showing sudden changes on the day of the full moon including crisis calls, suicide, and psychiatric admission rates as well as significant differences between the quarter waning and quarter waxing moon, including increases in homicides and crisis calls [27]. The authors presented positive findings regarding the relationship between lunar cycles and psychopathology, violence and admission to psychiatric institutions, highlighting the importance of using a more detailed approach than just the full moon. In addition, they suggest analyses should be stratified by gender and diagnostic categories.
Based on the literature the present study examined whether different stages of the lunar cycle have an impact on psychiatric patient admissions, discharges and length of stay in psychiatric clinics, as well as possible moderating influences of the lunar cycle on the relationship of these variables with psychiatric diagnosis and gender. We hypothesised that the phases of the lunar cycle will show no relationship to admission or discharge of patients to psychiatric inpatient treatment, nor will it have any bearing on the length of stay.
The present study was conducted in the Cantons Grisons, a rural alpine area located in south-eastern Switzerland. The study’s catchment area is characterised by the following features: it is geographically the largest canton of Switzerland with 7105 square kilometres; there are approximately 200,000 inhabitants; it lacks any major cities with populations over 50,000; the predominant business sectors include the tourism industry, agriculture and forestry. The Canton Grisons is entirely mountainous, located in the Swiss Alps (41% of the population lives at 3000 feet above sea level or higher) [28–30]. The clinics studied were operated by the Psychiatrische Dienste Graubünden (PDGR; English: Psychiatric Services of Grisons). PDGR is a state-owned but independently run network of inpatient and outpatient services, including two inpatient psychiatric clinics (clinic Waldhaus and clinic Beverin) with a combined total of 15 wards and 230 beds, including general acute psychiatry wards as well as specialised wards for the treatment of substance use disorders, personality disorders, forensic populations and geriatric patients. Both clinics provide psychiatric and physical healthcare, offer community mental health services, are legally obliged to provide healthcare to all individuals from the Canton Grisons, and are part of a single-tier psychiatric care system. With the exception of a small, privately funded clinic for the treatment of work-related burnout, PDGR is the sole provider of psychiatric services in Canton Grisons. Therefore, all psychiatric emergency admissions are sent to PDGR, which has the Cantonal mandate for psychiatric healthcare delivery for the region.
Patients admitted at least once from January 2005 to December 2015 were included. Data were documented as part of routine treatment and were anonymised before analysis. Because the study relied exclusively on anonymised, routine clinical data we did not require approval from the local ethics committee. The current study was performed in accordance with all national and international legal regulations and with the Declaration of Helsinki (7th revision, 2013).
Inclusion criteria for the study were admission to psychiatric inpatient treatment on one of the 15 wards from 2005 to 2015. Cases admitted before 2005 or dismissed after 2015 were excluded. No further inclusion or exclusion criteria were defined to ensure a naturalistic sample. The resulting dataset contained a total of 17,966 cases.
We used the structured routine data for sociodemographic data, clinical data and data about admission and discharge. Diagnostic classification was based on the International classification of Disease, 10th edition (ICD-10) [31]. All diagnoses were made by a board-certified psychiatrist. The analyses included only the main diagnosis of the patient; comorbid diagnoses were not included.
The lunar calendar was obtained from the website of the US Naval Observatory [32] and was used to calculate the dates of the full moon according to the geographic location of the clinics (coordinates: 46°51′N 9°32′E). We chose the city of Chur (capital of the Canton Grisons) as our reference point. The two clinics are within a 20 km radius and therefore affected by the same lunar cycle. We defined the following phases of the moon throughout the lunar cycle: (a) full moon, (b) quarter waxing moon, (c) new moon, and (d) quarter waning moon. In addition, we coded one day and two days preceding every lunar phase as well as the two days following the respective phases of the moon. This adds up to a total of 20 different lunar phases. Admissions were defined as the day the patient physically entered one of the two clinics. Discharges were defined analogously as the day the patient physically left the clinic. The length of stay was consequently characterised as the time between these two days, including the day of admission and the day the person was discharged.
