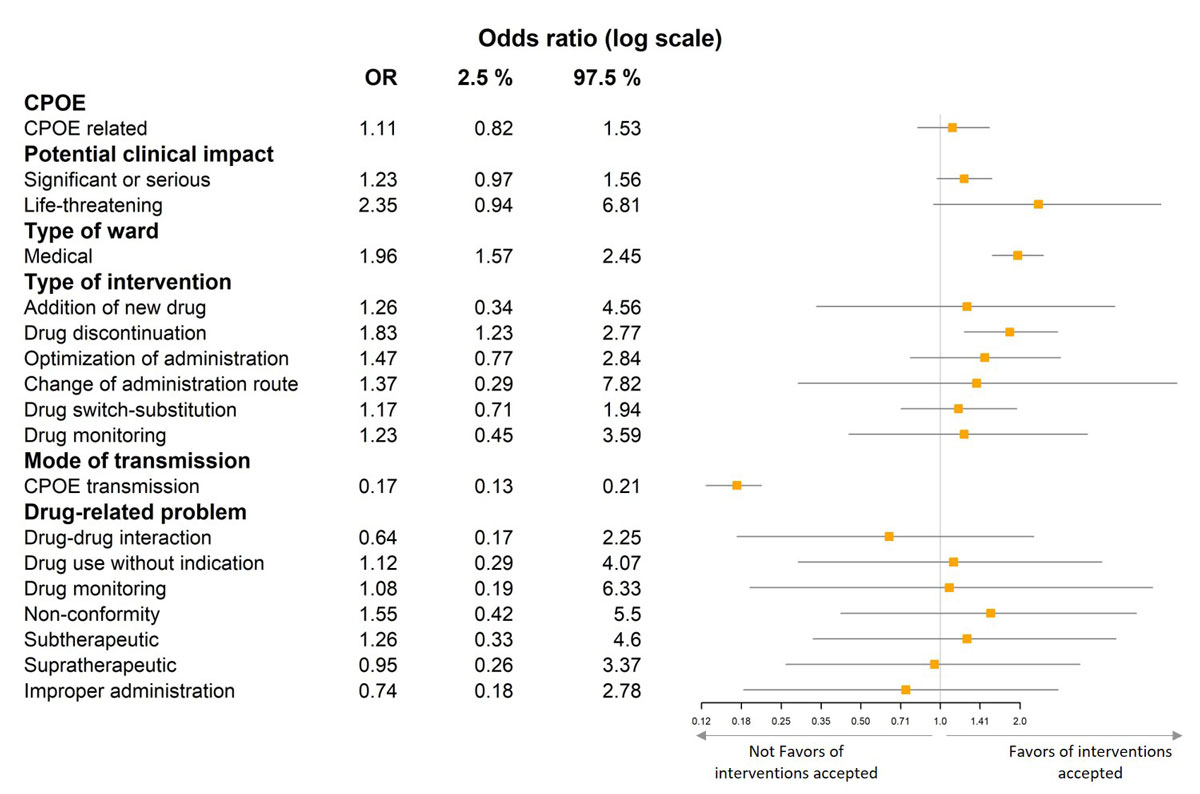
Figure 1 Forest plot showing the association between acceptance and various characteristics (multivariate analysis).
DOI: https://doi.org/10.4414/smw.2019.20015
Prescribing errors (PE) are frequent in hospitals and responsible for adverse drug events (ADEs) associated with longer hospital stays [1]. Most prescribing errors do not lead to ADEs. Computerised physician order entry (CPOE) and pharmacy validation were developed to reduce PEs. The interception of PEs by clinical pharmacists have been effective in decreasing the ADEs potentially generated by electronic prescriptions [2]. Although computerised prescriber order entry reduces medication errors, it also generates new types of errors. Koppel et al. were the first to analyse the role of electronic prescribing system use in the generation of medication errors [3]. Other studies have investigated the negative effects of computerisation, including an increase in the risk of medication errors [4]. In 2007, we evaluated the impact of the combination of interventions by pharmacists and CPOE on the prescribing process [5]. Pharmacy validation had a moderate short-term effect in reducing potential prescribing errors. However, pharmacy validation may also provide ongoing benefits by identifying necessary improvements in the CPOE. This study aimed to identify and evaluate intervention during the pharmaceutical analysis of medical prescriptions on a CPOE system, their acceptance by physicians, the potential clinical impact for patients, and whether the prescribing errors were due to computerisation. The study further aimed to assess the evolution of these aspects 10 years after a first assessment.
The European Georges-Pompidou Hospital (HEGP) is a French teaching hospital (tertiary care) with 714 beds and 106 day beds. There are 39 care units allocated between 28 medical and 11 surgical wards. The mean duration of hospitalisation is 6.1 days. A patient information system, integrating an electronic health record (EHR) and a CPOE system (DxCare® Medasys), has been used throughout the hospital since 2000. The CPOE system is combined with a clinical decision support system (CDSS) that checks for duplicate treatment and drug-drug interactions. The CPOE collates structured observations, prescribing examinations, prescribed drugs, pharmaceutical analysis of prescribed drugs, and imaging procedures. All health professionals have access to the CPOE. Electronic prescription is available for all units except for three intensive care units.
