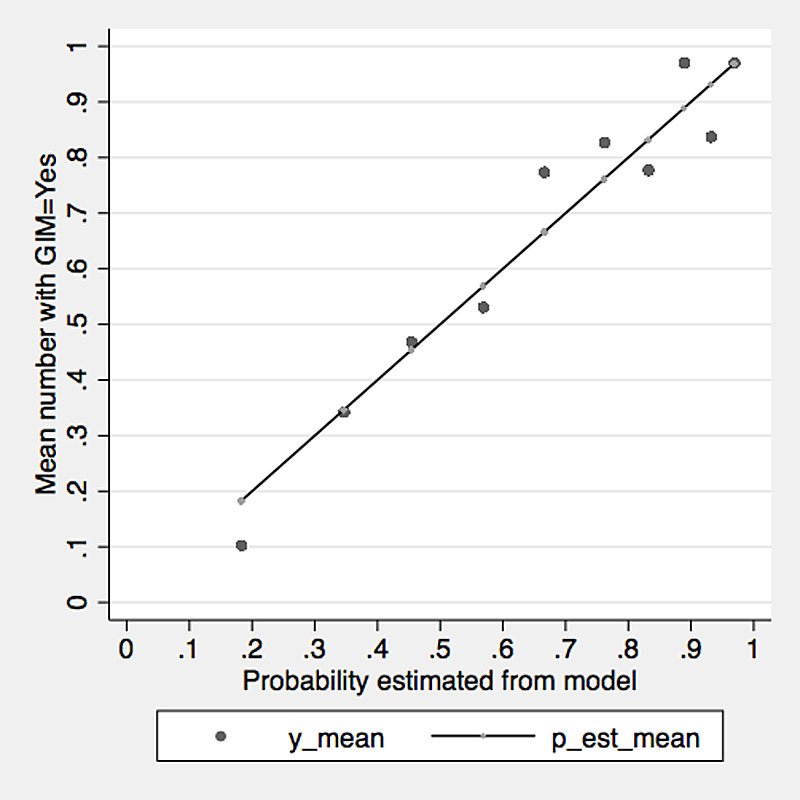
Figure 1 Predictions and actual counts by decile, based on the combined model of logistic regression with the variables named above.
DOI: https://doi.org/10.4414/smw.2018.14696
A new generation of physicians, millennials (also known as Generation Y), are entering residency programmes in internal medicine. These young men and women, born between 1980 and 2000, learn and work in ways that are different from past generations. Generation Y is defined by an increased grasp of technology, mobility and an ideology that seeks a balance in life [1]. In 2020 and 2025 they will account for 40% and 75% of the workforce, respectively [2]. Understanding the aspirations and expectations of millennials is essential, as the provision of medical services for the population depends on the medical specialties in which doctors choose to pursue a career. Switzerland, like many other Western countries, faces a shortage of physicians, particularly of general practitioners (GPs). Even though the number of GPs increased by 30% from 2008 to 2016, the increase was mainly due to the fact that many GPs continue to work beyond the official retirement age [3, 4]. Currently, the ageing GP population in Switzerland has a shortage of 2,000 physicians, a situation that will get worse by 2025, by which time 60% of GPs will have retired. At that time, Switzerland will be about 5000 GPs short [5]. Concurrently with the lack of GPs, a shortage of internists is also emerging. Recently, the Swiss Society of General Internal Medicine reported a reduced attractiveness of generalist careers [6]. The society stated that the continuation of this medical specialty, and therefore inpatient and outpatient care, is under threat, and it launched a campaign to enhance the attractiveness of internal medicine and to promote the next generation of physicians [6]. Factors such as curricular planning of postgraduate training, mentoring and career counselling, as well as requirements such as more time for patient care and the reduction of administrative burden were identified as important for attracting young physicians to this specialty [6].
Several studies have shown that residency is more important than medical school for career decisions [7, 8]. However, little is known as to the criteria used by the current generation of postgraduate physicians working in residency facilities in general internal medicine when choosing a career in general medicine or in an internal medicine subspecialty. Several factors have been identified, including gender, lifestyle (personal time free of practice requirements for leisure, family and non-vocational pursuits, and control of total weekly hours spent on professional responsibilities), prestige, social status and financial incentives [8–10]. Length, quality and structure of residency programmes and mentorship are also factors mentioned in the context of choosing a specialty [7, 11].
In Switzerland, the content of postgraduate training in internal medicine and its subspecialties is determined by the Swiss Institute for Advanced Medical Training and Education (SIWF, Schweizerisches Institut für ärztliche Weiter- und Fortbildung) together with specialist bodies. Head physicians, together with senior physicians, are responsible for implementing the postgraduate training concepts within their departments. Advanced training in internal medicine generally lasts 5 years, consisting of 3 years of basic training in general internal medicine (“common trunk”) and two years of individually selectable training positions (e.g. “specialisation” in hospital medicine vs family medicine). Depending on the medical subspecialty (SUB), training takes another 3–4 years after the “common trunk.” Swiss trainees must also meet other requirements, such as passing a national examination and completing required courses [12].
The aim of the present study was to investigate the attractiveness to young residents of a career in general internal medicine (GIM) compared with medical subspecialties (SUB). First, we hypothesised that young residents choose their medical career in conjunction with decisions concerning their work-life balance and capacity for family and/or private life. Second, we hypothesised that female residents are more likely than male residents to choose a career in general internal medicine (GIM) without a subspecialty. We also aimed to investigate the difference between future physicians in internal medicine and physicians aspiring to a medical subspecialty in terms of mentoring, as well as sociodemographic factors and variables concerning personality factors, career motivation, importance of life goals and work-life balance.
