Figure 1 Assessment of tongue lacerations.
DOI: https://doi.org/10.4414/smw.2018.14683
Tongue lacerations, usually from falls or sports injuries, are common in children and involve mostly the anterior dorsum of the tongue, followed by the mid-dorsum and anterior ventrum [1–3]. Tongue lacerations may lead to haemorrhage, tongue dysfunction, disfigurement and possible airway obstruction [3, 4].
Choosing an optimal treatment for tongue lacerations remains a challenge due to contradictory recommendations and a lack of current guidelines. Over 40 years ago, English et al. proposed that small lacerations do not need to be sutured when margins are at a good approximation [5]. In the 1990s, several other propositions were made: suturing both dorsum and lateral border injuries [6], loosely suturing tongue wounds and placing deep wounds in layers [7], and suturing only wounds larger than 2 cm or when haemorrhaging is a concern [8]. However, suturing may predispose the tongue to invasive closed space infection [7]. These contradictory guidelines are also confusing for general practitioners and paediatricians, who must often decide which children need to be transferred to a paediatric emergency department (ED) for treatment.
The purpose of a primary wound closure is to approximate the wound edges in order to facilitate the healing process for normal function with minimal risk of infection and give a satisfactory cosmetic result. Most patients are young children and therefore suturing mostly requires general anaesthesia with possible complications. An alternative treatment is to leave the laceration alone to heal secondarily. This is an option because the tongue has a rich vascular supply with an effective regeneration capacity and thus a marked tendency for self-healing [8–10].
The emergency department (ED) of the University Children’s Hospital Zurich treats approximately 30 children with tongue lacerations annually. In recent years, the treatment of choice has shifted from generally suturing the wounds to advising secondary wound healing, mostly with the belief that the outcome is approximately the same. Nevertheless, it is still necessary to define which tongue lacerations benefit from suturing.
The aim of this study is to analyse the tongue lacerations treated at the ED of University Children’s Hospital Zurich in order to develop guidance for the optimal management of tongue lacerations in children.
Patients aged 0 to 16 years who had been diagnosed with a tongue laceration at the ED of the University Children’s Hospital Zurich between 1 January 2010 and 31 August 2015 were included in this retrospective, single-centre cohort study. Exclusion criteria were no informed consent and known coagulation or wound-healing disorders. The local ethics board approved this study.
Clinical records of all the patients included were reviewed and the following data were collected:
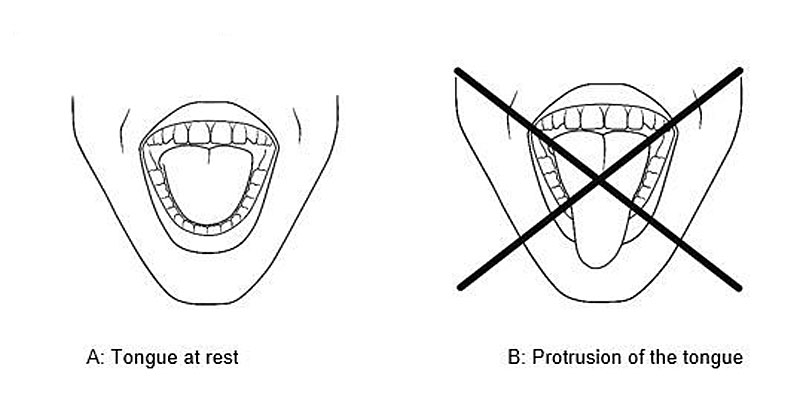
Two procedures were followed. First, whether wound edges were gaping was assessed with the tongue in rest position and not upon protrusion of the tongue, a standardised examination technique at our ED (fig. 1). Second, to complete the data, all families were contacted for informed consent, photo documentation of the healed tongue and a telephone interview. If we did not have photo documentation, we accepted an estimation or description of the wound.