The clinical pharmacy department consists of 10 pharmacists: seven senior pharmacists and three pharmacy residents (7.1 full-time equivalents). From Monday to Friday, each pharmacist reviews prescriptions from three or four wards through the CPOE system and participates in medical rounds with the medical staff in the wards (641 beds). Prescriptions are reviewed directly at the pharmacy. On nights and weekends, the prescriptions are reviewed the next day, if they have not expired, by pharmacists or the pharmacy resident on duty. Each prescription is checked, drug by drug (dose unit, time and route of administration, drug interactions, etc.), against the biological data and medical records (comorbidities, allergies, etc.) of the patient. If a pharmacist is absent, prescriptions in their clinical wards are analysed by another member of the team. Interventions by pharmacists can result from such prescription analysis. These interventions can be accessed by the prescribers and/or nurses via a symbol inserted in front of a given prescription order line (validated, refused, substitution, or equivalence) as well as by a pharmaceutical comment added to the prescription line. Since April 2015, the pharmacist records each intervention prospectively into the CPOE system using a modified version of the intervention by a pharmacist codification tool developed by the French Society of Clinical Pharmacy [6]. The interventions are recorded prospectively within the pharmaceutical analysis in a structured questionnaire directly available in the CPOE. The item ‘drug adverse reaction’ was deleted and an item was added to assess whether the medication error was due to CPOE or not. A comment on the prescription line does not lead systematically to an intervention by a pharmacist recorded in the structured questionnaire. Discrepancies were previously highlighted between the performance of pharmacists who analysed the same prescriptions in a published study [7]. Thus, a weekly pharmaceutical staff meeting was initiated to discuss interventions made during the week to standardise practices between pharmacists, residents, and students, share experiences to be more efficient, and improve knowledge of the software. The interventions by pharmacists in the structured questionnaire can be seen by physicians on a day-by-day basis. This allows the pharmacy manager to evaluate clinical pharmaceutical activities.
We performed a prospective observational study to evaluate the incidence of interventions by pharmacists, the acceptance rate of these interventions by physicians, the proportion of interventions due to CPOE-related errors, and the clinical impact of the interventions on patient safety. The main outcome was the number of clinical interventions by pharmacists prospectively collected over thirteen months (April 2015 to May 2016) from medical and surgical wards throughout the hospital. The acceptance of interventions and CPOE-related problems were assessed and the potential impact of interventions on patient safety was evaluated by a multidisciplinary committee.
Interventions by pharmacists recorded using the structured questionnaires were extracted from the CPOE in an Excel spreadsheet. For each intervention made, the pharmacists recorded data prospectively in the questionnaire using a dropdown menu: drug anatomical therapeutic chemical (ATC) classification, drug-related problem, type of intervention, mode of transmission to physicians of the intervention according to the French Society of Clinical Pharmacy tool (oral communication in the unit or by phone or communication using the CPOE), acceptance of the intervention by the clinician, type of ward, and implication of CPOE. CPOE-related errors were subjectively classified by pharmacists (1) when they were more likely to occur because of the presence of informatics, (2) when they would have been less likely to happen with a traditional handwritten prescription, or (3) when the physician said he or she was unable to prescribe what he or she wanted.
The acceptance of interventions by pharmacists were categorised as ‘accepted and modified’, ‘accepted but not modified’, ‘not assessable’, ‘no modification required’, or ‘unaccepted’. Interventions were considered to be ‘accepted but not modified’ when physicians said they agreed with the pharmacist’s advice but did not change the prescription order because, for example, the patient was discharged. ‘Not assessable’ interventions were those for which the physician was notified, but the patient was discharged before the prescription was checked. ‘Unaccepted’ interventions were those refused by physicians (no modifications after several days or expressed refusal). Two senior pharmacists (MCL, SB) checked all interventions by pharmacists for accuracy.
Three senior pharmacists (MCL, SB, BS) independently reviewed all of the interventions to rate the potential clinical impact for the patient. They had access to the interventions in detail, but were blinded to acceptance, the prescriber name, and the patient name. A three-category scale (none, purely preventive, serious or significant, and life-threatening) adapted from previous publications was used [8, 9]. Discrepancies were resolved by a multidisciplinary committee composed of two physicians (AK, PD) and the three senior pharmacists. The committee had access to the entire prescription if needed.
In our hospital, medical data of the EHR are stored in a clinical data warehouse approved by the French National Commission for Data Protection and Liberties (CNIL). All patients included in the study were informed about the use of their personal data for institutional-initiated research studies and had an electronic option to decline.
The results for categorical variables are presented as numbers and associated percentages with their 95% confidence interval (CI). Group comparisons were performed using the chi-square test (or Fisher’s exact test, when appropriate). The relationship between intervention acceptance and variables (type of ward, mode of transmission, potential clinical impact, drug-related problems, and type of intervention) were investigated using a logistic regression model. The relationship between CPOE-related errors and risk factors were also studied. All variables were analysed by univariate and multivariate analysis. Results are expressed as an odds ratio (OR) with the 95% CI. A threshold p-value of 0.05 was considered for statistical significance. All analyses were performed using R Studio software (version 1.0.143).
A total of 2159 interventions by pharmacists occurred during the study period (0.76 PIs for 100 prescription order lines). Among these, 2141 were analysed. Eighteen interventions were excluded (n = 18; 0.83%, 95% CI 0.82–0.85): 13 because the interventions were difficult to understand and were not assessable based on the French Society of Clinical Pharmacy codification tool (see supplementary table S1 in appendix 1) and five because of incomplete information despite access to the entire prescription and EHR.
There were 1,475 interventions in the medical wards (68.9%) and 666 in the surgical wards (31.1%). The characteristics of the interventions by pharmacists are summarised in table 1. The most commonly identified type of drug-related problem was a ‘supratherapeutic dose’, followed by ‘subtherapeutic dose’ and ‘drug-drug interaction’. Among the ‘drug-drug interactions’, 225 (96.6, 95% CI 93.3–98.5) were contraindication. Among these, 145 (64.4, 95% CI 57.8–70.7) concerned the ATC class ‘nervous system’. Interventions by pharmacists were mainly transmitted orally, either by phone or face-to-face to the physicians.