The present study relied on a retrospective observational design, using a comparative cross-sectional analysis.
We used a Welch t-test to test for differences between men and women in the continuous variables, assuming unequal variances of the tested variables. To analyse gender differences in the categorical variables we used chi-squared tests. A significance level of p <0.05 was assumed.
We constructed two statistical models to determine whether (1) the distribution of the number of admissions follows a hypothesised Poisson distribution independently of the lunar phases, (2) the distribution of the number of discharges follows a hypothesised Poisson distribution, independently of the lunar phases. Based on the mean and variance of the daily count of admissions and discharges we analysed the possible Poisson distribution. We tested the Poisson distribution with a quantile-quantile (q-q) plot, with a straight line indicating a violation of the Poisson assumption. In order to test the models, we used a chi-square goodness-of-fit test to confirm the hypothesis that admissions and discharges will follow a Poisson distribution based on the natural variance, independently of the lunar phase at the day of admission or at discharge.
To test the strength of association, a Goodman and Kruskal’s tau was run to determine whether the lunar phase at admission or at discharge was associated with the type of main diagnosis of the individual.
The impact of the lunar phases at admission on the length of stay was analysed with a linear regression model adjusting for gender, age, marital status, treating clinic, citizenship, highest level of education and main diagnosis. The covariates, chosen based on the literature and experience, were variables that might influence the length of stay of inpatient psychiatric treatment. We tested the model assumptions, including an analysis of linearity as assessed by partial regression plots and a plot of studentised residuals against the predicted values, independence of residuals, using a Durbin-Watson statistic, and homoscedasticity, as assessed by visual inspection of a plot of studentised residuals versus unstandardised predicted values. There was no evidence of multicollinearity.
All statistical analyses were performed using IBM Software SPSS statistical software, version 24 (SPSS, 2010).
In total, 17,966 cases were included. As presented in table 1, female participants were significantly older than the men and more likely to be of Swiss citizenship. Men were more likely than women to have finished vocational school, technical school and college or university.
Table 1 Sociodemographic patient characteristics.
| Females | Males | p-value | |
|---|---|---|---|
| Number of cases | 8852 | 9114 | |
| Age (years), mean (SD) | 47.0 (19.2) | 44.3 (17.4) | <0.001 |
| Marital status, n (%) | <0.001 | ||
| Single | 3202 (36.2) | 4362 (47.9) | |
| Married | 2505 (28.3) | 2250 (24.7) | |
| Separated/divorced | 1716 (19.4) | 1746 (19.2) | |
| Widowed | 956 (10.8) | 232 (2.5) | |
| Unknown | 473 (5.3) | 524 (5.7) | |
| Citizenship, n (%) | <0.001 | ||
| Switzerland | 7492 (84.6) | 7355 (80.7) | |
| Other countries | 1068 (12.1) | 1446 (15.9) | |
| Unknown | 292 (3.3) | 313 (3.4) | |
| Highest level of education (%) | <0.001 | ||
| Elementary school | 1772 (20.0) | 1632 (17.9) | |
| High school | 132 (1.5) | 133 (1.5) | |
| Vocational school | 2901 (32.8) | 3563 (39.1) | |
| Technical school | 851 (9.6) | 939 (10.3) | |
| College or university | 172 (1.9) | 338 (3.7) | |
| No school | 673 (7.6) | 645 (7.1) | |
| Unknown | 2341 (26.5) | 1859 (20.4) |
SD = standard deviation
The clinical variables of the population are presented in table 2. The average length of stay was 38 days, with no relevant gender difference. Admitting diagnosis varied significantly by gender, with affective disorders being the most common diagnosis for women, followed by substance use and schizophrenia spectrum disorders. In contrast, among men substance abuse was the most common diagnosis, followed by affective and schizophrenia spectrum disorders.
