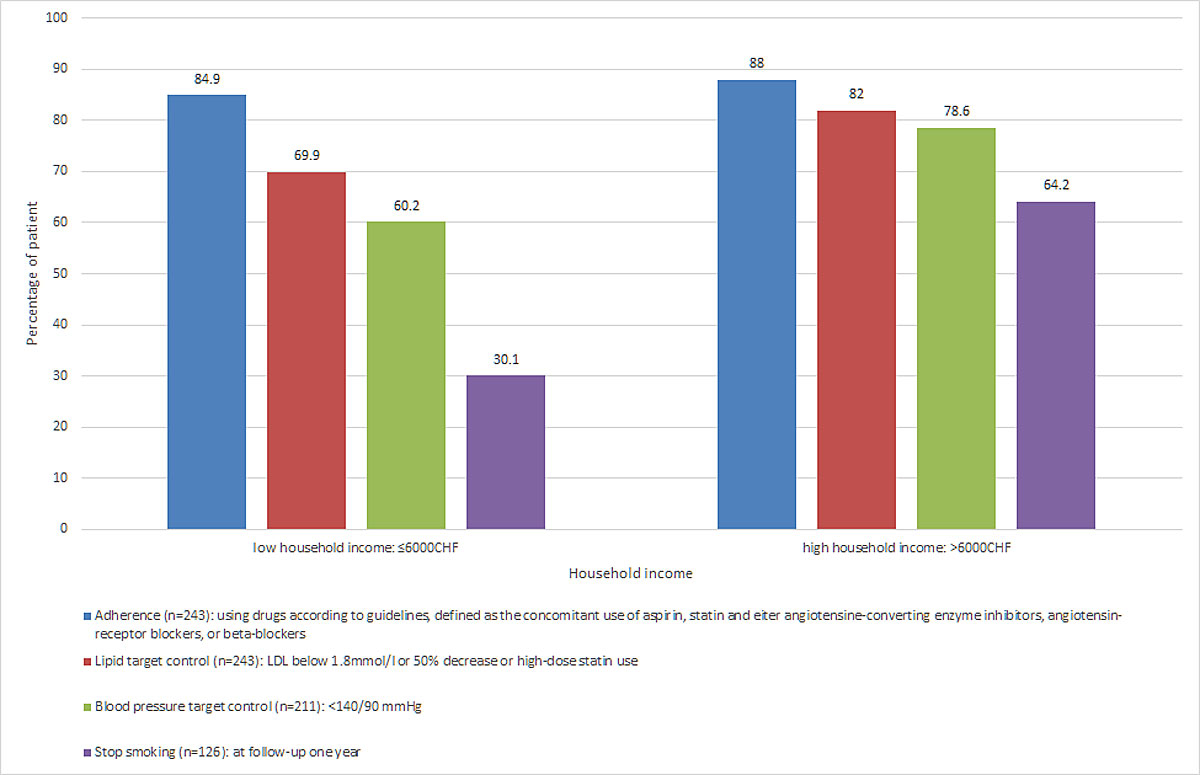
Figure 1 Association between income and control of cardiovascular risk factors one year after acute coronary syndrome.
DOI: https://doi.org/10.4414/smw.2019.20049
Socioeconomic status is a major determinant of a healthy life. In Europe and worldwide, socioeconomic status has been associated with cardiovascular events and mortality in many observational studies [1–10]. However, the mechanisms underlining these associations are debatable because socioeconomic status encompasses many components, including education and professional, familial and cultural status. In particular, few studies have focused on the relationship between income and cardiovascular disease, maybe because many industrialised countries, including Switzerland, have implemented universal health insurance. The concept of universal health insurance is to extend access to health care as widely as possible, limiting the impact of individual wealth.
Switzerland is a rich country, with a median salary of CHF 6189 (€ 5683) in 2014 according to the Federal Statistical Office [11]. Moreover, universal health insurance coverage is compulsory in Switzerland in order to protect the population against the renunciation of private health care. In this context, we aim to assess the association between income and control of cardiovascular risk factors one year after an acute coronary syndrome (ACS).
