Home visits made by general practitioners in the canton of Vaud between 2006 and 2015
DOI: https://doi.org/10.4414/smw.2019.20037
Yolanda K.
Mueller, Stéphane
David, Christine
Cohidon, Isabella
Locatelli, Nicolas
Senn
Department of Family Medicine / Center for Primary Care and Public Health (Unisanté), University of Lausanne, Switzerland
Summary
AIM OF THE STUDY
Although physicians’ home visits are highly valued by patients, and are among the measures that contribute to maintaining elderly patients at home, their number is decreasing worldwide. We aimed to describe the trends in home visits made by general practitioners (GPs) in the canton of Vaud in Switzerland between 2006 and 2015, and to explore their associated characteristics.
METHODS
We retrospectively analysed billing data from family physicians (internists, generalists and practicing physicians) transmitted to the cantonal trust centre between 2006 and 2015. We explored physician and patient characteristics, first over the entire 10-year study period and then averaged by year. To explore factors associated with the number of home visits, we fitted a mixed effect negative binomial regression of the annual number of home visits per physician.
RESULTS
Over ten years, 631 physicians billed a total of 451,634 home visits, of which 19.8% (n = 89,966) were emergency visits, and 9.7% (n = 43,915) were over the weekend. Home visits represented 2.5% of all consultations. Although the average annual number of physicians doing home visits remained stable at around 400, the mean annual number of visits per physician decreased from 125 in 2006 to 75 in 2015, resulting in a 40% decline in the absolute number of visits. Male physicians undertook more home visits than their female counterparts did, although the difference diminished over time. Visits to elderly patients (65+) represented 84.2% of the home visits.
CONCLUSIONS
Although most physicians in the canton of Vaud continue to visit patients at home, the overall number of home visits is declining. Most home visits consist of routine visits to elderly patients. Physicians’ gender, age and specialty are associated with the number of home visits. In the rapidly evolving context of an ageing population and the development of home care, physicians’ role in home care provision should be revised, taking into account patient expectations and current health system constraints.
Introduction
Population ageing is a major challenge for health systems, as they are confronted with an increase in the number of multimorbid and frail patients. In addition to the somatic challenges in the care of these patients, mental health [1–3] and social issues such as isolation and deprivation become increasingly important. Still, patients wish to remain at home as long as possible [4], which is also in line with current public health strategies, both to limit costs and because of the limited availability of institutional beds. In addition, palliative home care caters to the wishes of most patients when they are approaching end-of-life [5].
General practitioners’ (GPs’) home visits are an important component of home care [6]. By home visits we mean visits to a patient's home by professional personnel for the purpose of diagnosis and/or treatment. Reasons to undertake home visits are diverse, and include routine follow-up, emergency visits [7], palliative care [8, 9] and post-discharge follow-up [10] for patients that are usually unable to travel to the GP practice. GP home visits are highly valued by patients [4], and among the measures that contribute to maintaining elderly patients at home [11].
Indeed, regular home visits have been shown to reduce unnecessary emergency department visits and hospital admissions [12], reduce readmissions [13, 14], and prevent falls [15], functional decline and long-term institutionalisation [16]. GP home visits used to be the main mode of care delivery in Europe before the Second World War, but their number has since decreased progressively in all industrialised countries [17–22]. In Switzerland, most GPs do carry out home visits, but only 43% do so frequently (compared with 6% in the USA and 88% in the Netherlands, for example) [23]. Swiss GPs tend to do fewer home visits than their European counterparts [24, 25], and the mean weekly number of home visits per week has decreased from 7.7 in 1992 to 3.2 in 2012 [26]. In a population survey conducted in the canton of Vaud in Western Switzerland, only 36% of older individuals thought of GP home visits as easily accessible [27].
Various factors have been reported to influence the number of home visits [28]. These include factors at GP level (age, gender, personal preferences, workload), patient level (multimorbidity, age, psychosocial factors) and organisational level (practice location, practice type, financial aspects). In addition, both the health system and society have evolved in recent years, especially with respect to the development of home-based care and changing patterns of emergency care use (development of walk-in clinics and private companies specialising in home visits). Changes have also occurred in transportation (driving ability control policy for the elderly, evolution of public transport networks) which may have modified access to GP practices. Within this context, the aim of this study was to describe the trends in home visits made by GPs in the canton of Vaud over a period of ten years (2006–2015), and to explore patient and physician characteristics associated with the number of visits.
Material and methods
This is a retrospective analysis of billing data voluntarily transmitted by physicians to the cantonal trust centre (Centre de confiance de la Société Vaudoise de Médecine) between 2006 and 2015. The canton of Vaud is the most populous canton in French-speaking Switzerland, with a resident population of 708,177 in 2010 (study mid-period) and 540 general practitioners (general internal medicine specialists or practicing physicians) active in the ambulatory sector according to national statistics [29]. This project used anonymised data that did not contain personal health-related information. It was therefore not under the scope of the Swiss human research law and did not require formal ethical review.