Table 2 Clinical patient characteristics.
| Females | Males | p-value | |
|---|---|---|---|
| Number of cases | 8852 | 9114 | |
| Length of stay (days), mean (SD) | 38.0 (55.4) | 38.6 (88.5) | 0.617 |
| Main diagnosis, n (%) | <0.001 | ||
| Organic mental disorder | 465 (5.3) | 430 (4.7) | |
| Substance use disorder | 1515 (17.1) | 3317(36.4) | |
| Schizophrenia spectrum disorder | 1420 (16.0) | 1506 (16.5) | |
| Affective disorder | 2976 (33.6) | 1984 (21.8) | |
| Neurotic, stress related, somatoform disorder | 1047 (11.8) | 878 (9.6) | |
| Behavioural syndromes with physiological disturbances | 122 (1.4) | 13 (0.1) | |
| Personality disorder | 714 (8.1) | 354 (3.9) | |
| Mental retardation | 47 (0.5) | 53 (0.6) | |
| Disorders of psychological development | 4 (0.0) | 7 (0.1) | |
| Childhood onset disorders | 59 (0.7) | 75 (0.8) | |
| Non-psychiatric disorder | 483 (5.5) | 497 (5.5) |
SD = standard deviation
Of the 17,966 cases included in the study, 626 were admitted on a full moon, 640 on a new moon, 618 on a quarter waxing moon, and 619 on a quarter waning moon. Regarding the discharges, 586 cases were discharged on a full moon, 580 on a new moon, 619 on a quarter waxing moon, and 577 on a quarter waning moon. The number of admissions and discharges stratified by lunar phases are shown in figure 1.
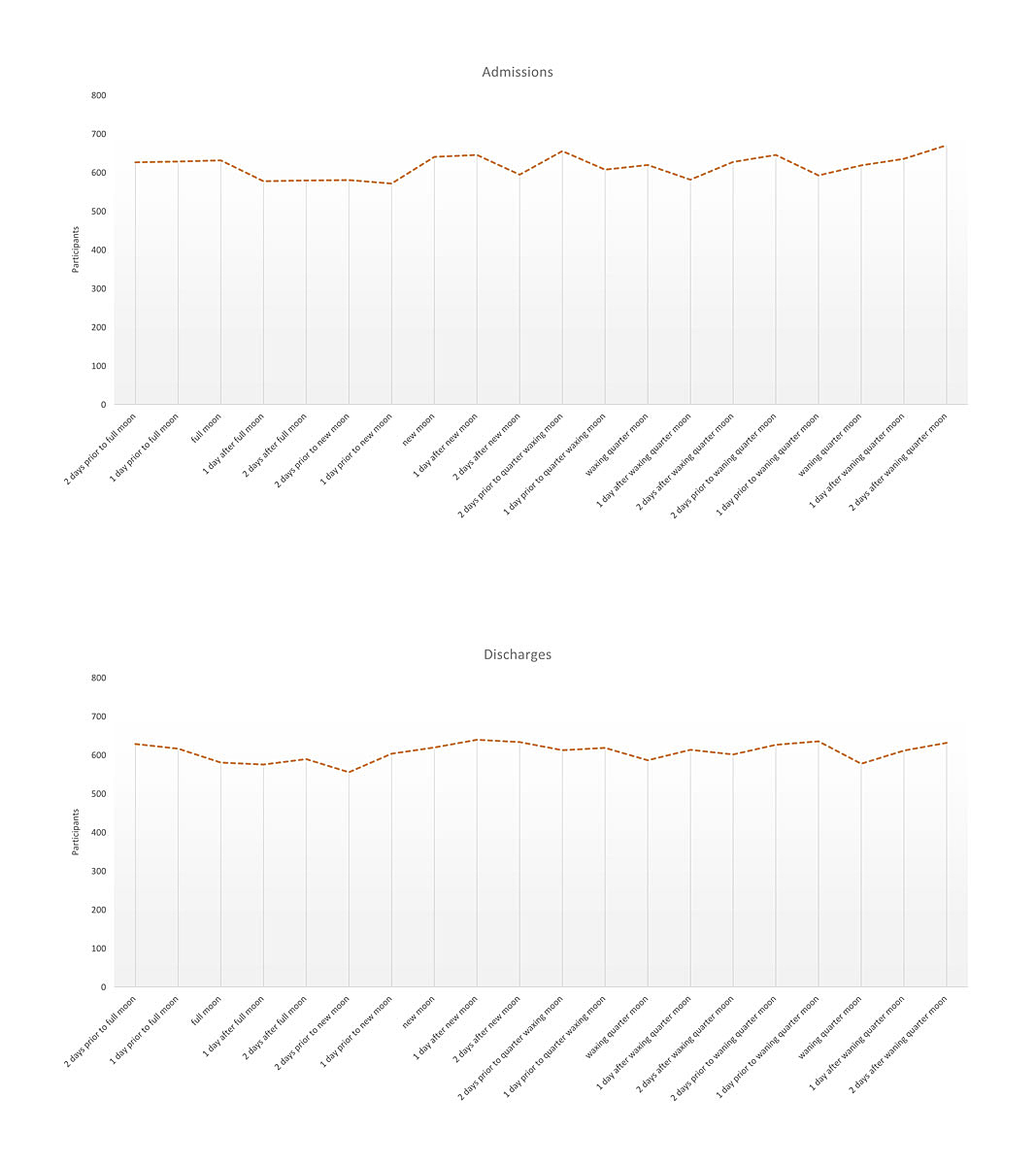
Figure 1 Number of admissions and discharges stratified by lunar phases.