Between 28 January 2013 and 12 August 2014, we recruited 277 patients hospitalised with ACS in a university hospital in Switzerland as part of the SPUM-ACS cohort [12]. The inclusion criteria were a main diagnosis of ACS with increased troponins, modifications of electrocardiography and the presence of atherosclerosis in angiography. An exclusion criterion was the refusal to participate in the one-year follow-up visit.
Self-reported household income was defined as the income of all the people living under the same roof and after the deduction of compulsory social insurance contributions, pension funds and child allowances. In the questionnaire, patients could choose to state their annual income in two different ways. They could directly state their net household income, or they could select from predefined income categories: less than CHF 3000 (€ 2560); less than CHF 4500 (€ 3413.30); more than CHF 4500 (€ 3413.30); less than CHF 6000 (€ 5120); less than CHF 6000 (€ 5120); less than CHF 9000 (€ 7680); less than CHF 9000 (€ 7680) (table S1 in appendix 1). We excluded 22 patients for whom income information was missing. The final sample was 255 patients. We then classified patients into two income categories: high-income (higher than CHF 6000 (€ 5120) per month) and low-income (less than or equal to CHF 6000 (€ 5120) per month), based on the median monthly income in Switzerland of CHF 6189 (€ 5683) [11].
Demographic and socioeconomic status were assessed with a validated self-reported questionnaire at baseline and/or at one year. Education was categorised into high-school level or higher, or less than high-school. Marital status was classified as married or not. Living status was classified as living alone or with someone. Working status comprised full time, part time and unemployed. Smoking status was categorised into never, former and current smoker. Health insurance deductibles was categorised in two groups: low, defined as CHF 300 or 500 (€ 256 or € 426.60), and high, defined as CHF 1000, 1500, 2000 or 2500 (€ 853.30, € 1280, € 1706.60 or € 2133.30). Hypertension was defined as systolic blood pressure >140 mm Hg and diastolic >90 mm Hg or use of antihypertensive drugs. Physical activity was measured with the International Physical Activity Questionnaire (IPAQ). We used a validated self-assessed questionnaire, the 20-items Center for Epidemiologic Studies Depression Scale (CES-D), to screen for depression (score ≥16) during hospitalisation [13]. The cut-off values used to stratify the variables were based on standards used for cardiovascular disease prevention in clinics [14].
One year after hospital discharge, control of cardiovascular risk factors was assessed during a face-to-face clinical visit with a study nurse. Lipid profile was measured and processed locally using standardised and certified dosage methods. LDL cholesterol was calculated using the Friedewald formula when triglyceride levels were below 4.5 mmol/l. Targets for cardiovascular risk factors one year after discharge included:
Baseline characteristics are presented as means ± standard deviations or frequencies and percentages. To assess the association between income and control of cardiovascular risk factors one year after hospitalisation, we used unadjusted and multivariate adjusted logistic regression models for each outcome and reported odds ratios (ORs) with 95% confidence intervals (95% CIs). In model I, crude analysis was performed. In model II, we adjusted for age and sex, and in model III we further adjusted for education, living status and working status to take into account major socio-demographic variables. The variables included in the multivariate-adjusted model were not determined according to statistical significance, but based on their potential socioeconomic impact. To avoid overadjustment, marital status was not included in the model, because married patients had a higher household income that patients who lived alone. Due to the observational nature of the study, no formal sample size calculation was performed, but all available patients with information on income were included. All hypothesis tests were two-sided, and the significance level was set at 5%. Statistical analyses were performed using STATA 14® (STATA Corp, College Station, TX, USA).
The Medical Ethics Committee of Lausanne approved the study and all participants gave written informed consent to participation in the study.
Overall, 52.2% (n = 133) of patients with ACS were in the low-income category, and 47.8% (n = 122) in the high-income category. A monthly household income of below CHF 3000 (€ 2560) was reported by 29(11.4%) of patients. This is close to the threshold of poverty in Switzerland, defined as below CHF 2500 (€ 2133.30). The baseline characteristics of the study population by income category are reported in table 1. Patients in the low-income category were older and more frequently men than those in the high-income category. Patients in the low-income category also had a lower level of education, more frequently lived alone, and worked full-time less frequently compared to patients in the high-income category.