Remuneration of Swiss GPs is based on a fee-for-service system. In addition, GPs can bill consultation time according to a unified payment system (Tarmed). Within this system, home visits can be identified by a specific tariff heading corresponding to transportation time. Visits to residential patients are included in these data and cannot be differentiated from the other visits. In addition, there is a separate heading for emergency visits, which are defined as pressing unscheduled visits, or visits that occur outside regular consultation time (evenings, nights and week-ends).
The dataset consisted of billing data from every physician that was either a general internal medicine specialist (title corresponding to five years of post-graduate training in Switzerland) or a practicing physician (title corresponding to three years of post-graduate training), and who had billed at least one consultation in the canton of Vaud between 2006 and 2015. Data from paediatricians were not included. The physicians’ variables were age, gender, specialty title, postal code, annual number of consultations, annual number of home visits and annual total duration of home visits. For each home visit, information was provided on the patient’s coded identifier, gender and age, the date, the amount and type of medical services billed, and whether the home visit was an emergency visit (defined as an unplanned visit that took place immediately after being requested by the patient or the patient’s “entourage”).
We first examined physician and patient characteristics for the entire 10-year study period. The total number of visits was categorised by day of the week and whether or not they were emergency visits. We then categorised the patients according to the number of visits per patient and explored factors associated with the number of visits. Hypothesis testing was based on a chi square test for categorical variables and Poisson regression for count variables.
We looked at the total number of visits, number of visits per GP and patient characteristics according to year. We calculated visit rates by dividing the number of visits by the resident population of the canton of Vaud. We observed the relative difference between 2006 and 2015 in the calculated indicators.
Finally, we further explored factors associated with the number of home visits per GP and their evolution over time, as this parameter showed the most variation. For this, we fitted a mixed effect negative binomial regression model of the annual number of home visits per physician, including a random intercept for each physician. Year, physician gender, physician age at baseline (2006) and physician specialty were the covariates. Linear, quadratic and cubic time effects were considered. Interactions between time and all the covariates were tested, and only the significant ones were kept. GPs who had billed more than 500 visits in at least one year were excluded in order to have a distribution of the outcome variable close to the chosen regression model, and because these were considered to be “frequent visitors” whose behaviour was likely to differ from that of other physicians. The fit of the model was assessed by comparing observed and predicted values according to year. In a sensitivity analysis, the model was rerun without the exclusion of “frequent visitors”.
Results
GP and patient characteristics, entire 2006–2015 period
Between 2006 and 2015, 631 physicians out of 688 (91.7%) billed at least one consultation (68.8% men, median age in 2010 52 years, IQR 42 to 60). Most held a specialist title either in general internal, general or internal medicine, while 10.3% (71/688) were medical practitioners. Overall, 87,062 patients received a total of 451,634 visits, which represented 2.5% of all consultations. One in five home visits (19.9%, 89,966/451,634; table 1) was billed as emergency visit, and 9.7% (43,915/451,634) took place over the weekend. More than half of patients (55.6%) received only a single visit, which was then mostly an emergency visit (in 71.2% of cases; table 1). The mean age of visit beneficiaries was 67.1 years (SD 23.2), with 58.7% of them women. Both age and proportion of women increased with the number of visits (p <0.001, table 1). Visits to older patients (65+) represented 84.3% of the total number of visits (380,469/451,333; age missing for 148 patients = 301 visits), and visits to very old patients (85+) represented 43.4% (n = 195,727).
Table 1 Number and proportion of patients, sex/gender, age, total number of home visits and number of emergency home visits, by category of number of visits per patient.
|
Patients
|
Women
|
Age in years
|
Total home visits
|
Emergency visits
|
|
n
|
Column %
|
n
|
Row %
|
Mean
|
Standard deviation
|
n
|
Column %
|
n
|
Row %
|
|
Number of home visits per patient
|
|
|
|
|
|
|
|
|
|
|
| A single home visit |
48,383 |
55.6 |
26,453 |
54.7 |
58.9 |
24.3 |
48,383 |
10.7 |
34,451 |
71.2 |
| 2 to 10 home visits |
28,661 |
32.9 |
17,734 |
61.9 |
75.5 |
18.2 |
113,638 |
25.2 |
32,921 |
29.0 |
| More than 10 home visits |
10,018 |
11.5 |
6,947 |
69.4 |
82.1 |
12.3 |
289,613 |
64.1 |
22,594 |
7.8 |
|
Total
|
87,062
|
100.0
|
51,134
|
58.7
|
67.1
|
23.2
|
451,634
|
100.0
|
89,966
|
19.9
|
|
p-value
|
|
|
<0.001*
|
|
<0.001†
|
|
|
|
<0.001*
|
|
Time trends
We analysed the variation over time in the number of consultations and patient characteristics between 2006 and 2015 in the canton of Vaud (table 2). There was a slight increase in the annual number of both consulting physicians (+5.7%) and physicians doing home visits (+5.8%), while the number of consultations per physician remained stable (−1.9%). However, the mean annual number of home visits per physician decreased from 125 (SD 165) in 2006 to 75 (SD 136) in 2015, resulting in a 36.9% decline in the absolute number of home visits. While the number of visits per patient remained stable (three per patient on average), the total number of beneficiaries decreased by 41.4% despite the fact that the resident population of the canton increased by 16.5%. The proportion of women among visit beneficiaries remained stable over time, but the proportion of patients aged 65+ increased from 66.7% to 76.5% of all beneficiaries. The relative increase was even more pronounced in the proportion of beneficiaries aged 85+ (+45.5%).
