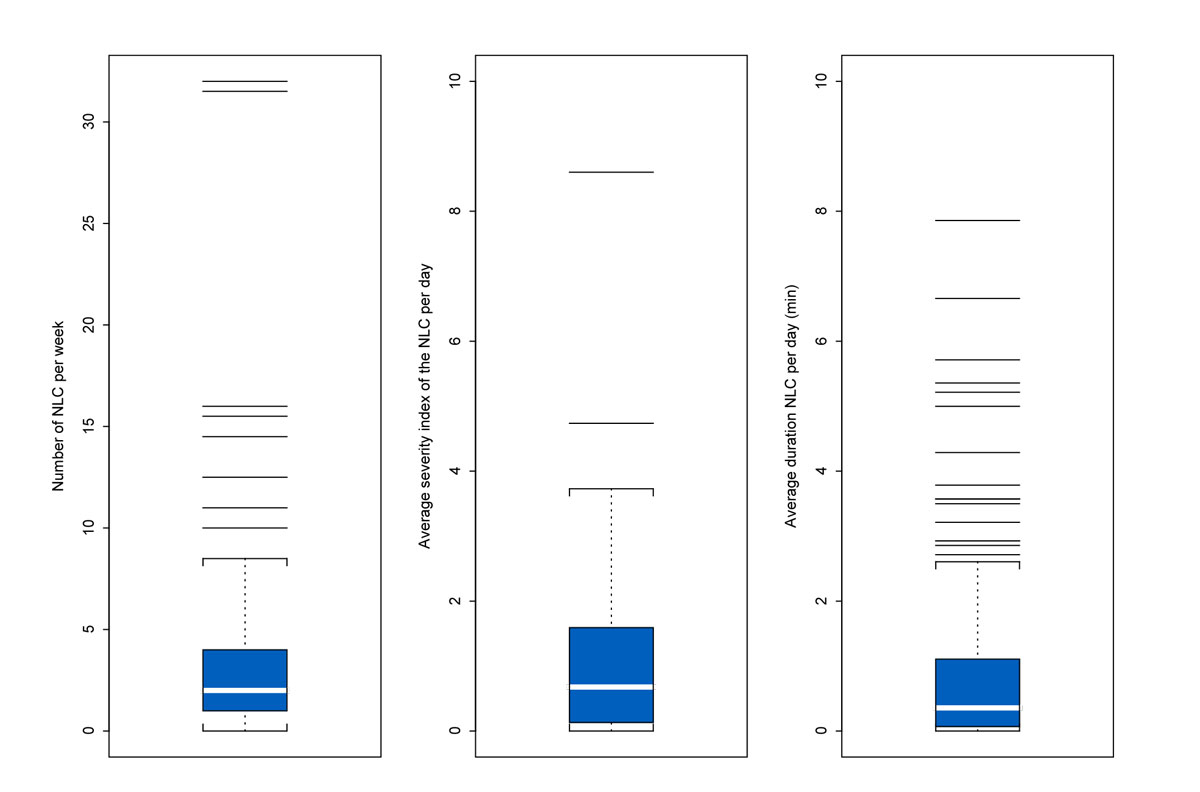
Figure 1 Number of nocturnal leg cramps (NLC) per week, average severity index per day, and average duration in minutes per day per patient (n = 129).
DOI: https://doi.org/10.4414/smw.2019.20048
Nocturnal leg cramps are a musculoskeletal disorder characterised by sudden and painful involuntary contractions of the lower limbs occurring during prolonged rest periods, mostly at night [1–3]. They often cause sleep disturbances, which can seriously affect quality of life [1, 3–5]. Nocturnal leg cramps are particularly common among older adults, although they can occur in all decades of life [1–3, 5–7], and among pregnant women [1, 8–10]. Few data are available in primary care, but a recent French study estimated their prevalence in patients above the age of 60 years (n = 516) to be 46% [7], slightly lower than in an older study of US veterans (n = 515) which showed that 56% suffered from nocturnal leg cramps [11].
There is no consensus about the pathophysiology and aetiology of nocturnal leg cramps, but this condition probably covers three distinct entities: (1) idiopathic leg cramps, the most frequent entity, (2) pregnancy related leg cramps, for which potential contributing factors may include low levels of certain minerals (for example magnesium), extracellular fluid volume depletion and prolonged sitting or inappropriate leg position during sedentary activity, and (3) secondary leg cramps related to other medical conditions (neurological, endocrine, metabolic, vascular, medication-related, toxic and congenital) [1, 2, 7]. Indeed, associations with various conditions have been reported. However, some of them may represent non-causal associations. Moreover, since nocturnal leg cramps are frequent and poorly defined in many studies, associations with common conditions may have occurred by chance [3].
Quinine, the only treatment proven to be (modestly) effective, may result in serious side effects and is no longer recommended for routine use [1, 3, 12–16]. Unlike quinine, magnesium has a favourable side-effect profile and has become a mainstay for the treatment of nocturnal leg cramps in Europe [1]. Unfortunately, we recently showed in a systematic review that magnesium does not seem to be more effective than placebo in the treatment of these cramps, except possibly in pregnant women [17]. Studies of the effectiveness of prophylactic stretching in preventing nocturnal leg cramps have provided conflicting results [18–20]. Patients report trying a large range of other unproven treatments, which suggests the need to build stronger therapeutic evidence for this common condition [21].
One step towards this aim is to gain a better understanding of the characteristics of nocturnal leg cramps in primary care patients, which is essential for researchers planning future trials of interventions to treat these cramps. Therefore, we sought to determine their main features (number, duration, severity and sleep disturbance), and to assess whether these features are associated with patient characteristics, in a sample of patients visiting primary care physicians. In contrast to earlier observational surveys, we used a prospective design to provide a more accurate picture of the burden of this disorder in primary care.