Table 1 Baseline characteristics by household income status (n = 255).
|
Low income*
(n = 133) |
High income†
(n = 122) |
p-value | ||
|---|---|---|---|---|
| Demographics | Age, years | 64.2 (13) | 59.8 (10.4) | 0.004 |
| Men, no. (%) | 91 (68.4) | 111 (91) | <0.001 | |
| Caucasian, no. (%) | 131 (98.5) | 120 (98.4) | 0.51 | |
| Education (n = 253) |
High school or higher, no. (%) | 29 (22.1) | 56 (45.9) | <0.001 |
| Marital status | Married, no. (%) | 57 (42.9) | 88 (72.1) | <0.001 |
| Living status (n = 229) |
Alone, no. (%) | 53 (39.9) | 18 (14.9) | <0.001 |
| Working status (n = 253) |
Full time, no. (%) | 41 (30.8) | 62 (51.7) | 0.003 |
| Part time, no. (%) | 16 (12) | 11 (9.2) | ||
| Unemployed, no. (%) | 76 (57.1) | 47 (39.2) | ||
| Health insurance | Monthly premium, CHF (n = 253) | 425 (149) | 416 (129) | 0.63 |
| Low deductible‡, no. (%) (n = 247) | 102 (80.9) | 78 (64.5) | 0.004 | |
| Supplemental private, no. (%) (n = 154) | 45 (54.2) | 52 (73.2) | 0.015 | |
| Smoking status | Never, no. (%) | 41 (30.8) | 44 (36.1) | 0.33 |
| Former, no. (%) | 23 (17.3) | 26 (21.3) | ||
| Current, no. (%) | 69 (51.9) | 52 (42.6) | ||
| Elevated alcohol use§, no. (%) (n = 248) | 31 (24.0) | 32 (26.9) | 0.6 | |
| Low physical activity¶, no. (%) (n = 221) | 20 (18.2) | 15 (13.5) | 0.34 | |
| Comorbidities | Hypertension‖, no. (%) | 69 (51.9) | 54 (44.3) | 0.22 |
| Systolic blood pressure, mm Hg | 134 (22) | 130 (25) | 0.2 | |
| LDL cholesterol, mmol/l | 3.2 (1.0) | 3.5 (1.2) | 0.08 | |
| Diabetes**, no. (%) | 23 (17.3) | 16 (13.1) | 0.35 | |
| Obesity, no. (%) | 26 (19.5) | 26 (21.3) | 0.73 | |
| Depression††, no. (%) (n = 246) | 36 (27.7) | 27 (23.3) | 0.42 | |
| Medication before hospitalisation | Statins, no. (%) | 27 (20.3) | 38 (31.2) | 0.047 |
| High-dose statins, no. (%) | 7 (5.3) | 9 (7.4) | 0.49 | |
| Antihypertensive drugs, no. (%) | 68 (51.1) | 45 (36.9) | 0.022 | |
| LDL = low density lipoprotein; MET = metabolic equivalent Data are given as means (standard deviations) unless otherwise indicated. * Low household income: CHF 6000 (€ 5120) or less. † High household income: more than CHF 6000 (€ 5120). ‡ Defined as CHF 300 or 500 (€ 256 or 426.60), compared to CHF 1000, 1500, 2000 or 2500 (€ 853.30, € 1280, € 1706.60 or € 2133.30). § Defined as more than 14 units of alcohol per week. ¶ Defined as less than 500 MET-min per week. ‖ Defined as a systolic blood pressure ≥140 mm Hg, a diastolic blood pressure ≥90 mm Hg, or use of blood pressure lowering drugs. ** Based on patients’ self-reporting, use of antidiabetic medication/insulin, or a haemoglobin A1c of ≥6.5%. †† Defined as a score ≥16 on the 20 items Centre for Epidemiologic Studies Depression Scale (CES-D). |
||||
One-year rates of ideal cholesterol management did not differ significantly between the two income categories, although there was a trend, with 82% achieving ideal cholesterol management for the high and 69.8% for the low-income category (age- and sex-adjusted OR 1.6, 95% CI 0.84–3.03, p = 0.15) (table 2 and fig. 1). In contrast, more patients in the high-income category reached blood pressure targets than in the low-income category (78.2% vs 60.2%, age- and sex-adjusted OR 2.37, 95%CI 1.25–4.52, p = 0.008). This association was slightly modified after further adjustment for education, living status and working status (multivariate-adjusted OR 2.19, 95% CI 1.09–4.41, p = 0.029). One year after hospital discharge, more baseline smokers in the high-income category had stopped smoking than in the low-income category (64.2% vs 30.1%, age- and sex-adjusted OR 4.74, 95% CI 2.13–10.59, p <0.001; multivariate-adjusted OR 3.82, 95% CI 1.58–9.24, p = 0.003). There were no differences in the rates of treatment adherence between the two income categories, with 88% for the high- and 84.9% for the low-income category (age- and sex-adjusted OR 1.08, 95% CI 0.49–2.38, p = 0.86; multivariate-adjusted OR 1.27, 95%CI 0.55–2.94, p = 0.58).