A cross-sectional online survey was completed by residents working in residency facilities in GIM in German-speaking Switzerland. The survey took place between 16 January 2017 and 28 February 2017. We selected residency facilities in GIM at hospitals and institutions approved by the SIWF [13]. Accordingly, 146 head physicians at residency facilities in GIM in German-speaking Switzerland (67% of all residency facilities in GIM at hospitals and institutions in Switzerland) were sent an e-mail explaining the aim and purpose of the survey. The head physicians were asked to forward the e-mail, with a link to the online survey, to their junior residents. In this way, a potential 1818 junior residents were addressed (66% of all junior residents at residency facilities in GIM in Switzerland). A reminder was sent by e-mail on 12 February 2017. We received 403 responses. Eleven responses had to be excluded because they were incomplete or not interpretable. In total, 392 junior residents completed the survey, which corresponds to a response rate of about 22%.
The online survey was designed in three parts. In the first part, we asked for respondents’ sociodemographic characteristics, i.e., age, sex, medical school, year of graduation, experience in research, clinical experience and family characteristics.
In the second part, we asked about: the specialty and/or subspecialty for which the respondent wanted to qualify, the career aspired to (medical practice, hospital or academic career), important criteria in the choice of medical specialty (each on a five-point Likert-type scale), and mentoring during their residency. The following “medical specialties” were subsumed under SUB: angiology, immunology, occupational medicine, endocrinology, gastroenterology, haematology, infectious diseases, intensive care, cardiology, pharmacology, medical oncology, nephrology, pulmonology, and rheumatology.
The third part contained instruments measuring personality and career-related factors for the purpose of comparison with the findings by Buddeberg [8, 10]. These comprised: The Sense of Coherence Scale (SOC) [14], measuring a person’s resistance and ability to manage stress; the Career Motivation Questionnaire (CMQ) [15] on a person’s general career motivation; the Occupational Self-Efficacy Expectation (Berufliche Selbstwirksamkeitserwartung, BSW) [16], a five-point Likert-type scale; and the Life Goals Questionnaire (GOALS) [17], a five-point Likert-type scale.
Finally, the person’s work-life balance, life expectations and future aspirations were assessed [10].
Data were collected using Unipark online software (www.unipark.de) and transferred to a spreadsheet in Microsoft Excel Version 2010 (Redmond, WA, USA). We managed data and conducted statistical analyses using Stata Statistical Software: Release 13 (StataCorp, College Station, TX, USA) and IBM SPSS Statistics Version 22 (IBM Corp, Armonk, NY, USA) for the personality and career-related factors. Chi-square and Fisher tests were used to compare counts and the t-test was used for continuous data. We chose a significance level of 0.05, two-sided.
In view of the research questions, data were analysed mainly by two covariates: the medical specialty aspired to (GIM or SUB) and gender. First, we did bivariate tabulations of all collected variables in the survey by these covariates. Second, we analysed factors that might be causally related to career choice. To assess the simultaneous effect of several variables accounting for mutual correlations, we applied stepwise logistic regression to the response “medical specialty”. Initially, all variables discriminating significantly (p <0.05) between the GIM and SUB groups were included. As the probability of inclusion, we chose, accordingly, p <0.05. Variables were excluded if p >0.10. See also supplementary table S1, appendix 1.
According to current Swiss law on human research (Humanforschungsgesetz, HFG), the analysis of data that are collected anonymously and not patient-related does not require approval by local ethics committees. The data in this study were collected anonymously (only age and gender, no hospital affiliation).
Of the residents participating in the survey (n = 392), 66.3% were women (table 1). The mean age of the population was 31.5 years (standard deviation [SD] 3.8), with a range of 25 to 47 years. On average, the residents had graduated from medical school 4.8 years prior to taking the survey, and 38% had a medical degree from outside Switzerland. By the time of the survey, the physicians had been in clinical training for 35.5 months on average, and of these, 26.1 months were in internal medicine on average. A quarter of the residents (25.3%) had worked in clinical research full-time, with an average duration of 11 months.
Table 1 Population characteristics of the residents working in a training facility in internal medicine in German-speaking Switzerland and participating in the survey (n = 392).
| Gender (%) | |
| Male | 33.7 |
| Female | 66.3 |
| Age (years, mean) | 31.5 (SD 3.8) |
| Age, range | 25–47 |
| University education (%) | |
| German-language university in Switzerland | 59.4 |
| French-language university in Switzerland | 2.6 |
| University outside Switzerland | 38.0 |
| Time since state examination (year, mean) | 4.8 (SD 2.8) |
| Work experience (months) | |
| Clinical experience | 35.5 (SD 27.3) |
| Experience in internal medicine | 26.1 (SD 21.2) |
| Employment (%) | |
| 100% employment FTE | 87.3 |
| 80% employment | 4.3 |
| <80% employment | 8.4 |
| First title of specialisation already acquired (%) | |
| Yes | 9.4 |
| No | 90.6 |
| Targeted specialisation (first and second, in %) | |
| General internal medicine | 57.9 |
| Subspecialty | 28.8 |
| Other, non GIM specialty | 13.3 |
| Living with a partner/spouse (%) | |
| Yes | 76.8 |
| No | 23.2 |
| Children (%) | |
| Yes | 16.1 |
| No | 83.9 |
| Family planned in the future (%) | |
| Yes | 80.9 |
| No | 5.1 |
| Unclear | 14.0 |
| FTE = full-time equivalent; GIM = general internal medicine; SD = standard deviation | |
Of all residents, 87.3% worked full-time, 4.3% worked 80%, and 8.4% less than 80%. With regard to gender, 96.2% of male and 82.7% of female residents worked full-time. 44.6% found their working time higher than they wished. 41.4% wanted to reduce working time by 20% or more.