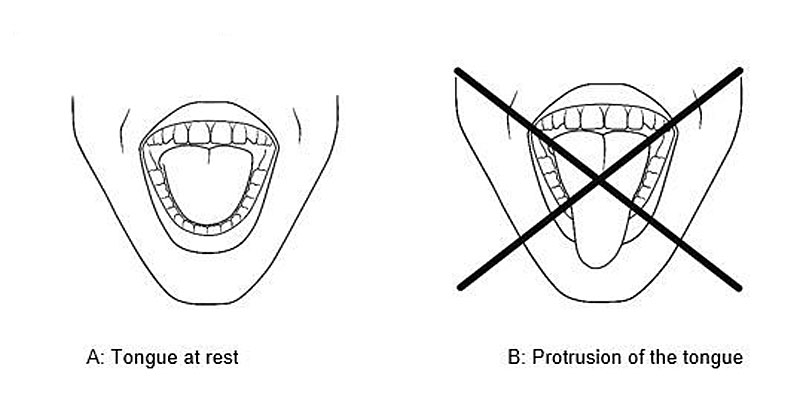
Figure 1 Assessment of tongue lacerations.
Regardless of the method chosen for wound closure, all patients were examined for concomitant injuries, and wounds were carefully inspected for possible foreign bodies, especially teeth fragments. Tongue lacerations were always sutured by an emergency physician with Vicryl® 3-0 or 4-0 (coated polyglactin 910, Ethicon), as well as with single and recessed button sutures. Antibiotics were never prescribed; the only analgesic treatment was with paracetamol or non-steroidal antiphlogistic medication.
Categorical data were described as frequencies, while continuous variables were described as means with standard deviation (SD) or medians, as appropriate. Statistical analyses were performed with the IBM® SPSS® statistics version 24.
A total of 133 children with tongue lacerations were treated during the study period. Sixty (45.1%) patients had to be excluded because there was no informed consent (although families had been contacted up to three times). Overall, 73 (54.9%) cases could be analysed, of which 55 (75.3%) involved boys. The mean age was 4 ± 2.6 years (range: 6 months to 13.5 years).
The time elapsed between the accident and presentation at the ED was 2.6 ± 6.1 hours.
Table 1 illustrates that tongue lacerations on which a primary wound suture was performed were larger than those in the spontaneous healing group, and presented gaping wound edges and involvement of the tongue borders more often. None of our tongue lacerations were complex injuries with active haemorrhage or bisecting wounds.
Table 1 Age, wound characteristics, and outcome in the two intervention groups.
|
Primary wound suture
(n = 12) |
Secondary wound
healing (n = 61) |
Total
(n = 73) |
p-value | |
|---|---|---|---|---|
| Age in years, mean ± SD | 4.5 ± 3.3 | 3.9 ±2.5 | 4.0 ± 2.6 | 0.488 |
| Length of tongue laceration in mm, mean ± SD | 21.0 ± 10.0 | 10.8 ± 6.8 | 12.5 ± 8.3 | 0.000 |
| Gaping wound edges, n (%) | 11 (91.7%) | 20 (32.8%) | 31 (42.5%) | 0.000 |
| Tongue border involvement, n (%) | 11 (91.7%) | 40 (65.6%) | 51 (69.9%) | 0.114 |
| Tip of the tongue, n | 6 | 16 | 22 | |
| Lateral tongue, n | 5 | 24 | 29 | |
| Through-and-through, n (%) | 11 (91.7%) | 12 (19.7%) | 23 (31.5%) | 0.000 |
| Complications, n (%) | 3 (25%) | 2 (3.3%) | 5 (6.8%) | 0.029 |
| Duration of complaints in days, mean ± SD | 32.4 ± 49.2 | 11.2 ± 23.8 | 14.7 ± 30.1 | 0.025 |
| SD = standard deviation | ||||
A remaining scar existed in 28 (38.4%) treated patients, of which seven were primary sutured due to gaping wounds, six had a through-and-through laceration and five had affected tongue borders.
The median duration of complaints was 13 days in the sutured group and 6.2 days in the spontaneous healing group.
In 81% of cases, the time interval between the ED visit and the standardized telephone interview was twelve months or longer.
Examples of tongue lacerations at the time of the accident and after healing can be seen in figure 2.