Table 1 Characteristics of the 2141 investigated and appropriate interventions by pharmacists.
| Characteristics | n | % (95% CI) | |
|---|---|---|---|
| Total n (%) | 2141 | 100 | |
| Type of ward | Medical | 1475 | 68.9 (68.88–68.92) |
| Surgical | 666 | 31.1 (31.08–31.12) | |
| Graded by pharmacists | |||
| Drug-related problem | Supratherapeutic dose | 700 | 32.7 (32.68–32.72) |
| Subtherapeutic dose | 398 | 18.6 (18.58–18.62) | |
| Drug-drug interaction (all levels of severity) | 233 | 10.9 (10.89–10.91) | |
| Non-conformity to guidelines/contraindication | 212 | 9.9 (9.89–9.91) | |
| Improper administration | 203 | 9.5 (9.49–9.51) | |
| Drug use without indication | 200 | 9.3 (9.29–9.31) | |
| Untreated indication | 174 | 8.1 (8.09–8.11) | |
| Drug monitoring | 19 | 0.9 (0.90–0.90) | |
| Failure to receive drug | 2 | 0.1* | |
| Type of intervention | Dose adjustment | 943 | 44.0 (43.98–44.02) |
| Drug discontinuation | 438 | 20.5 (20.48–20.52) | |
| Drug switch-substitution | 362 | 16.9 (16.88–16.92) | |
| Addition of new drug | 176 | 8.2 (8.19–8.21) | |
| Optimisation of administration | 175 | 8.2 (8.19–8.21) | |
| Drug monitoring | 38 | 1.8 (1.79–1.81) | |
| Change of administration route | 9 | 0.4 (0.40–0.40) | |
| Mode of transmission | Oral communication | 1485 | 69.4 (69.38–69.42) |
| Computerised physician order entry | 656 | 30.6 (30.58–30.62) | |
| ATC class | N - Nervous system | 537 | 25.1 (25.08–25.12) |
| J - Anti-infectives for systemic use | 411 | 19.2 (19.18–19.22) | |
| C - Cardiovascular system | 315 | 14.7 (14.69–14.71) | |
| B - Blood and blood forming organs | 301 | 14 (13.99–14.01) | |
| A - Alimentary tract and metabolism | 274 | 12.8 (12.79–12.81) | |
| R - Respiratory system | 74 | 3.7 (3.69–3.71) | |
| H - Systemic hormonal preparations, excluding sex hormones and insulins | 63 | 2.9 (2.89–2.91) | |
| L - Antineoplastic and immunomodulating agents | 51 | 2.4 (2.39–2.41) | |
| M - Musculoskeletal system | 40 | 1.5 (1.49–1.51) | |
| G - Genito-urinary system and sex hormones | 29 | 1.4 (1.40–1.40) | |
| V - Various | 24 | 1.2 (1.20–1.20) | |
| S - Sensory organs | 11 | 0.6 (0.60–0.60) | |
| P - Antiparasitic products, insecticides and repellents | 10 | 0.5 (0.50–0.50) | |
| D - Dermatological | 1 | 0.05* | |
| Graded by review committee | |||
| Potential clinical impact | Significant or serious | 1136 | 53.0 (52.98–53.02) |
| None, purely preventive | 963 | 45.0 (44.98–45.02) | |
| Life-threatening | 42 | 2.0 (1.99–2.01) | |
* Non-significant CI
Most interventions by pharmacists considered prescriptions having a significant or serious potential clinical impact for the patient (n = 1136; 53%) and 42 (2%) of them were considered to be life-threatening (table 1). The potential ‘life-threatening’ impact mainly concerned the ATC classes ‘anti-infective’ (n = 16; 38.1%) and ‘nervous system’ (n = 6; 14.2%). Among these, 17 were due to an allergy recorded in the CPOE, while 8 (19%) concerned the ATC ‘blood and blood forming organs’, mostly anticoagulant prescription (see table S2 in appendix 1).
Of the 2141 interventions by pharmacists, 1587 (74.1, 95% CI 72.2–76) were accepted. Non-assessable interventions by pharmacists were pooled into the unaccepted category for statistical analyses. Acceptance of the interventions was associated with the potential clinical impact for the patient (p = 0.002), the mode of transmission (p <0.001), the type of ward (p <0.001), and drug-related problems (p = 00.2) (table 2).
Table 2 Association between acceptance and variable.
| Variables |
Interventions accepted
n = 1587 (74.1%) |
Interventions not accepted
n = 554 (25.9%) |
p-value | |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Drug-related problem | Supratherapeutic dose | 505 (31.8) | 195 (35.2) | 0.02 |
| Subtherapeutic dose | 305 (19.2) | 93 (16.8) | ||
| Drug-drug interaction (all levels of severity) | 163 (10.3) | 70 (12.6) | ||
| Non-conformity to guidelines/contraindication | 168 (10.6) | 44 (7.9) | ||
| Improper administration | 137 (8.6) | 66 (11.9) | ||
| Drug use without indication | 159 (10.1) | 41 (7.4) | ||
| Untreated indication | 135 (8.5) | 39 (7.1) | ||
| Drug monitoring | 13 (0.8) | 6 (1.1) | ||
| Failure to receive drug | 2 (0.1) | |||
| Type of intervention | Dose adjustment | 689 (43.4) | 254 (45.8) | 0.17 |
| Addition of new drug | 137 (8.6) | 39 (7.1) | ||
| Drug discontinuation | 339 (21.4) | 99 (17.9) | ||
| Optimisation of administration | 120 (7.6) | 55 (9.9) | ||
| Change of administration route | 6 (0.4) | 3 (0.5) | ||
| Drug switch-substitution | 270 (17) | 92 (16.6) | ||
| Drug monitoring | 26 (1.6) | 12 (2.2) | ||
| Type of ward | Medical | 1,160 (73.1) | 315 (56.9) | <0.001 |
| Surgical | 427 (26.9) | 239 (43.1) | ||
| Mode of transmission | Oral communication | 1,263 (79.6) | 222 (40.1) | <0.001 |
| Computerised physician order entry | 324 (20.4) | 332 (59.9) | ||
| Graded by review committee | ||||
| Potential clinical impact | None, purely preventive | 681 (42.9) | 282 (50.9) | 0.002 |
| Significant or serious | 870 (54.8) | 266 (48) | ||
| Life-threatening | 36 (2.3) | 6 (1.1) | ||
In the multivariate analysis, acceptance of the interventions by pharmacists was associated with the medical ward (OR 1.96, 95% CI 1.57–2.45) and ‘drug discontinuation’ intervention (OR 1.83, 95% CI 1.23–2.77). Non-acceptance of the interventions was associated with CPOE transmission (OR = 0.17, 95% CI 0.13–0.21). These results are illustrated in figure 1.