Asked about their choice of medical specialty, 9.4% (n = 37) of the residents stated that they had already qualified in GIM (81.1% of the 37), 86.7% (n = 340) of the residents aspired to qualify in GIM, and 113 (28.8%) of these aspired to a subspecialty (SUB). 13.2% (52) had not made up their mind at this point in time or were aiming for another specialty such as anaesthesiology, paediatrics or other. 71% (n = 164) of female residents chose GIM and not a SUB vs 57.8% (N = 63) of the male residents (Fisher, p <0.019).
Of the 392 residents participating in the survey, 33.2% (n = 130) aimed for a career in hospital, 37.2% (n = 146) in private practice, 6.9% (n = 27) in academic research (including completing the postdoctoral qualification [habilitation]), and 1% (n = 4) in the pharmaceutical industry. 21.7% (n = 85) were still unclear about their career goals, with no statistical differences by gender and/or medical specialty. Female GIM residents saw their future work environment primarily in private practice (50.0%) or in hospital (26.2%). This relationship was inverted for female SUB residents (p = 0.0005), who preferred working in hospital (47.8%) and in private practice (20.9%). In contrast, no statistical differences in these preferences were found for male residents (p = 0.055).
The criteria most often mentioned in favour of choosing a medical specialty were “a clear interest in the field” (99.5%), “a good working environment/atmosphere” (97.9%), “a good learning atmosphere” (93.9%) and a “good work-life balance” (91.6%).
GIM residents rated “broad range of expertise” (p = 0.016), “flexible work hours” (p = 0.007), “work-life balance” (p = 0.032) and “reconciliation of work, family and private life” (p = 0.011) higher than residents aiming at a SUB did (table 2).
Table 2 Criteria for the choice of medical specialty by medical qualification aimed for (n = 339) and by gender (n = 392). Each criterion was rated on a scale from 1 “not important,” to 3 “neutral,” to 5 “very important.” The table shows mean scores, standard deviations (SD), and the p-value by the covariates reported.
| Question 16, single items | General internal medicine (GIM) | Subspecialty (SUB) | p-value | GIM < SUB | Females | Males | p-value | Females < males |
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||||
| Interest in the field | 4.84 (0.37) | 4.90 (0.33) | 0.107 | 4.86 (0.36) | 4.85 (0.38) | 0.749 | ||
| Broad range of expertise | 4.36 (0.74) | 4.14 (0.85) | 0.016 | Yes | 4.27 (0.79) | 4.19 (0.88) | 0.396 | |
| Lead in treating multimorbid patients | 3.17 (0.99) | 2.98 (1.06) | 0.105 | 3.17 (0.99) | 2.80 (1.07) | 0.001 | Yes | |
| Flexible work hours | 4.04 (0.83) | 3.76 (0.97) | 0.007 | Yes | 4.03 (0.87) | 3.80 (0.92) | 0.015 | Yes |
| Low bureaucracy | 3.83 (0.90) | 3.76 (0.98) | 0.432 | 3.81 (0.93) | 3.93 (0.88) | 0.220 | ||
| Good working environment/atmosphere | 4.71 (0.48) | 4.70 (0.62) | 0.909 | 4.73 (0.47) | 4.71 (0.60) | 0.772 | ||
| Salary potential/earning capacities | 3.37 (0.90) | 3.42 (1.05) | 0.658 | 3.30 (0.91) | 3.51 (1.00) | 0.131 | ||
| Social prestige | 2.54 (1.03) | 2.50 (1.05) | 0.812 | 2.48 (0.99) | 2.71 (1.12) | 0.037 | No | |
| Work-life balance | 4.56 (0.60) | 4.39 (0.74) | 0.032 | Yes | 4.55 (0.61) | 4.37 (0.73) | 0.010 | Yes |
| Job security | 3.91 (0.83) | 3.87 (0.94) | 0.629 | 3.94 (0.82) | 3.88 (0.94) | 0.577 | ||
| Social commitment | 3.62 (0.85) | 3.52 (0.97) | 0.315 | 3.70 (0.89) | 3.30 (0.85) | <0.0001 | Yes | |
| Good learning atmosphere | 4.33 (0.67) | 4.64 (0.65) | 0.155 | 4.47 (0.65) | 4.37 (0.67) | <0.0001 | Yes | |
| Research activities | 2.34 (1.08) | 3.18 (1.11) | <0.0001 | No | 2.61 (1.20) | 2.64 (1.07) | 0.833 | |
| Career opportunities | 2.96 (1.04) | 3.51 (0.93) | <0.0001 | No | 3.08 (1.04) | 3.33 (0.98) | 0.022 | No |
| Opportunities for habilitation | 2.11 (1.05) | 2.82 (1.10) | <0.0001 | No | 2.35 (1.09) | 2.42 (1.14) | 0.530 | |
| Well-structured curriculum | 3.82 (0.95) | 4.20 (0.83) | <0.0004 | No | 3.96 (0.88) | 3.93 (0.95) | 0.733 | |
| Short medical training period | 2.99 (1.02) | 3.03 (1.03) | 0.764 | 3.07 (0.99) | 2.88 (1.06) | 0.076 | ||
| Reconciliation of work, family and private life | 4.39 (0.84) | 4.12 (1.05) | 0.011 | Yes | 4.31 (0.92) | 4.20 (0.87) | 0.272 | |
| Manual and interventional tasks | 3.71 (0.88) | 3.81 (1.04) | 0.363 | 3.76 (0.95) | 3.82 (0.91) | 0.557 | ||
| Opportunity to work independently | 3.90 (0.88) | 4.10 (1.04) | 0.015 | No | 4.01 (0.71) | 3.90 (0.81) | 0.138 |
The SUB residents evaluated career-related criteria (“research activities”, “career opportunities”, “opportunities for an academic career”) as significantly more important than GIM residents did (p <0.0001). Moreover, “a well-structured curriculum” (p <0.0001) and the “opportunity to work independently” (p = 0.015) were more important criteria to them than to GIM residents.