Table 2 One-year control of cardiovascular risk factors and household income
| n | Achieved target (n) | OR (95% CI) | p-value | R2 | Age- and sex-adjusted OR | p-value | R2 | Multivariate-adjusted OR* | p-value | R2 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lipid target† | 243 | ||||||||||
| Low income | 88 | 1.00 | NA | 1.00 | NA | 1.00 | NA | ||||
| High income | 96 | 1.97 (1.08–3.62) | 0.02 | 0.02 | 1.60 (0.84–3.03) | 0.15 | 0.04 | 1.72 (0.86–3.45) | 0.12 | 0.05 | |
| Blood pressure target‡ | 211 | ||||||||||
| Low income | 65 | 1.00 | NA | 1.00 | NA | 1.00 | NA | ||||
| High income | 81 | 2.44 (1.33–4.48) | 0.004 | 0.03 | 2.37 (1.25–4.52) | 0.008 | 0.04 | 2.19 (1.09–4.41) | 0.029 | 0.06 | |
| Stop smoking | 126 | ||||||||||
| Low income | 22 | 1.00 | NA | 1.00 | NA | 1.00 | NA | ||||
| High income | 34 | 4.15 (1.96–8.80) | <0.001 | 0.08 | 4.74 (2.13–10.59) | <0.001 | 0.11 | 3.82 (1.58–9.24) | 0.003 | 0.16 | |
| Adherence§ | 243 | ||||||||||
| Low income | 107 | 1.00 | NA | 1 | NA | 1.00 | NA | ||||
| High income | 103 | 1.31 (0.62–2.74) | 0.48 | 0.003 | 1.08 (0.49–2.38) | 0.86 | 0.02 | 1.27 (0.55–2.94) | 0.58 | 0.05 |
CI = confidence interval; LDL = low density lipoprotein; NA = not available OR = odds ratio; R2 = goodness of fit Low household income: CHF 6000 (€ 5120) or less; high household income: more than CHF 6000 (€ 5120). * Adjusted for age, sex, education, living status and working status. † LDL below 1.8 mmol/l, 50% decrease or high-dose statin use. ‡ Blood pressure <140/90 mm Hg. § Using drugs according to guidelines, defined as the concomitant use of aspirin, statin and either angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers or beta-blockers.
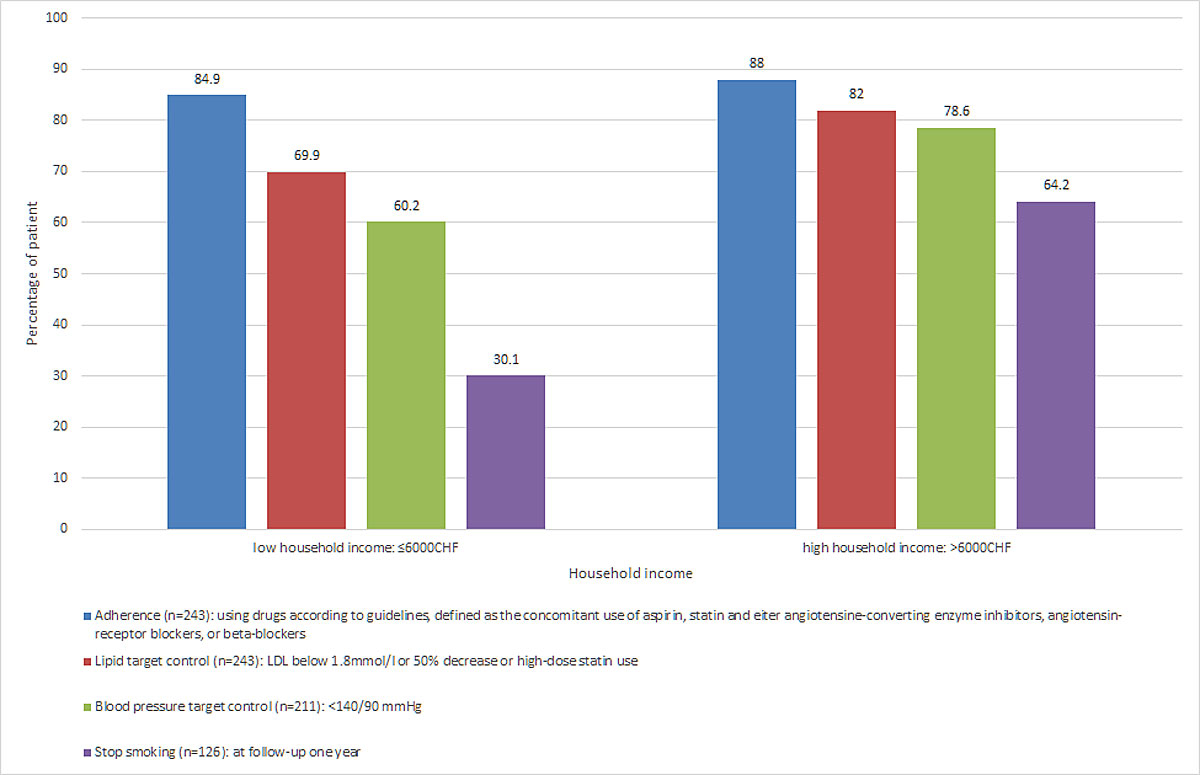
Figure 1 Association between income and control of cardiovascular risk factors one year after acute coronary syndrome.