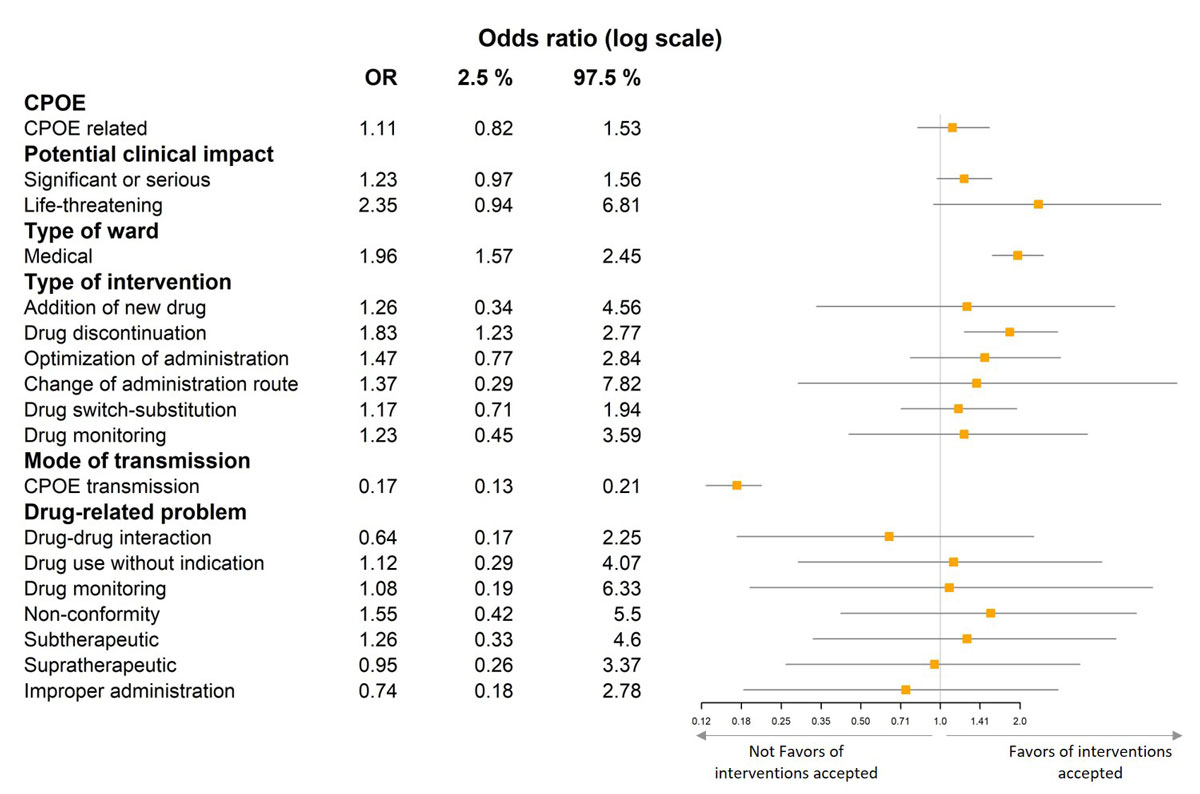
Figure 1 Forest plot showing the association between acceptance and various characteristics (multivariate analysis).
Among all interventions by pharmacists, a possible role of the CPOE system in the error was attributed to 315 (14.7, 95% CI13.2–16.3). Drug-related problems of the interventions due to the use of CPOE are summarised in table 3 and mainly concern ‘subtherapeutic dose’ (n = 119; 37.8, 95% CI 32.4–43.4), ‘supratherapeutic dose’ (n = 114; 36.2, 95% CI 30.9–41.8), ‘drug without indication’ (n = 39; 12.4, 95% CI 9–16.5), and ‘untreated indication’ (n = 12; 3.8, 95% CI 2–6.6). The CPOE system was not associated with potential severity for the patient (p = 0.62).
Table 3 Association between computerised physician order entry involvement in prescription errors and variable (univariate analysis).
| Variables |
Not computerised physician order entry related
n = 1826 (85.3%) |
Computerised physician order entry related
n = 315 (14.7%) |
p-value |
|---|---|---|---|
| n (row %) | n (row %) | ||
| Drug-related problem | |||
| Supratherapeutic dose | 586 (32.0) | 114 (36.2) | |
| Subtherapeutic dose | 279 (15.3) | 119 (37.8) | |
| Drug-drug interaction (all levels of severity) | 232 (12.7) | 1 (0.3) | |
| Non-conformity to guidelines/contraindication | 200 (10.9) | 12 (3.8) | |
| Improper administration | 188 (10.3) | 15 (4.8) | |
| Drug use without indication | 161 (8.8) | 39 (12.4) | |
| Untreated indication | 162 (8.9) | 12 (3.8) | |
| Drug monitoring | 18 (1.0) | 1 (0.3) | |
| Failure to receive drug | 0 (0.0) | 2 (0.6) | |
| Potential clinical impact | |||
| None, purely preventive | 814 (44.6) | 149 (43.7) | 0.62 |
| Significant or serious | 975 (53.4) | 161 (51.1) | |
| Life-threatening | 37 (2) | 5 (1.6) | |
Of the 2141 potential prescribing errors, the most frequent was ‘supratherapeutic dose’ (32.7%). Physician acceptance was 74.1%. A total of 315 (14.7%) errors were ascribed to CPOE. Among all interventions by pharmacists, 1136 (53%) interventions concerned prescriptions with potentially significant or serious impact for the patient and 42 (2%) of them were considered to be life-threatening. This is the first prospective observational study that analysed interventions by pharmacists over an extended period (13 months) and also rated the potential clinical impact for the patient.