A chi-square goodness-of-fit test was used to determine whether the cases admitted and discharges did not follow natural variation rates based on a Poisson distribution due to a possible influence of the moon. For the number of admissions, the minimum expected frequency was 616. The chi-square goodness-of-fit test indicated that the number of admitted participants was not statistically significantly different from an expected Poisson distribution of admissions (χ2(2) = 22.913, degrees of freedom [df] = 19, p = 0.241). For discharges, the minimum expected frequency was 607.4. The chi-square goodness-of-fit test indicated that the number of admitted participants was not statistically significantly different from an expected Poisson distribution of discharges (χ2(2) = 15.208, df = 19, p = .709).
In figure 2 the admissions according to the lunar phases are presented stratified by main diagnosis (represented by ICD-10 code groups). Goodman and Kruskal’s tau was run to determine whether the lunar phase at admission or at discharge was associated with the type of main diagnosis of the individual. Goodman and Kruskal’s tau was 0.015. This was a statistically nonsignificant reduction in the proportion of errors due to the category of main diagnosis as a predictor of the lunar phase at admission, p = 0.141. Also for the lunar phases at discharge there was no significance, Goodman and Kruskal’s tau was 0.015, p = 0.495.
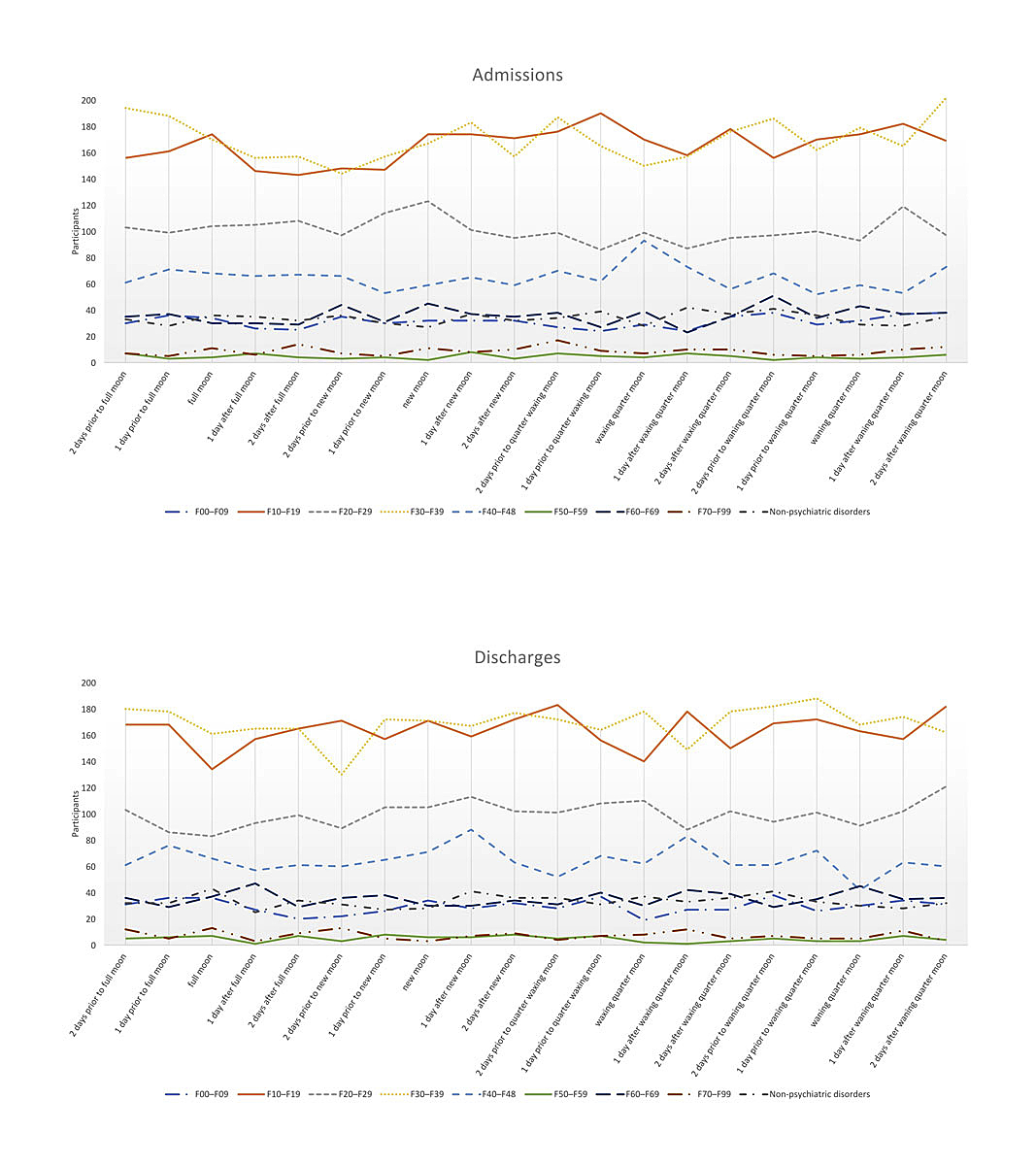
Figure 2 Number of admissions and discharges stratified by lunar phases and diagnosis.
There was no significant association between lunar cycle and length of stay. Regression coefficients and standard errors can be found in table 3.
Table 3 Multiple linear regression analysis: adjusted impact of the moon phases at admission on the length of stay.