Visits to a primary care physician one year after acute coronary syndrome did not differ significantly between the two income categories, with 98.3% for the high- and 97.6% for the low-income category (p = 0.71) (table 3). In contrast, more patients in the high-income category visited a cardiologist than in the low-income category (96.6 vs 82.9%, p = 0.001). One year after hospital discharge, there was no significant difference for cardiac rehabilitation between the two income categories, with 79.8% for the high- and 72.6% for the low-income category (p = 0.19). There was no difference in use of hypertensive drugs between the two income categories, with 97.6% for the low- and 94% for the high-income category (p = 0.16).
Table 3 Quality of care measured one year after discharge, by household income
|
Low income*
(n = 133) |
High income†
(n = 122) |
p-value | |
|---|---|---|---|
| Visit to a primary care physician, no. (%) (n = 242) | 122 (97.6) | 115 (98.3) | 0.71 |
| Visit to a cardiologist, no. (%) (n = 240) | 102 (82.9) | 113 (96.6) | 0.001 |
| Cardiac rehabilitation, no. (%) (n = 238) | 90 (72.6) | 91 (79.8) | 0.19 |
| Use of hypertensive drugs, no. (%) (n = 243) | 123 (97.6) | 110 (94.0) | 0.16 |
| Use of statins, no. (%) (n = 243) | 115 (91.3) | 113 (96.6) | 0.09 |
| Use of aspirin, no. (%) (n = 243) | 119 (94.4) | 113 (96.6) | 0.42 |
* Low household income: CHF 6000 (€ 5120) or less † High household income: more than CHF 6000 (€ 5120).
Among patients with ACS from a university hospital living in the French-speaking part of Switzerland, with universal health insurance coverage, we found that long-term control of cardiovascular risk factors was worse among patients with an income below the Swiss median compared to those with an income above the Swiss median. One year after hospital discharge for ACS, rates of smoking cessation and blood pressure control were lower among patients with a lower income than patients with a higher income, even after adjusting for other socio-demographic variables such as education, living status and working status.