Table 2 Number and characteristics of GP home visits made in the canton of Vaud, Switzerland, by year, and relative difference between 2006 and 2015.
|
2006
|
2007
|
2008
|
2009
|
2010
|
2011
|
2012
|
2013
|
2014
|
2015
|
Annual mean
|
% difference between 2006 and 2015
|
| Number of physicians who billed at least one consultation |
455 |
447 |
440 |
437 |
454 |
462 |
475 |
487 |
482 |
481 |
462 |
+5.7% |
| Number of physicians who billed at least one home visit, % |
397, 87% |
402, 90% |
384, 87% |
387, 89% |
390, 86% |
400, 87% |
422, 89% |
432, 89% |
425, 88% |
420, 87% |
406, 88% |
+5.8% |
| Total annual number of home visits |
57 034 |
56 481 |
53 980 |
50 557 |
46 384 |
41 248 |
38 964 |
35 947 |
35 068 |
35 971 |
45 163 |
−36.9% |
| Mean number of home visits per physician (SD) |
125 (165) |
126 (162) |
123 (156) |
116 (142) |
102 (137) |
89 (133) |
82 (127) |
74 (108) |
73 (129) |
75 (136) |
98 (142) |
−40.0% |
| Mean number of consultations per physician (SD) |
3 894 (2605) |
4 078 (2588) |
4 155 (2620) |
4 076 (2573) |
3 999 (2554) |
3 859 (2585) |
3 772 (2540) |
3 764 (2558) |
3 767 (2563) |
3 821 (2464) |
3 918 (2566) |
−1.9% |
| Proportion of all consultations which are home visits |
3.2% |
3.1% |
3.0% |
2.8% |
2.6% |
2.3% |
2.2% |
2.0% |
1.9% |
2.0% |
2.5% |
−39.2% |
| Number of emergency calls, % |
11 221, 19.7% |
11 250, 19.9% |
11 421, 21.2% |
10 476, 20.7% |
9 404, 20.3% |
7 963, 19.3% |
6 882, 17.7% |
6 878, 19.1% |
7 514, 21.4% |
6 960, 19.4% |
9848, 19.8% |
−38.0% |
| Number of beneficiaries of home visits |
19 418 |
18 798 |
18 108 |
17 546 |
15 965 |
13 887 |
12 712 |
12 094 |
11 569 |
11 373 |
15 147 |
−41.4% |
| Mean number of home visits per patient (SD) |
2.94 (4.35) |
3.01 (4.44) |
2.98 (4.29) |
2.88 (3.96) |
2.91 (3.91) |
2.97 (4.00) |
3.01 (3.92) |
3.07 (3.92) |
2.98 (3.88) |
3.17 (4.24) |
2.98 (4.11) |
+7.8% |
| Resident population |
658 659 |
668 581 |
684 922 |
697 802 |
708 177 |
721 561 |
729 971 |
743 317 |
755 369 |
767 497 |
707 877 |
+16.5% |
| Proportion of beneficiaries among total resident population |
2.95% |
2.81% |