We followed the STROBE recommendations for the reporting of this prospective observational study. A convenience sample of 20 community-based primary care physicians who practiced in the canton of Geneva and were members of the professional organisation of Geneva-based physicians were recruited by post and asked to enrol up to 20 consecutive patients coming to the practice for a planned consultation. The patient eligibility criteria were an age older than 50 years, able to understand and write French, and having suffered from nocturnal leg cramps during the previous three months. The definition of nocturnal leg cramps used as an eligibility criterion for inclusion in the study was any cramp (i.e. a sudden, involuntary and painful sensation associated with muscle hardness or tightness, indicating a strong muscle contraction) in the legs or feet occurring during sleep or while at rest [3, 7, 22]. Patients were not eligible for the study if they had an unplanned consultation, if they were suffering from a terminal illness or from disorders affecting their ability to consent, if they were not able to speak and write French, or if they had no contact phone number.
Data collection took place from January 2015 until June 2016. One of the study investigators (HM) met all participating physicians to inform them about the aims and the procedures of the study, and to provide them with the study documents (physician’s information sheet and patient’s daily log, questionnaire, information and consent forms) and prepaid postage envelopes. Patients were screened during the consultation and asked to provide oral consent to be contacted further by the research team. They were given a questionnaire to complete at home. The questionnaire asked about their socio-demographic characteristics (age, sex, nationality, marital status and work status), their estimated health status in response to the question “in general, would you say that your health is: excellent, very good, good, moderate or poor?”, their number of consultations in the last six months (for whatever reason), their health problems requiring medication, their current medication, and whether they had taken a treatment against nocturnal leg cramps in the past. In addition, they were asked to use the daily log for two weeks to record daily (1) the number of cramps, (2) their mean duration (in minutes), (3) their mean severity (on a 10-cm long visual analogue scale going from “no pain” to the “worst possible pain”), and 4) the mean level of sleep disturbance during nights when they had cramps (on a 10-cm long visual analogue scale going from “no sleep disturbance” to “large sleep disturbance”). When using the visual analogue scale, patients were asked to indicate a position along a continuous line between the two end-points. They were then asked to return the completed documents using the prepaid postage envelope.
Shortly after the consultation and at weeks 1 and 2 research assistants phoned the patients to provide renewed information about the study and to ask them to confirm their consent to participation (and if so to sign and send back the consent form). The research assistants asked the patients whether they had questions and/or difficulties in completing the questionnaire and the daily log. They also asked whether the documents were completed correctly (at weeks 1 and 2), and in the third phone call they reminded patients to return all completed documents by post.
The research assistants were seven medical students who had been trained to conduct the phone interviews. They were also trained by one of the study investigators (HM) to differentiate during each phone interview between nocturnal leg cramps and other frequent sleep-related disorders (restless legs syndrome, periodic limb movement disorder, peripheral neuropathy and peripheral vascular disease). The typical features of each of these disorders were carefully highlighted to the research assistants.
The patient questionnaire and the daily log were pretested in four primary care practices to identify any difficulties patients might face when completing the questionnaire and the log.
All collected data remained confidential. Tacit consent was presumed from the physicians if they agreed to participate. In contrast, we obtained written informed consent from all patients. The research protocol was approved by the Research Ethics Committee of Geneva (ref: 14-232).
We used frequency tables to describe categorical variables, means ± standard deviation to summarise continuous socio-demographic variables and medians (interquartile range) to summarise the characteristics of cramps (number, severity, duration, and sleep disturbance due to cramps).
The day-to-day number of cramps for every patient was modelled by a generalised mixed effects model (Poisson) with a random effect for the intercept at the patient level. The other potential covariates, measured at baseline, were taken as fixed effects. They were first considered one by one in univariate models, and then incorporated into a multivariate model whenever the associated p-value was lower than 0.15. All p-values less than 0.05 were considered significant evidence against the tests’ null hypotheses. The association between the number and the severity of cramps, and the number of cramps and sleep disturbance, was modelled by a linear mixed effects model with a random effect for the intercept at the patient level.
We estimated that a sample size of 110 patients would be adequate to detect an effect size of 0.65 (weekly number of cramps) when comparing two groups with different characteristics and the same number of patients using a Wilcoxon-Mann-Whitney test and with Type I and II error rates both set at 5%. This sample size was estimated with G*Power version 3.1.9.2, Universität Kiel, Germany. All other analyses were done with R version 1.0.143, R Foundation for Statistical Computing, Vienna, Austria, and TIBCO Spotfire S+ 8.1 for Windows, TIBCO Software Inc, Palo alto, CA, USA.
Twenty primary care physicians (male: 55%; mean age: 46) agreed to enrol patients for the study. Thirteen physicians were in solo practice, four in duo practice and three in trio practice. The study was proposed to 550 consecutive patients suffering from cramps. Of these, 42% (n = 233) agreed to be contacted for the study, 55% of whom (n = 129) formally consented to participate in the study and completed the questionnaire and daily journal (follow-up rate: 100%). Each physician recruited a mean number of 6.5 patients (min 1, max 26).
Table 1 presents the patients’ main socio-demographic characteristics. They were predominantly male (67%) and were on average 71 years old (SD 9). They used a mean number of 3.7 medications to treat a range of different medical conditions. Half the patients reported having already used a treatment against nocturnal leg cramps in the past.