Ten years earlier, Estellat et al. studied the impact of pharmacy validation in a CPOE context at our hospital. At that time, the acceptance rate was 23%, but pharmacists did not take part in medical rounds. Pharmacists analysed the prescriptions in the pharmacy unit and were not integrated into the medical staff. Our acceptance rate is now 74%. These results may be explained by the development of clinical pharmacy with pharmacists on the medical staff and/or rounds. Moreover, 14.7% of errors were attributed to the use of the software, whereas 10 years earlier the rate of errors was 49%. These results are likely due to improved knowledge of the software. The pharmacists are well known in the ward and are responsible for improving the knowledge of the software by pharmacists and senior doctors. The Department of Medical Information trains prescribers at the beginning of each resident semester. During rounds, pharmacists aid the residents in writing prescriptions and provide advice.
Many previous studies assessed interventions by pharmacists using the French Society of Clinical Pharmacy tool, as we did, but they used the Act IP® to record them. The major drug-related problems of interventions by pharmacists vary from one study to another [10]. Our major drug-related problem was ‘supratherapeutic dose’, similar to the review of French interventions by pharmacists using the Act-IP® [11]. However, 20.1% were due to administrative errors, whereas this issue was associated with 10% of interventions by pharmacists in our study. The lower rate of administrative errors is likely due to the development of systems and protocols to ease prescribing and provide administrative information to nurses. For example, antibiotics were set up in electric syringe pumps or for infusion, taking into account the stability of the medicine, depending on the concentration. Other studies of handwritten prescriptions reported incorrect doses as the most common drug-related problem [12, 13], consistent with our study. The ATC class most affected by the interventions by pharmacists was the ‘nervous system’ (n = 537; 25.1%), likely due to hydroxyzine. This followed the publication of a note by the French National Agency for Medicines and Health Products Safety (ANSM) and the European Medicines Agency (EMA) concerning hydroxyzine, which warned of the recurrent risk of potentially severe drug-drug interactions, especially with other QT interval-prolonging drugs, and recommended reducing the maximum recommended daily dose. The next most common interventions by pharmacists concerned ‘anti-infective’ and ‘cardiovascular’ drugs. The characteristics of the interventions by pharmacists were almost the same, with a few exceptions. Only a few types of drugs and errors constituted most of the interventions, and knowledge of such drugs and errors could help pharmacists to be more efficient [14]. Most interventions by pharmacists (n = 1829; 85%) were not related to the use of CPOE and 1012 (55%) were considered to have a potentially significant, serious, or life-threatening clinical impact. Bouchand et al. highlighted the important role pharmacists still have in reducing prescribing errors, despite computerisation [15].
The acceptance rate (74.1%) is similar to previous studies of pharmacists in medical rounds [11, 16]. Communication is mostly oral and the acceptance rate is higher when the interventions by pharmacists are communicated orally. Medical wards had a better acceptance rate than surgical wards. This finding confirms a previous study that showed that acceptance is higher when the pharmacist is well integrated in the ward [11]. It is more difficult for pharmacists to be involved in surgical wards because surgeons are often in the operating room. This may also be explained by the fact that the physician can see the pharmacist’s comment without informing the pharmacist. The software does not allow physicians to respond to the pharmacist’s comment, requiring that he or she must directly ask the physician if he or she wants an explanation. If the pharmacist judges that a quick modification is needed, he or she might make a phone call to the physician [17] or even to the nurse to ensure that the drug is not administered.
CPOE-related errors accounted for 14.7% of the total. This is less than other studies, which reported CPOE-related errors from 19.9% to 44.3% of all prescription errors [18–20]. We defined CPOE-related errors as those that occurred more easily than they would have in the traditional medication ordering system. In contrast, Hellot-Guersing et al. considered CPOE-related errors as those that would not have occurred if the clinician had prescribed manually [20]. Although our definition was wider, we found a lower frequency of CPOE-related errors. This may be because our study took place 15 years after implementation of the software and pharmacists and physicians now have improved knowledge of the software. This finding suggests the importance of regular training and the sharing of knowledge between users of the same CPOE system working in different hospitals. Such knowledge could perhaps decrease medication prescription errors. We did not record the cause of the CPOE error and thus we cannot quantify them. However, ‘supratherapeutic and subtherapeutic doses’ were mostly due to the use of the wrong units. ‘Supratherapeutic doses’ were also due to duplications. In addition, ‘drugs without indication’ were due to selection of the wrong medicine in the dropdown menu and ‘untreated indication’ because the prescription order line was finished and not extended.
Our study has several limitations. First, we did not evaluate drug administration but rather prescribing errors, which did not generally lead to administration errors, due to the nurse who already corrected them. Second, the acceptance or refusals were underestimated because we did not limit the time to respond. Thus, many interventions by pharmacists were in standby mode and reasons for non-compliance with the pharmacist’s advice were not investigated. Third, the records are subjective, likely not exhaustive, and may be incomplete, as in many studies. Some pharmacists may have not recorded all of their interventions in the CPOE, because they can be seen by all physicians and they may have not bothered for those that were judged to be ‘non-significant’. Comments added by a pharmacist on the prescription orders were not systematically deemed to be interventions by pharmacists. This could occur, for example, for the wrong unit due to use of the software: 1 mg of cotrimoxazole 400 mg instead of one tablet, because it was not possible for the nurse to administer only 1mg; when the nurse had already seen the error; or when the interventions by pharmacists were systematically denied (e.g., drug-drug interaction). Finally, rating all allergies as having potential life-threatening impact for patients without distinguishing immediate and delayed hypersensitivity (with lack of information on the CPOE) may have overestimated this category.