Regarding gender differences, female residents rated the criterion of “having the lead in treating multimorbid patients” as significantly more important than male residents did (p = 0.001). Furthermore, “work-life balance” (p = 0.010), “flexible work hours” (p = 0.015) and “social commitment” (p <0.0001) were significantly more important to female residents, whereas male residents rated “social prestige” (p = 0.037), “a good learning atmosphere” (p <0.0001) and “career opportunities” (p=0.022) as more important than female residents did.
Thirty-five percent (n = 137) of the junior physicians had experience with a mentor. There was a sizeable difference in the percentage with mentoring between GIM and SUB residents (28.2 vs 49.6%, p <0.0005). In general, male residents reported having had significantly more career talks than female residents did (89.0 vs 80.0%, p = 0.0409) in the last 12 months, most having had one talk within a year (48.4 vs 40.7%). However, there was no gender difference in the availability of career talks by medical specialty (p = 0.8722). Of the 35% of junior physicians who had experience with a mentor, 63.5% (n = 87) rated mentoring in their career planning as supportive. Among physicians not yet having had experience with a mentor, 84.7% (n = 216) expected that mentoring would be helpful for their career planning.
When testing for various personality and career related factors, we found only a few differences by medical specialty and gender (table 3). There were no statistically significant differences in sense of coherence (SOC) and occupational self-efficacy expectation by either medical specialty or gender.
Table 3 Personality and career related factors; importance of life goals by medical specialty (n = 340) and by gender (n = 392) (Buddeberg-Fischer et al. 2006 [8]). The table shows mean scores, standard deviations (SD) and p-values.
| General internal medicine (GIM) | Subspecialty (SUB) | p-value | Females | Males | p-value | |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Sense of Coherence | ||||||
| SOC | 4.93 (0.04) | 4.87 (0.69) | 0.366 | 4.97 (0.04) | 4.85 (0.72) | 0.112 |
| Occupational Self-Efficacy Expectation | ||||||
| BSW | 3.67 (0.68) | 3.71 (0.64) | 0.633 | 3.64 (0.67) | 3.77 (0.69) | 0.083 |
| Career Motivation* | ||||||
| CMQ Intrinsic motivation | 5.90 (0.66) | 6.06 (0.51) | 0.025 | 5.94 (0.60) | 5.94 (0.74) | 0.955 |
| CMQ Extrinsic motivation | 3.91 (0.90) | 4.01 (0.80) | 0.090 | 3.96 (0.89) | 4.04 (0.82) | 0.349 |
| CMQ Extraprofessional concerns | 4.64 (0.91) | 4.40 (0.82) | 0.019 | 4.59 (0.90) | 4.39 (0.90) | 0.039 |
| Importance of Life Goals† | ||||||
| Intimacy | 4.50 (0.49) | 4.46 (0.51) | 0.553 | 4.53 (0.49) | 4.36 (0.52) | 0.003 |
| Affiliation | 3.69 (0.73) | 3.50 (0.69) | 0.026 | 3.67 (0.72) | 3.59 (0.75) | 0.295 |
| Altruism | 3.87 (0.65) | 3.93 (0.66) | 0.394 | 3.96 (0.69) | 3.77 (0.69) | 0.005 |
| Power | 2.68 (0.82) | 2.80 (0.85) | 0.210 | 2.66 (0.82) | 2.86 (0.86) | 0.025 |
| Achievement | 4.31 (0.49) | 4.37 (0.48) | 0.362 | 4.35 (0.03) | 4.29 (0.50) | 0.306 |
| Variation | 3.89 (0.74) | 3.87 (0.75) | 0.833 | 3.89 (0.74) | 3.95 (0.76) | 0.468 |
* Career motivation: intrinsic motivation (i.e., enjoying and interest in professional activities), extrinsic motivation (i.e., striving for promotion, income, prestige), extraprofessional concerns (i.e., starting a family, convenient working hours, job security as a priority) † Importance of life goals - six major life domains: intimacy (close relationship based on mutual trust and affection), affiliation (spending time with other people, common activities), altruism (acting for the welfare of others), power (ascertaining oneself, seeking social status), achievement (improving on oneself, meeting standards) and variation (seeking new experiences and excitement).
Regarding their career motivation, GIM residents rated extraprofessional concerns significantly higher than SUB residents (p = 0.019). In contrast, SUB residents scored significantly higher on intrinsic motivation than GIM residents (p = 0.025). In both cases, the differences were small. Above all, there was no difference in extrinsic motivation (i.e., striving for promotion, income, prestige) between the two specialties or between men and women.
When we looked for variations in life goal settings, the only statistical difference by medical specialty found was for “affiliation”, with GIM residents putting more weight on this criterion than SUB residents (p = 0.026). Overall, there were no significant differences in personality traits by specialty. Nevertheless, we found some significant gender effects. Female residents put significantly more emphasis on “intimacy” (p = 0.003) and “altruism” (p = 0.005). For male residents, “power” (p = 0.025) as a life goal was significantly more important.