Table 1 Patient characteristics (n = 129).
| Characteristics | n* (%) | Mean ± standard deviation | |
|---|---|---|---|
| Men (n = 129) | 86 (66.7) | ||
| Age (years) (n = 128) | 70.9 ± 9.3 | ||
| <65 | 37 (28.9) | ||
| 65–75 | 47 (36.7) | ||
| >75 | 44 (34.4) | ||
| Marital status (n = 126) | |||
| Single | 11 (8.7) | ||
| Married | 76 (60.3) | ||
| Divorced or separated | 23 (18.3) | ||
| Widowed | 16 (12.7) | ||
| Work status (n = 126) | |||
| Occupational activity | 27 (21.4) | ||
| Retired | 78 (61.9) | ||
| Recipient of unemployment or invalidity insurance | 6 (4.8) | ||
| Other (mainly housewife/husband and without employment) | 15 (11.9) | ||
| General health status (n = 126) | |||
| Excellent or very good | 36 (28.6) | ||
| Good | 72 (57.1) | ||
| Moderate or poor | 18 (14.3) | ||
| Number of consultations in the last six months (n = 122) | 3.3 ± 2.4 | ||
| 1–2 | 56 (45.9) | ||
| 3–4 | 39 (32.0) | ||
| ≥5 | 27 (22.1) | ||
| Medical condition requiring medication (n = 129) | |||
| Hypertension | 53 (41.1) | ||
| Dyslipidaemia | 26 (20.2) | ||
| Diabetes | 8 (6.2) | ||
| Sleep disturbance | 25 (19.4) | ||
| Depression | 24 (18.6) | ||
| Hypothyroidism | 10 (7.8) | ||
| Number of current drugs (n = 128) | 3.7 ± 2.8 | ||
| 0–1 | 31 (24.2) | ||
| 2–3 | 38 (29.7) | ||
| ≥4 | 59 (46.1) | ||
| Previous cramps treatment (n = 113) | 58 (51.3) | ||
| Current drug treatment (n = 129) | |||
| Diuretics | 12 (9.3) | ||
| Other antihypertensive drugs | 53 (41.1) | ||
| Lipid-lowering drugs | 26 (20.2) | ||
| Aspirin, clopidogrel and/or anticoagulants | 31 (24.0) | ||
| Antidiabetic drugs | 8 (6.2) | ||
| Levothyroxine | 10 (7.8) | ||
| Pain drugs | 69 (53.5) | ||
| Antidepressants | 24 (18.6) | ||
| Benzodiazepine sleeping pills | 16 (12.4) | ||
| Other sleeping pills | 9 (6.7) | ||
| Magnesium | 32 (24.8) | ||
| Vitamins and/or iron (except calcium and vitamin D) | 17 (13.2) | ||
| Calcium and/or vitamin D | 40 (31.0) | ||
| Proton pump inhibitors | 25 (19.4) | ||
| Oestrogens and/or progestins | 4 (3.1) | ||
* n = number with factor considered; denominators do not add up to 129 because of missing values