This study provides several important findings. The development of clinical pharmacy in our hospital over the last 10 years is having a positive impact. This is reflected by the acceptance rate of interventions by pharmacists, particularly for medical wards. Pharmacists still have to make progress in the surgical wards to improve the acceptance of their interventions. This will involve an improved knowledge of how the service functions because surgeons spend most of their time in the operating room. The analysis, during a weekly pharmacy staff meeting, of interventions by pharmacists that are often denied, frequent, and/or CPOE-related should help pharmacists to have a greater impact. Discussions with physicians and surgeons about denied interventions could result in recommendations. We are planning to improve the feedback of medication errors to physicians, as requested by the hospital drug committee. CPOE-related problems are transmitted to the informatics service and recurrent CPOE-related errors should encourage targeted training [21].
An incorrect dose, notably a supratherapeutic dose, was the major cause of intervention. This is sometimes due to prescriptions that require dosage adjustments based on renal function. However, a study in our hospital showed that implementing alerts at the time of ordering medications did not result in a significant decrease in inappropriate prescriptions [22]. This finding highlights the importance of developing prescription alerts. Incorrect doses also occur due to the use of the wrong units. Our hospital decided to use units such as milligrams, micrograms, grams, etc. as the default option for prescriptions instead of tablets, syringes, etc. This would avoid, for example, the prescription of 10 tablets of bisoprolol 5 mg that could lead to adverse drug event, whereas the physician wanted to prescribe 10 mg of bisoprolol 5 mg. Our CPOE system had dose checking but this function was inactivated at the demand of the physicians because it was set up incorrectly and the alerts were irrelevant. We are planning to reactivate it again, but to target the alerts to high risk medications commonly associated with prescribing errors and narrow therapeutic index medications [23].
The potential clinical impact of interventions evaluated in this study shows that the main life-threatening prescriptions concern the ATC class ‘anti-infective’, most of which were due to allergies recorded in the EHR. However, six of the potential life-threatening prescriptions were not accepted by physicians because patients were not actually allergic.
Despite there being a clinical decision support system (CDSS) to check for drug-drug interactions in our hospital, ‘drug-drug interaction’ was the third most common drug-related problem. This is likely due to irrelevant warnings and alert fatigue. Computerised physician order entry vendors should develop a CDSS that takes into account the prescribed dose. Local customisation and development of a more sophisticated CDSS are needed [24]. Moreover, CDSSs have to take into account the allergy recorded in the EHR.
In conclusion, the development of clinical pharmacy with pharmacists participating in medical rounds and being part of the medical staff and the real time computerisation of interventions by pharmacists in the EHR has led to an improved acceptance rate compared to 10 years ago. This encouraging trend shows the importance of regular training and collaboration with healthcare staff to reduce errors. The routine analysis of interventions by pharmacists with medical staff feedback should continue to improve their relevance and guarantee that they remain effective. Moreover, the development of targeted CDSSs, notably on the types of errors identified in this study, should help to reduce prescribing errors in hospitals using different processes or software.
Table S1 The 13 interventions by pharmacists excluded because they were not assessable by the French Society of Clinical Pharmacy tool.
| ATC | Interventions by pharmacists |
|---|---|
| A - Alimentary tract and metabolism | Gliclazide and rapid-acting insulin alone in type 2 diabetes. |
| Repaglinid prescription in free text: memo different from the prescription. | |
| B - Blood and blood forming organs | Heparin treatment to continue with preventive or curative dose. |
| C - Cardiovascular system | Prescription of perindopril in free text written as ‘do not give’. The prescriber meant: do not give if arterial tension is under 12 mm Hg. |
| Prescription of ramipril 5 mg until 24 November but it is not written in the hospital report. | |
| Nicardipine in electric syringe pump 1 mg in 1 ml instead of 50 mg in 50 ml. | |
| Heparin sodium in electric syringe pump: modification of the concentration. | |
| J - Anti-infectives for systemic use | efotaxim shortage: switch to ceftriaxone upon agreement of the microbiology team. |
| Cefotaxim shortage: switch to ceftriaxone upon agreement of the microbiology team. | |
| L - Antineoplastic and immunomodulating agents | Mitomycin C written ‘not in the therapeutic booklet’, whereas it is. |
| Hydroxycarbamide 100 mg is not in the therapeutic booklet. The SRN cannot administrate 800 mg by day because we only have tablets of 1000 mg. | |
| P- Antiparasitic products, insecticides and repellents | Handwritten prescription of caspofungin: wrong patient. |
Table S2 Description of the interventions concerning prescriptions rated as ‘life-threatening’ for the three main ATC classes concerned.