| Variable | B | SE | p-value |
|---|---|---|---|
| Constant | 1.158 | ||
| Moon phases | 0.087 | 0.084 | 0.302 |
| Gender | 2.081 | 1.181 | 0.078 |
| Age | 0.424 | 0.036 | <0.001 |
| Marital status | −1.931 | 0.437 | <0.001 |
| Education level | −1.384 | 0.276 | <0.001 |
| Citizenship | 0.128 | 0.170 | 0.452 |
| Clinic | 4.349 | 1.190 | <0.001 |
| Main diagnosis | 0.232 | 0.037 | <0.001 |
B = unstandardised regression coefficient, SE = standard error of the coefficient
The results of this 10-year naturalistic observational study show that lunar cycles have no connection with the number of admissions or discharges of psychiatric inpatients. The large sample size and naturalistic study design, the inclusion of two psychiatric clinics, the addition of all diagnostic categories, and the availability of data over an extended observation period all enhance the generalisability of our findings. Furthermore, the two clinics were legally obliged to provide care to all individuals from their catchment area (Canton Grisons), which reduced the role of a possible admission bias (e.g., patients with certain mental illnesses or violent behaviour being preferentially admitted to adjacent hospitals) that could potentially be related to the phases of the moon [33]. Although the quality of data from prospective studies is generally superior to that from observational studies, evidence suggests that routine data can be of a quality suitable for these types of analyses [34]. The quality of data from the participating clinics was warranted by Swiss board-certified psychiatrists, centralised data management and systematic quality control.