Outcomes (i.e., the main features of the 848 cramps recorded prospectively during the two-week follow-up of the 129 patients) are shown in Table 2. Figures 1 and 2 present these data in graphic form (box plots and a contour plot, respectively) to facilitate data visualisation. There were relatively few cramps recorded per patient (median number per week: 2), and 16 patients (12%) did not report any cramps during the study period. However, 40 patients (31%) reported more than three cramps per week. In addition, cramps were reported to be relatively mild (median severity index: 0.7/10), their duration was short (median: 0.4 min) and they were associated with only mild sleep disturbances (median severity index: 0.8/10). There was no association between the daily number and the severity of cramps (correlation = 0.04; p-value t-test = 0.304), but the daily number of cramps was associated with sleep disturbance (correlation = 0.15; p-value t-test = 0.001).
Table 2 Main features of patients’ cramps (n = 129 patients).
| Characteristics | % | Median (IQR) | Range | |
|---|---|---|---|---|
| Number of cramps per patient, per week | 2.0 (3.0) | 0–32 | ||
| 0 | 12.4 | |||
| 0.5–1 | 26.4 | |||
| 1.5–2 | 17.8 | |||
| 2.5–3 | 12.4 | |||
| >3 | 31.0 | |||
| Severity index of cramps recorded on numerical scale* | 0.7 (1.5) | 0.0–8.6 | ||
| 0.0 to <0.5 | 44.6 | |||
| 0.5 to <1.0 | 17.4 | |||
| 1.0 to <2.0 | 21.5 | |||
| 2.0 to <6.0 | 15.7 | |||
| 6.0 to 10 | 0.8 | |||
| Duration of cramps in minutes* | 0.4 (1.0) | 0.0–10.9 | ||
| 0.0 to <0.5 | 51.9 | |||
| 0.5 to <1.0 | 19.4 | |||
| 1.0 to <2.0 | 12.4 | |||
| 2.0 to <6.0 | 13.9 | |||
| >6.0 | 2.3 | |||
| Sleep disturbances due to cramps index recorded on a numerical scale* | 0.8 (0.9) | 0.0–8.7 | ||
| 0.0 to <0.5 | 56.6 | |||
| 0.5 to <1.0 | 19.4 | |||
| 1.0 to <2.0 | 13.2 | |||
| 2.0 to <6.0 | 10.1 | |||
| >6.0 | 0.8 |
IQR = interquartile range * measured as the average number per patient over two weeks
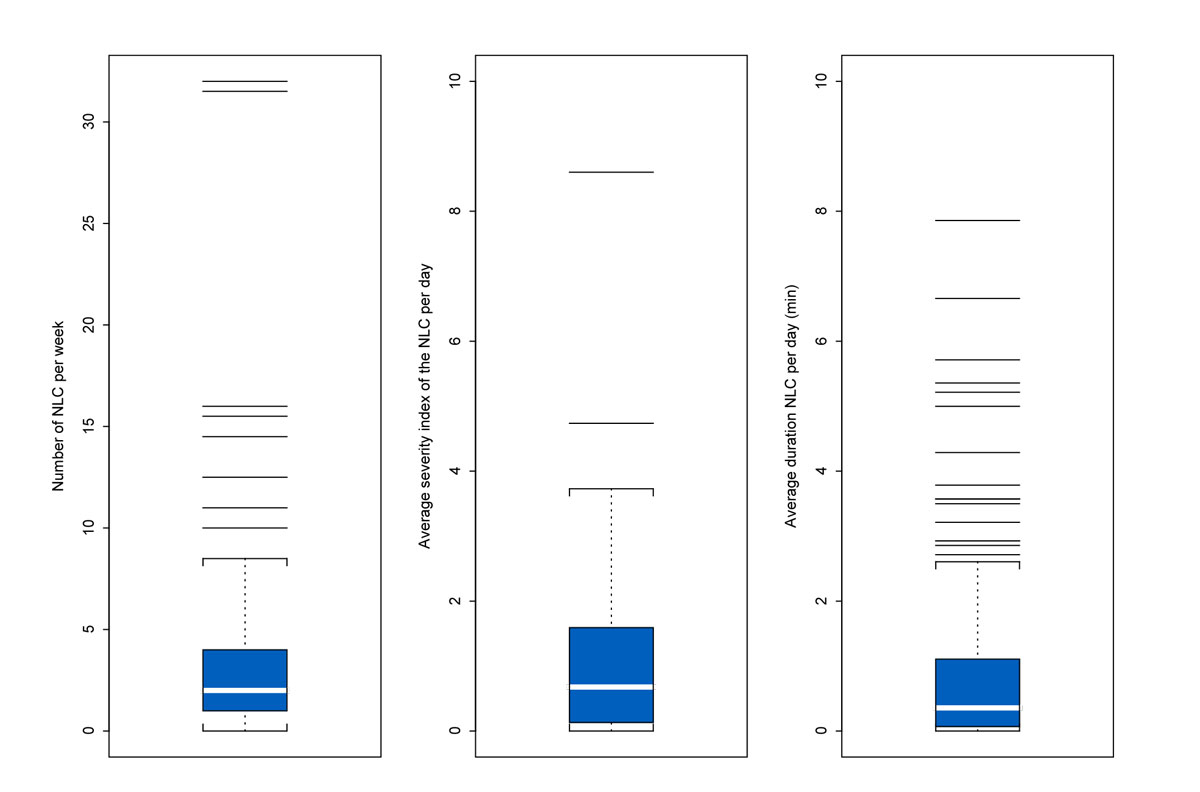
Figure 1 Number of nocturnal leg cramps (NLC) per week, average severity index per day, and average duration in minutes per day per patient (n = 129).
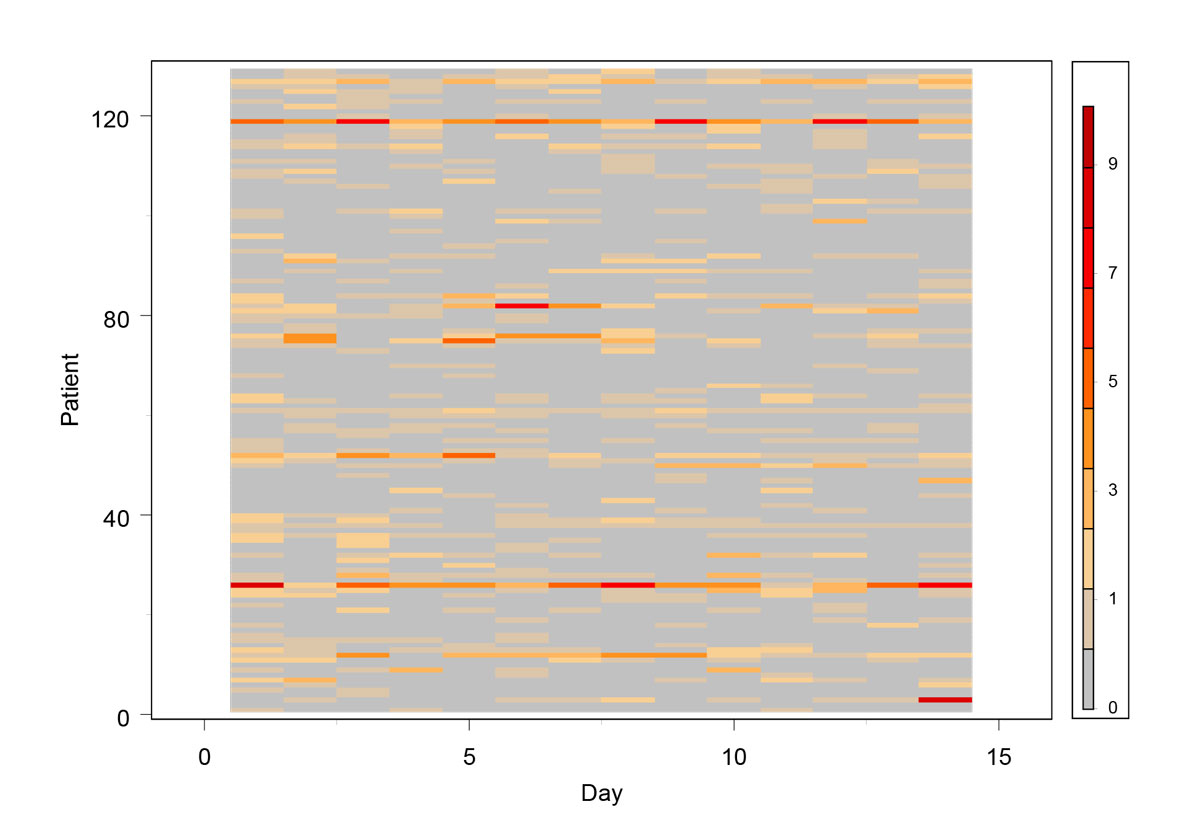
Figure 2 Contour plot of the number of nocturnal leg cramps per day, day by day for every patient (n = 129).