| ATC class | Drug-related problem | Interventions by pharmacists |
|---|---|---|
| A – Anti-infectives for systemic use | Non-conformity to guidelines/contra-indication | Prescription of piperacillin/tazobactam despite an allergy to penicillin (cutaneous rash) recorded in the electronic health record. |
| Non-conformity to guidelines/contra-indication | Prescription of piperacillin despite an allergy to penicillin (cutaneous rash) recorded in the electronic health record. | |
| Untreated indication | Shock septic care by piperacillin/tazobactam, metronidazole and gentamicin. Prescription of gentamicin only, order lines of piperacillin/tazobactam and metronidazole were for one day. | |
| Subtherapeutic dose | Prescription of vancomycin 20 mg/kg/day: drug dosage was too low. Modification of the prescription 23 mg/h (= 550 mg a day) instead of 23 mg/kg/day. | |
| Non-conformity to guidelines/contra-indication | Prescription of amoxicillin/clavulanate potassium despite an allergy to penicillin (angio-oedema) recorded in the electronic health record. | |
| Supratherapeutic dose | Prescription of amphotericin B 30 mg/kg/day instead of 3 mg/kg/day. | |
| Subtherapeutic dose | Prescription of cefotaxime 4 g 3 times a day instead of 4 g 4 times a day for a meningitis. | |
| Non-conformity to guidelines/contra-indication | Prescription of piperacillin/tazobactam despite an allergy to amoxicillin (unspecified) recorded in the electronic health record. | |
| Non-conformity to guidelines/contra-indication | Prescription of piperacillin despite an allergy to penicillin (anaphylactic shock) recorded in the electronic health record. | |
| Non-conformity to guidelines/contra-indication | Prescription of piperacillin despite an allergy to penicillin (unspecified) recorded in the electronic health record. | |
| Non-conformity to guidelines/contra-indication | Prescription of piperacillin/tazobactam despite an allergy to penicillin (unspecified) recorded in the electronic health record. | |
| Non-conformity to guidelines/contra-indication | Prescription of amoxicillin/clavulanate potassium despite an allergy to penicillin (unspecified) recorded in the electronic health record. | |
| Non-conformity to guidelines/contraindication | Prescription of amoxicillin despite an allergy to penicillin (positive toxidermia) recorded in the electronic health record. | |
| Non-conformity to guidelines/contra-indication | Prescription of amoxicillin despite an allergy to penicillin (unspecified) recorded in the electronic health record. | |
| Non-conformity to guidelines/contra-indication | Prescription of amoxicillin/clavulanate potassium despite an allergy to penicillin (unspecified) recorded in the electronic health record. | |
| Drug monitoring | Prescription of cotrimoxazole despite an allergy to cotrimoxazole (unspecified) recorded in the electronic health record. | |
| B - Blood and blood forming organs | Drug use without indication | Prescription in the perfusion of 4 g of potassium chloride in the rehydration whereas serum potassium of the day is 5.4 mmol/l. |
| Supratherapeutic dose | Prescription of clopidogrel 300 mg for 10 days instead of loading dose of clopidogrel 300 mg for one day followed by clopidogrel 75 mg. | |
| Drug use without indication | Prescription simultaneously of enoxaparin (low molecular weight heparin), rivaroxaban (direct oral anticoagulant) and fluindione (anti-vitamin K). | |
| Supratherapeutic dose | Prescription of clopidogrel 300 mg for 30 days instead of loading dose of clopidogrel 300 mg for one day followed by clopidogrel 75 mg. | |
| Supratherapeutic dose | Prescription of 2 electric syringe pumps of potassium chloride simultaneously (2 g and 4 g). | |
| Non-conformity to guidelines/contra-indication | Prescription of low molecular weight heparin despite a history of heparin-induced thrombocytopenia. | |
| Non-conformity to guidelines/contra-indication | Prescription of enoxaparin despite an allergy to enoxaparin (unspecified) recorded in the electronic health record. | |
| Subtherapeutic dose | Inappropriate heparin dosage for a patient with mechanical valve implant. | |
| N - Nervous system | Non-conformity to guidelines/contraindication | Prescription of diazepam in a patient with porphyria despite contraindication to the use of the drug according to website: https://www.porphyrie.net/medicaments/. |
| Non-conformity to guidelines/contra-indication | Prescription of tramadol despite a history of epilepsy under tramadol recorded in the electronic health record. | |
| Drug use without indication | Prescription of Hypnomidate® (etomidate) in electric syringe pump instead of Hypnovel® (midazolam). | |
| Non-conformity to guidelines/contra-indication | Prescription of tramadol/acetaminophen despite an allergy to tramadol (unspecified) recorded in the electronic health record. | |
| Non-conformity to guidelines/contra-indication | Prescription of tramadol despite an allergy to tramadol (unspecified) recorded in the electronic health record. | |
| Non-conformity to guidelines/contra-indication | Prescription of acetaminophen despite an allergy to acetaminophen (unspecified) recorded in the electronic health record. |
We would like to thank J. Camacho and J. Gariépy of the Department of Medical Information.
We would also like to thank the pharmacists T. Caruba, E. Jaccoulet, M. Nowak, D. Maramotti, and V. Savoldelli, and the residents at the study hospital for their cooperation in data collection and analysis.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Bates DW , Teich JM , Lee J , Seger D , Kuperman GJ , Ma’Luf N , et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc. 1999;6(4):313–21. doi:.https://doi.org/10.1136/jamia.1999.00660313
2 Charpiat B , Bedouch P , Conort O , Rose FX , Juste M , Roubille R , et al. Opportunités d’erreurs médicamenteuses et interventions pharmaceutiques dans le cadre de la prescription informatisée : revue des données publiées par les pharmaciens hospitaliers français [Opportunities for medication errors and pharmacist’s interventions in the context of computerized prescription order entry: a review of data published by French hospital pharmacists]. Ann Pharm Fr. 2012;70(2):62–74. Article in French. doi:.https://doi.org/10.1016/j.pharma.2012.02.002
3 Koppel R , Metlay JP , Cohen A , Abaluck B , Localio AR , Kimmel SE , et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293(10):1197–203. doi:.https://doi.org/10.1001/jama.293.10.1197
4 Villamañán E , Larrubia Y , Ruano M , Vélez M , Armada E , Herrero A , et al. Potential medication errors associated with computer prescriber order entry. Int J Clin Pharm. 2013;35(4):577–83. doi:.https://doi.org/10.1007/s11096-013-9771-2
5 Estellat C , Colombet I , Vautier S , Huault-Quentel J , Durieux P , Sabatier B . Impact of pharmacy validation in a computerized physician order entry context. Int J Qual Health Care. 2007;19(5):317–25. doi:.https://doi.org/10.1093/intqhc/mzm025
6 Conort O , Bedouch P , Juste M , Augereau L , Charpiat B , Roubille R , et al. Validation d’un outil de codification des interventions de pharmacie clinique. J Pharm Clin. 2004;23:141–7.