When asked about their work-life balance, 47.7% of female residents reported a good work-life balance compared to 39.4% of male residents. However, no gender effect (p = 0.133) and no differences between the two specialties were found (p = 0.818, data not shown).
Concerning personal perceptions of the future in the next five years (table 4), GIM residents rated “part-time work to have more private time” higher than SUB residents did (p = 0.001), whereas SUB residents rated finding a “leading position as a main goal” (p = 0.000) higher.
Table 4 Perceptions of the future in the next 5 years, by medical specialty (n = 340) and by gender (n = 392). Scale from 1 “not at all” to 5 “completely”. The table shows mean scores, standard deviations (SD) and p-values.
| Items | General internal medicine (GIM) | Subspecialty (SUB) | p-value | Females | Males | p-value |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Leading position as a main goal | 2.22 (1.11) | 2.95 (1.14) | 0.000 | 2.40 (1.14) | 2.70 (1.17) | 0.013 |
| Challenges at work but also time for other things | 4.74 (0.55) | 4.71 (0.54) | 0.614 | 4.76 (0.54) | 4.63 (0.63) | 0.031 |
| Part-time work to have more private time | 4.46 (0.87) | 4.09 (1.17) | 0.001 | 4.41 (0.98) | 4.14 (1.10) | 0.014 |
| May leave work to do something else | 1.97 (1.10) | 1.90 (1.15) | 0.557 | 1.86 (1.11) | 2.10 (1.11) | 0.044 |
| Reduction of work to temporarily have more family time | 3.45 (1.25) | 3.19 (1.30) | 0.072 | 3.37 (1.33) | 3.17 (1.18) | 0.133 |
Regarding gender differences, female residents aimed more often for a good balance between “challenges at work but also time for other things” (p = 0.031) and “part-time work to have more private time” (p = 0.014). For male residents, finding a “leading position as a main goal” (p = 0.013) and “may leave work to do something else” (p = 0.044) were more important than for female residents.
The results presented in tables 2 to 4 and in the text above give a first overview of which factors might be causally related to career choice. In the second step, we computed a stepwise logistic regression using the response “probability of aspiring to a GIM career.” We found that only about half of the variables that were individually significant remained significant in the regression, i.e. when accounting for mutual correlations between factors (supplementary table S1, appendix 1).
Significant variables in the logistic regression were age, gender, and the importance attached to the items “career goals”, “broad range of expertise”, “opportunity to work independently”, “research activities”, “reconciliation of work, family and private life” and the availability and use of a “mentor.” These factors resulted in a combined model that was useful to predict whether residents would choose a GIM or SUB career. Figure 1 shows the quality of fit observed with this model. Estimated probabilities correlate well in the range 20% to 90%. For probabilities below 20% and above 90%, sufficient information for a model check was not available.
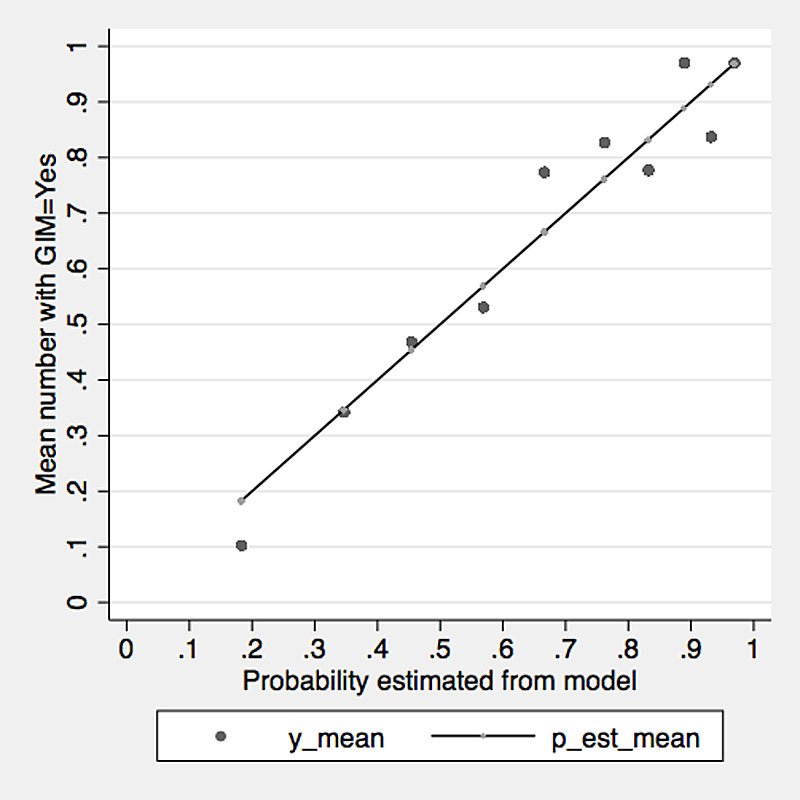
Figure 1 Predictions and actual counts by decile, based on the combined model of logistic regression with the variables named above.
A closer examination showed that in our sample, women and older residents (age) were more likely to aspire to a GIM career. Furthermore, physicians who attached importance to “a broad range of expertise” as well as “reconciliation of work, family and private life” and sought personal “affiliation” were more likely to aspire to a GIM career. The availability of a mentor had a positive effect on the inclination to choose GIM.
On the other hand, a high rating for the “opportunity to work independently” and the availability of research activities were less important to residents aspiring to a GIM career than to residents aspiring to a SUB career (i.e., if those factors were important to a resident, he/she was less likely to aim for a career in GIM). Considering the quality of the prediction of a GIM career (fig. 1), the model predicts probabilities between 20% and 90%, i.e., a large part of the range of probabilities is covered.