The median number of cramps per week was associated with work status (2.5 for retired vs. 1.3 for professionally active), the median severity index was associated with gender (0.8/10 for male vs. 0.4/10 for female) and the median duration of cramps was associated with the number of different types of medication (0.7 min for ≥4 drugs vs. 0.1 min for <4 drugs). There was no evidence of other associations between cramp features and patient characteristics.
Table S1 in appendix 1 lists the types of medication used by the patients and shows the median number of cramps per week, separated into two groups (users and non-users). Most drugs were grouped into drug classes due to small numbers. The median number of cramps per week was not associated with the type of medication, except for calcium and vitamin D (2.8 for users vs 1.5 for non-users).
Table 3 shows the unadjusted and adjusted associations between the number of cramps per day and patient characteristics. Multivariate analysis showed that older age and previous cramp treatment were associated with more cramps per day, while the use of magnesium and/or psychotropic drugs was associated with fewer cramps per day.
Table 3 Unadjusted and adjusted association between the number of cramps per day and patient characteristics (n = 129).
| Characteristics | Number of additional cramps: parameter λ Poisson model (e λ and 95% confidence interval) | p-value | Multivariate* | |
|---|---|---|---|---|
| Number of additional cramps: parameter λ Poisson model (e λ and 95% confidence interval) | p-value | |||
|
Men
Reference group: women |
−0.1174 0.889 (0.726–1.089) |
0.2554 | ||
|
Age group (years)
Reference group: <65 |
<0.0001† | <0.0001† | ||
| 65–75 | +0.5309 1.700 (1.310–2.207) |
+0.4070 1.502 (1.137–1.985) |
||
| >75 | +0.7050 2.024 (1.566–2.616) |
+0.7488 2.114 (1.602–2.791) |
||
|
Separated, widow, single
Reference group: married |
−0.2978 0.742 (0.609–0.904) |
0.0030† | −0.0664 0.941 (0.772–1.147) |
0.4593 |
|
Excellent or very good general health status
Reference group: bad, poor, good |
−0.0579 0.943 (0.763–1.167) |
0.5924 | ||
|
≥3 consultations in the last six months
Reference group: <3 |
+0.0316 1.032 (0.850–1.253) |
0.1879 | ||
|
≥4 current drugs
Reference group: ≤3 drugs |
+0.1981 1.219 (1.013–1.467) |
0.0359† | +0.0958 1.110 (0.733–1.127) |
0.1471 |
|
Previous cramp treatment
Reference group: no previous cramp treatment |
+0.8052 2.237 (1.816–2.755) |
<0.0001† | +0.6265 1.871 (1.523–2.230) |
<0.0001† |
| Medical condition | ||||
| Hypertension | −0.0287 0.972 (0.803–1.175) |
0.7677 | ||
| Dyslipidaemia | −0.0820 0.921 (0.726–1.169) |
0.4991 | ||
| Depression | −0.2150 0.807 (0.625–1.041) |
0.0990 | 0.1449 1.156 (0.817–1.635) |
0.4105 |
| Current treatment | ||||
| Anti-hypertensive drugs | −0.0287 0.972 (0.803–1.175) |
0.7677 | ||
| Diuretics | −0.2656 0.769 (0.539–1.098) |
0.1480 | −0.1103 0.896 (0.618–1.297) |
0.2333 |
| Other anti-hypertensive drugs | −0.0287 0.918 (0.803–1.175) |
0.7677 | ||
| Lipid-lowering drugs | −0.0820 0.921 (0.726–1.169) |
0.4991 | ||
| Pain drugs | −0.0273 0.973 (0.807–1.173) |
0.7748 | ||
| Psychotropic drugs | −0.2650 0.767 (0.628–0.937) |
0.0095† | −0.3062 0.736 (0.556–0.976) |
0.0326† |
| Magnesium | −0.3089 0.734 (0.591–0.912) |
0.0052† | −0.3205 0.726 (0.571–0.923) |
0.0052† |
| Calcium and/or vitamin D | +0.2178 1.243 (1.023–1.512) |
0.0289† | +0.0746 1.077 (0.869–1.335) |
0.4856 |
* Adjusted by age group, civil status, number of drugs, previous cramp treatment, use of diuretics, psychotropic drugs, magnesium, and calcium and/or vitamin D † p-value less than 0.05
In this sample of primary care patients suffering from nocturnal leg cramps, the median number of cramps per week was moderate (two per week). Cramps were generally mild and of short duration, leading only to mild or moderate sleep disturbances. In multivariate analysis, older age and previous cramp treatment were associated with more cramps per day, while the use of magnesium and/or psychotropic drugs was associated with fewer cramps per day.