Our findings with respect to admissions related to full moon are in line with those of Gorvin and Roberts [10], who did not find a higher number of psychiatric hospital admission during full moon. However, our results extend these findings, showing that not only does full moon have no association with admissions, but also all the other phases during a lunar cycle, such as quarter waning moon, new moon, and quarter waxing moon fail to show any relationship with admission rates to psychiatric inpatient treatment. On the contrary, the degree of consistency in admission rates across the various lunar phases is striking. These results stand in contrast to the statements of Parmar et al. [5], who proposed a more detailed analysis of phases of the moon, possibly demonstrating an impact on patients of lunar cycles. Also, we were not able to show any differences related to the gender of the participants, which contrasts with the results of Kollerstrom and Steffert [24]. Despite several authors describing possible connections between lunar cycle and different diagnostic categories, our analysis did not show variations regarding admission rates if stratified by diagnosis [22, 27, 35]. To our knowledge, no previous study has analysed the impact of the lunar phases on discharge rates from psychiatric inpatient treatment. Analogously to the results from inpatient admission, no connection with lunar phases was present in the discharge data. Furthermore, the analysis stratified by gender or diagnostic category did not result in any significant findings. An additional analysis developed a regression model examining the influence of various factors, including lunar phases, on length of stay in a psychiatric inpatient hospital. However, the moon did not show a relationship to the length of stay.
Despite the widely-held popular belief that the moon effects peoples’ mental health and subsequently psychiatric treatment, our study was unable to support any connection between any phase of the lunar cycle and either admission or discharge rates, nor with length of stay, at psychiatric inpatient clinics. The belief that the moon affects our lives and especially our emotions has existed for thousands of years and appears to be part of a collective, lay wisdom. Such beliefs seem largely impervious to the fact that a great deal of research, including the present study, has failed to support them. Research results as presented in this study need to be used for de-stigmatisation of mental illness in society, which continues to be a major issue and is also driven by the use of language as discussed in the introduction section. The reasons for the persistence of such beliefs may not be found in a rational understanding but more in a primal, emotional desire to believe that we are not solely responsible for our own behaviours, rather that some superior force also influences our actions and feelings.
The data from the two clinics that are part of the PDGR network represent non-profit, government owned hospitals serving catchment areas ranging from rural to (minor) urban areas. They are therefore representative of a part of the Swiss healthcare system. However, our findings might not be representative of settings such as university hospitals or private clinics, which might be able to choose which patients to treat. Since routine data were used in the current study, some clinically desirable information was not available for analyses, including information on the patients’ attitudes concerning lunar cycles, medication, and course of treatment. Data concerning educational attainment was missing for almost 25% of the sample, a factor which could arguably vary with beliefs about the effects of the moon on mental health. The study had a retrospective design, limiting the information to correlations between the moon and the analysed variables and precluding any causal inferences. Also, confounding variables not analysed could affect the relationship between the lunar cycles and the length of stay.
We believe that mental health providers should be aware of such popular beliefs while at the same time ensuring that they are aware of the scientific evidence supporting and refuting such beliefs, in order to ensure both that treatment remains evidence-based, and that patients are increasingly socialised in, and increasingly come to expect, an evidence-based approach to mental health care.
The authors would like to thank Mrs. Doris Rizzi, the secretary of the research department at Psychiatrische Dienste Graubünden, and Mr Romedo Meier, for their great help provided during data collection.
No financial support and no other potential conflict of interest relevant to this article was reported.
1Carroll RT. Full moon and lunar effects. In: The skeptic's dictionary: A collection of strange beliefs, amusing deceptions, and dangerous delusions. Hoboken, NJ: John Wiley & Sons; 2006.