Although reduced attractiveness of a generalist career is a significant issue, little is known about the factors influencing the choice of career in this medical specialty. In this study, we therefore looked for personal preferences, characteristics and criteria influencing the choice of a career in GIM or SUB on the basis of a survey of young residents at residency facilities in German-speaking Switzerland. Our findings revealed several differences in the factors analysed that may be meaningful and perhaps even modifiable.
Half of the residents in our survey are not satisfied with their work-life balance, independent of gender and specialty choice. One reason might be that the workload of residents is high: although an official weekly working time of 50 hours for residents was introduced in 2005, the average working time in was still 56 hours per week in 2016 [18]. Many residents in internal medicine cannot fulfil their duties in the scheduled time. In a time and motion study by Wenger et al. with internal medicine residents in a Swiss university hospital, day shifts lasted 1.6 hours longer on average than the official 10 hours scheduled [19]. Adequate work-life balance is an issue of growing importance for the millennial generation [10, 20, 21]. Millennials are highly committed to their work but want sufficient time for private and family activities. It is reasonable to assume that this generation tends to blend personal interests into the workday, and work activities into the evening [21]. Thus, residency programme directors must find innovative ways to provide patient care whilst allowing residents the time for rest and family [21].
To enhance the attractiveness of internal medicine, work content should also be modified. Internal medicine residents spend their working day mainly on activities indirectly related to patients [19]. Less bureaucracy, through the use of support personnel (e.g., care coordinators), and more manual tasks, such as ultrasound and invasive bedside procedures, could upgrade the profession of GIM [22, 23]. The Swiss Society of General Internal Medicine intends to continue implementing these points in a catalogue of measures to convey a positive image of GIM [23].
The proportion of women in GIM has increased greatly over the last 20 years, which is sometimes referred to as “the feminisation” of this medical specialty [4]. In our survey, two thirds of the respondents were women. They rate part-time work and flexible work hours as very important criteria for their choice of discipline. The results thus indicate that the attractiveness of a career in GIM could be enhanced by developing and implementing flexible working time models.
This study shows that residents aiming at a clinical and/or academic career are more likely to choose SUB. In the past, academic research took place predominantly in SUB, in particular with basic science as the gold standard [24]. Today, chronic conditions and multimorbidity offer attractive new research opportunities. Patient-oriented clinical research benefitting people with multiple acute and chronic conditions will actively contribute to a more cost-effective health system, and could at the same time offer research opportunities to GIM-oriented residents. These topics need to be addressed and funded in a new GIM research agenda [25]. Also, corresponding research structures have to be implemented and funded in order to attract intrinsically motivated young doctors with academic ambitions to a career in GIM.
To address the shortage of internists in the near future, junior physicians interested in GIM should have easy access to guidance and career-relevant information through a well-structured curriculum. One problem is that young doctors usually get contracts for up to two years. There is a lack of structure and coordination, i.e., a lack of a continuous sequence of increasingly demanding tasks for the whole duration of residency. Thus, a training track for residents interested in an academic career in GIM should be established and coordinated across several hospitals and general practices, and it should include protected time for research.
Receiving feedback is important to millennials [21], and it can be assumed that they are more interested in mentorship than previous generations [26]. In our survey, less than a third of GIM residents had a mentor, in contrast to SUB residents, 50% of whom had mentors. From an internist’s point of view, this result is worrying, as in academic medicine, mentoring has an important influence on personal development, career choice, career guidance and research productivity [27]. Specialist bodies (e.g., the Swiss Society of Internal Medicine) or head physicians should play a more active role in mentoring junior physicians. Funding and protected time for mentoring might be a successful approach to honouring the time cost of mentorship [28]. Another reason for the low number of mentees might be that mentorship strategies for millennial residents are not well understood [29]. This may result in frustration, miscommunication and attrition in mentor-mentee dyads [29]. From this perspective, it may not be surprising that in our survey, residents with no mentoring experience expected mentoring to be more helpful for their career than the group of residents with the experience of a mentor did.
With the higher proportion of women in GIM and the expectations of millennials towards working conditions, medical training should moreover not only focus on the professional career, but also consider extraprofessional issues such as flexible work hours and work-life balance. New forms of mentoring may need to be tested, as some millennials tend to have multiple mentors: the traditional older managers, but also peer mentors and coaches [26].
Gender has an impact on the criteria for choice of specialty, career motivation (intrinsic vs extraprofessional motivation) and the importance of life goals (affiliation, e.g., spending time with other people, common activities), but not on the sense of coherence or occupational self-efficacy expectation. There were only minor differences in personality traits, career motivation and importance of life goals between GIM and SUB residents in our survey. The scores in our survey were equivalent to the scores of Swiss physicians in their fourth year of residency who aspired to primary care and internal medicine more than 10 years ago [8]. In the study by Buddeberg et al., there was no further subgrouping of physicians who aspired to an internal medicine subspecialty [8]. In 2008, a survey by Buddeberg et al. of Swiss residents in their fifth to sixth year of training found that future family physicians (who included residents aspiring to GIM) rated intrinsic and extrinsic career motivation lower and extraprofessional concerns higher than specialists [10]. Buddeberg et al. concluded that family physicians like their job, but that family, friends and leisure activities are equally important to them. This may be in contrast to the previous generation of family physicians, who often regarded their profession as a vocation and sacrificed themselves for their patients [10, 30].