7 Caruba T , Boussadi A , Lenain E , Korb-Savoldelli V , Gillaizeau F , Durieux P , et al. A simulation study of the interception of prescribing errors by clinical pharmacists in an acute hospital setting. J Eval Clin Pract. 2015;21(4):673–80. doi:.https://doi.org/10.1111/jep.12363
8 Bobb A , Gleason K , Husch M , Feinglass J , Yarnold PR , Noskin GA . The epidemiology of prescribing errors: the potential impact of computerized prescriber order entry. Arch Intern Med. 2004;164(7):785–92. doi:.https://doi.org/10.1001/archinte.164.7.785
9 Bates DW , Cullen DJ , Laird N , Petersen LA , Small SD , Servi D , et al.; ADE Prevention Study Group. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. JAMA. 1995;274(1):29–34. doi:.https://doi.org/10.1001/jama.1995.03530010043033
10 Charpiat B , Conort O , Juste M , Rose FX , Roubille R , Bedouch P , et al. The French Society of Clinical Pharmacy ACT-IP© project: Ten years onward, results and prospects. Pharm Hosp Clin. 2015;50(2):e15–24. doi:.https://doi.org/10.1016/j.phclin.2015.04.006
11 Bedouch P , Sylvoz N , Charpiat B , Juste M , Roubille R , Rose F-X , et al.; French Society of Clinical Pharmacy’s Act-IP© Group. Trends in pharmacists’ medication order review in French hospitals from 2006 to 2009: analysis of pharmacists’ interventions from the Act-IP© website observatory. J Clin Pharm Ther. 2015;40(1):32–40. doi:.https://doi.org/10.1111/jcpt.12214
12 Blix HS , Viktil KK , Reikvam A , Moger TA , Hjemaas BJ , Pretsch P , et al. The majority of hospitalised patients have drug-related problems: results from a prospective study in general hospitals. Eur J Clin Pharmacol. 2004;60(9):651–8. doi:.https://doi.org/10.1007/s00228-004-0830-4
13 Kucukarslan SN , Peters M , Mlynarek M , Nafziger DA . Pharmacists on rounding teams reduce preventable adverse drug events in hospital general medicine units. Arch Intern Med. 2003;163(17):2014–8. doi:.https://doi.org/10.1001/archinte.163.17.2014
14 Bedouch P , Charpiat B , Conort O , Rose F-X , Escofier L , Juste M , et al. Assessment of clinical pharmacists’ interventions in French hospitals: results of a multicenter study. Ann Pharmacother. 2008;42(7–8):1095–103. doi:.https://doi.org/10.1345/aph.1L045
15 Bouchand F , Thomas A , Zerhouni L , Dauphin A , Conort O . [Pharmacists’ interventions before and after prescription computerization in an internal medicine department]. Presse Med. 1983;2007(36):410–8.
16 Ferracini AC , Rodrigues AT , de Barros AA , Derchain SF , Mazzola PG . Prescribing errors intercepted by pharmacist intervention in care of patients hospitalised with breast and gynaecological cancer at a Brazilian teaching hospital. Eur J Cancer Care (Engl). 2018;27(1).
17 Bedouch P , Tessier A , Baudrant M , Labarere J , Foroni L , Calop J , et al. Computerized physician order entry system combined with on-ward pharmacist: analysis of pharmacists’ interventions. J Eval Clin Pract. 2012;18(4):911–8. doi:.https://doi.org/10.1111/j.1365-2753.2011.01704.x
18 Vialle V , Tiphine T , Poirier Y , Raingeard E , Feldman D , Freville J-C . Connaître, comprendre et lutter contre les erreurs médicamenteuses induites par l’informatisation du circuit du médicament [To know, understand and combating medication errors related to computerized physician order entry]. Ann Pharm Fr. 2011;69(3):165–76. Article in French. doi:.https://doi.org/10.1016/j.pharma.2011.01.005
19 Abdel-Qader DH , Harper L , Cantrill JA , Tully MP . Pharmacists’ interventions in prescribing errors at hospital discharge: an observational study in the context of an electronic prescribing system in a UK teaching hospital. Drug Saf. 2010;33(11):1027–44. doi:.https://doi.org/10.2165/11538310-000000000-00000
20 Hellot-Guersing M , Jarre C , Molina C , Leromain A-S , Derharoutunian C , Gadot A , et al. Erreurs médicamenteuses induites par l’informatisation de la prescription à l’hôpital : recueil et analyse sur une période de 4ans [Medication errors related to computerized physician order entry at the hospital: Record and analysis over a period of 4 years]. Ann Pharm Fr. 2016;74(1):61–70. Article in French. doi:.https://doi.org/10.1016/j.pharma.2015.06.001
21 Korb-Savoldelli V , Boussadi A , Durieux P , Sabatier B . Prevalence of computerized physician order entry systems-related medication prescription errors: A systematic review. Int J Med Inform. 2018;111:112–22. doi:.https://doi.org/10.1016/j.ijmedinf.2017.12.022
22 Sellier E , Colombet I , Sabatier B , Breton G , Nies J , Zapletal E , et al. Effect of alerts for drug dosage adjustment in inpatients with renal insufficiency. J Am Med Inform Assoc. 2009;16(2):203–10. doi:.https://doi.org/10.1197/jamia.M2805
23 Slight SP , Eguale T , Amato MG , Seger AC , Whitney DL , Bates DW , et al. The vulnerabilities of computerized physician order entry systems: a qualitative study. J Am Med Inform Assoc. 2016;23(2):311–6. doi:.https://doi.org/10.1093/jamia/ocv135
24 Brown CL , Mulcaster HL , Triffitt KL , Sittig DF , Ash JS , Reygate K , et al. A systematic review of the types and causes of prescribing errors generated from using computerized provider order entry systems in primary and secondary care. J Am Med Inform Assoc. 2017;24(2):432–40. doi:.https://doi.org/10.1093/jamia/ocw119
No financial support and no other potential conflict of interest relevant to this article was reported.