2 Trapp CE . Lunacy and the moon. Am J Psychiatry. 1937;94(2):339–43. doi:.https://doi.org/10.1176/ajp.94.2.339
3 Lilienfeld SO , Arkowitz H . Lunacy and the full moon. Sci Am Mind. 2009;20(1):64–5. doi:.https://doi.org/10.1038/scientificamericanmind0209-64
4 Calver LA , Stokes BJ , Isbister GK . The dark side of the moon. Med J Aust. 2009;191(11-12):692–4.
5 Parmar VS , Talikowska-Szymczak E , Downs E , Szymczak P , Meiklejohn E , Groll D . Effects of Full-Moon Definition on Psychiatric Emergency Department Presentations. ISRN Emergency Medicine. 2014;2014:398791. doi:.https://doi.org/10.1155/2014/398791
6 McLay RN , Daylo AA , Hammer PS . No effect of lunar cycle on psychiatric admissions or emergency evaluations. Mil Med. 2006;171(12):1239–42. doi:.https://doi.org/10.7205/MILMED.171.12.1239
7 Bauer SF , Hornick EJ . Lunar effect on mental illness: the relationship of moon phase to psychiatric emergencies. Am J Psychiatry. 1968;125(5):696–7. doi:.https://doi.org/10.1176/ajp.125.5.696
8 Belleville G , Foldes-Busque G , Dixon M , Marquis-Pelletier E , Barbeau S , Poitras J , et al. Impact of seasonal and lunar cycles on psychological symptoms in the ED: an empirical investigation of widely spread beliefs. Gen Hosp Psychiatry. 2013;35(2):192–4. doi:.https://doi.org/10.1016/j.genhosppsych.2012.10.002
9 Kamat S , Maniaci V , Linares MY , Lozano JM . Pediatric psychiatric emergency department visits during a full moon. Pediatr Emerg Care. 2014;30(12):875–8. doi:.https://doi.org/10.1097/PEC.0000000000000291
10 Gorvin JJ , Roberts MS . Lunar phases and psychiatric hospital admissions. Psychol Rep. 1994;75(3, suppl):1435–40. doi:.https://doi.org/10.2466/pr0.1994.75.3f.1435
11 Amaddeo F , Bisoffi G , Micciolo R , Piccinelli M , Tansella M . Frequency of contact with community-based psychiatric services and the lunar cycle: a 10-year case-register study. Soc Psychiatry Psychiatr Epidemiol. 1997;32(6):323–6. doi:.https://doi.org/10.1007/BF00805436
12 Wilkinson G , Piccinelli M , Roberts S , Micciolo R , Fry J . Lunar cycle and consultations for anxiety and depression in general practice. Int J Soc Psychiatry. 1997;43(1):29–34. doi:.https://doi.org/10.1177/002076409704300103
13 Núñez S , Pérez Méndez L , Aguirre-Jaime A . Moon cycles and violent behaviours: myth or fact? Eur J Emerg Med. 2002;9(2):127–30. doi:.https://doi.org/10.1097/00063110-200206000-00005
14 Owen C , Tarantello C , Jones M , Tennant C . Lunar cycles and violent behaviour. Aust N Z J Psychiatry. 1998;32(4):496–9. doi:.https://doi.org/10.3109/00048679809068322
15 Biermann T , Asemann R , McAuliffe C , Ströbel A , Keller J , Sperling W , et al. Relationship between lunar phases and serious crimes of battery: a population-based study. Compr Psychiatry. 2009;50(6):573–7. doi:.https://doi.org/10.1016/j.comppsych.2009.01.002