Our study has several limitations, the main limitation being the low response rate of 22%. This is not unusual for social surveys, however. Second, two thirds of the respondents were women. On a basic level, our sample evidently reflects women’s views more than men’s. In 2017 in German-speaking Switzerland, 67% of the specialist titles awarded in GIM went to females [4], i.e., a similar percentage.
Third, the respondents were mainly residents aiming towards a GIM career. These facts may contribute to a selection bias. Nevertheless, the similarity of our results with those of Buddeberg et al. limit the extent of selection bias [8]. Moreover, the regression model shows that many factors beyond gender alone affect the professional choices of residents towards either GIM or SUB.
Another limitation is that this study is based on self-reported data: there may be effects of social desirability or recall bias, etc.
On the positive side, the responses were collected anonymously. Other studies in this field report similar findings to those in our study, suggesting that the current issues in GIM are pervasive. In addition, it is worth mentioning that the logistic regression model shows that many of the variables collected contribute to discriminating between the wish to pursue a GIM or a SUB career.
There are considerable differences between GIM and SUB residents regarding career motivation and their views on working conditions and work-life balance. It is essential to understand the factors that motivate or deter the next generation in order to ensure the attractiveness of the profession of GIM.
Table S1 Logistic regression including all factors showing a significant difference between GIM and SUB residents. Response: probability of choosing GIM over SUB; n = 327; likelihood ratio for whole model: 94.50 on 13 df (p <0.005); pseudo R2 = 0.23.
| Covariable | Coef. | SD | z-value | p-value | 95% CI | |
|---|---|---|---|---|---|---|
| Career aim: academic (reference category) | 1.000 | 0.000 | – | – | – | – |
| Career aim: work in hospital | −0.941 | 0.554 | −1.7 | 0.09 | −2.027 | 0.146 |
| Career aim: general practice | 0.103 | 0.612 | 0.17 | 0.867 | −1.096 | 1.301 |
| Career aim: undecided | −0.369 | 0.589 | −0.63 | 0.531 | −1.522 | 0.785 |
| Age | 0.097 | 0.039 | 2.49 | 0.013 | 0.021 | 0.173 |
| Gender | −0.698 | 0.294 | −2.37 | 0.018 | −1.275 | −0.122 |
| Satisfaction with private life | −0.146 | 0.084 | −1.74 | 0.082 | −0.311 | 0.019 |
| Broad range of expertise | 0.592 | 0.184 | 3.22 | 0.001 | 0.232 | 0.951 |
| Life goals: affiliation | 0.410 | 0.210 | 1.96 | 0.051 | −0.001 | 0.821 |
| Reconciliation of work and family | 0.373 | 0.172 | 2.17 | 0.03 | 0.036 | 0.710 |
| Research activities | −0.506 | 0.148 | −3.41 | 0.001 | −0.796 | −0.215 |
| Mentoring | 0.625 | 0.288 | 2.17 | 0.03 | 0.061 | 1.188 |
| Opportunity to work independently | −0.660 | 0.205 | −3.23 | 0.001 | −1.062 | −0.259 |
| Well-structured curriculum | −0.313 | 0.180 | −1.74 | 0.081 | −0.665 | 0.039 |
The authors thank Prof. Barbara Buddeberg-Fischer and Prof. Richard Klaghofer for support in the design of the trial and analyses of the data.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Mitchell DA . Generation Z--striking the balance: healthy doctors for a healthy community. Aust Fam Physician. 2008;37(8):665–7.
2 Waljee JF , Chopra V , Saint S . Mentoring Millennials. JAMA. 2018;319(15):1547–8. doi:.https://doi.org/10.1001/jama.2018.3804
3 Hostettler S , Kraft E . FMH-Ärztestatistik 2016 – 36175 berufstätige Ärztinnen und Ärzte. Schweiz Arzteztg. 2017;98(13):394–400. doi:.https://doi.org/10.4414/saez.2017.05522
4fmh.ch. [Internet]. Bern: Swiss Medical Association [cited 2018 June 03]. FMH-Ärztestatistik. Available from: https://www.fmh.ch/services/statistik/aerztestatistik.html
5hausaerzteschweiz.ch. [Internet]. Bern: Haus- und Kinderärzte Schweiz [cited 2018 June 3]. Zeller A, Tschudi B. Medizinische Grundversorgung: Neue Studie prognostiziert rasant steigenden Hausarztmangel mit hohen Kostenfolgen, 31 March 2016. Available from: http://www.hausaerzteschweiz.ch/fileadmin/user_upload/hausaerzteschweiz/Dokumente/Tag_der_Hausarztmedizin/mfe_Medienmitteilung_310316_D.pdf
6sgaim.ch. [Internet]. Bern: Swiss Society of General Internal Medicine [cited 2018 June 3]. Offensive für mehr ärztlichen Nachwuchs in der Allgemeinen Inneren Medizin, 1 December 2017. Available from: http://www.sgaim.ch/nc/de/meta/mediennews/newsdetail/news/offensive-fuer-mehr-aerztlichen-nachwuchs-in-der-allgemeinen-inneren-medizin.html
7 Tandjung R , Senn O , Marty F , Krauss L , Rosemann T , Badertscher N . Career after successful medical board examination in general practice--a cross-sectional survey. Swiss Med Wkly. 2013;143:w13839. doi:.https://doi.org/10.4414/smw.2013.13839
8 Buddeberg-Fischer B , Klaghofer R , Abel T , Buddeberg C . Swiss residents’ speciality choices--impact of gender, personality traits, career motivation and life goals. BMC Health Serv Res. 2006;6(1):137. doi:.https://doi.org/10.1186/1472-6963-6-137
9 Jones L , Fisher T . Workforce trends in general practice in the UK: results from a longitudinal study of doctors’ careers. Br J Gen Pract. 2006;56(523):134–6.