We showed that patients had relatively few cramps in general (only half of patients had more than two cramps per week), despite the fact that only patients above the age of 50 years who had already suffered from nocturnal leg cramps during the previous three months were enrolled. Our results are in line with a recent study (n = 516) in which only a quarter of patients with cramps had them as frequently as once to three times a week [7]. Our results are also consistent with those of a relatively old survey carried out in the UK (n = 233) which showed that, despite an overall prevalence of nocturnal leg cramps of 37% (and even 54% in patients >80 years old), 60% had cramps less than three times per week [5]. This highlights that although many elderly patients suffer from cramps [2, 3, 5–7, 23], the number of cramps per week is relatively low.
We could not exclude a certain degree of bias due to underreporting, even though the study was of short duration (two weeks) and all participating patients were reminded on three occasions to keep a log of their cramps. In addition, our inclusion criterion (at least one nocturnal leg cramp in the previous three months) may not have been sufficiently restrictive, thus favouring the inclusion of patients who only very occasionally suffered from cramps. However, we believe that our study provides a representative picture of the (relatively low) number of nocturnal leg cramps in many patients reporting cramps in primary care.
In addition to showing that most patients had relatively few cramps, we also showed that these cramps were generally mild (0.7/10) and of short duration (0.4 min), leading to only mild sleep disturbances (0.8/10). These results contrast with those of two other studies. In a study involving 233 patients suffering from nocturnal leg cramps, the episodes lasted for 9 min on average, 24% of patients reported that their cramps were “very distressing”, and 26% that they caused a “major nuisance”. [5] Patients in this study were recruited from only one practice, which may have favoured a selection bias. In an Australian case-control study (80 cases, 80 age- and sex-matched controls recruited through advertisements on regional television, radio and newspaper), nocturnal leg cramps were associated with sleep disturbances and a lower health-related quality of life [4]. In this case again, the recruitment mode may have favoured a selection bias.
Whereas the association between age and the prevalence of cramps is well known [1, 2, 5, 6], we also found an association between age and the number of cramps. Age appears to be strongly related to the prevalence and number of nocturnal leg cramps per day, probably because the potential contributing factors of these cramps, such as low levels of certain minerals, extracellular fluid volume depletion and sedentary activity, often occur (and co-occur) in elderly patients [1, 2]. In contrast, the absence of any association between gender and the number of cramps is in line with several previous studies in which no association was found between gender and the prevalence of nocturnal leg cramps [5, 7].
We found that patients who had already used drugs to treat their cramps in the past had a higher number of cramps per day. These patients may have previously used treatments precisely because they had suffered from a relatively high number of cramps in the past.
The fact that patients taking magnesium had fewer cramps per day is probably because magnesium has become a mainstay in the treatment of nocturnal leg cramps (although its benefit is more likely related to a placebo effect) [17]. More surprisingly, we also found a negative association in multivariate analyses between the use of psychotropic drugs and the number of cramps. Further research is needed to confirm this finding. However, we could hypothesise that some patients treated for psychiatric conditions may have better control of their disease than patients not taking psychotropic drugs. Since it has been shown that some psychiatric conditions may be related to nocturnal leg cramps (for example, nocturnal leg cramps were highly associated with depression in a study exploring associations with a wide range of medical disorders), the use of psychotropic drugs may therefore be associated with fewer cramps per day.
Although cramps may arise as a side-effect of many drugs, the overall association between drugs and nocturnal leg cramps seems to be relatively weak [2]. Even diuretics, a potential aetiological factor due to electrolytic abnormalities, have not been shown to be associated with nocturnal leg cramps in evidence-based reviews [2]. Garrison et al., however, found that new prescriptions for quinine were more common in the year following the introduction of diuretics [24]. In the recent study by Maisonneuve et al., there were no differences in medication, including diuretics, between patients suffering from nocturnal leg cramps and a reference population [7].
Magnesium has a favourable side-effect profile, but unfortunately it seems no better than placebo in treating nocturnal leg cramps [1, 17, 25]. Therefore, and because the median number of cramps and their repercussions were relatively moderate in our study, it seems understandable, when patients request treatment, to continue to prescribe drugs such as magnesium. Alternatively, non-pharmacological treatments (such as leg stretching before sleep) could also be recommended as first-line therapy in these patients. However, some patients suffer from a higher number of cramps (30% in our study) and/or cramps seriously affecting their quality of life. These patients would probably benefit from a more effective treatment. More research is therefore warranted to develop new interventions with real therapeutic benefits.
In contrast to earlier observational surveys, we used a longitudinal design, asking participants to prospectively record the number and the main characteristics of their cramps in a daily log. We believe that our findings thus provide us with a more detailed and accurate picture of the burden of this disorder in primary care. In addition, all participating patients were personally contacted by research assistants on three occasions (at Weeks 0, 1 and 2) to improve the quality of data collection.
However, some limitations must be pointed out and kept in mind when considering our results. The patients were recruited in a single region (Geneva area), and the findings cannot necessarily be generalised to other regions in Switzerland or Europe. Selection bias cannot be completely excluded. Indeed, physicians (and not the study investigators) were asked to report whether patients declined to participate, and we therefore cannot be sure that no eligible patients were missed. The study was proposed to 550 consecutive patients with cramps, 42% of them agreed to be contacted for the study and 55% of these formally consented to participate and completed the questionnaire and daily journal. Therefore, we cannot exclude that our sample may have been biased towards patients who were more concerned by cramps. If this were the case, it would only highlight our findings that the burden of disease related to nocturnal leg cramps may not be as severe as previously described. We did not collect any data on patients who declined participation, and therefore we could not assess potential differences between responders and non-responders. Although the number of cramps recorded was high (n = 848), our data were based on a relatively small sample size (number of patients: 129). The research assistants were trained to differentiate between nocturnal leg cramps and other sleep related disorders. However, some cramp episodes could have been erroneously identified as nocturnal leg cramps. Only patients who had suffered from cramps in the previous three months before the start of the study were included. Factors associated with the number of cramps in this group of patients may therefore not be associated with the occurrence of cramps (vs. no cramps) per se. We only recorded medical conditions requiring medication. Health problems without medication at the time of the study were not recorded, and this may have led to some degree of information bias. Finally, we used self-administered questionnaires and daily logs as well as telephone interviews to collect our study data. These methods raise the issue of underreporting and/or measurement error.