Several studies have previously reported an association between socioeconomic status and cardiovascular outcomes among patients with pre-existing cardiovascular disease [7, 9, 15]. These studies showed that patients with low socioeconomic status face worse cardiovascular outcomes and have a worse lifestyle compared to patients with a high socioeconomic status. However, only a few studies have examined the income of patients in the context of ACS [1, 3, 8, 9, 15, 16]. In these studies, the outcomes that were evaluated were mainly the recurrence of cardiovascular events or mortality, but not many studies reported comprehensive data on the control of cardiovascular risk factors. A previous study from Canada examined the association between income and one-year use of statins and antihypertensive drugs after ACS [1]. They found that patients with lower incomes had a lower use of statins and antihypertensive drugs one year after ACS compared to those with higher incomes. One study of healthy participants in the USA showed that among that group both income and education were independently associated with systolic blood pressure [16]. Consistent with these studies, we also found a worse one-year control of blood pressure in the low-income group compared to the high-income group, even though baseline levels of systolic blood pressure were not different. However, we did not find major differences in drug adherence between the two income categories one year after ACS. Therefore, it remains unclear whether patients in the high-income category better control their blood pressure through lifestyle changes or through optimal drug adherence.
We found that one-year smoking cessation was more commonly achieved by patients in the high-income category than those in the low-income category, even after adjustment for socio-demographic variables. Previous studies performed in the general population have reported a consistent association between income and smoking cessation rates [17, 18]. However, among patients with ACS, the specific role of income for smoking cessation has been studied less. Similar to our results, one previous study among patients with ACS from the USA found that smokers with higher household incomes had substantially higher odds of quitting than low-income smokers, but the follow-up duration was limited to eight months [17]. Among patients undergoing percutaneous coronary intervention, a study from Luxembourg found that smoking cessation was also significantly associated with income, but less than 20% of these patients had ACS [18]. Consistent with these studies, we also found a lower rate of smoking cessation in the low-income group than in the high-income group among ACS patients. Furthermore, we were able to demonstrate that income remained significantly associated with smoking cessation rates even after adjustment for education, living status and working status, thus demonstrating the specific role of income. The reason for this strong effect of income compared to social status or education remains unclear. It is possible that income better reflects social status and lifestyle than other parameters in today’s society.
Our study has several limitations. Firstly, information on income was obtained using a self-reported questionnaire. Although most previous studies have examined outcomes with self-reported questionnaires rather than with administrative records, we cannot exclude a misclassification bias in our study [19, 20]. In fact, one review highlighted the many possible contributors to inaccurate reporting during the measurement of income in surveys [20]. However, in our study we measured household income rather than the income of individuals in order to take into account the family situation and to avoid someone claiming the income of the main earner as his or her own income. This is a strength of our approach. Secondly, we had a relatively small sample of ACS patients with income information available. Therefore, we could not examine the interactions between all confounding factors. Still, we were able to adjust our results for important social variables such as education, working status and living status. Furthermore, we examined the impact of income after an ACS in a country with universal health insurance, in which patients have access to health care independently of their income.
Among patients with ACS who have mandatory universal health insurance, the optimal control of cardiovascular risk factors one year after hospital discharge differed according to household income. Inequalities were evident for smoking cessation and blood pressure control, but not for the use of recommended drugs after ACS, or for attaining a lipid target. Universal health insurance coverage may limit the impact of income inequality regarding drug use after ACS, but not regarding changes in lifestyle and behaviour.
Table S1 Income categories based on the original self-reported questionnaire (n = 255).
| Number | Percentage (%) | |
|---|---|---|
| <CHF 3000 (<€ 2560) | 29 | 11.4 |
| CHF 3000 (€ 2560) | 7 | 2.7 |
| CHF 3000 to 4500 (€ 2560 to € 3840) | 37 | 14.5 |
| CHF 4500 (€ 3840) | 8 | 3.1 |
| CHF 4500 to 6000 (€ 3840 to € 5120) | 52 | 20.4 |
| CHF 6000 (€ 5120) | 12 | 4.7 |
| CHF 6000 to 9000 (€ 5120 to € 7680) | 59 | 23.1 |
| CHF 9000 (€ 7680) | 6 | 2.4 |
| >CHF 9000 (>€ 7680) | 45 | 17.6 |
Table S2 One-year smoking cessation and household income, according to different scenarios for missing information.