2.64% |
2.51% |
2.25% |
1.92% |
1.74% |
1.63% |
1.53% |
1.48% |
2.14% |
−49.7% |
| Proportion of women among beneficiaries |
68.2% |
68.5% |
69.7% |
68.2% |
68.4% |
68.3% |
67.6% |
67.0% |
67.8% |
67.9% |
68.1% |
−0.5% |
| Proportion of beneficiaries ≥65 years old |
66.7% |
68.4% |
69.9% |
69.2% |
72.1% |
73.8% |
75.2% |
75.9% |
75.2% |
76.5% |
72.3% |
14.7% |
| Proportion of beneficiaries ≥85 years old |
27.5% |
29.7% |
31.2% |
30.9% |
33.7% |
35.2% |
37.4% |
38.4% |
39.3% |
40.0% |
34.3% |
45.5% |
GP characteristics associated with number of visits
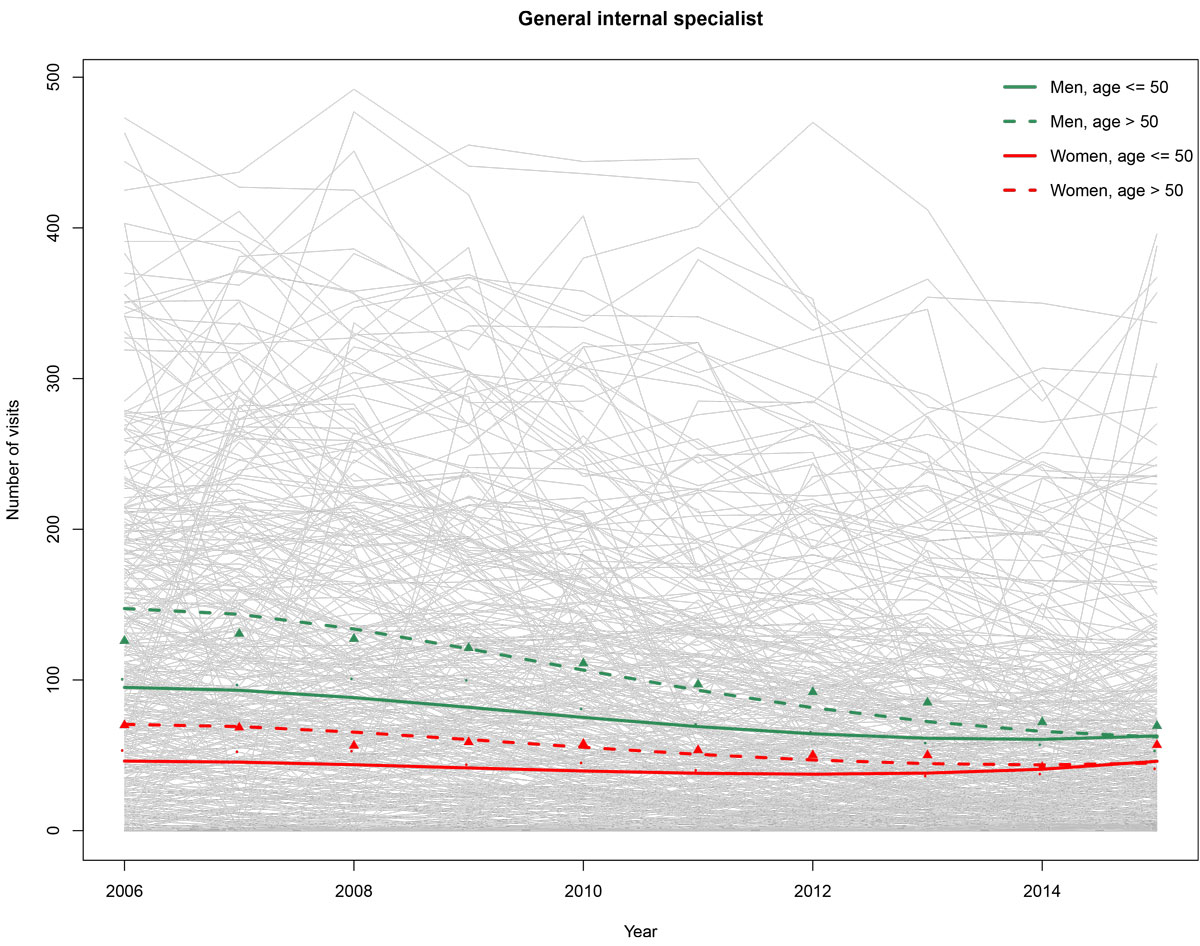
The annual number of home visits varied greatly between physicians and fluctuated over time for the same physician (fig. 1). Twenty-seven physicians (3.9% of total) made over 500 visits in one year, and were responsible for 23.7% of all home visits. These physicians were not different from other physicians in terms of specialty title, gender or age, although they did carry out fewer emergency visits (16.5 vs 21.0%, p <0.001) and the mean age of their patients was slightly lower (77.9 v. 78.7 years old, p <0.001) After excluding these “frequent visitors”, we constructed a random effect negative binomial regression model of the annual number of home visits per physician (table 3; fig. 1), which estimated that 69% of the total variability could be explained by the inter-physician variability (ICC). The estimated annual number of home visits per physician decreased over time, with a stabilisation observed during the final years of the study (table 3, fig 1). At baseline (2006), the number of home visits was higher for male and older physicians (p <0.001 and p = 0.006, respectively). General internal specialists carried out more home visits compared with medical practitioners (p = 0.002). The differences according to gender, age class and specialist title decreased over time, as shown by the interaction terms with time in the model that counterbalance the direct effect of the covariates. The parameters of the model did not differ markedly when frequent visitors were included.