16 Dowling KW . The effect of lunar phases on domestic violence incident rates. Forensic Exam. 2005;14(4):13–8.
17 Schafer JA , Varano SP , Jarvis JP , Cancino JM . Bad moon on the rise? Lunar cycles and incidents of crime. J Crim Justice. 2010;38(4):359–67. doi:.https://doi.org/10.1016/j.jcrimjus.2010.04.003
18 Biermann T , Estel D , Sperling W , Bleich S , Kornhuber J , Reulbach U . Influence of lunar phases on suicide: the end of a myth? A population-based study. Chronobiol Int. 2005;22(6):1137–43. doi:.https://doi.org/10.1080/07420520500398114
19 Koyuncu M , Ozturk D , Gülen B , Biberoglu S , Topal E , Duman A , et al. Does lunar cycle influence suicide attempts? AMED. 2019. doi:.https://doi.org/10.4328/AEMED.148
20 Cordi M , Ackermann S , Bes FW , Hartmann F , Konrad BN , Genzel L , et al. Lunar cycle effects on sleep and the file drawer problem. Curr Biol. 2014;24(12):R549–50. doi:.https://doi.org/10.1016/j.cub.2014.05.017
21 Haba-Rubio J , Marques-Vidal P , Tobback N , Andries D , Preisig M , Kuehner C , et al. Bad sleep? Don’t blame the moon! A population-based study. Sleep Med. 2015;16(11):1321–6. doi:.https://doi.org/10.1016/j.sleep.2015.08.002
22 Cajochen C , Altanay-Ekici S , Münch M , Frey S , Knoblauch V , Wirz-Justice A . Evidence that the lunar cycle influences human sleep. Curr Biol. 2013;23(15):1485–8. doi:.https://doi.org/10.1016/j.cub.2013.06.029
23 Röösli M , Jüni P , Braun-Fahrländer C , Brinkhof MW , Low N , Egger M . Sleepless night, the moon is bright: longitudinal study of lunar phase and sleep. J Sleep Res. 2006;15(2):149–53. doi:.https://doi.org/10.1111/j.1365-2869.2006.00520.x
24 Kollerstrom N , Steffert B . Sex difference in response to stress by lunar month: a pilot study of four years’ crisis-call frequency. BMC Psychiatry. 2003;3(1):20. doi:.https://doi.org/10.1186/1471-244X-3-20
25 Neal RD , Colledge M . The effect of the full moon on general practice consultation rates. Fam Pract. 2000;17(6):472–4. doi:.https://doi.org/10.1093/fampra/17.6.472
26 Parmeshwaran R , Patel V , Fernandes JM . Lunar phase and psychiatric illness in goa. Indian J Psychiatry. 1999;41(1):60–5.
27 Radin DI , Rebmam JM . Lunar correlates of normal, abnormal and anomalous human behavior. Subtle Energies. 1994;5(3):209–38.
28Kanton Graubünden. Wirtschaft. Graubünden im Überblick 2015. [15.02.2015]; Available from: https://www.gr.ch/DE/kanton/ueberblick/Seiten/Wirtschaft.aspx.
29Kanton Graubünden. Bevölkerung. Graubünden im Überblick 2015. [15.02.2015]; Available from: https://www.gr.ch/DE/kanton/ueberblick/Seiten/Bevoelkerung.aspx.
30Kanton Graubünden. Geografie. Graubünden im Überblick 2015. [15.02.2015]; Available from: https://www.gr.ch/DE/kanton/ueberblick/Seiten/Geografie.aspx.
31WHO. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines, Vol. 1. Geneva: World Health Organization; 1992.
32United States Navy Observatory. Phases of the Moon. Naval Oceanography Portal 2016. [08/10/2016].
33 Durm MW , Terry CL , Hammonds CR . Lunar phase and acting-out behavior. Psychol Rep. 1986;59(2):987–90. doi:.https://doi.org/10.2466/pr0.1986.59.2.987
34 Jaeger S , Flammer E , Steinert T . Basisdokumentation in der klinischen Praxis: Wie zuverlässig sind BADO-Daten? [Psychiatric basic documentation in practice: how reliable is the data?]. Psychiatr Prax. 2011;38(5):244–9. German. doi:.https://doi.org/10.1055/s-0030-1266084
35 Kazemi-Bajestani SMR , Amirsadri A , Samari SA , Javanbakht A . Lunar phase cycle and psychiatric hospital emergency visits, inpatient admissions and aggressive behavior. Asian J Psychiatr. 2011;4(1):45–50. doi:.https://doi.org/10.1016/j.ajp.2010.12.002
No financial support and no other potential conflict of interest relevant to this article was reported.