Though relatively common in primary care, in particular in older patients, the disease burden of nocturnal leg cramps does not appear to be as severe and overwhelming as expected so far. As some patients suffer from a relatively high number of cramps and/or cramps seriously affecting their quality of life, future research should focus on the development of new approaches with real therapeutic benefits to treat these patients.
Table S1 Current drug treatment, and number of cramps per week (n = 129)*; this table compares the median number of cramps per week in patients using and not using the drug in question.
| Characteristics | Number of patients using each of these drugs at the time of the study |
Number of cramps per week
median (IQR) |
p-value | |
|---|---|---|---|---|
| Not using this drug | Using this drug | |||
| Anti-hypertensive drugs | 53 | 1.5 (3.0) | 2.5 (4.0) | 0.480 |
| Diuretics | 12 | 2.0 (3.5) | 2.3 (1.9) | 0.747 |
| Non-diuretics | 53 | 1.5 (3.0) | 2.5 (4.0) | 0.480 |
| Lipid-lowering drugs | 26 | 2.0 (3.3) | 1.5 (2.0) | 0.610 |
| Aspirin, clopidogrel and/or anticoagulants | 31 | 1.5 (3.4) | 2.5 (3.5) | 0.066 |
| Antidiabetic drugs | 8 | 2.0 (3.0) | 1.5 (3.0) | 0.324 |
| Levothyroxine | 10 | 1.5 (3.0) | 3.0 (5.3) | 0.226 |
| Pain drugs | 69 | |||
| Paracetamol, anti-inflammatory drugs, codeine, tramadol and/or morphine | 18 | 2.0 (3.3) | 2.0 (3.1) | 0.436 |
| …taken occasionally | 49 | 1.5 (3.9) | 2.5 (3.0) | 0.184 |
| Gabapentin and/or pregabalin | 4 | 2.0 (3.0) | 2.5 (1.5) | 0.478 |
| Muscle relaxants | 6 | 2.0 (3.3) | 0.8 (0.9) | 0.219 |
| …taken occasionally | 3 | 1.8 (3.0) | 3.0 (1.0) | 0.275 |
| Chondroitin sulphate | 11 | 2.0 (3.4) | 2.0 (1.8) | 0.732 |
| Psychotropic drugs | 47 | 2.0 (3.5) | 1.5 (3.0) | 0.727 |
| Anti-depressants | 24 | 2.0 (3.0) | 1.5 (2.8) | 0.691 |
| Benzodiazepine sleeping pills | 16 | 2.0 (3.0) | 1.3 (4.1) | 0.643 |
| …taken occasionally | 14 | 2.0 (3.8) | 2.5 (1.0) | 0.363 |
| Other sleeping pills | 9 | 2.0 (3.1) | 1.5 (2.5) | 0.673 |
| …taken occasionally | 7 | 2.0 (3.4) | 2.5 (2.3) | 0.942 |
| Magnesium | 32 | 2.0 (3.5) | 1.5 (2.8) | 0.184 |
| …taken occasionally | 8 | 1.8 (3.0) | 3.0 (3.5) | 0.299 |
| Vitamins and/or iron (except calcium and vitamin D) | 17 | 1.5 (3.0) | 2.5 (3.5) | 0.427 |
| Calcium and/or vitamin D | 40 | 1.5 (3.0) | 2.8 (3.6) | 0.023 † |
| Proton pump inhibitors | 25 | 2.0 (3.0) | 1.5 (4.0) | 0.829 |
| …taken occasionally | 9 | 1.8 (3.0) | 3.0 (3.5) | 0.501 |
| Oestrogens and/or progestins | 4 | 2.0 (3.0) | 4.5 (1.8) | 0.139 |
* The main features of cramps are computed by patient, per week. Kruskal Wallis tests were used to compare the subgroups. † p-value less than 0.05
We would like to warmly thank all the doctors and patients who participated in this study, as well as Asmaa Dhina, Melody Favre, Romain Guemara, Dominique Ricard-Gauthier, Leandro Sanz, Farana Haque and Zoe Koul, the medical students who conducted the phone interviews.
This project was supported by institutional funding from the Faculty of medicine, University of Geneva.
Provisional – author forms not received
No potential conflict of interest relevant to this article was reported.