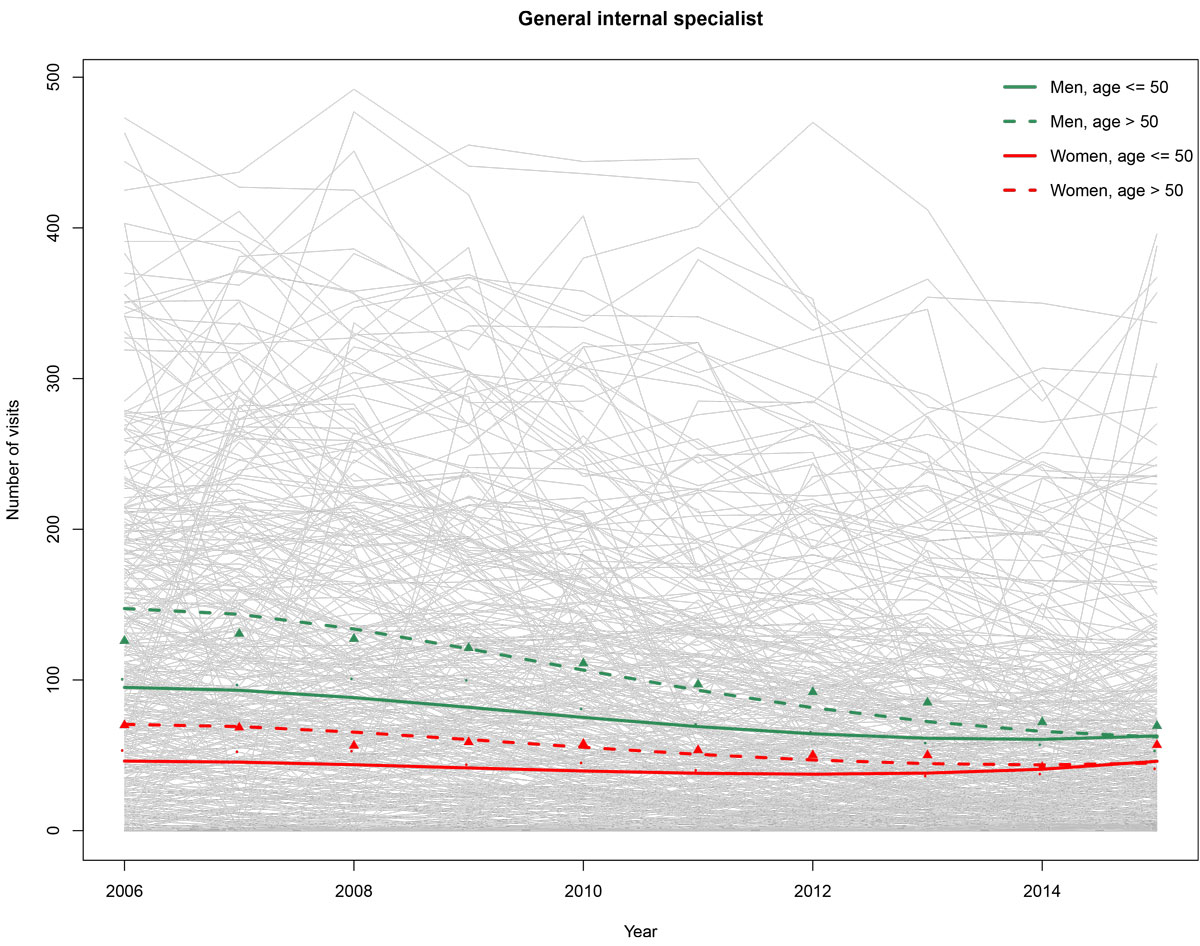
Figure 1 Evolution of home visits made by general internists in the canton of Vaud between 2006 and 2015, by gender and baseline age. Grey solid lines: spaghetti plot of annual number of visits per physician; 1 line = 1 physician. Dots: observed average number of home visits per year per physician, physicians up to 50 years old, green = men, red = women. Triangles: observed average number of home visits per year per physician, physicians older than 50 years, green = men, red = women. Green and red lines: predicted values of average number of home visits from the regression model, green = men, red = women, solid line = physicians up to 50 years old, dashed line = physicians older than 50 years.
Table 3 Mixed effect negative binomial regression model of annual number of home visits per physician. Frequent visitors, defined as physicians who billed more than 500 visits during a single year, were excluded (n = 27).
|
Coefficient
|
95% confidence interval
|
p-value
|
| Male physician |
0.965 |
0.621–1.310 |
<0.001 |
| Physician’s baseline age >50 years |
0.424 |
0.104–0.744 |
0.009 |
| Specialty (practitioner vs general internal specialist) |
−0.859 |
−1.404 – −0.314 |
0.002 |
| Year2
|
−0.017 |
−0.023 – −0.012 |
<0.001 |
| Year3
|
0.002 |
0.001–0.002 |
<0.001 |
| Year2 * male |
−0.005 |
−0.007 – −0.003 |
<0.001 |
| Year2 * (age >50) |
−0.006 |
−0.008 – −0.004 |
<0.001 |
| Year2 * specialty |
0.005 |
0.001–0.010 |
0.018 |
Discussion
Main findings
Physicians of the canton of Vaud undertook almost half a million (451,634) home visits between 2006 and 2015. Almost two thirds of all visits were to about 10,000 patients, mostly women and older individuals, representing 1.4% of the resident population. Over 85% of physicians provided home visits throughout the study period. However, the number of visits per physician decreased by 40%, reducing both the absolute number of visits and the proportion of beneficiaries in the population.