| n |
Achieved target
(n) |
OR (95% CI) | p-value | R2 | Age- and sex-adjusted OR | p-value | R2 | Multivariate-adjusted OR* | p-value | R2 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Stop smoking† | 126 | ||||||||||
| Low income | 22 | 1.00 | NA | 1.00 | NA | 1.00 | NA | ||||
| High income | 34 | 4.15 (1.96–8.80) | <0.001 | 0.08 | 4.74 (2.13–10.59) | <0.001 | 0.11 | 3.82 (1.58–9.24) | 0.003 | 0.16 | |
| Stop smoking‡ | 126 | ||||||||||
| Low income | 26 | 1.00 | NA | 1.00 | NA | 1.00 | NA | ||||
| High income | 37 | 4.18 (1.96–8.91) | <0.001 | 0.08 | 4.59 (2.07–10.18) | <0.001 | 0.10 | 4.15 (1.71–10.07) | 0.002 | 0.15 | |
| CI = confidence interval; NA = not available OR = odds ratio; R2 = goodness of fit Low household income: CHF 6000 (€ 5120) or less; high household income: more than CHF 6000 (€ 5120). * Adjusted for age, sex, education, living status and working status. † considering the seven smokers with missing information for smoking cessation at one year as current smokers (worst case scenario). ‡ considering the seven smokers with missing information for smoking cessation at one year as non-smokers (best case scenario). |
|||||||||||
We acknowledge the cooperation of the participating centre, practicing physicians, referring doctors and institutions.
This study was supported by a grant from the Department of Community Medicine and Health, University of Lausanne, Switzerland. The SPUM-ACS cohort is supported by the Swiss National Science Foundation (SNSF 33CM30-124112, Inflammation and ACSs (ACS) – Novel strategies for prevention and clinical management, and SNSF 32473B_163271, Long-term benefit of the multi-centre, multi-dimensional secondary prevention program in patients with ACSs). None of the funding bodies had any role in the design and conduct of the study, the collection, management, analysis and interpretation of the data, or the preparation, review and approval of the manuscript.
TL has received research or educational grants and/or honoraria from AstraZeneca, Amgen, Daiichi-Sankyo, Sanofi and Novartis.
1 Alter DAFB , Franklin B , Ko DT , Austin PC , Lee DS , Oh PI , et al. Socioeconomic status, functional recovery, and long-term mortality among patients surviving acute myocardial infarction. PLoS One. 2013;8(6):e65130. doi:.https://doi.org/10.1371/journal.pone.0065130
2 Ng DK , Brotman DJ , Lau B , Young JH . Insurance status, not race, is associated with mortality after an acute cardiovascular event in Maryland. J Gen Intern Med. 2012;27(10):1368–76. doi:.https://doi.org/10.1007/s11606-012-2147-9
3 Fabreau GELA , Leung AA , Southern DA , Knudtson ML , McWilliams JM , Ayanian JZ , et al. Sex, socioeconomic status, access to cardiac catheterization, and outcomes for acute coronary syndromes in the context of universal healthcare coverage. Circ Cardiovasc Qual Outcomes. 2014;7(4):540–9. doi:.https://doi.org/10.1161/CIRCOUTCOMES.114.001021
4 Tang KL , Rashid R , Godley J , Ghali WA . Association between subjective social status and cardiovascular disease and cardiovascular risk factors: a systematic review and meta-analysis. BMJ Open. 2016;6(3):e010137. doi:.https://doi.org/10.1136/bmjopen-2015-010137
5 Jones DAHJ , Howard JP , Rathod KS , Gallagher SM , Knight CJ , Jain AK , et al. The impact of socio-economic status on all-cause mortality after percutaneous coronary intervention: an observational cohort study of 13,770 patients. EuroIntervention. 2015;10(10):e1–8. doi:.https://doi.org/10.4244/EIJV10I10A196
6 Fournier S , Muller O , Ludman AJ , Lauriers N , Eeckhout E . Influence of socioeconomic factors on delays, management and outcome amongst patients with acute myocardial infarction undergoing primary percutaneous coronary intervention. Swiss Med Wkly. 2013;143:w13817. doi:.https://doi.org/10.4414/smw.2013.13817
7 Stringhini S , Carmeli C , Jokela M , Avendaño M , Muennig P , Guida F , et al.; LIFEPATH consortium. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1·7 million men and women. Lancet. 2017;389(10075):1229–37. doi:.https://doi.org/10.1016/S0140-6736(16)32380-7
8 van Oeffelen AA , Agyemang C , Bots ML , Stronks K , Koopman C , van Rossem L , et al. The relation between socioeconomic status and short-term mortality after acute myocardial infarction persists in the elderly: results from a nationwide study. Eur J Epidemiol. 2012;27(8):605–13. doi:.https://doi.org/10.1007/s10654-012-9700-z
9 Jakobsen L , Niemann T , Thorsgaard N , Thuesen L , Lassen JF , Jensen LO , et al. Dimensions of socioeconomic status and clinical outcome after primary percutaneous coronary intervention. Circ Cardiovasc Interv. 2012;5(5):641–8. doi:.https://doi.org/10.1161/CIRCINTERVENTIONS.112.968271
10 Stringhini S , Sabia S , Shipley M , Brunner E , Nabi H , Kivimaki M , et al. Association of socioeconomic position with health behaviors and mortality. JAMA. 2010;303(12):1159–66. doi:.https://doi.org/10.1001/jama.2010.297
11Travail et rémunération, enquête suisse sur le niveau et la structure des salaires 2014. In: Confédération suisse Dfdli, Office fédéral de la statistique (ed.). Neuchâtel, Suisse: Office fédéral de la statistique service de presse; 2015.