10 Buddeberg-Fischer B , Stamm M , Buddeberg C , Klaghofer R . The new generation of family physicians--career motivation, life goals and work-life balance. Swiss Med Wkly. 2008;138(21-22):305–12. doi:.https://doi.org/10.4414/smw.2008.12103
11 Studerus L , Ahrens R , Häuptle C , Goeldlin A , Streit S . Optional part-time and longer GP training modules in GP practices associated with more trainees becoming GPs - a cohort study in Switzerland. BMC Fam Pract. 2018;19(1):5. doi:.https://doi.org/10.1186/s12875-017-0706-1
12siwf.ch. [Internet]. Bern: Allgemeine Innere Medizin: Schweizerisches Institut für ärztliche Weiter- und Fortbildung [cited 2018 June 3]. Available from: https://www.fmh.ch/bildung-siwf/fachgebiete/facharzttitel-und-schwerpunkte/allgemeine-innere-medizin.html
13siwf-register.ch. [Internet]. Bern: Allgemeine Innere Medizin: Schweizerisches Institut für ärztliche Weiter- und Fortbildung [cited 2018 August 25]. Available from: https://www.siwf-register.ch/
14Abel T, Kohlmann T. Der Fragebogen zum Kohärenzsinn. In: Brähler E, Schumacher J, Strauss B, editors. Diagnostische Verfahren in der Psychotherapie. Höttingen: Hogrefe, 2002. p. 326-330.
15Abele AE. Karriereorientierungen angehender Akademikerinnen und Akademiker. Bielefeld: Kleine; 1994.
16 Abele AE , Stief M , Andrä MS . Zur ökonomischen Erfassung beruflicher Selbstwirksamkeitserwartungen: Neukonstruktion einer BSW-Skala. Z Arb Organpsychol. 2000;44(3):145–51. doi:.https://doi.org/10.1026//0932-4089.44.3.145
17 Poehlmann K , Brunstein JC . GOALS: Ein Fragebogen zur Messung von Lebenszielen. Diagnostica. 1997;43:63–79.
18vsao.ch. [Internet]. Bern: Verband Schweizerischer Assistenz- und Oberärztinnen und -ärzte [cited 2018 June 3]. Mitgliederbefragung 2017. Available from: http://www2.vsao.ch/content/default.asp?txtParentID=47&txtCatID=675#collapse1
19 Wenger N , Méan M , Castioni J , Marques-Vidal P , Waeber G , Garnier A . Allocation of internal medicine resident time in a Swiss hospital: a time and motion study of day and evening shifts. Ann Intern Med. 2017;166(8):579–86. doi:.https://doi.org/10.7326/M16-2238
20 Buddeberg-Fischer B , Stamm M , Klaghofer R . Career paths in physicians’ postgraduate training - an eight-year follow-up study. Swiss Med Wkly. 2010;140:w13056. doi:.https://doi.org/10.4414/smw.2010.13056
21 Aaron M , Levenberg P . The millennials in medicine: tips for teaching the next generation of physicians. Journal of Academic Ophthalmology. 2014;7:e17–20.
22 Bassetti S , Héritier F . Wir brauchen ein möglichst flexibles Weiterbildungsprogramm. Schweiz Arzteztg. 2018;99(11):357–8. doi:.https://doi.org/10.4414/saez.2018.06398
23 Gaspoz JM , Héritier F , Aujesky D , Capaul R , Providoli R , Tronnolone D , et al. Allgemeine Innere Medizin: Nachwuchs ins Zentrum gerückt. Schweiz Arzteztg. 2018;99(10):300–2. doi:.https://doi.org/10.4414/saez.2018.06512
24 Armstrong K , Keating NL , Landry M , Crotty BH , Phillips RS , Selker HP ; Council of the Society of General Internal Medicine. Academic general internal medicine: a mission for the future. J Gen Intern Med. 2013;28(6):845–51. doi:.https://doi.org/10.1007/s11606-013-2334-3
25 Aujesky D . Allgemeine Innere Medizin am Universitätsspital. Schweiz Arzteztg. 2015;96:71–4.
26forbes.com. [Internet]. New York: Forbes Magazine [cited 2018 August 25]. Moore K: The modern mentor in a millennial workplace, 11 September 2014. Available from: https://www.forbes.com/consent/?toURL=https://www.forbes.com/sites/karlmoore/2014/09/11/the-modern-mentor-in-a-millennial-workplace/
27 Sambunjak D , Straus SE , Marusić A . Mentoring in academic medicine: a systematic review. JAMA. 2006;296(9):1103–15. doi:.https://doi.org/10.1001/jama.296.9.1103
28 Luckhaupt SE , Chin MH , Mangione CM , Phillips RS , Bell D , Leonard AC , et al. Mentorship in academic general internal medicine. Results of a survey of mentors. J Gen Intern Med. 2005;20(11):1014–8. doi:.https://doi.org/10.1111/j.1525-1497.2005.215.x
29 Chopra V , Arora VM , Saint S . Will you be my mentor? - Four archetypes to help mentees succeed in academic medicine. JAMA Intern Med. 2018;178(2):175–6. doi:.https://doi.org/10.1001/jamainternmed.2017.6537
30 Buddeberg-Fischer B , Stamm M , Marty F . Attraktivitätssteigerung der Hausarztmedizin- Ansichten und Vorschläge von praktizierenden Hausärzten. Prim Care. 2007;42:639–41.
No financial support and no other potential conflict of interest relevant to this article was reported.