Decrease in home visits
This decrease in home visits has been described throughout industrialised countries, including Switzerland [22, 26, 30–32], with the exception of the US, where a recent increase in home visits to Medicare patients has been reported [21]. The mean number of home visits per physician is even lower in our study than in self-reported figures from a sample of Swiss GPs (82 per year vs 3.2 per week in 2012) [33]. This could be due to an overestimation in self-reported data compared to actual billing data, but we cannot exclude the possibility that figures in the canton of Vaud are lower than national figures. Indeed, compared with the rest of the country, Western Switzerland has a high density of home care on offer [34], and the number of home care beneficiaries increased by 26% during the study period (source: Statistique Vaud). This relatively high level of home care provision in Vaud (in comparison with other areas of Switzerland) could play a role in the number of home visits. However, collecting data to assess this association was beyond the scope of the current study.
Emergency home visits
In our study, routine visits to elderly patients represented the bulk of all home visits, and emergency care only a small part (20%). This is important, as the public debate around home visits often focusses on the emergency response. Indeed, there are an increasing number of professional medical companies that specialise in the provision of emergency home visits. As of 2015, these do not appear to play an important role in care provision in the canton of Vaud, where most home visits were still undertaken by traditional practice physicians. We identified some “frequent visitors” in our data, corresponding to GPs who had billed at least 500 visits during a single year. However, based on GP and patient characteristics, these did not correspond to either emergency professionals or GPs affiliated with residential homes.
GP characteristics
Physician characteristics such as age and gender were associated with a decrease in the number of home visits. This was supported by the results of the regression model, thereby confirming earlier findings [24, 35]. While the effect of physicians’ age tends to disappear in final years of the study, the ongoing feminisation of family medicine in Switzerland could result in a further decrease in the overall number of home visits. It is also of concern that the resident population is growing three times faster than the number of general practitioners, potentially resulting in increased time pressure on GPs. Indeed, the decrease in home visits was not related to a general decrease in physicians’ activity, as shown by the stable number of consultations per physician in our study. If a GP has to serve a larger fraction of the population, there might be less time available for home visits. Furthermore, this would lead to questions about the ability of the GP to systematically visit chronic patients at home. There may be less burn out among physicians that carry out home visits [36], and it is certainly beneficial in terms of the patient-doctor relationship, but other health professionals such as nurses, especially nurses working in the same practice as the GP, could perform some of these visits. Such models of care exist in North America and Europe [37, 38] and are being developed in Switzerland [39]. Home visits could be among the tasks delegated by GPs in these new models.
Study limitations
There are several limitations to our results. The main limitation is that we cannot differentiate between visits to patients’ private homes and visits to patients in residential homes, but the fact that the mean age of home visit beneficiaries was much lower than the mean age of patients in residential homes (85 years) indicates that this was not a major phenomenon. It was also not possible to differentiate between home visits made in the context of medical duty service and home visits made to a physician’s own patients. More detailed data, including the motive and the context of the visit, will be collected through the Sentinella Surveillance Network in 2019, which should be a useful adjunct to our results. The absence of data from paediatricians and other specialists who may also perform home visits may preclude extrapolation to the paediatric population. In addition, not all physicians are members of the Société Vaudoise de Médecine and some underreporting cannot be excluded, although we estimate that this is a minor phenomenon based on the comparison between the number of physicians in our dataset and national statistics on number of practicing physicians in the ambulatory sector. In addition, we may have underestimated the number of home visits if physicians omitted to bill the transport costs associated with a visit, resulting in the classification of the visit as a normal practice consultation.
Conclusion
In summary, although the vast majority of physicians in the Canton of Vaud continue to visit patients at home, the overall number of home visits is declining. In the rapidly evolving context of an ageing population and the development of home care, the role of physicians and the way they provide care are changing. An in-depth assessment of the reasons for home visits and home care from the perspective of physicians, patients and home care actors, for example using qualitative methods, would be needed in order to characterise potential gaps and inform policy-makers on possible improvements to the system so that it better meets patient needs. In addition, new models of care currently being developed should address the demand for home visits.
Acknowledgement
L. Herzig and T. Bischoff for initial study support and negociations with trust centre.
References
1
Wilson
K
,
Bachman
SS
. House Calls: The Impact of Home-Based Care for Older Adults With Alzheimer’s and Dementia. Soc Work Health Care. 2015;54(6):547–58. doi:.https://doi.org/10.1080/00981389.2015.1045576
2
Crome
P
,
Malham
A
,
Baker
D
,
Smith
AE
,
Bloor
R
. Domiciliary visits to the old and the mentally ill: how valuable?