12 Nanchen D , Gencer B , Muller O , Auer R , Aghlmandi S , Heg D , et al. Prognosis of Patients With Familial Hypercholesterolemia After Acute Coronary Syndromes. Circulation. 2016;134(10):698–709. doi:.https://doi.org/10.1161/CIRCULATIONAHA.116.023007
13 Vilagut G , Forero CG , Barbaglia G , Alonso J . Screening for Depression in the General Population with the Center for Epidemiologic Studies Depression (CES-D): A Systematic Review with Meta-Analysis. PLoS One. 2016;11(5):e0155431. doi:.https://doi.org/10.1371/journal.pone.0155431
14 Piepoli MF , Hoes AW , Agewall S , Albus C , Brotons C , Catapano AL , et al.; ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–81. doi:.https://doi.org/10.1093/eurheartj/ehw106
15 Khaing W , Vallibhakara SA , Attia J , McEvoy M , Thakkinstian A . Effects of education and income on cardiovascular outcomes: A systematic review and meta-analysis. Eur J Prev Cardiol. 2017;24(10):1032–42. doi:.https://doi.org/10.1177/2047487317705916
16 Cundiff JM , Uchino BN , Smith TW , Birmingham W . Socioeconomic status and health: education and income are independent and joint predictors of ambulatory blood pressure. J Behav Med. 2015;38(1):9–16. doi:.https://doi.org/10.1007/s10865-013-9515-8
17 Holtrop JS , Stommel M , Corser W , Holmes-Rovner M . Predictors of smoking cessation and relapse after hospitalization for acute coronary syndrome. J Hosp Med. 2009;4(3):E3–9. doi:.https://doi.org/10.1002/jhm.415
18 Tchicaya A , Lorentz N , Demarest S . Income-related inequality in smoking cessation among adult patients with cardiovascular disease: a 5-year follow-up of an angiography intervention in Luxembourg. BMC Cardiovasc Disord. 2017;17(1):107. doi:.https://doi.org/10.1186/s12872-017-0541-2
19 Galobardes B , Shaw M , Lawlor DA , Lynch JW , Davey Smith G . Indicators of socioeconomic position (part 1). J Epidemiol Community Health. 2006;60(1):7–12. doi:.https://doi.org/10.1136/jech.2004.023531
20 Moore JC , Welniak EJ . Income Measurement Error in Surveys: A review. J Off Stat . 2000;16(4):331.
This study was supported by a grant from the Department of Community Medicine and Health, University of Lausanne, Switzerland. The SPUM-ACS cohort is supported by the Swiss National Science Foundation (SNSF 33CM30-124112, Inflammation and ACSs (ACS) – Novel strategies for prevention and clinical management, and SNSF 32473B_163271, Long-term benefit of the multi-centre, multi-dimensional secondary prevention program in patients with ACSs). None of the funding bodies had any role in the design and conduct of the study, the collection, management, analysis and interpretation of the data, or the preparation, review and approval of the manuscript.
TL has received research or educational grants and/or honoraria from AstraZeneca, Amgen, Daiichi-Sankyo, Sanofi and Novartis.