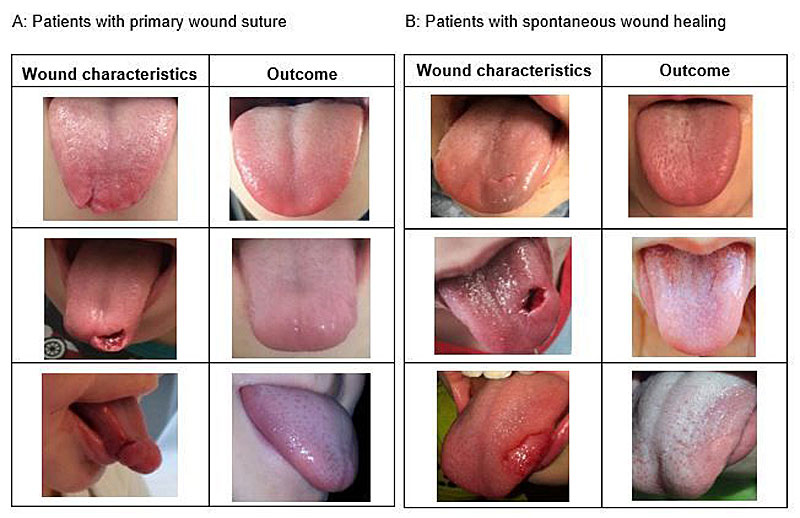
Figure 2 Tongue lacerations before and after treatment.
The optimal treatment of a child presenting with a tongue laceration is a challenge for the treating medical team, with the question of whether to suture or not. The results of our study indicate that most tongue lacerations probably do not require suturing due to the tongue’s marked regeneration capacity.
Most patients in our study were young children with a mean age of 4 years, a majority of whom were boys. This result is in line with previous research that has demonstrated that there are more male patients in this age group [11]. Many parents came directly to the ED within 3 hours of the injury, other parents were referred to our ED for tongue laceration treatment by general practitioners or paediatricians in light of their previous experience.
Tongue lacerations were mostly located at the anterior dorsum of the tongue and the mean size was approximately 12 mm. Although the tongue borders were involved in 51 cases (69.9%), suturing was only performed in 11 of them (21.6%). Thus, it is likely that the decisive factors determining whether a primary wound closure was performed were the length of the tongue laceration and whether the wound edges were gaping when the tongue was at rest rather than the involvement of the tongue border. Furthermore, we recommend that a tongue laceration be assessed with the tongue at rest because this position is the most frequent position. If wound edges are not gaping in this position, then the chances of a satisfactory secondary wound healing are high.
Not suturing, a conservative wound management of tongue lacerations, seems to pose fewer disadvantages, is less traumatic for the child and parents, and entails less time and fewer costs than suturing. An alternative treatment with tissue adhesive was suggested by Rudresh et al. [12] and Flinzberg et al. [13] in individual cases; however, it remains unclear whether no intervention might have resulted in the same outcome.
The decision to suture a tongue laceration in a child needs to be assessed carefully. Normally, the surgical procedure must be performed under general anaesthesia, which incurs potential risks. Furthermore, children occasionally lose their sutures shortly after the operation because they chew on the stiches [3]. This is why we recommend a suture technique with single and recessed button sutures and with absorbable thread of sufficient thickness (e.g., Vicryl® 3-0/4-0). Moreover, suturing does not in general improve functional and cosmetic outcomes [12]. Complex tongue lacerations which require repair are bisecting wounds, large flaps, and wounds with active haemorrhage [14].
The tongue lacerations we analysed resulted in desirable outcomes with normal functioning after healing, with only a small number of complications (6.8% of cases). For example, granuloma may develop after wound suturing with non-absorbable material due to a foreign-body reaction [15]. Impairments to wound healing due to granuloma formation were noted in 5.5% of children. This resolved itself spontaneously in 75% (3 of the 4 children) of cases. Lisping occurred in one child (1.4%) after wound suturing. No wound infection occurred, which indicates both that secondary wound closure does not increase the risk of infection and that there is no need for antibiotic prophylaxis.