J R Soc Med. 2000;93(4):187–90. doi:.https://doi.org/10.1177/014107680009300408
3
Sharifi
V
,
Tehranidoost
M
,
Yunesian
M
,
Amini
H
,
Mohammadi
M
,
Jalali Roudsari
M
. Effectiveness of a low-intensity home-based aftercare for patients with severe mental disorders: a 12-month randomized controlled study. Community Ment Health J. 2012;48(6):766–70. doi:.https://doi.org/10.1007/s10597-012-9516-z
4
van Kempen
JA
,
Robben
SH
,
Zuidema
SU
,
Olde Rikkert
MGM
,
Melis
RJ
,
Schers
HJ
. Home visits for frail older people: a qualitative study on the needs and preferences of frail older people and their informal caregivers. Br J Gen Pract. 2012;62(601):e554–60. doi:.https://doi.org/10.3399/bjgp12X653606
5
Borgsteede
SD
,
Graafland-Riedstra
C
,
Deliens
L
,
Francke
AL
,
van Eijk
JT
,
Willems
DL
. Good end-of-life care according to patients and their GPs. Br J Gen Pract. 2006;56(522):20–6.
6
Theile
G
,
Kruschinski
C
,
Buck
M
,
Müller
CA
,
Hummers-Pradier
E
. Home visits - central to primary care, tradition or an obligation? A qualitative study. BMC Fam Pract. 2011;12(1):24. doi:.https://doi.org/10.1186/1471-2296-12-24
7
Reuben
DB
,
Fried
TR
,
Wachtel
TJ
,
Tinetti
ME
. When the patient cannot come to the doctor: a medical housecalls program. J Am Geriatr Soc. 1998;46(2):226–31. doi:.https://doi.org/10.1111/j.1532-5415.1998.tb02544.x
8
Burge
FI
,
Lawson
B
,
Johnston
G
. Home visits by family physicians during the end-of-life: Does patient income or residence play a role?
BMC Palliat Care. 2005;4(1):1. doi:.https://doi.org/10.1186/1472-684X-4-1
9
Pivodic
L
,
Harding
R
,
Calanzani
N
,
McCrone
P
,
Hall
S
,
Deliens
L
, et al.
Home care by general practitioners for cancer patients in the last 3 months of life: An epidemiological study of quality and associated factors. Palliat Med. 2016;30(1):64–74.
10
Rytter
L
,
Jakobsen
HN
,
Rønholt
F
,
Hammer
AV
,
Andreasen
AH
,
Nissen
A
, et al.
Comprehensive discharge follow-up in patients’ homes by GPs and district nurses of elderly patients. A randomized controlled trial. Scand J Prim Health Care. 2010;28(3):146–53. doi:.https://doi.org/10.3109/02813431003764466
11
Ploeg
J
,
Feightner
J
,
Hutchison
B
,
Patterson
C
,
Sigouin
C
,
Gauld
M
. Effectiveness of preventive primary care outreach interventions aimed at older people: meta-analysis of randomized controlled trials. Can Fam Physician. 2005;51:1244–5.
12
Sandberg
M
,
Kristensson
J
,
Midlöv
P
,
Jakobsson
U
. Effects on healthcare utilization of case management for frail older people: a randomized controlled trial (RCT). Arch Gerontol Geriatr. 2015;60(1):71–81. doi:.https://doi.org/10.1016/j.archger.2014.10.009
13
Hansen
LO
,
Young
RS
,
Hinami
K
,
Leung
A
,
Williams
MV
. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–8. doi:.https://doi.org/10.7326/0003-4819-155-8-201110180-00008
14
Lykkegaard
J
,
Larsen
PV
,
Paulsen
MS
,
Søndergaard
J
. General practitioners’ home visit tendency and readmission-free survival after COPD hospitalisation: a Danish nationwide cohort study. NPJ Prim Care Respir Med. 2014;24(1):14100. doi:.https://doi.org/10.1038/npjpcrm.2014.100
15
Brandis
SJ
,
Tuite
AT
. Falls prevention: partnering occupational therapy and general practitioners. Aust Health Rev. 2001;24(1):37–42. doi:.https://doi.org/10.1071/AH010037
16
Elkan
R
,
Kendrick
D
,
Dewey
M
,
Hewitt
M
,
Robinson
J
,
Blair
M
, et al.
Effectiveness of home based support for older people: systematic review and meta-analysis. BMJ. 2001;323(7315):719–25. doi:.https://doi.org/10.1136/bmj.323.7315.719
17
Joyce
C
,
Piterman
L
. Trends in GP home visits. Aust Fam Physician. 2008;37(12):1039–42.
18
Javorić
H
,
Topolovec-Nižetić
V
,
Pavleković
G
. Home visits in Croatian family practice: a longitudinal study: 1995-2012. Coll Antropol. 2014;38(Suppl 2):55–9.
19
Peterson
LE
,
Landers
SH
,
Bazemore
A
. Trends in physician house calls to Medicare beneficiaries. J Am Board Fam Med. 2012;25(6):862–8. doi:.https://doi.org/10.3122/jabfm.2012.06.120046
20
Whewell
J
,
Marsh
GN
,
McNay
RA
. Changing patterns of home visiting in the north of England. Br Med J (Clin Res Ed). 1983;286(6373):1259–61. doi:.https://doi.org/10.1136/bmj.286.6373.1259
21
Sairenji
T
,
Jetty
A
,
Peterson
LE
. Shifting Patterns of Physician Home Visits. J Prim Care Community Health. 2016;7(2):71–5.