1 Monderer RS , Wu WP , Thorpy MJ . Nocturnal leg cramps. Curr Neurol Neurosci Rep. 2010;10(1):53–9. doi:.https://doi.org/10.1007/s11910-009-0079-5
2 Allen RE , Kirby KA . Nocturnal leg cramps. Am Fam Physician. 2012;86(4):350–5.
3 Rabbitt L , Mulkerrin EC , O’Keeffe ST . A review of nocturnal leg cramps in older people. Age Ageing. 2016;45(6):776–82. doi:.https://doi.org/10.1093/ageing/afw139
4 Hawke F , Chuter V , Burns J . Impact of nocturnal calf cramping on quality of sleep and health-related quality of life. Qual Life Res. 2013;22(6):1281–6. doi:.https://doi.org/10.1007/s11136-012-0274-8
5 Naylor JR , Young JB . A general population survey of rest cramps. Age Ageing. 1994;23(5):418–20. doi:.https://doi.org/10.1093/ageing/23.5.418
6 Grandner MA , Winkelman JW . Nocturnal leg cramps: Prevalence and associations with demographics, sleep disturbance symptoms, medical conditions, and cardiometabolic risk factors. PLoS One. 2017;12(6):e0178465. doi:.https://doi.org/10.1371/journal.pone.0178465
7 Maisonneuve H , Chambe J , Delacour C , Muller J , Rougerie F , Haller DM , et al. Prevalence of cramps in patients over the age of 60 in primary care : a cross sectional study. BMC Fam Pract. 2016;17(1):111. doi:.https://doi.org/10.1186/s12875-016-0509-9
8 Hensley JG . Leg cramps and restless legs syndrome during pregnancy. J Midwifery Womens Health. 2009;54(3):211–8. doi:.https://doi.org/10.1016/j.jmwh.2009.01.003
9 Salvatore CA . Leg cramp syndrome in pregnancy. Obstet Gynecol. 1961;17:634–9.
10 Nygaard IH , Valbø A , Pethick SV , Bøhmer T . Does oral magnesium substitution relieve pregnancy-induced leg cramps? Eur J Obstet Gynecol Reprod Biol. 2008;141(1):23–6. doi:.https://doi.org/10.1016/j.ejogrb.2008.07.005
11 Oboler SK , Prochazka AV , Meyer TJ . Leg symptoms in outpatient veterans. West J Med. 1991;155(3):256–9.
12 Young G . Leg cramps. BMJ Clin Evid. 2009;Mar 26.
13 Katzberg HD , Khan AH , So YT . Assessment: symptomatic treatment for muscle cramps (an evidence-based review): report of the therapeutics and technology assessment subcommittee of the American academy of neurology. Neurology. 2010;74(8):691–6. doi:.https://doi.org/10.1212/WNL.0b013e3181d0ccca
14 Man-Son-Hing M , Wells G , Lau A . Quinine for nocturnal leg cramps: a meta-analysis including unpublished data. J Gen Intern Med. 1998;13(9):600–6. doi:.https://doi.org/10.1046/j.1525-1497.1998.00182.x
15 Man-Son-Hing M , Wells G . Meta-analysis of efficacy of quinine for treatment of nocturnal leg cramps in elderly people. BMJ. 1995;310(6971):13–7. doi:.https://doi.org/10.1136/bmj.310.6971.13
16 Hogan DB . Quinine: not a safe drug for treating nocturnal leg cramps. CMAJ. 2015;187(4):237–8. doi:.https://doi.org/10.1503/cmaj.150044
17 Sebo P , Cerutti B , Haller DM . Effect of magnesium therapy on nocturnal leg cramps: a systematic review of randomized controlled trials with meta-analysis using simulations. Fam Pract. 2014;31(1):7–19. doi:.https://doi.org/10.1093/fampra/cmt065
18 Garrison SR . Prophylactic stretching is unlikely to prevent nocturnal leg cramps. J Physiother. 2014;60(3):174. doi:.https://doi.org/10.1016/j.jphys.2014.05.004
19 Hallegraeff JM , van der Schans CP , de Ruiter R , de Greef MHG . Stretching before sleep reduces the frequency and severity of nocturnal leg cramps in older adults: a randomised trial. J Physiother. 2012;58(1):17–22. doi:.https://doi.org/10.1016/S1836-9553(12)70068-1
20 Coppin RJ , Wicke DM , Little PS . Managing nocturnal leg cramps--calf-stretching exercises and cessation of quinine treatment: a factorial randomised controlled trial. Br J Gen Pract. 2005;55(512):186–91.
21 Lorenzo M , Schaeffer M , Haller DM , Maisonneuve H . Treatment of nocturnal leg cramps by primary care patients over the age of 60. Fam Pract. 2018;35(1):29–33. doi:.https://doi.org/10.1093/fampra/cmx062
22 Hallegraeff J , de Greef M , Krijnen W , van der Schans C . Criteria in diagnosing nocturnal leg cramps: a systematic review. BMC Fam Pract. 2017;18(1):29. doi:.https://doi.org/10.1186/s12875-017-0600-x
23 Abdulla AJ , Jones PW , Pearce VR . Leg cramps in the elderly: prevalence, drug and disease associations. Int J Clin Pract. 1999;53(7):494–6.
24 Garrison SR , Dormuth CR , Morrow RL , Carney GA , Khan KM . Nocturnal leg cramps and prescription use that precedes them: a sequence symmetry analysis. Arch Intern Med. 2012;172(2):120–6. doi:.https://doi.org/10.1001/archinternmed.2011.1029
25 Roguin Maor N , Alperin M , Shturman E , Khairaldeen H , Friedman M , Karkabi K , et al. Effect of Magnesium Oxide Supplementation on Nocturnal Leg Cramps: A Randomized Clinical Trial. JAMA Intern Med. 2017;177(5):617–23. doi:.https://doi.org/10.1001/jamainternmed.2016.9261
PS, DH and HM were involved in the conception of the study and data interpretation. PS drafted the first version of the manuscript. BC was involved in the data analysis and data interpretation. All authors read and approved the final manuscript. BC can be contacted for access to the dataset underlying the current analysis.
This project was supported by institutional funding from the Faculty of medicine, University of Geneva.
Provisional – author forms not received
No potential conflict of interest relevant to this article was reported.