A scar was noticed in 38.4% of patients. In the conservative management group (no sutures), the rate was 34.4% (21/61 patients), whereas in the surgical management group (sutures) it was 58.3% (7/12 patients). The injuries in the primary wound closure group were probably more severe than in the secondary wound closure group, which might explain the higher rate of scarring. The duration of complaints also lasted twice as long in the primary wound closure group (2 weeks) than the secondary wound closure group (1 week).
The Zurich Tongue Scheme (ZTS) is a method, based on the data from our study, to identify which tongue lacerations in children benefit from suturing (fig. 3). As well as complex tongue lacerations with functional loss of the tongue (bisecting wounds and large flaps) and persistent active haemorrhage, the following tongue injuries with gaping wound edges in a rest position seem to benefit from a primary wound closure: tongue lacerations affecting the tip of the tongue and those with a length of more than 2 cm on the dorsum of the tongue. Not suturing these lacerations could result in either an unsatisfactory cosmetic outcome on the tip of the tongue or delayed wound healing. The ZTS is also intended as a guide to the correct selection of patients who need to be transferred to an ED for suturing. It should thus assist all caregivers and paediatricians as they make decisions on whether to suture or not. Nevertheless, regardless of the choice of wound management, clinicians need to assess the wound carefully so as not to overlook foreign bodies and to rule out the involvement of teeth injuries.
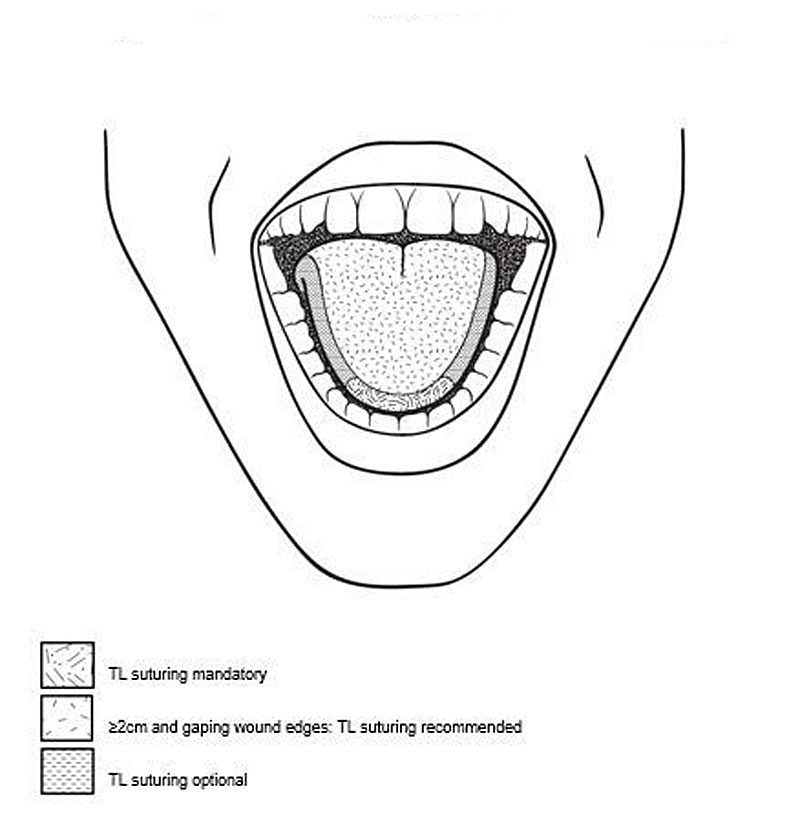
Figure 3 Zurich Tongue Scheme for non-complex tongue lacerations in children.