22
van den Berg
MJ
,
Cardol
M
,
Bongers
FJ
,
de Bakker
DH
. Changing patterns of home visiting in general practice: an analysis of electronic medical records. BMC Fam Pract. 2006;7(1):58. doi:.https://doi.org/10.1186/1471-2296-7-58
23
Osborn
R
,
Moulds
D
,
Schneider
EC
,
Doty
MM
,
Squires
D
,
Sarnak
DO
. Primary Care Physicians In Ten Countries Report Challenges Caring For Patients With Complex Health Needs. Health Aff (Millwood). 2015;34(12):2104–12. doi:.https://doi.org/10.1377/hlthaff.2015.1018
24
Boerma
WGW
,
Groenewegen
PP
. GP home visiting in 18 European countries Adding the role of health system features. Eur J Gen Pract. 2001;7(4):132–7. doi:.https://doi.org/10.3109/13814780109094331
25Merçay C. Médecins de premier recours – Situation en Suisse, tendances récentes et comparaison internationale. Analyse de l’International Health Policy Survey 2015 du Commonwealth Fund sur mandat de l’Office fédéral de la santé publique (OFSP). In: Obsan Dossier 50. Neuchâtel: Observatoire suisse de la santé; 2015.
26
Cohidon
C
,
Cornuz
J
,
Senn
N
. Primary care in Switzerland: evolution of physicians’ profile and activities in twenty years (1993-2012). BMC Fam Pract. 2015;16(1):107. doi:.https://doi.org/10.1186/s12875-015-0321-y
27
Sauter
M
,
Santos-Eggimann
B
,
Spagnoli
J
. Older persons’ perceptions of general practitioner or specialist primary care physicians: same point of view?
Swiss Med Wkly. 2015;145:w14085. doi:.https://doi.org/10.4414/smw.2015.14085
28
Efstathopoulou
A
,
David
S
,
Herzig
L
. Visite à domicile par le médecin de famille : état des lieux en Europe et en Suisse [Home visits by GPs - Considerations in Europe and in Switzerland]. Rev Med Suisse. 2016;12(537):1874–8.
29Statistique médicale FMH 2010 [Internet] https://www.fmh.ch/fr/services/statistique/statistique_medicale.html
30
Aylin
P
,
Majeed
FA
,
Cook
DG
. Home visiting by general practitioners in England and Wales. BMJ. 1996;313(7051):207–10. doi:.https://doi.org/10.1136/bmj.313.7051.207
31
Meyer
GS
,
Gibbons
RV
. House calls to the elderly--a vanishing practice among physicians. N Engl J Med. 1997;337(25):1815–20. doi:.https://doi.org/10.1056/NEJM199712183372507
32
Snijder
EA
,
Kersting
M
,
Theile
G
,
Kruschinski
C
,
Koschak
J
,
Hummers-Pradier
E
, et al.
Hausbesuche: Versorgungsforschung mit hausärztlichen Routinedaten von 158.000 Patienten [Home visits in German general practice: findings from routinely collected computer data of 158,000 patients]. Gesundheitswesen. 2007;69(12):679–85. doi:.https://doi.org/10.1055/s-2007-993181
33
http://catalog.interrai.org/CHA-community-health-assessment-manual
34Ankers N, Serdaly C, Personnes âgées peu dépendantes de soins: prise en charge dans cinq cantons romands. Lausanne: Plateforme d'information du Système de Santé Vaudois; 2017.
35
Boerma
WG
,
van den Brink-Muinen
A
. Gender-related differences in the organization and provision of services among general practitioners in Europe: a signal to health care planners. Med Care. 2000;38(10):993–1002. doi:.https://doi.org/10.1097/00005650-200010000-00003
36
Weidner
AKH
,
Phillips
RL, Jr
,
Fang
B
,
Peterson
LE
. Burnout and Scope of Practice in New Family Physicians. Ann Fam Med. 2018;16(3):200–5. doi:.https://doi.org/10.1370/afm.2221
37
Prasad
S
,
Dunn
W
,
Hillier
LM
,
McAiney
CA
,
Warren
R
,
Rutherford
P
. Rural geriatric glue: a nurse practitioner-led model of care for enhancing primary care for frail older adults within an ecosystem approach. J Am Geriatr Soc. 2014;62(9):1772–80. doi:.https://doi.org/10.1111/jgs.12982
38
Faber
MJ
,
Burgers
JS
,
Westert
GP
. A sustainable primary care system: lessons from the Netherlands. J Ambul Care Manage. 2012;35(3):174–81. doi:.https://doi.org/10.1097/JAC.0b013e31823e83a4
39Schubli D, Hodel M. Nouveaux modèles de soins pour la médecine de premier recours“. Rapport du Groupe de travail „Nouveaux modèles de soins pour la médecine de premier recours“ de la CDS et de l’OFSP. In : Berne: GDK-CDS; 2012.