This was a retrospective study and therefore entails a number of limitations. First, these results cannot be generalised because it was monocentric. Second, no randomisation was performed because each treating ED physician chose the treatment regime. Third, the documentation concerning wound size and the duration of complaints was sometimes imprecise because it was estimated by the parents. Additionally, the standard deviations regarding the length of tongue lacerations, especially in the secondary wound healing group, were large, probably due to clinicians missing guidelines and accepting larger wounds for spontaneous healing over the years. Fourth, the retrospective methodology meant that no wound controls were assessed in a standard way. We therefore recommend that a prospective, randomised trial be conducted to assess the ZTS.
Tongue lacerations typically occur in young children and therefore careful assessment is needed to determine whether a primary wound closure under general anaesthesia, with its possible related complications, is required. We recommend the ZTS as a guide for caregivers/physicians when they make their decisions; we also recommend conservative wound management, even in lacerations with gaping wound edges, for all tongue lacerations smaller than 2 cm, except if the tip of the tongue is affected.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Bolt RW , Watts PG . The relationship between aetiology and distribution of facial lacerations. Inj Extra. 2004;35(1):6–11. doi:.https://doi.org/10.1016/j.injury.2003.11.010
2 Bringhurst C , Herr RD , Aldous JA . Oral trauma in the emergency department. Am J Emerg Med. 1993;11(5):486–90. doi:.https://doi.org/10.1016/0735-6757(93)90091-O
3 Lamell CW , Fraone G , Casamassimo PS , Wilson S . Presenting characteristics and treatment outcomes for tongue lacerations in children. Pediatr Dent. 1999;21(1):34–8.
4 Banks K , Merlino PG . Minor oral injuries in children. Mt Sinai J Med. 1998;65(5-6):333–42.
5English GM. Otolaryngology. New York: Harper and Row; 1976. p 463.
6Andreasen JO, Andreasen FM. Textbook and color atlas of traumatic injuries to the teeth. St Louis: Mosby-Year; 2007. pp 587–93.
7Powers MP, Bertz J, Fonseca RJ. Management of soft tissue injuries. In: Fonseca RJ, Walker RV, editors. Oral and maxillofacial trauma. Philadelphia: WB Saunders; 1991. pp 618–48.
8Donat TL, Maisel RH, Mathog RH. Injuries to the mouth, pharynx and esophagus. In: Bluestone CD, Stool SE, Kenna MA, editors. Pediatric otolaryngology 3rd ed. Philadelphia: WB Saunders; 1996. pp 1183–4.
9Touloukian RJ. Pediatric trauma. St. Louis: CV Mosby; 1990. p 204.
10 Ud-din Z , Aslam M , Gull S . Should minor mucosal tongue lacerations be sutured in children? Emerg Med J. 2007;24(2):123–4. doi:.https://doi.org/10.1136/emj.2006.045211
11 Morrongiello BA , Ondejko L , Littlejohn A . Understanding toddlers’ in-home injuries: I. Context, correlates, and determinants. J Pediatr Psychol. 2004;29(6):415–31. doi:.https://doi.org/10.1093/jpepsy/jsh046
12 Rudresh KB , Prashanth R , Bhattacharjee B , Vinod B , Nandan RP . Paediatric tongue laceration – a unique repair. Int J Oral Health Med Res. 2016;3(3):50–3.
13 Flinzberg S , Friedrich RE , Vesper M , Schmelzle R . Komplikation bei der Anwendung des 2-Octyl-Cyanoacrylat-Gewebeklebers (Dermabond) [Injury by the use of 2-octocyanoacrylate tissue adhesive Dermabond]. Trauma und Berufskrankheit. 2001;3(2):156–8. Article in German. doi:.https://doi.org/10.1007/s100390100419
14 Brown DJ , Jaffe JE , Henson JK . Advanced laceration management. Emerg Med Clin North Am. 2007;25(1):83–99. doi:.https://doi.org/10.1016/j.emc.2006.11.001
15 Rettenbacher T , Macheiner P , Hollerweger A , Gritzmann N , Weismann C , Todoroff B . Suture granulomas: sonography enables a correct preoperative diagnosis. Ultrasound Med Biol. 2001;27(3):343–50. doi:.https://doi.org/10.1016/S0301-5629(00)00364-1
No financial support and no other potential conflict of interest relevant to this article was reported.